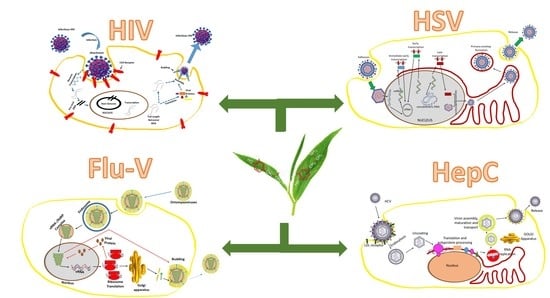
Bioactive Natural Antivirals: An Updated Review of the Available Plants and Isolated Molecules
Abstract
:1. Introduction
2. Methodology
3. Human Immunodeficiency Virus (HIV)
4. Herpes Simplex Virus
5. Influenza Virus
6. Hepatitis C Virus
7. Conclusions
Funding
Acknowledgments
Conflicts of Interest
References
- Wang, S.-X.; Wang, Y.; Lu, Y.-B.; Li, J.-Y.; Song, Y.-J.; Nyamgerelt, M.; Wang, X.-X. Diagnosis and treatment of novel coronavirus pneumonia based on the theory of traditional Chinese medicine. J. Integr. Med. 2020, 18, 275–283. [Google Scholar] [CrossRef]
- Brito, A.F.; Pinney, J.W. Protein-protein interactions in virus—host systems. Front. Microbiol. 2017, 8, 1557. [Google Scholar] [CrossRef] [PubMed]
- Virgin, H.W.; Wherry, E.J.; Ahmed, R. Redefining chronic viral infection. Cell 2009, 138, 30–50. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Deigendesch, N.; Stenzel, W. Acute and chronic viral infections. In Handbook of Clinical Neurology; Elsevier: Amsterdam, The Nederlands, 2018; Volume 145, pp. 227–243. [Google Scholar]
- Bhutta, Z.A.; Sommerfeld, J.; Lassi, Z.S.; Salam, R.A.; Das, J.K. Global burden, distribution, and interventions for infectious diseases of poverty. Infect. Dis. Poverty 2014, 3, 21. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ribeiro, R.M.; Bonhoeffer, S.; Nowak, M.A. The frequency of resistant mutant virus before antiviral therapy. AIDS 1998, 12, 461–465. [Google Scholar] [CrossRef]
- Martinez, J.; Sasse, F.; Brönstrup, M.; Diez, J.; Meyerhans, A. Antiviral drug discovery: Broad-spectrum drugs from nature. Nat. Prod. Rep. 2015, 32, 29–48. [Google Scholar] [CrossRef] [PubMed]
- Farnsworth, N.R.; Akerele, O.; Bingel, A.S.; Soejarto, D.D.; Guo, Z. Medicinal plants in therapy. Bull. World Health Organ. 1985, 63, 965. [Google Scholar] [CrossRef] [Green Version]
- Solecki, R.S. Shanidar IV, a Neanderthal flower burial in northern Iraq. Science 1975, 190, 880–881. [Google Scholar] [CrossRef]
- Pandey, A.; Galvani, A.P. The global burden of HIV and prospects for control. Lancet HIV 2019, 6, e809–e811. [Google Scholar] [CrossRef] [Green Version]
- Lazarus, J.V.; Safreed-Harmon, K.; Barton, S.E.; Costagliola, D.; Dedes, N.; del Amo Valero, J.; Gatell, J.M.; Baptista-Leite, R.; Mendão, L.; Porter, K. Beyond viral suppression of HIV—The new quality of life frontier. BMC Med. 2016, 14, 94. [Google Scholar] [CrossRef]
- Frank, T.D.; Carter, A.; Jahagirdar, D.; Biehl, M.H.; Douwes-Schultz, D.; Larson, S.L.; Arora, M.; Dwyer-Lindgren, L.; Steuben, K.M.; Abbastabar, H. Global, regional, and national incidence, prevalence, and mortality of HIV, 1980–2017, and forecasts to 2030, for 195 countries and territories: A systematic analysis for the Global Burden of Diseases, Injuries, and Risk Factors Study 2017. Lancet HIV 2019, 6, e831–e859. [Google Scholar] [CrossRef] [Green Version]
- International Committee on Taxonomy of Viruses. 61.0.6. Lentivirus. National Institutes of Health. Available online: http://www.ncbi.nlm.nih.gov/ICTVdb/ICTVdB/61060000.htm (accessed on 9 October 2020).
- Soudeyns, H.; Champagne, P.; Holloway, C.L.; Silvestri, G.U.; Ringuette, N.; Samson, J.; Lapointe, N.; Sékaly, R.-P. Transient T cell receptor β-chain variable region-specific expansions of CD4+ and CD8+ T cells during the early phase of pediatric human immunodeficiency virus infection: Characterization of expanded cell populations by T cell receptor phenotyping. J. Infect. Dis. 2000, 181, 107–120. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Varmus, H. Regulation of HIV and HTLV gene expression. Genes Dev. 1988, 2, 1055–1062. [Google Scholar] [CrossRef] [Green Version]
- Yang, S.S.; Cragg, G.M.; Newman, D.J.; Bader, J.P. Natural product-based anti-HIV drug discovery and development facilitated by the NCI developmental therapeutics program. J. Nat. Prod. 2001, 64, 265–277. [Google Scholar] [CrossRef] [PubMed]
- Vaishnav, Y.N.; Wong-Staal, F. The biochemistry of AIDS. Annu. Rev. Biochem. 1991, 60, 577–630. [Google Scholar] [CrossRef] [PubMed]
- Kuznetsov, Y.G.; McPherson, A. Atomic force microscopy in imaging of viruses and virus-infected cells. Microbiol. Mol. Biol. Rev. 2011, 75, 268–285. [Google Scholar] [CrossRef] [Green Version]
- Tanser, F.; Bärnighausen, T.; Grapsa, E.; Zaidi, J.; Newell, M.-L. High coverage of ART associated with decline in risk of HIV acquisition in rural KwaZulu-Natal, South Africa. Science 2013, 339, 966–971. [Google Scholar] [CrossRef] [Green Version]
- Bangsberg, D.R.; Kroetz, D.L.; Deeks, S.G. Adherence-resistance relationships to combination HIV antiretroviral therapy. Curr. HIV/AIDS Rep. 2007, 4, 65. [Google Scholar] [CrossRef]
- Bock, C.; Lengauer, T. Managing drug resistance in cancer: Lessons from HIV therapy. Nat. Rev. Cancer 2012, 12, 494–501. [Google Scholar] [CrossRef]
- Cragg, G.; Newman, D. Plants as a source of anti-cancer and anti-HIV agents. Ann. Appl. Biol. 2003, 143, 127–133. [Google Scholar] [CrossRef]
- Barreca, M.L.; Ferro, S.; Rao, A.; De Luca, L.; Zappalà, M.; Monforte, A.-M.; Debyser, Z.; Witvrouw, M.; Chimirri, A. Pharmacophore-based design of HIV-1 integrase strand-transfer inhibitors. J. Med. Chem. 2005, 48, 7084–7088. [Google Scholar] [CrossRef] [PubMed]
- De Clercq, E. The role of non-nucleoside reverse transcriptase inhibitors (NNRTIs) in the therapy of HIV-1 infection. Antivir. Res. 1998, 38, 153–179. [Google Scholar] [CrossRef]
- Nair, V.; Chi, G. HIV integrase inhibitors as therapeutic agents in AIDS. Rev. Med Virol. 2007, 17, 277–295. [Google Scholar] [CrossRef] [PubMed]
- Meixenberger, K.; Yousef, K.P.; Smith, M.R.; Somogyi, S.; Fiedler, S.; Bartmeyer, B.; Hamouda, O.; Bannert, N.; von Kleist, M.; Kücherer, C. Molecular evolution of HIV-1 integrase during the 20 years prior to the first approval of integrase inhibitors. Virol. J. 2017, 14, 223. [Google Scholar] [CrossRef] [Green Version]
- Tewtrakul, S.; Subhadhirasakul, S.; Kummee, S. Anti-HIV-1 integrase activity of medicinal plants used as self medication by AIDS patients. Songklanakarin J. Sci. Technol. 2006, 28, 785–790. [Google Scholar]
- Basu, V.P.; Song, M.; Gao, L.; Rigby, S.T.; Hanson, M.N.; Bambara, R.A. Strand transfer events during HIV-1 reverse transcription. Virus Res. 2008, 134, 19–38. [Google Scholar] [CrossRef]
- Flexner, C. HIV-protease inhibitors. N. Engl. J. Med. 1998, 338, 1281–1293. [Google Scholar] [CrossRef]
- Gills, J.J.; LoPiccolo, J.; Tsurutani, J.; Shoemaker, R.H.; Best, C.J.; Abu-Asab, M.S.; Borojerdi, J.; Warfel, N.A.; Gardner, E.R.; Danish, M. Nelfinavir, A lead HIV protease inhibitor, is a broad-spectrum, anticancer agent that induces endoplasmic reticulum stress, autophagy, and apoptosis in vitro and in vivo. Clin. Cancer Res. 2007, 13, 5183–5194. [Google Scholar] [CrossRef] [Green Version]
- Siwe-Noundou, X.; Ndinteh, D.; Olivier, D.; Mnkandhla, D.; Isaacs, M.; Muganza, F.; Mbafor, J.; Van Vuuren, S.; Patnala, S.; Hoppe, H. Biological activity of plant extracts and isolated compounds from Alchornea laxiflora: Anti-HIV, antibacterial and cytotoxicity evaluation. S. Afr. J. Bot. 2019, 122, 498–503. [Google Scholar] [CrossRef]
- Suedee, A.; Tewtrakul, S.; Panichayupakaranant, P. Anti-HIV-1 integrase activity of Mimusops elengi leaf extracts. Pharm. Biol. 2014, 52, 58–61. [Google Scholar] [CrossRef] [Green Version]
- Kapewangolo, P.; Tawha, T.; Nawinda, T.; Knott, M.; Hans, R. Sceletium tortuosum demonstrates in vitro anti-HIV and free radical scavenging activity. S. Afr. J. Bot. 2016, 106, 140–143. [Google Scholar] [CrossRef]
- Kapewangolo, P.; Knott, M.; Shithigona, R.E.; Uusiku, S.L.; Kandawa-Schulz, M. In vitro anti-HIV and antioxidant activity of Hoodia gordonii (Apocynaceae), a commercial plant product. BMC Complement. Altern. Med. 2016, 16, 1–7. [Google Scholar] [CrossRef] [Green Version]
- Au, T.; Lam, T.; Ng, T.; Fong, W.; Wan, D. A comparison of HIV-1 integrase inhibition by aqueous and methanol extracts of Chinese medicinal herbs. Life Sci. 2001, 68, 1687–1694. [Google Scholar] [CrossRef]
- Bunluepuech, K.; Tewtrakul, S. Anti-HIV-1 integrase activity of Thai medicinal plants in longevity preparations. Sonklanakarin J. Sci. Technol. 2011, 33, 693. [Google Scholar]
- Lee, J.S.; Kim, H.J.; Lee, Y.S. A new anti-HIV flavonoid glucuronide from Chrysanthemum morifolium. Planta Med. 2003, 69, 859–861. [Google Scholar] [PubMed]
- Matsuse, I.; Lim, Y.; Hattori, M.; Correa, M.; Gupta, M. A search for anti-viral properties in Panamanian medicinal plants: The effects on HIV and its essential enzymes. J. Ethnopharmacol. 1998, 64, 15–22. [Google Scholar] [CrossRef]
- Narayan, C.; Rai, R.V.; Tewtrakul, S. A screening strategy for selection of anti-HIV-1 integrase and anti-HIV-1 protease inhibitors from extracts of Indian medicinal plants. Int. J. Phytomed. 2011, 3, 312. [Google Scholar]
- Chaniad, P.; Wattanapiromsakul, C.; Pianwanit, S.; Tewtrakul, S. Anti-HIV-1 integrase compounds from Dioscorea bulbifera and molecular docking study. Pharm. Biol. 2016, 54, 1077–1085. [Google Scholar] [CrossRef] [Green Version]
- Kim, H.K.; Lee, H.-K.; Shin, C.-G.; Huh, H. HIV integrase inhibitory activity ofAgastache rugosa. Arch. Pharmacal Res. 1999, 22, 520–523. [Google Scholar] [CrossRef]
- Geuenich, S.; Goffinet, C.; Venzke, S.; Nolkemper, S.; Baumann, I.; Plinkert, P.; Reichling, J.; Keppler, O.T. Aqueous extracts from peppermint, sage and lemon balm leaves display potent anti-HIV-1 activity by increasing the virion density. Retrovirology 2008, 5, 27. [Google Scholar] [CrossRef] [Green Version]
- Min, B.S.; Bae, K.H.; Kim, Y.H.; Shimotono, K.; Miyashiro, H.; Hattori, M. Inhibitory activities of Korean plants on HIV-1 protease. Nat. Prod. Sci. 1998, 4, 241–244. [Google Scholar]
- Eid, A.M.M.; Elmarzugi, N.A.; El-Enshasy, H.A. A review on the phytopharmacological effect of Swietenia macrophylla. Int. J. Pharm. Pharm. Sci. 2013, 3, 5. [Google Scholar]
- Asres, K.; Bucar, F.; Kartnig, T.; Witvrouw, M.; Pannecouque, C.; De Clercq, E. Antiviral activity against human immunodeficiency virus type 1 (HIV-1) and type 2 (HIV-2) of ethnobotanically selected Ethiopian medicinal plants. Phytother. Res. Int. J. Devoted Pharmacol. Toxicol. Eval. Nat. Prod. Deriv. 2001, 15, 62–69. [Google Scholar] [CrossRef]
- Rege, A.A.; Ambaye, R.Y.; Deshmukh, R.A. Evaluation of in vitro inhibitory effect of selected plants and Shilajit on HIV-reverse transcriptase. Indian J. Nat. Prod. Resour. 2012, 3, 145–151. [Google Scholar]
- Woradulayapinij, W.; Soonthornchareonnon, N.; Wiwat, C. In vitro HIV type 1 reverse transcriptase inhibitory activities of Thai medicinal plants and Canna indica L. rhizomes. J. Ethnopharmacol. 2005, 101, 84–89. [Google Scholar] [CrossRef]
- Silprasit, K.; Seetaha, S.; Pongsanarakul, P.; Hannongbua, S.; Choowongkomon, K. Anti-HIV-1 reverse transcriptase activities of hexane extracts from some Asian medicinal plants. J. Med. Plants Res 2011, 5, 4194–4201. [Google Scholar]
- Grzybek, J.; Wongpanich, V.; Mata-Greenwood, E.; Angerhofer, C.K.; Pezzuto, J.M.; Cordell, G.A. Biological evaluation of selected plants from Poland. Int. J. Pharm. 1997, 35, 1–5. [Google Scholar] [CrossRef]
- Mlinaric, A.; Kreft, S.; Umek, A.; Strukelj, B. Screening of selected plant extracts for in vitro inhibitory activity on HIV-1 reverse transcriptase (HIV-1 RT). Die Pharm. 2000, 55, 75–77. [Google Scholar]
- Gujjeti, R.P.; Mamidala, E. Anti-HIV activity of phytosterol isolated from Aerva lanata roots. Pharm. J. 2017, 9, 112–116. [Google Scholar] [CrossRef] [Green Version]
- Ali, H.; König, G.; Khalid, S.; Wright, A.; Kaminsky, R. Evaluation of selected Sudanese medicinal plants for their in vitro activity against hemoflagellates, selected bacteria, HIV-1-RT and tyrosine kinase inhibitory, and for cytotoxicity. J. Ethnopharmacol. 2002, 83, 219–228. [Google Scholar] [CrossRef]
- McMahon, J.B.; Currens, M.J.; Gulakowski, R.J.; Buckheit, R.; Lackman-Smith, C.; Hallock, Y.F.; Boyd, M.R. Michellamine B, a novel plant alkaloid, inhibits human immunodeficiency virus-induced cell killing by at least two distinct mechanisms. Antimicrob. Agents Chemother. 1995, 39, 484–488. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bicchi, C.; Rubiolo, P.; Ballero, M.; Sanna, C.; Matteodo, M.; Esposito, F.; Zinzula, L.; Tramontano, E. HIV-1-inhibiting activity of the essential oil of Ridolfia segetum and Oenanthe crocata. Planta Med. 2009, 75, 1331–1335. [Google Scholar] [CrossRef] [PubMed]
- Esposito, F.; Mandrone, M.; Del Vecchio, C.; Carli, I.; Distinto, S.; Corona, A.; Lianza, M.; Piano, D.; Tacchini, M.; Maccioni, E. Multi-target activity of Hemidesmus indicus decoction against innovative HIV-1 drug targets and characterization of Lupeol mode of action. Pathog. Dis. 2017, 75, ftx065. [Google Scholar] [CrossRef]
- Rukunga, G.M.; Kofi-Tsekpo, M.W.; Kurokawa, M.; Kageyama, S.; Mungai, G.M.; Muli, J.M.; Tolo, F.M.; Kibaya, R.M.; Muthaura, C.N.; Kanyara, J.N. Evaluation of the HIV-1 reverse transcriptase inhibitory properties of extracts from some medicinal plants in Kenya. Afr. J. Health Sci. 2002, 9, 81–90. [Google Scholar] [CrossRef] [Green Version]
- Chukwujekwu, J.; Ndhlala, A.; De Kock, C.; Smith, P.; Van Staden, J. Antiplasmodial, HIV-1 reverse transcriptase inhibitory and cytotoxicity properties of Centratherum punctatum Cass. and its fractions. S. Afr. J. Bot. 2014, 90, 17–19. [Google Scholar] [CrossRef] [Green Version]
- Hnatyszyn, O.; Broussalis, A.; Herrera, G.; Muschietti, L.; Coussio, J.; Martino, V.; Ferraro, G.; Font, M.; Monge, A.; Martínez-Irujo, J.J. Argentine plant extracts active against polymerase and ribonuclease H activities of HIV-1 reverse transcriptase. Phytother. Res. 1999, 13, 206–209. [Google Scholar] [CrossRef] [Green Version]
- Harnett, S.; Oosthuizen, V.D.V.; Van de Venter, M. Anti-HIV activities of organic and aqueous extracts of Sutherlandia frutescens and Lobostemon trigonus. J. Ethnopharmacol. 2005, 96, 113–119. [Google Scholar] [CrossRef]
- Bedoya, L.M.; Beltrán, M.; Sancho, R.; Olmedo, D.A.; Sánchez-Palomino, S.; del Olmo, E.; López-Pérez, J.L.; Muñoz, E.; San Feliciano, A.; Alcamí, J. 4-Phenylcoumarins as HIV transcription inhibitors. Bioorganic Med. Chem. Lett. 2005, 15, 4447–4450. [Google Scholar] [CrossRef]
- Chang, C.-W.; Lin, M.-T.; Lee, S.-S.; Liu, K.C.C.; Hsu, F.-L.; Lin, J.-Y. Differential inhibition of reverse transcriptase and cellular DNA polymerase-α activities by lignans isolated from Chinese herbs, Phyllanthus myrtifolius Moon, and tannins from Lonicera japonica Thunb and Castanopsis hystrix. Antivir. Res. 1995, 27, 367–374. [Google Scholar] [CrossRef]
- Bessong, P.O.; Obi, C.L.; Andréola, M.-L.; Rojas, L.B.; Pouységu, L.; Igumbor, E.; Meyer, J.M.; Quideau, S.; Litvak, S. Evaluation of selected South African medicinal plants for inhibitory properties against human immunodeficiency virus type 1 reverse transcriptase and integrase. J. Ethnopharmacol. 2005, 99, 83–91. [Google Scholar] [CrossRef]
- Mamidala, E.; Paindla, P.; Gurrapu, S. Hiv-1 Reverse Transcriptase Inhibition by Phenolic Compounds Isolated From Acalypha Indica (L.) Plant Leaves Extract. Int. J. Appl. Bioeng. 2017, 11, 17–21. [Google Scholar]
- Fang, E.F.; Lin, P.; Wong, J.H.; Tsao, S.W.; Ng, T.B. A lectin with anti-HIV-1 reverse transcriptase, antitumor, and nitric oxide inducing activities from seeds of Phaseolus vulgaris cv. extralong autumn purple bean. J. Agric. Food Chem. 2010, 58, 2221–2229. [Google Scholar] [CrossRef]
- Thayil Seema, M.; Thyagarajan, S. Methanol and aqueous extracts of Ocimum kilimandscharicum (Karpuratulasi) inhibits HIV-1 reverse transcriptase in vitro. Int. J. Pharm. Pharmacogn. Res. 2016, 8, 1099–1103. [Google Scholar]
- Lavignon, M.; Bertrand, J.-R.; Rayner, B.; Imbach, J.-L.; Malvy, C.; Paoletti, C. Inhibition of Moloney murine leukemia virus reverse transcriptase by α-anomeric oligonucleotides. Biochem. Biophys. Res. Commun. 1989, 161, 1184–1190. [Google Scholar] [CrossRef]
- Esposito, F.; Sanna, C.; Del Vecchio, C.; Cannas, V.; Venditti, A.; Corona, A.; Bianco, A.; Serrilli, A.M.; Guarcini, L.; Parolin, C. Hypericum hircinum L. components as new single-molecule inhibitors of both HIV-1 reverse transcriptase-associated DNA polymerase and ribonuclease H activities. Pathog. Dis. 2013, 68, 116–124. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alam, M.S.; Quader, M.; Rashid, M. HIV-inhibitory diterpenoid from Anisomeles indica. Fitoterapia 2000, 71, 574–576. [Google Scholar] [CrossRef]
- Miraj, S.; Azizi, N.; Kiani, S. A review of chemical components and pharmacological effects of Melissa officinalis L. Pharm. Lett. 2016, 8, 229–237. [Google Scholar]
- Kapewangolo, P.; Omolo, J.J.; Fonteh, P.; Kandawa-Schulz, M.; Meyer, D. Triterpenoids from Ocimum labiatum activates latent HIV-1 expression in vitro: Potential for use in adjuvant therapy. Molecules 2017, 22, 1703. [Google Scholar] [CrossRef] [Green Version]
- Hatano, T.; Yasuhara, T.; Matsuda, M.; Yazaki, K.; Yoshida, T.; Okuda, T. Oenothein B, a dimeric hydrolyzable tannin of cyclic structure. Chem. Pharm. Bull. 1989, 37, 2269–2271. [Google Scholar] [CrossRef] [Green Version]
- Ogata, T.; Higuchi, H.; Mochida, S.; Matsumoto, H.; Kato, A.; Endo, T.; Kaji, A.; Kaji, H. HIV-1 reverse transcriptase inhibitor from Phyllanthus niruri. Aids Res. Hum. Retrovir. 1992, 8, 1937–1944. [Google Scholar] [CrossRef]
- Esposito, F.; Carli, I.; Del Vecchio, C.; Xu, L.; Corona, A.; Grandi, N.; Piano, D.; Maccioni, E.; Distinto, S.; Parolin, C. Sennoside A, derived from the traditional Chinese medicine plant Rheum L. is a new dual HIV-1 inhibitor effective on HIV-1 replication. Phytomedicine 2016, 23, 1383–1391. [Google Scholar] [CrossRef] [PubMed]
- Reutrakul, V.; Krachangchaeng, C.; Tuchinda, P.; Pohmakotr, M.; Jaipetch, T.; Yoosook, C.; Kasisit, J.; Sophasan, S.; Sujarit, K.; Santisuk, T. Cytotoxic and anti-HIV-1 constituents from leaves and twigs of Gardenia tubifera. Tetrahedron 2004, 60, 1517–1523. [Google Scholar] [CrossRef]
- Xu, H.X.; Wan, M.; Loh, B.N.; Kon, O.L.; Chow, P.W.; Sim, K.Y. Screening of Traditional Medicines for their Inhibitory Activity against HIV-1 Protease. Phytother. Res. 1996, 10, 207–210. [Google Scholar] [CrossRef]
- Kusumoto, I.T.; Nakabayashi, T.; Kida, H.; Miyashiro, H.; Hattori, M.; Namba, T.; Shimotohno, K. Screening of various plant extracts used in ayurvedic medicine for inhibitory effects on human immunodeficiency virus type 1 (HIV-1) protease. Phytother. Res. 1995, 9, 180–184. [Google Scholar] [CrossRef]
- Tewtrakul, S.; Subhadhirasakul, S.; Cheenpracha, S.; Karalai, C. HIV-1 protease and HIV-1 integrase inhibitory substances from Eclipta prostrata. Phytother. Res. Int. J. Devoted Pharmacol. Toxicol. Eval. Nat. Prod. Deriv. 2007, 21, 1092–1095. [Google Scholar]
- Min, B.S.; Bae, K.H.; Kim, Y.H.; Miyashiro, H.; Hattori, M.; Shimotohno, K. Screening of Korean plants against human immunodeficiency virus type 1 protease. Phytother. Res. Int. J. Devoted Pharmacol. Toxicol. Eval. Nat. Prod. Deriv. 1999, 13, 680–682. [Google Scholar] [CrossRef]
- Chingwaru, W.; Vidmar, J.; Kapewangolo, P.T. The potential of sub-saharan african plants in the management of human immunodeficiency virus infections: A review. Phytother. Res. 2015, 29, 1452–1487. [Google Scholar] [CrossRef] [PubMed]
- Magadula, J.J.; Tewtrakul, S. Anti-HIV-1 protease activities of crude extracts of some Garcinia species growing in Tanzania. Afr. J. Biotechnol. 2010, 9. [Google Scholar] [CrossRef] [Green Version]
- Asres, K.; Seyoum, A.; Veeresham, C.; Bucar, F.; Gibbons, S. Naturally derived anti-HIV agents. Phytother. Res. Int. J. Devoted Pharmacol. Toxicol. Eval. Nat. Prod. Deriv. 2005, 19, 557–581. [Google Scholar] [CrossRef]
- Zhang, C.-F.; Nakamura, N.; Tewtrakul, S.; Hattori, M.; Sun, Q.-S.; Wang, Z.-T.; Fujiwara, T. Sesquiterpenes and alkaloids from Lindera chunii and their inhibitory activities against HIV-1 integrase. Chem. Pharm. Bull. 2002, 50, 1195–1200. [Google Scholar] [CrossRef] [Green Version]
- Jiang, C.; Luo, P.; Zhao, Y.; Hong, J.; Morris-Natschke, S.L.; Xu, J.; Chen, C.-H.; Lee, K.-H.; Gu, Q. Carolignans from the aerial parts of Euphorbia sikkimensis and their anti-HIV activity. J. Nat. Prod. 2016, 79, 578–583. [Google Scholar] [CrossRef] [Green Version]
- Modi, M.; Dezzutti, C.S.; Kulshreshtha, S.; Rawat, A.K.S.; Srivastava, S.K.; Malhotra, S.; Verma, A.; Ranga, U.; Gupta, S.K. Extracts from Acacia catechu suppress HIV-1 replication by inhibiting the activities of the viral protease and Tat. Virol. J. 2013, 10, 309. [Google Scholar]
- Wang, H.; Ng, T. Ascalin, a new anti-fungal peptide with human immunodeficiency virus type 1 reverse transcriptase-inhibiting activity from shallot bulbs. Peptides 2002, 23, 1025–1029. [Google Scholar] [CrossRef]
- Gómez-Cansino, R.; Espitia-Pinzón, C.I.; Campos-Lara, M.G.; Guzmán-Gutiérrez, S.L.; Segura-Salinas, E.; Echeverría-Valencia, G.; Torras-Claveria, L.; Cuevas-Figueroa, X.M.; Reyes-Chilpa, R. Antimycobacterial and HIV-1 reverse transcriptase activity of Julianaceae and Clusiaceae plant species from Mexico. Evid. Based Complement. Altern. Med. 2015. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Narayan, L.C.; Rai, V.R.; Tewtrakul, S. Emerging need to use phytopharmaceuticals in the treatment of HIV. J. Pharm. Res. 2013, 6, 218–223. [Google Scholar] [CrossRef]
- Kuo, R.-Y.; Qian, K.; Morris-Natschke, S.L.; Lee, K.-H. Plant-derived triterpenoids and analogues as antitumor and anti-HIV agents. Nat. Prod. Rep. 2009, 26, 1321–1344. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bringmann, G.; Steinert, C.; Feineis, D.; Mudogo, V.; Betzin, J.; Scheller, C. HIV-inhibitory michellamine-type dimeric naphthylisoquinoline alkaloids from the Central African liana Ancistrocladus congolensis. Phytochemistry 2016, 128, 71–81. [Google Scholar] [CrossRef]
- Tietjen, I.; Gatonye, T.; Ngwenya, B.N.; Namushe, A.; Simonambanga, S.; Muzila, M.; Mwimanzi, P.; Xiao, J.; Fedida, D.; Brumme, Z.L. Croton megalobotrys Müll Arg. and Vitex doniana (Sweet): Traditional medicinal plants in a three-step treatment regimen that inhibit in vitro replication of HIV-1. J. Ethnopharmacol. 2016, 191, 331–340. [Google Scholar] [CrossRef] [PubMed]
- Sanna, C.; Rigano, D.; Corona, A.; Piano, D.; Formisano, C.; Farci, D.; Franzini, G.; Ballero, M.; Chianese, G.; Tramontano, E. Dual HIV-1 reverse transcriptase and integrase inhibitors from Limonium morisianum Arrigoni, an endemic species of Sardinia (Italy). Nat. Prod. Res. 2019, 33, 1798–1803. [Google Scholar] [CrossRef]
- Hisayoshi, T.; Shinomura, M.; Yokokawa, K.; Kuze, I.; Konishi, A.; Kawaji, K.; Kodama, E.N.; Hata, K.; Takahashi, S.; Nirasawa, S. Inhibition of the DNA polymerase and RNase H activities of HIV-1 reverse transcriptase and HIV-1 replication by Brasenia schreberi (Junsai) and Petasites japonicus (Fuki) components. J. Nat. Med. 2015, 69, 432–440. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.; Ding, Z.-H.; Liu, J.-K.; Zheng, Y.-T. Xanthohumol, a novel anti-HIV-1 agent purified from Hops Humulus lupulus. Antivir. Res. 2004, 64, 189–194. [Google Scholar] [CrossRef]
- Zhang, H.; Ma, Z.F. Phytochemical and pharmacological properties of Capparis spinosa as a medicinal plant. Nutrients 2018, 10, 116. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Singh, I.P.; Bharate, S.B.; Bhutani, K. Anti-HIV natural products. Curr. Sci. 2005, 89, 269–290. [Google Scholar]
- Pailee, P.; Kuhakarn, C.; Sangsuwan, C.; Hongthong, S.; Piyachaturawat, P.; Suksen, K.; Jariyawat, S.; Akkarawongsapat, R.; Limthongkul, J.; Napaswad, C. Anti-HIV and cytotoxic biphenyls, benzophenones and xanthones from stems, leaves and twigs of Garcinia speciosa. Phytochemistry 2018, 147, 68–79. [Google Scholar] [CrossRef] [PubMed]
- Chaturonrutsamee, S.; Kuhakarn, C.; Surawatanawong, P.; Prabpai, S.; Kongsaeree, P.; Jaipetch, T.; Piyachaturawat, P.; Jariyawat, S.; Akkarawongsapat, R.; Suksen, K. Polycyclic polyprenylated acylphloroglucinols and biphenyl derivatives from the roots of Garcinia nuntasaenii Ngerns. & Suddee. Phytochemistry 2018, 146, 63–74. [Google Scholar] [PubMed]
- Palamthodi, S.; Lele, S. Nutraceutical applications of gourd family vegetables: Benincasa hispida, Lagenaria siceraria and Momordica charantia. Biomed. Prev. Nutr. 2014, 4, 15–21. [Google Scholar] [CrossRef]
- Bekut, M.; Brkić, S.; Kladar, N.; Dragović, G.; Gavarić, N.; Božin, B. Potential of selected Lamiaceae plants in anti (retro) viral therapy. Pharmacol. Res. 2018, 133, 301–314. [Google Scholar] [CrossRef]
- Zhao, Q.; Chen, X.-Y.; Martin, C. Scutellaria baicalensis, the golden herb from the garden of Chinese medicinal plants. Sci. Bull. 2016, 61, 1391–1398. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Looker, K.J.; Welton, N.J.; Sabin, K.M.; Dalal, S.; Vickerman, P.; Turner, K.M.; Boily, M.-C.; Gottlieb, S.L. Global and regional estimates of the contribution of herpes simplex virus type 2 infection to HIV incidence: A population attributable fraction analysis using published epidemiological data. Lancet Infect. Dis. 2020, 20, 240–249. [Google Scholar] [CrossRef] [Green Version]
- Whitley, R.J.; Roizman, B. Herpes simplex virus infections. The lancet 2001, 357, 1513–1518. [Google Scholar] [CrossRef]
- Forni, D.; Pontremoli, C.; Clerici, M.; Pozzoli, U.; Cagliani, R.; Sironi, M. Recent out-of-Africa migration of human herpes simplex viruses. Mol. Biol. Evol. 2020, 37, 1259–1271. [Google Scholar] [CrossRef] [PubMed]
- Dropulic, L.K.; Cohen, J.I. Update on new antivirals under development for the treatment of double-stranded DNA virus infections. Clin. Pharmacol. Ther. 2010, 88, 610–619. [Google Scholar] [CrossRef] [Green Version]
- van den Pol, A.N.; Ozduman, K.; Wollmann, G.; Ho, W.S.; Simon, I.; Yao, Y.; Rose, J.K.; Ghosh, P. Viral strategies for studying the brain, including a replication-restricted self-amplifying delta-G vesicular stomatis virus that rapidly expresses transgenes in brain and can generate a multicolor Golgi-like expression. J. Comp. Neurol. 2009, 516, 456–481. [Google Scholar] [CrossRef] [Green Version]
- Chuanasa, T.; Phromjai, J.; Lipipun, V.; Likhitwitayawuid, K.; Suzuki, M.; Pramyothin, P.; Hattori, M.; Shiraki, K. Anti-herpes simplex virus (HSV-1) activity of oxyresveratrol derived from Thai medicinal plant: Mechanism of action and therapeutic efficacy on cutaneous HSV-1 infection in mice. Antivir. Res. 2008, 80, 62–70. [Google Scholar] [CrossRef] [PubMed]
- Neyts, J.; De Clercq, E. Mechanism of action of acyclic nucleoside phosphonates against herpes virus replication. Biochem. Pharmacol. 1994, 47, 39–41. [Google Scholar] [CrossRef]
- Hassan, S.T.; Masarčíková, R.; Berchová, K. Bioactive natural products with anti-herpes simplex virus properties. J. Pharm. Pharmacol. 2015, 67, 1325–1336. [Google Scholar] [CrossRef] [PubMed]
- Brady, R.C.; Bernstein, D.I. Treatment of herpes simplex virus infections. Antivir. Res. 2004, 61, 73–81. [Google Scholar] [CrossRef]
- Corey, L. Challenges in genital herpes simplex virus management. J. Infect. Dis. 2002, 186 (Suppl. 1), S29–S33. [Google Scholar] [CrossRef]
- Benzekri, R.; Limam, F.; Bouslama, L. Combination effect of three anti-HSV-2 active plant extracts exhibiting different modes of action. Adv. Tradit. Med. 2020, 20, 223–231. [Google Scholar] [CrossRef]
- Musarra-Pizzo, M.; Pennisi, R.; Ben-Amor, I.; Smeriglio, A.; Mandalari, G.; Sciortino, M.T. In Vitro Anti-HSV-1 Activity of Polyphenol-Rich Extracts and Pure Polyphenol Compounds Derived from Pistachios Kernels (Pistacia vera L.). Plants 2020, 9, 267. [Google Scholar] [CrossRef] [Green Version]
- Reichling, J.; Neuner, A.; Sharaf, M.; Harkenthal, M.; Schnitzler, P. Antiviral activity of Rhus aromatica (fragrant sumac) extract against two types of herpes simplex viruses in cell culture. Die Pharm. Int. J. Pharm. Sci. 2009, 64, 538–541. [Google Scholar]
- Karimi, A.; Rafieian-Kopaei, M.; Moradi, M.-T.; Alidadi, S. Anti–Herpes Simplex Virus Type-1 Activity and Phenolic Content of Crude Ethanol Extract and Four Corresponding Fractions of Quercus brantii L Acorn. J. Evid. Based Complement. Altern. Med. 2017, 22, 455–461. [Google Scholar] [CrossRef] [PubMed]
- Benassi-Zanqueta, É.; Marques, C.F.; Valone, L.M.; Pellegrini, B.L.; Bauermeister, A.; Ferreira, I.C.P.; Lopes, N.P.; Nakamura, C.V.; Dias Filho, B.P.; Natali, M.R.M. Evaluation of anti-HSV-1 activity and toxicity of hydroethanolic extract of Tanacetum parthenium (L.) Sch. Bip. (Asteraceae). Phytomedicine 2019, 55, 249–254. [Google Scholar] [CrossRef]
- Yoosook, C.; Bunyapraphatsara, N.; Boonyakiat, Y.; Kantasuk, C. Anti-herpes simplex virus activities of crude water extracts of Thai medicinal plants. Phytomedicine 2000, 6, 411–419. [Google Scholar] [CrossRef]
- Shamsabadipour, S.; Ghanadian, M.; Saeedi, H.; Rahimnejad, M.R.; Mohammadi-Kamalabadi, M.; Ayatollahi, S.M.; Salimzadeh, L. Triterpenes and steroids from Euphorbia denticulata Lam. with anti-Herpes symplex virus activity. Iran. J. Pharm. Res. IJPR 2013, 12, 759. [Google Scholar]
- Lipipun, V.; Kurokawa, M.; Suttisri, R.; Taweechotipatr, P.; Pramyothin, P.; Hattori, M.; Shiraki, K. Efficacy of Thai medicinal plant extracts against herpes simplex virus type 1 infection in vitro and in vivo. Antivir. Res. 2003, 60, 175–180. [Google Scholar] [CrossRef]
- El-Toumy, S.A.; Salib, J.Y.; El-Kashak, W.A.; Marty, C.; Bedoux, G.; Bourgougnon, N. Antiviral effect of polyphenol rich plant extracts on herpes simplex virus type 1. Food Sci. Hum. Wellness 2018, 7, 91–101. [Google Scholar] [CrossRef]
- Palomino, S.S.; Abad, M.J.; Bedoya, L.M.; García, J.; Gonzales, E.; Chiriboga, X.; Bermejo, P.; Alcami, J. Screening of South American plants against human immunodeficiency virus: Preliminary fractionation of aqueous extract from Baccharis trinervis. Biol. Pharm. Bull. 2002, 25, 1147–1150. [Google Scholar] [CrossRef] [Green Version]
- Rezazadeh, F.; Moshaverinia, M.; Motamedifar, M.; Alyaseri, M. Assessment of anti HSV-1 activity of Aloe vera gel extract: An in vitro study. J. Dent. 2016, 17, 49. [Google Scholar]
- Padma, P.; Pramod, N.; Thyagarajan, S.; Khosa, R. Effect of the extract of Annona muricata and Petunia nyctaginiflora on Herpes simplex virus. J. Ethnopharmacol. 1998, 61, 81–83. [Google Scholar] [CrossRef]
- Andrighetti-Fröhner, C.; Sincero, T.; Da Silva, A.; Savi, L.; Gaido, C.; Bettega, J.; Mancini, M.; De Almeida, M.; Barbosa, R.; Farias, M. Antiviral evaluation of plants from Brazilian atlantic tropical forest. Fitoterapia 2005, 76, 374–378. [Google Scholar] [CrossRef]
- Zaharieva, M.M.; Genova-Kalou, P.; Dincheva, I.; Badjakov, I.; Krumova, S.; Enchev, V.; Najdenski, H.; Markova, N. Anti-Herpes Simplex virus and antibacterial activities of Graptopetalum paraguayense E. Walther leaf extract: A pilot study. Biotechnol. Biotechnol. Equip. 2019, 33, 1251–1259. [Google Scholar] [CrossRef] [Green Version]
- Bisignano, C.; Mandalari, G.; Smeriglio, A.; Trombetta, D.; Pizzo, M.M.; Pennisi, R.; Sciortino, M.T. Almond skin extracts abrogate HSV-1 replication by blocking virus binding to the cell. Viruses 2017, 9, 178. [Google Scholar] [CrossRef]
- Churqui, M.P.; Lind, L.; Thörn, K.; Svensson, A.; Savolainen, O.; Aranda, K.T.; Eriksson, K. Extracts of Equisetum giganteum L and Copaifera reticulate Ducke show strong antiviral activity against the sexually transmitted pathogen herpes simplex virus type 2. J. Ethnopharmacol. 2018, 210, 192–197. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nocchi, S.R.; Companhoni, M.V.P.; de Mello, J.C.P.; Dias Filho, B.P.; Nakamura, C.V.; Carollo, C.A.; Silva, D.B.; Ueda-Nakamura, T. Antiviral activity of crude hydroethanolic extract from Schinus terebinthifolia against Herpes simplex Virus Type 1. Planta Med. 2017, 234, 509–518. [Google Scholar] [CrossRef] [Green Version]
- Hinkov, A.; Angelova, P.; Marchev, A.; Hodzhev, Y.; Tsvetkov, V.; Dragolova, D.; Todorov, D.; Shishkova, K.; Kapchina-Toteva, V.; Blundell, R. Nepeta nuda ssp. nuda L. water extract: Inhibition of replication of some strains of human alpha herpes virus (genus simplex virus) in vitro, mode of action and NMR-based metabolomics. J. Herb. Med. 2020, 21, 100334. [Google Scholar] [CrossRef]
- Lavoie, S.; Côté, I.; Pichette, A.; Gauthier, C.; Ouellet, M.; Nagau-Lavoie, F.; Mshvildadze, V.; Legault, J. Chemical composition and anti-herpes simplex virus type 1 (HSV-1) activity of extracts from Cornus canadensis. BMC Complement. Altern. Med. 2017, 17, 123. [Google Scholar] [CrossRef]
- Boff, L.; Silva, I.; Argenta, D.; Farias, L.; Alvarenga, L.; Pádua, R.; Braga, F.; Leite, J.; Kratz, J.; Simões, C. Strychnos pseudoquina A. St. Hil.: A Brazilian medicinal plant with promising in vitro antiherpes activity. J. Appl. Microbiol. 2016, 121, 1519–1529. [Google Scholar] [CrossRef]
- Siqueira, E.M.d.S.; Lima, T.L.; Boff, L.; Lima, S.G.; Lourenço, E.M.; Ferreira, É.G.; Barbosa, E.G.; Machado, P.R.; Farias, K.J.; Ferreira, L.D.S. Antiviral Potential of Spondias mombin L. Leaves Extract Against Herpes Simplex Virus Type-1 Replication Using In Vitro and In Silico Approaches. Planta Med. 2020, 86, 505–515. [Google Scholar] [CrossRef]
- Di Sotto, A.; Di Giacomo, S.; Amatore, D.; Locatelli, M.; Vitalone, A.; Toniolo, C.; Rotino, G.L.; Lo Scalzo, R.; Palamara, A.T.; Marcocci, M.E. A polyphenol rich extract from Solanum melongena L. DR2 peel exhibits antioxidant properties and anti-Herpes Simplex Virus Type 1 activity in vitro. Molecules 2018, 23, 2066. [Google Scholar] [CrossRef] [Green Version]
- Wang, Y.-Q.; Cai, L.; Zhang, N.; Zhang, J.; Wang, H.-H.; Zhu, W. Protective effect of total flavonoids from Ixeris Sonchifolia on herpes simplex virus keratitis in mice. BMC Complement. Med. Ther. 2020, 20, 1–8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nawawi, A.A.; Nakamura, N.; Hattori, M.; Kurokawa, M.; Shiraki, K. Inhibitory effects of Indonesian medicinal plants on the infection of herpes simplex virus type 1. Phytother. Res. Int. J. Devoted Pharmacol. Toxicol. Eval. Nat. Prod. Deriv. 1999, 13, 37–41. [Google Scholar] [CrossRef]
- Benzekri, R.; Bouslama, L.; Papetti, A.; Hammami, M.; Smaoui, A.; Limam, F. Anti HSV-2 activity of Peganum harmala (L.) and isolation of the active compound. Microb. Pathog. 2018, 114, 291–298. [Google Scholar] [CrossRef] [PubMed]
- Ben Sassi, A.; Harzallah-Skhiri, F.; Bourgougnon, N.; Aouni, M. Antiviral activity of some Tunisian medicinal plants against Herpes simplex virus type 1. Nat. Prod. Res. 2008, 22, 53–65. [Google Scholar] [CrossRef]
- Gavanji, S.; Sayedipour, S.S.; Larki, B.; Bakhtari, A. Antiviral activity of some plant oils against herpes simplex virus type 1 in Vero cell culture. J. Acute Med. 2015, 5, 62–68. [Google Scholar] [CrossRef] [Green Version]
- Donalisio, M.; Cagno, V.; Civra, A.; Gibellini, D.; Musumeci, G.; Rittà, M.; Ghosh, M.; Lembo, D. The traditional use of Vachellia nilotica for sexually transmitted diseases is substantiated by the antiviral activity of its bark extract against sexually transmitted viruses. J. Ethnopharmacol. 2018, 213, 403–408. [Google Scholar] [CrossRef]
- Nakamura, N.; Hattori, M.; Kurokawa, M.; Shiraki, K.; Kashiwaba, N.; Ono, M. Anti-herpes simplex virus activity of alkaloids isolated from Stephania cepharantha. Biol. Pharm. Bull. 1999, 22, 268–274. [Google Scholar]
- Ghosh, M.; Civra, A.; Rittà, M.; Cagno, V.; Mavuduru, S.G.; Awasthi, P.; Lembo, D.; Donalisio, M. Ficus religiosa L. bark extracts inhibit infection by herpes simplex virus type 2 in vitro. Arch. Virol. 2016, 161, 3509–3514. [Google Scholar] [CrossRef]
- Verma, H.; Patil, P.; Kolhapure, R.; Gopalkrishna, V. Antiviral activity of the Indian medicinal plant extract, Swertia chirata against herpes simplex viruses: A study by in-vitro and molecular approach. Indian J. Med Microbiol. 2008, 26, 322. [Google Scholar]
- Hayashi, K.; Niwayama, S.; Hayashi, T.; Nago, R.; Ochiai, H.; Morita, N. In vitro and in vivo antiviral activity of scopadulcic acid B from Scoparia dulcis, Scrophulariaceae, against herpes simplex virus type 1. Antivir. Res. 1988, 9, 345–354. [Google Scholar] [CrossRef]
- Ojha, D.; Das, R.; Sobia, P.; Dwivedi, V.; Ghosh, S.; Samanta, A.; Chattopadhyay, D. Pedilanthus tithymaloides inhibits HSV infection by modulating NF-κB signaling. PLoS ONE 2015, 10, e0139338. [Google Scholar] [CrossRef] [PubMed]
- Wiart, C.; Kumar, K.; Yusof, M.; Hamimah, H.; Fauzi, Z.; Sulaiman, M. Antiviral properties of ent-labdene diterpenes of Andrographis paniculata Nees, inhibitors of herpes simplex virus type 1. Phytother. Res. Int. J. Devoted Pharmacol. Toxicol. Eval. Nat. Prod. Deriv. 2005, 19, 1069–1070. [Google Scholar]
- Hafidh, R.R.; Abdulamir, A.S.; Bakar, F.A.; Sekawi, Z.; Jahansheri, F.; Jalilian, F.A. Novel antiviral activity of mung bean sprouts against respiratory syncytial virus and herpes simplex virus−1: An in vitro study on virally infected Vero and MRC-5 cell lines. BMC Complement. Altern. Med. 2015, 15, 179. [Google Scholar] [CrossRef] [Green Version]
- Karimi, A.; Moradi, M.-T.; Saeedi, M.; Asgari, S.; Rafieian-Kopaei, M. Antiviral activity of Quercus persica L.: High efficacy and low toxicity. Adv. Biomed. Res. 2013, 2, 36. [Google Scholar]
- Elanchezhiyan, M.; Rajarajan, S.; Rajendran, P.; Subramanian, S.; Thyagarajan, S. Antiviral properties of the seed extract of an Indian medicinal plant, Pongamia pinnata, Linn., against herpes simplex viruses: In-vitro studies on Vero cells. J. Med. Microbiol. 1993, 38, 262–264. [Google Scholar] [CrossRef] [Green Version]
- Cheng, H.-Y.; Lin, T.-C.; Yang, C.-M.; Wang, K.-C.; Lin, C.-C. Mechanism of action of the suppression of herpes simplex virus type 2 replication by pterocarnin A. Microbes Infect. 2004, 6, 738–744. [Google Scholar] [CrossRef]
- Namazi, R.; Zabihollahi, R.; Behbahani, M.; Rezaei, A. Inhibitory activity of Avicennia marina, a medicinal plant in Persian folk medicine, against HIV and HSV. Iran. J. Pharm. Res. IJPR 2013, 12, 435. [Google Scholar]
- Jadhav, P.; Kapoor, N.; Thomas, B.; Lal, H.; Kshirsagar, N. Antiviral potential of selected Indian medicinal (ayurvedic) plants against herpes simplex virus 1 and 2. N. Am. J. Med Sci. 2012, 4, 641. [Google Scholar] [CrossRef]
- Jaime, M.F.V.; Redko, F.; Muschietti, L.V.; Campos, R.H.; Martino, V.S.; Cavallaro, L.V. In vitro antiviral activity of plant extracts from Asteraceae medicinal plants. Virol. J. 2013, 10, 245. [Google Scholar] [CrossRef] [Green Version]
- Lin, L.-C.; Kuo, Y.-C.; Chou, C.-J. Anti-herpes simplex virus type-1 flavonoids and a new flavanone from the root of Limonium sinense. Planta Med. 2000, 66, 333–336. [Google Scholar] [CrossRef]
- Zhang, Y.; But, P.P.-H.; Ooi, V.E.-C.; Xu, H.-X.; Delaney, G.D.; Lee, S.H.; Lee, S.F. Chemical properties, mode of action, and in vivo anti-herpes activities of a lignin—carbohydrate complex from Prunella vulgaris. Antivir. Res. 2007, 75, 242–249. [Google Scholar] [CrossRef] [PubMed]
- Konigheim, B.S.; Beranek, M.; Comini, L.R.; Aguilar, J.J.; Marioni, J.; Cabrera, J.L.; Contigiani, M.S.; Montoya, S.C.N. In Vitro antiviral activity of Heterophyllaea pustulata extracts. Nat. Prod. Commun. 2012, 7, 1025–1028. [Google Scholar] [CrossRef] [Green Version]
- Lin, Y.-M.; Flavin, M.T.; Schure, R.; Chen, F.-C.; Sidwell, R.; Barnard, D.I.; Huffmann, J.H.; Kern, E.R. Antiviral activities of biflavonoids. Planta Med. 1999, 65, 120–125. [Google Scholar] [CrossRef] [PubMed]
- Martin, S.F. The amaryllidaceae alkaloids. In The Alkaloids: Chemistry and Pharmacology; Elsevier: Amsterdam, The Netherlands, 1987; Volume 30, pp. 251–376. [Google Scholar]
- Bourne, K.Z.; Bourne, N.; Reising, S.F.; Stanberry, L.R. Plant products as topical microbicide candidates: Assessment of in vitro and in vivo activity against herpes simplex virus type 2. Antivir. Res. 1999, 42, 219–226. [Google Scholar] [CrossRef]
- Andersen, D.O.; Weber, N.D.; Wood, S.G.; Hughes, B.G.; Murray, B.K.; North, J.A. In vitro virucidal activity of selected anthraquinones and anthraquinone derivatives. Antivir. Res. 1991, 16, 185–196. [Google Scholar] [CrossRef]
- Chokchaisiri, R.; Srijun, J.; Chaichompoo, W.; Cheenpracha, S.; Ganranoo, L.; Suksamrarn, A. Anti-herpes simplex type-1 (HSV-1) activity from the roots of Jatropha multifida L. Med. Chem. Res. 2020, 29, 328–333. [Google Scholar] [CrossRef]
- Killingley, B.; Greatorex, J.; Cauchemez, S.; Enstone, J.; Curran, M.; Read, R.; Lim, W.; Hayward, A.; Nicholson, K.; Nguyen-Van-Tam, J. Virus shedding and environmental deposition of novel A (H1N1) pandemic influenza virus: Interim findings. Health Technol Assess 2010, 14, 237–354. [Google Scholar] [CrossRef] [Green Version]
- Simonsen, L.; Clarke, M.J.; Schonberger, L.B.; Arden, N.H.; Cox, N.J.; Fukuda, K. Pandemic versus epidemic influenza mortality: A pattern of changing age distribution. J. Infect. Dis. 1998, 178, 53–60. [Google Scholar] [CrossRef]
- Jester, B.J.; Uyeki, T.M.; Jernigan, D.B. Fifty Years of Influenza A (H3N2) Following the Pandemic of 1968. Am. J. Public Health 2020, 110, 669–676. [Google Scholar] [CrossRef]
- Xue, L.; Zeng, G. An Evaluation of China’s Influenza A (H1N1) Emergency Response Measures. In A Comprehensive Evaluation on Emergency Response in China; Springer: Singapore, 2019; pp. 107–158. [Google Scholar]
- Dixit, R. Influenza in Vulnerable Populations. PhD Thesis, Faculty of Medicine, Sydney University, Sydney, Australia, 2018. [Google Scholar]
- Chow, A.; Ma, S.; Ling, A.E.; Chew, S.K. Influenza-associated deaths in tropical Singapore. Emerg. Infect. Dis. 2006, 12, 114. [Google Scholar] [CrossRef]
- Taubenberger, J.K.; Kash, J.C. Influenza virus evolution, host adaptation, and pandemic formation. Cell Host Microbe 2010, 7, 440–451. [Google Scholar] [CrossRef] [Green Version]
- Chandler, J.D.; Hu, X.; Ko, E.-J.; Park, S.; Fernandes, J.; Lee, Y.-T.; Orr, M.L.; Hao, L.; Smith, M.R.; Neujahr, D.C. Low-dose cadmium potentiates lung inflammatory response to 2009 pandemic H1N1 influenza virus in mice. Environ. Int. 2019, 127, 720–729. [Google Scholar] [CrossRef]
- Su, S.; Gu, M.; Liu, D.; Cui, J.; Gao, G.F.; Zhou, J.; Liu, X. Epidemiology, evolution, and pathogenesis of H7N9 influenza viruses in five epidemic waves since 2013 in China. Trends Microbiol. 2017, 25, 713–728. [Google Scholar] [CrossRef]
- Nachbagauer, R.; Krammer, F. Universal influenza virus vaccines and therapeutic antibodies. Clin. Microbiol. Infect. 2017, 23, 222–228. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, T.; Yin, C.; Boyd, D.F.; Quarato, G.; Ingram, J.P.; Shubina, M.; Ragan, K.B.; Ishizuka, T.; Crawford, J.C.; Tummers, B. Influenza virus Z-RNAs induce ZBP1-mediated necroptosis. Cell 2020, 180, 1115–1129. [Google Scholar] [CrossRef]
- Jang, Y.; Jin, M.; Seo, S.H. Histamine contributes to severe pneumonia in pigs infected with 2009 pandemic H1N1 influenza virus. Arch. Virol. 2018, 163, 3015–3022. [Google Scholar] [CrossRef] [PubMed]
- Ng, S.; Nachbagauer, R.; Balmaseda, A.; Stadlbauer, D.; Ojeda, S.; Patel, M.; Rajabhathor, A.; Lopez, R.; Guglia, A.F.; Sanchez, N. Novel correlates of protection against pandemic H1N1 influenza A virus infection. Nat. Med. 2019, 25, 962–967. [Google Scholar] [CrossRef] [PubMed]
- Lau, H.; Deng, Y.-M.; Xu, X.; Sessions, W.; Barr, I.G. Rapid detection of new B/Victoria-lineage haemagglutinin variants of influenza B viruses by pyrosequencing. Diagn. Microbiol. Infect. Dis. 2019, 93, 311–317. [Google Scholar] [CrossRef]
- Chan, W.M.; Wong, L.H.; So, C.F.; Chen, L.L.; Wu, W.L.; Ip, J.D.; Lam, A.H.Y.; Yip, C.C.; Yuen, K.Y.; To, K.K. Development and evaluation of a conventional RT-PCR for differentiating emerging influenza B/Victoria lineage viruses with hemagglutinin amino acid deletion from B/Yamagata lineage viruses. J. Med Virol. 2019, 92, 382–385. [Google Scholar] [CrossRef]
- DiPiazza, A.; Nogales, A.; Poulton, N.; Wilson, P.C.; Martínez-Sobrido, L.; Sant, A.J. Pandemic 2009 H1N1 Influenza Venus reporter virus reveals broad diversity of MHC class II-positive antigen-bearing cells following infection in vivo. Sci. Rep. 2017, 7, 10857. [Google Scholar] [CrossRef]
- Reina, J.; Reina, N. Universal influenza vaccination: Future prospects. Vacunas (Engl. Ed.) 2019, 20, 72–81. [Google Scholar] [CrossRef]
- Rafiq, D.; Batool, A.; Bazaz, M. Three months of COVID-19: A systematic review and meta-analysis. Rev. Med. Virol. 2020, 30, e2113. [Google Scholar] [CrossRef] [PubMed]
- Glathe, H.; Hilgenfeld, M.; Lebhardt, A.; Strittmatter, H.; Schulze, P.; Brandt, B. The intestine of ferret—A possible site of influenza virus replication. Acta Virol. 1984, 28, 287. [Google Scholar]
- Neumann, G.; Brownlee, G.; Fodor, E.; Kawaoka, Y. Orthomyxovirus replication, transcription, and polyadenylation. In Biology of Negative Strand RNA Viruses: The Power of Reverse Genetics; Springer: Heidelberg, Germany, 2004; pp. 121–143. [Google Scholar]
- Portela, A.; Zürcher, T.; Nieto, A.; Ortín, J. Replication of orthomyxoviruses. In Advances in Virus Research; Elsevier: Amsteerdam, The Netherlands, 1999; Volume 54, pp. 319–348. [Google Scholar]
- Long, C. Challenging contingency: Viruses and the nature of molecular life. Secur. Dialogue 2019, 51, 323–339. [Google Scholar] [CrossRef]
- Xue, L.; Zeng, G. Global Strategies and Response Measures to the Influenza A (H1N1) Pandemic. In A Comprehensive Evaluation on Emergency Response in China; Springer: Singapore, 2019; pp. 15–44. [Google Scholar]
- Kannan, S.; Kolandaivel, P. Antiviral potential of natural compounds against influenza virus hemagglutinin. Comput. Biol. Chem. 2017, 71, 207–218. [Google Scholar] [CrossRef]
- Tochino, Y.; Fujioka, M.; Sakazaki, H.; Ikuno, Y.; Tochino, R.; Yoshii, N.; Shintaku, H.; Hirata, K. Current usage and effectiveness of influenza medications and factors regarding the time taken to alleviate fever based on postcard questionnaire survey. J. Gen. Fam. Med. 2017, 18, 386–392. [Google Scholar] [CrossRef] [PubMed]
- Paul, D.; Bartenschlager, R. Architecture and biogenesis of plus-strand RNA virus replication factories. World J. Virol. 2013, 2, 32. [Google Scholar] [CrossRef]
- Ludwig, S.; Planz, O.; Pleschka, S.; Wolff, T. Influenza-virus-induced signaling cascades: Targets for antiviral therapy? Trends Mol. Med. 2003, 9, 46–52. [Google Scholar] [CrossRef]
- Garman, E.; Laver, G. Controlling influenza by inhibiting the virus’s neuraminidase. Curr. Drug Targets 2004, 5, 119–136. [Google Scholar] [CrossRef]
- Müller, B.; Kräusslich, H.-G. Antiviral strategies. In Antiviral Strategies; Springer: Singapore, 2009; pp. 1–24. [Google Scholar]
- Weiss, G.; Schaible, U.E. Macrophage defense mechanisms against intracellular bacteria. Immunol. Rev. 2015, 264, 182–203. [Google Scholar] [CrossRef] [Green Version]
- Wang, X.; Jia, W.; Zhao, A.; Wang, X. Anti-influenza agents from plants and traditional Chinese medicine. Phytother. Res. 2006, 20, 335–341. [Google Scholar] [CrossRef] [PubMed]
- Droebner, K.; Ehrhardt, C.; Poetter, A.; Ludwig, S.; Planz, O. CYSTUS052, a polyphenol-rich plant extract, exerts anti-influenza virus activity in mice. Antivir. Res. 2007, 76, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Ji Na, W.; Seo Yong, L.; Dae Sub, S.; Har Young, P. Antiviral Activity of the Plant Extracts from Thuja orientalis, Aster spathulifolius, and Pinus thunbergii Against Influenza Virus A/PR/8/34. J. Microbiol. Biotechnol. 2013, 23, 125–130. [Google Scholar]
- GabAllah, M.; Kandeil, A.; Mousa, A.E.-B.; Ahmed Ali, M. Antiviral activity of water extracts of some medicinal and nutritive plants from the Apiaceae family. Nov. Res. Microbiol. J. 2020, 4, 725–735. [Google Scholar] [CrossRef]
- Ombito, J.O.; Salano, E.N.; Yegon, P.K.; Ngetich, W.K.; Mwangi, E.M.; Koe, G. A review of the chemistry of some species of genus Aloe (Xanthorrhoeaceae family). J. Sci. Innov. Res. 2015, 4, 49–53. [Google Scholar]
- Moradi, M.-T.; Karimi, A.; Shahrani, M.; Hashemi, L.; Ghaffari-Goosheh, M.-S. Anti-Influenza Virus Activity and Phenolic Content of Pomegranate (Punica granatum L.) Peel Extract and Fractions. Avicenna J. Med. Biotechnol. 2019, 11, 285–291. [Google Scholar]
- Choi, J.-G.; Kim, Y.S.; Kim, J.H.; Chung, H.-S. Antiviral activity of ethanol extract of Geranii Herba and its components against influenza viruses via neuraminidase inhibition. Sci. Rep. 2019, 9, 12132. [Google Scholar] [CrossRef]
- Rajasekaran, D.; Palombo, E.A.; Chia Yeo, T.; Lim Siok Ley, D.; Lee Tu, C.; Malherbe, F.; Grollo, L. Identification of traditional medicinal plant extracts with novel anti-influenza activity. PLoS ONE 2013, 8, e79293. [Google Scholar] [CrossRef] [Green Version]
- Tran, T.T.; Kim, M.; Jang, Y.; Lee, H.W.; Nguyen, H.T.; Nguyen, T.N.; Park, H.W.; Le Dang, Q.; Kim, J.-C. Characterization and mechanisms of anti-influenza virus metabolites isolated from the Vietnamese medicinal plant Polygonum chinense. BMC Complement. Altern. Med. 2017, 17, 162. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shi, Y.; Zhang, B.; Lu, Y.; Qian, C.; Feng, Y.; Fang, L.; Ding, Z.; Cheng, D. Antiviral activity of phenanthrenes from the medicinal plant Bletilla striata against influenza A virus. BMC Complement. Altern. Med. 2017, 17, 273. [Google Scholar] [CrossRef]
- Shoji, M.; Woo, S.-Y.; Masuda, A.; Win, N.N.; Ngwe, H.; Takahashi, E.; Kido, H.; Morita, H.; Ito, T.; Kuzuhara, T. Anti-influenza virus activity of extracts from the stems of Jatropha multifida Linn. collected in Myanmar. BMC Complement. Altern. Med. 2017, 17, 96. [Google Scholar] [CrossRef] [Green Version]
- He, W.; Han, H.; Wang, W.; Gao, B. Anti-influenza virus effect of aqueous extracts from dandelion. Virol. J. 2011, 8, 538. [Google Scholar] [CrossRef] [Green Version]
- Zhang, T.; Lo, C.-Y.; Xiao, M.; Cheng, L.; Pun Mok, C.K.; Shaw, P.-C. Anti-influenza virus phytochemicals from Radix Paeoniae Alba and characterization of their neuraminidase inhibitory activities. J. Ethnopharmacol. 2020, 253, 112671. [Google Scholar] [CrossRef] [PubMed]
- Mohamed, M.S.; Idriss, M.T.; Alruwaili, N.K.; Alotaibi, N.H.; Elsaman, T.; Mohamed, M.A. Investigation of the potential anti-influenza activity of five plants grown in Sudan and used folklorically for respiratory infections. J. Appl. Pharm. Sci. 2020, 10, 054–061. [Google Scholar]
- Moradi, M.-T.; Karimi, A.; Rafieian-Kopaei, M.; Rabiei-Faradonbeh, M.; Momtaz, H. Pomegranate peel extract inhibits internalization and replication of the influenza virus: An in vitro study. Avicenna J. Phytomed. 2020, 10, 143–151. [Google Scholar]
- Zhang, L.; Chen, J.; Ke, C.; Zhang, H.; Zhang, S.; Tang, W.; Liu, C.; Liu, G.; Chen, S.; Hu, A.; et al. Ethanol Extract of Caesalpinia decapetala Inhibits Influenza Virus Infection In Vitro and In Vivo. Viruses 2020, 12, 557. [Google Scholar] [CrossRef]
- Brown, E. Influenza virus genetics. Biomed. Pharm. 2000, 54, 196–209. [Google Scholar] [CrossRef]
- Ghildiyal, R.; Prakash, V.; Chaudhary, V.; Gupta, V.; Gabrani, R. Phytochemicals as Antiviral Agents: Recent Updates. In Plant-Derived Bioactives; Springer: Singapore, 2020; pp. 279–295. [Google Scholar]
- Moradi, M.-T.; Karimi, A.; Lorigooini, Z. Alkaloids as the natural anti-influenza virus agents: A systematic review. Toxin Rev. 2018, 37, 11–18. [Google Scholar] [CrossRef]
- Hazra, S.; Chattopadhyay, S. An overview of lignans with special reference to podophyllotoxin, a cytotoxic lignan. Chem. Biol. Lett. 2016, 3, 1–8. [Google Scholar]
- Kazakova, O.; Smirnova, I.; Baltina, L.; Boreko, E.; Savinova, O.; Pokrovskii, A. Antiviral activity of acyl derivatives of betulin and betulinic and dihydroquinopimaric acids. Russ. J. Bioorganic Chem. 2018, 44, 740–744. [Google Scholar] [CrossRef]
- Liu, G.; Xiong, S.; Xiang, Y.-F.; Guo, C.-W.; Ge, F.; Yang, C.-R.; Zhang, Y.-J.; Wang, Y.-F.; Kitazato, K. Antiviral activity and possible mechanisms of action of pentagalloylglucose (PGG) against influenza A virus. Arch Virol. 2011, 156, 1359–1369. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wu, W.; Li, R.; Li, X.; He, J.; Jiang, S.; Liu, S.; Yang, J. Quercetin as an antiviral agent inhibits influenza A virus (IAV) entry. Viruses 2016, 8, 6. [Google Scholar] [CrossRef]
- Sithisarn, P.; Michaelis, M.; Schubert-Zsilavecz, M.; Cinatl Jr, J. Differential antiviral and anti-inflammatory mechanisms of the flavonoids biochanin A and baicalein in H5N1 influenza A virus-infected cells. Antivir. Res. 2013, 97, 41–48. [Google Scholar] [CrossRef]
- Bang, S.; Ha, T.K.Q.; Lee, C.; Li, W.; Oh, W.-K.; Shim, S.H. Antiviral activities of compounds from aerial parts of Salvia plebeia R. Br. J. Ethnopharmacol. 2016, 192, 398–405. [Google Scholar] [CrossRef] [PubMed]
- Zhang, G.; Zhang, B.; Zhang, X.; Bing, F. Homonojirimycin, an alkaloid from dayflower inhibits the growth of influenza A virus in vitro. Acta Virol. 2013, 57, 85–86. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, R.; Liu, T.; Liu, M.; Chen, F.; Liu, S.; Yang, J. Anti-influenza A virus activity of dendrobine and its mechanism of action. J. Agric. Food Chem. 2017, 65, 3665–3674. [Google Scholar] [CrossRef]
- Soriano, V.; Vispo, E.; Poveda, E.; Labarga, P.; Martin-Carbonero, L.; Fernandez-Montero, J.V.; Barreiro, P. Directly acting antivirals against hepatitis C virus. J. Antimicrob. Chemother. 2011, 66, 1673–1686. [Google Scholar] [CrossRef] [Green Version]
- Smyth, B.; O’Connor, J.; Barry, J.; Keenan, E. Retrospective cohort study examining incidence of HIV and hepatitis C infection among injecting drug users in Dublin. J. Epidemiol. Community Health 2003, 57, 310–311. [Google Scholar] [CrossRef] [Green Version]
- Kurniawan, J. Pangenotypic Direct Acting Antivirals Treatment for Chronic Hepatitis C Infection. Indones. J. Gastroenterol. Hepatol. Dig. Endosc. 2020, 21, 1–2. [Google Scholar] [CrossRef]
- Pietri, O.; Trottier-Tellier, F.; Bourlière, M. While direct-acting antivirals are effective, are there any unique safety considerations? Clin. Dilemmas in Viral Liver Dis. 2020, 97–105. [Google Scholar]
- Agnello, V.; Ábel, G.; Elfahal, M.; Knight, G.B.; Zhang, Q.-X. Hepatitis C virus and other flaviviridae viruses enter cells via low density lipoprotein receptor. Proc. Natl. Acad. Sci. USA 1999, 96, 12766–12771. [Google Scholar] [PubMed] [Green Version]
- Lindenbach, B.D.; Rice, C.M. Unravelling hepatitis C virus replication from genome to function. Nature 2005, 436, 933–938. [Google Scholar] [CrossRef] [PubMed]
- Denaro, M.; Smeriglio, A.; Barreca, D.; De Francesco, C.; Occhiuto, C.; Milano, G.; Trombetta, D. Antiviral activity of plants and their isolated bioactive compounds: An update. Phytother. Res. 2020, 34, 742–768. [Google Scholar] [PubMed]
- Yousaf, T.; Rafique, S.; Wahid, F.; Rehman, S.; Nazir, A.; Rafique, J.; Aslam, K.; Shabir, G.; Shah, S.M. Phytochemical profiling and antiviral activity of Ajuga bracteosa, Ajuga parviflora, Berberis lycium and Citrus lemon against Hepatitis C Virus. Microb. Pathog. 2018, 118, 154–158. [Google Scholar] [CrossRef] [PubMed]
- Wahyuni, T.S.; Tumewu, L.; Permanasari, A.A.; Apriani, E.; Adianti, M.; Rahman, A.; Widyawaruyanti, A.; Lusida, M.I.; Fuad, A.; Fuchino, H. Antiviral activities of Indonesian medicinal plants in the East Java region against hepatitis C virus. Virol. J. 2013, 10, 259. [Google Scholar] [PubMed] [Green Version]
- Ravikumar, Y.; Ray, U.; Nandhitha, M.; Perween, A.; Naika, H.R.; Khanna, N.; Das, S. Inhibition of hepatitis C virus replication by herbal extract: Phyllanthus amarus as potent natural source. Virus Res. 2011, 158, 89–97. [Google Scholar]
- Hussein, G.; Miyashiro, H.; Nakamura, N.; Hattori, M.; Kakiuchi, N.; Shimotohno, K. Inhibitory effects of Sudanese medicinal plant extracts on hepatitis C virus (HCV) protease. Phytother. Res. Int. J. Devoted Pharmacol. Toxicol. Eval. Nat. Prod. Deriv. 2000, 14, 510–516. [Google Scholar] [CrossRef]
- Ratnoglik, S.L.; Aoki, C.; Sudarmono, P.; Komoto, M.; Deng, L.; Shoji, I.; Fuchino, H.; Kawahara, N.; Hotta, H. Antiviral activity of extracts from Morinda citrifolia leaves and chlorophyll catabolites, pheophorbide a and pyropheophorbide a, against hepatitis C virus. Microbiol. Immunol. 2014, 58, 188–194. [Google Scholar]
- Wagoner, J.; Negash, A.; Kane, O.J.; Martinez, L.E.; Nahmias, Y.; Bourne, N.; Owen, D.M.; Grove, J.; Brimacombe, C.; McKeating, J.A. Multiple effects of silymarin on the hepatitis C virus lifecycle. Hepatology 2010, 51, 1912–1921. [Google Scholar] [CrossRef] [Green Version]
- Hsu, W.-C.; Chang, S.-P.; Lin, L.-C.; Li, C.-L.; Richardson, C.D.; Lin, C.-C.; Lin, L.-T. Limonium sinense and gallic acid suppress hepatitis C virus infection by blocking early viral entry. Antivir. Res. 2015, 118, 139–147. [Google Scholar] [CrossRef]
- Yang, X.-Y.; Zhang, Y.-Y.; Xie, W.-R.; He, S.H.; Wu, L.-H.; He, X.-X.; Xia, H.H.-X. Herbal Medicines for Hepatitis C Virus Infection: The Exploratory Journey from Bench to Bedside Still Has a Long Way to Go. J. Explor. Res. Pharmacol. 2019, 4, 9–18. [Google Scholar] [CrossRef]
- Hung, T.-C.; Jassey, A.; Lin, C.-J.; Liu, C.-H.; Lin, C.-C.; Yen, M.-H.; Lin, L.-T. Methanolic extract of Rhizoma Coptidis inhibits the early viral entry steps of hepatitis C virus infection. Viruses 2018, 10, 669. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Javed, T.; Ashfaq, U.A.; Riaz, S.; Rehman, S.; Riazuddin, S. In-vitro antiviral activity of Solanum nigrum against Hepatitis C Virus. Virol. J. 2011, 8, 26. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bachmetov, L.; Gal-Tanamy, M.; Shapira, A.; Vorobeychik, M.; Giterman-Galam, T.; Sathiyamoorthy, P.; Golan-Goldhirsh, A.; Benhar, I.; Tur-Kaspa, R.; Zemel, R. Suppression of hepatitis C virus by the flavonoid quercetin is mediated by inhibition of NS3 protease activity. J. Viral Hepat. 2012, 19, e81–e88. [Google Scholar] [CrossRef]
- Lin, C.-W.; Lo, C.-W.; Tsai, C.-N.; Pan, T.-C.; Chen, P.-Y.; Yu, M.-J. Aeginetia indica decoction inhibits hepatitis C virus life cycle. Int. J. Mol. Sci. 2018, 19, 208. [Google Scholar] [CrossRef] [Green Version]
- Zuo, G.; Li, Z.; Chen, L.; Xu, X. Activity of compounds from Chinese herbal medicine Rhodiola kirilowii (Regel) Maxim against HCV NS3 serine protease. Antivir. Res. 2007, 76, 86–92. [Google Scholar] [CrossRef]
- Qian, X.-J.; Zhang, X.-L.; Zhao, P.; Jin, Y.-S.; Chen, H.-S.; Xu, Q.-Q.; Ren, H.; Zhu, S.-Y.; Tang, H.-L.; Zhu, Y.-Z. A Schisandra-derived compound schizandronic acid inhibits entry of Pan-HCV genotypes into human hepatocytes. Sci. Rep. 2016, 6, 27268. [Google Scholar] [CrossRef]
- Chen, S.-R.; Wang, A.-Q.; Lin, L.-G.; Qiu, H.-C.; Wang, Y.-T.; Wang, Y. In vitro study on anti-hepatitis C virus activity of Spatholobus suberectus Dunn. Molecules 2016, 21, 1367. [Google Scholar] [CrossRef] [Green Version]
- Lee, S.; Yoon, K.D.; Lee, M.; Cho, Y.; Choi, G.; Jang, H.; Kim, B.; Jung, D.H.; Oh, J.G.; Kim, G.W. Identification of a resveratrol tetramer as a potent inhibitor of hepatitis C virus helicase. Br. J. Pharm. 2016, 173, 191–211. [Google Scholar] [CrossRef]
- Li, S.; Kodama, E.N.; Inoue, Y.; Tani, H.; Matsuura, Y.; Zhang, J.; Tanaka, T.; Hattori, T. Procyanidin B1 purified from Cinnamomi cortex suppresses hepatitis C virus replication. Antivir. Chem. Chemother. 2010, 20, 239–248. [Google Scholar] [CrossRef] [Green Version]
- Sola, M.A.W.M.; Permanasari, A.A.; Adianti, M.; Tumewu, L.; Widyawaruyanti, A.; Hafid, A.F. The Activity of Sterculia quadrifida R. br Stembark against Hepatitis C Virus. In Proceedings of the BROMO Conference (BROMO 2018), East Java, Indonesia, 11–12 July 2018; pp. 106–110. [Google Scholar] [CrossRef]
- Wagoner, J.; Morishima, C.; Graf, T.N.; Oberlies, N.H.; Teissier, E.; Pécheur, E.-I.; Tavis, J.E.; Polyak, S.J. Differential in vitro effects of intravenous versus oral formulations of silibinin on the HCV life cycle and inflammation. PLoS ONE 2011, 6, e16464. [Google Scholar] [CrossRef] [PubMed]
- Poon, T.Y.C.; Ong, K.L.; Cheung, B.M.Y. Review of the effects of the traditional Chinese medicine Rehmannia Six Formula on diabetes mellitus and its complications. J. Diabetes 2011, 3, 184–200. [Google Scholar] [CrossRef] [PubMed]
- Nahmias, Y.; Goldwasser, J.; Casali, M.; Van Poll, D.; Wakita, T.; Chung, R.T.; Yarmush, M.L. Apolipoprotein B-dependent hepatitis C virus secretion is inhibited by the grapefruit flavonoid naringenin. Hepatology 2008, 47, 1437–1445. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lin, Y.-T.; Wu, Y.-H.; Tseng, C.-K.; Lin, C.-K.; Chen, W.-C.; Hsu, Y.-C.; Lee, J.-C. Green tea phenolic epicatechins inhibit hepatitis C virus replication via cycloxygenase-2 and attenuate virus-induced inflammation. PLoS ONE 2013, 8, e54466. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ashfaq, U.A.; Idrees, S. Medicinal plants against hepatitis C virus. World J. Gastroenterol. WJG 2014, 20, 2941. [Google Scholar] [CrossRef]
- Liu, M.-M.; Zhou, L.; He, P.-L.; Zhang, Y.-N.; Zhou, J.-Y.; Shen, Q.; Chen, X.-W.; Zuo, J.-P.; Li, W.; Ye, D.-Y. Discovery of flavonoid derivatives as anti-HCV agents via pharmacophore search combining molecular docking strategy. Eur. J. Med. Chem. 2012, 52, 33–43. [Google Scholar] [CrossRef]
- Lan, K.H.; Wang, Y.W.; Lee, W.P.; Lan, K.L.; Tseng, S.H.; Hung, L.R.; Yen, S.H.; Lin, H.C.; Lee, S.D. Multiple effects of Honokiol on the life cycle of hepatitis C virus. Liver Int. 2012, 32, 989–997. [Google Scholar] [CrossRef]
- Wu, S.F.; Lin, C.K.; Chuang, Y.S.; Chang, F.R.; Tseng, C.K.; Wu, Y.C.; Lee, J.C. Anti-hepatitis C virus activity of 3-hydroxy caruilignan C from Swietenia macrophylla stems. J. Viral Hepat. 2012, 19, 364–370. [Google Scholar] [CrossRef]
- Calland, N.; Sahuc, M.-E.; Belouzard, S.; Pène, V.; Bonnafous, P.; Mesalam, A.A.; Deloison, G.; Descamps, V.; Sahpaz, S.; Wychowski, C. Polyphenols inhibit hepatitis C virus entry by a new mechanism of action. J. Virol. 2015, 89, 10053–10063. [Google Scholar] [CrossRef] [Green Version]
- Lee, W.-P.; Lan, K.-L.; Liao, S.-X.; Huang, Y.-H.; Hou, M.-C.; Lan, K.-H. Inhibitory effects of amentoflavone and orobol on daclatasvir-induced resistance-associated variants of hepatitis C virus. Am. J. Chin. Med. 2018, 46, 835–852. [Google Scholar] [CrossRef]
- Hassan, S.T.; Berchová-Bímová, K.; Petráš, J. Plumbagin, a Plant-Derived Compound, Exhibits Antifungal Combinatory Effect with Amphotericin B against Candida albicans Clinical Isolates and Anti-hepatitis C Virus Activity. Phytother. Res. 2016, 30, 1487–1492. [Google Scholar] [CrossRef] [PubMed]
- Batista, M.N.; Carneiro, B.M.; Braga, A.C.S.; Rahal, P. Caffeine inhibits hepatitis C virus replication in vitro. Arch. Virol. 2015, 160, 399–407. [Google Scholar] [CrossRef] [PubMed]
- Ma, C.-M.; Wei, Y.; Wang, Z.-G.; Hattori, M. Triterpenes from Cynomorium songaricium—Analysis of HCV protease inhibitory activity, quantification, and content change under the influence of heating. J. Nat. Med. 2009, 63, 9–14. [Google Scholar] [CrossRef] [PubMed]




| No. | Plant | Family | Part | Extract | Inhibition Target | Ref. |
|---|---|---|---|---|---|---|
| 1 | Alchornea laxiflora | Euphorbiaceae | Root | Methanol | HIV integrase | [31] |
| 2 | Mimusops elengi | Sapotaceae | Leaf | Ethanol | HIV integrase | [32] |
| 3 | Sceletium tortuosum | Aizoaceae | Whole plant | Ethanol | HIV integrase | [33] |
| 4 | Hoodia gordonii | Apocynaceae | Whole plant | Ethanol | HIV integrase | [34] |
| 5 | Panax notoginseng | Araliaceae | Whole plant | Methanol | HIV integrase | [35] |
| 6 | Arctium lappa | Asteraceae | Aerial | Methanol | HIV integrase | [35] |
| 7 | Blumea balsamifera | Asteraceae | Whole plant | Ethanol | HIV integrase | [36] |
| 8 | Chrysanthemum indicum | Asteraceae | Capitulum | Methanol | HIV integrase | [35] |
| 9 | Chrysanthemum morifolium | Asteraceae | Capitulum | Ethanol | HIV integrase | [37] |
| 10 | Eclipta prostrate | Asteraceae | Whole plant | Chloroform | HIV integrase | [27] |
| 11 | Senecio scandens | Asteraceae | Whole plant | Methanol | HIV integrase | [34] |
| 12 | Boraginaceae Cordia | Spinescens | Leaf | Methanol, Aqueous | HIV integrase | [38] |
| 13 | Calophyllum inophyllum | Clusiaceae | Bark | Methanol | HIV integrase | [39] |
| 14 | Dioscorea bulbifera | Dioscoreaceae | Whole plant | Methanol | HIV integrase | [40] |
| 15 | Albizia procera | Fabaceae | Whole plant | Methanol | HIV integrase | [35] |
| 16 | Caesalpinia sappan | Fabaceae | Stem | Methanol | HIV integrase | [35] |
| 17 | Agastache rugosa | Lamiaceae | Whole plant | Aqueous methanol | HIV integrase | [41] |
| 18 | Salvia miltiorrhiza | Lamiaceae | Root | Aqueous | HIV integrase | [42] |
| 19 | Lindera aggregate | Lamiaceae | Stem | Methanol | HIV integrase | [43] |
| 20 | Aglaia lawii | Meliaceae | Leaf | Methanol | HIV integrase | [44] |
| 21 | Bersama abyssinica | Melianthaceae | Root | Aqueous | HIV integrase | [45] |
| 22 | Avicennia officinalis | Acanthaceae | Leaf | Methanol | HIV-reverse transcription | [46] |
| 23 | Justicia gendarussa | Acanthaceae | Aerial | Ethanol | HIV-reverse transcription | [47] |
| 24 | Rhinacanthus nasutus | Acanthaceae | Aerial | Hexane | HIV-reverse transcription | [48] |
| 25 | Acorus calamus | Acoraceae | Rhizome | Hexane | HIV-reverse transcription | [48] |
| 26 | Sambucus nigra | Adoxaceae | Whole plant | Methanol | HIV-reverse transcription | [49] |
| 27 | Sambucus racemosa | Adoxaceae | Leaf | Methanol | HIV-reverse transcription | [50] |
| 28 | Aerva lanata | Amaranthaceae | Root | Hexane | HIV-reverse transcription | [51] |
| 29 | Crinum amabile | Amaryllidaceae | Bulb | Methanol | HIV-reverse transcription | [52] |
| 30 | Ancistrocladus korupensis | Ancistrocladaceae | Root | Methanol | HIV-reverse transcription | [53] |
| 31 | Polyalthia suberosa | Annonaceae | Stem | Methanol | HIV-reverse transcription | [47] |
| 32 | Ridolfia segetum | Apiaceae | Whole plant | Essential oil | HIV-reverse transcription | [54] |
| 33 | Hemidesmus indicus | Apocynaceae | Whole plant | Methanol | HIV-reverse transcription | [55] |
| 34 | Tabernaemontana stapfiana | Apocynaceae | Whole plant | Ethanol | HIV-reverse transcription | [56] |
| 35 | Calendula officinalis | Asteraceae | Leaf | Dichloromethane | HIV-reverse transcription | [57] |
| 36 | Gamochaeta simplicicaulis | Asteraceae | Whole plant | Pet ether | HIV-reverse transcription | [58] |
| 37 | Lobostemon trigonus | Boraginaceae | Whole plant | Aqueous | HIV-reverse transcription | [59] |
| 38 | Brassica rapa | Brassicaceae | Whole plant | Methanol | HIV-reverse transcription | [60] |
| 39 | Lonicera japonica | Caprifoliaceae | Flower | Ethanol | HIV-reverse transcription | [61] |
| 40 | Gymnosporia buchananii | Celastraceae | Whole plant | Methanol | HIV-reverse transcription | [56] |
| 41 | Salacia chinensis | Celastraceae | Stem | Methanol | HIV-reverse transcription | [48] |
| 42 | Combretum molle | Combretaceae | Root | Aqueous | HIV-reverse transcription | [62] |
| 43 | Ipomoea aquatic | Convolvulaceae | Whole plant | 80% ethanol | HIV-reverse transcription | [47] |
| 44 | Ipomoea cairica | Convolvulaceae | Aerial | Water | HIV-reverse transcription | [47] |
| 45 | Ipomoea carnea | Convolvulaceae | Aerial | Water | HIV-reverse transcription | [47] |
| 46 | Chamaesyce hyssopifolia | Euphorbiaceae | Whole plant | Methanol | HIV-reverse transcription | [38] |
| 47 | Acalypha Indica | Euphorbiaceae | Whole plant | Methanol | HIV-reverse transcription | [63] |
| 48 | Euphorbia polyacantha | Euphorbiaceae | Whole plant | Aqueous | HIV-reverse transcription | [52] |
| 49 | Mallotus philippensis | Euphorbiaceae | Flower | Methanol | HIV-reverse transcription | [48] |
| 50 | Bauhinia variegata | Fabaceae | Whole plant | Ethanol | HIV-reverse transcription | [60] |
| 51 | Phaseolus vulgaris | Fabaceae | Seed | Methanol | HIV-reverse transcription | [64] |
| 52 | Pterocarpus marsupium | Fabaceae | Whole plant | Aqueous | HIV-reverse transcription | [65] |
| 53 | Tripterospermum lanceolatum | Gentianaceae | Whole plant | Methanol | HIV-reverse transcription | [66] |
| 54 | Hypericum hircinum | Hypericaceae | Whole plant | Ethanol | HIV-reverse transcription | [67] |
| 55 | Ajuga decumbens | Lamiaceae | Whole plant | Methanol | HIV-reverse transcription | [68] |
| 56 | Hyssopus officinalis | Lamiaceae | Leaf | Methanol | HIV-reverse transcription | [69] |
| 57 | Ocimum kilimandscharicum | Lamiaceae | Whole plant | Methanol | HIV-reverse transcription | [70] |
| 58 | Ximenia caffra | Olacaceae | Whole plant | Aqueous | HIV-reverse transcription | [71] |
| 59 | Phyllanthus amarus | Phyllanthaceae | Whole plant | Aqueous | HIV-reverse transcription | [72] |
| 60 | Scoparia dulcis | Plantaginaceae | Leaf | Methanol | HIV-reverse transcription | [73] |
| 61 | Canthium coromandelicum | Rubiaceae | Leaf | Methanol | HIV-reverse transcription | [74] |
| 62 | Alisma plantago-aquatica | Alismataceae | Rhizome | Aqueous | HIV-protease | [75] |
| 63 | Toxicodendron acuminatum | Anacardiaceae | Whole | Methanol | HIV-protease | [76] |
| 64 | Xylopia frutescens | Annonaceae | Bark | Aqueous | HIV-protease | [38] |
| 65 | Ammi visnaga | Apiaceae | Fruit | Methanol | HIV-protease | [77] |
| 66 | Anethum graveolens | Apiaceae | Seed | Methanol | HIV-protease | [76] |
| 67 | Angelica grosseserrata | Apiaceae | Aerial | Aqueous | HIV-protease | [78] |
| 68 | Torilis japonica | Apiaceae | Seed | Methanol | HIV-protease | [78] |
| 69 | Gymnema sylvestre | Apocynaceae | Whole plant | Methanol | HIV-protease | [79] |
| 70 | Garcinia buchneri | Clusiaceae | Steam | Methanol | HIV-protease | [80] |
| 71 | Garcinia kingaensis | Clusiaceae | Steam | Methanol | HIV-protease | [80] |
| No. | Compound | Activity | Dose/IC50 | Ref. |
|---|---|---|---|---|
| 1 | Ellagic acid | Inhibition of HIV integrase | 90.23 μM | [30] |
| 2 | Gallocatechin | Inhibition of HIV integrase | 35.0 µM | [31] |
| 3 | Hernandonine | Inhibition of HIV integrase | 16.3 μM | [82] |
| 4 | Laurolistine | Inhibition of HIV integrase | 7.7 μM | [82] |
| 5 | 7-oxohernangerine | Inhibition of HIV integrase | 18.2 μM | [82] |
| 6 | Lindechunine A | Inhibition of HIV integrase | 21.1 μM | [82] |
| 7 | Quercitrin | RT inhibition | 60 μM | [83] |
| 8 | Gallic acid | Viral infection inhibition | 0.36 μg/mL | [84] |
| 9 | Erythro-7′-methylcarolignan E | Viral infection inhibition | 6.3 μM | [83] |
| 10 | Ascalin | RT inhibition | 10 μM | [85] |
| 11 | Justiprocumins A | RT inhibition | 200 μg/mL | [47] |
| 12 | Robustaflavone | RT inhibition | 65 μM | [86] |
| 13 | Hinokiflavone | RT inhibition | 65 μM | [86] |
| 14 | Agathisflavone | RT inhibition | 119 μM | [86] |
| 15 | Morelloflavone | RT inhibition | 100 μM | [86] |
| 16 | Michellamines A | RT inhibition | 1 μM | [87] |
| 17 | Betulinic acid | RT inhibition | 13 μM | [88] |
| 18 | Michellamines A2 | RT inhibition | 29.6 μM | [89] |
| 19 | Michellamines A3 | RT inhibition | 15.2 μM | [89] |
| 20 | Michellamines A4 | RT inhibition | 35.9 μM | [89] |
| 21 | Michellamines B | RT inhibition | 20.4 μM | [89] |
| 22 | Lupeol | RT inhibition | 3.8 μM | [55] |
| 23 | Lupeol acetate | RT inhibition | 6.4 μM | [55] |
| 24 | Chlorogenic acid | RT inhibition | 4.7 μM | [55] |
| 25 | Artemisinin | RT inhibition | 100 μM | [90] |
| 26 | Luteolin | RT inhibition | 12.8 μM | [91] |
| 27 | Gossypetin | RT inhibition | 2 μg/mL | [92] |
| 28 | Xanthohumol | RT inhibition | 0.5 μg/mL | [93] |
| 29 | Kaempferol 3-rhamnosyl-rutinosid | RT inhibition | 0.23 μM | [94] |
| 30 | Robustaflavone | RT inhibition | 65 μM | [95] |
| 31 | Protostanes | RT inhibition | 5.8 μg/mL | [96] |
| 32 | Morelloflavone | RT inhibition | 86 μM | [97] |
| 33 | Anolignan A | RT inhibition | 156 μg/mL | [95] |
| 34 | Cucurbitacins | RT inhibition | 28 μM | [98] |
| 35 | Oleanolic acid | RT inhibition | 2 μg/mL | [99] |
| 36 | p-cymene | RT inhibition | 7.6 μg/mL | [99] |
| 37 | Baicalein | RT inhibition | 2 μg/mL | [100] |
| No. | Plant | Family | Part | Extract | Mode of Action/Virus | Ref. |
|---|---|---|---|---|---|---|
| 1 | Peganum harmala | Nitrariaceae | Seed | Methanol | Virucidal action/HSV2 | [111] |
| 2 | Pistacia vera | Anacardiaceae | Seed | Methanol | Viral DNA synthesis inhibition/HSV1 | [112] |
| 3 | Rhus aromatica | Anacardiaceae | Root | Aqueous | Inhibit the virus penetration/HSV1 | [113] |
| 4 | Quercus brantii | Cynipidae | Fruit | Chloroform | Inhibit virus entry/HSV1 | [114] |
| 5 | Tanacetum parthenium | Asteraceae | Arial | Aqueous | Virus replication imbibition/HSV1 | [115] |
| 6 | Centella asiatica | Umbelliferae | Aerial | Aqueous | Inhibition of viral replication/HSV2 | [116] |
| 7 | Pistacia lentiscus | Anacardiaceae | Stem | Methanol | Virus absorption imbibition/HSV2 | [111] |
| 8 | Mangifera indica | Anacardiaceae | Leaves | Aqueous | Inhibition of viral replication/HSV2 | [116] |
| 9 | Eucalyptus denticulata | Myrtaceae | Aerial | Acetone | Inhibit virus entry/HSV1 | [117] |
| 10 | Aglaia odorata | Meliaceae | Leaf | Ethanol | Inhibition of viral replication/HSV2 | [118] |
| 11 | Euphorbia coopire | Euphorbiaceae | Flowers | Chloroform/methylene chloride | Inhibition of viral replication/HSV1 | [119] |
| 12 | Rhus aromatica | Anacardiaceae | Bark | Aqueous | Inhibit virus entry/HSV2 | [113] |
| 13 | Anacardium occidentale | Anacardiaceae | Leaf | Aqueous | Inhibition of viral replication/HSV2 | [120] |
| 14 | Phoradendron crassifolium | Loranthaceae | Leaf | Ethanol | Inhibition of viral replication/HSV2 | [120] |
| 15 | Morus alba | Moraceae | Leaf | Aqueous methanol | Inhibition of viral replication/HSV1 | [119] |
| 16 | Aloe vera | Liliaceae | Leaf | Gel | Replication inhibition/HSV1 | [121] |
| 17 | Annona muricata | Annonaceae | Stembark | Petroleum ether | Inhibition of viral replication/HSV2 | [122] |
| 18 | Petunia nyctaginiflora | Solanaceae | Stembark | Petroleum ether | Inhibition of viral replication/HSV2 | [122] |
| 19 | Cuphea carthagenensis | Lythraceae | Ariel | Ethanol | Inhibition of viral replication/HSV1 | [123] |
| 20 | Graptopetalum paraguayense | Crassulaceae | Leaf | Methanol/water | Inhibition of viral replication/HSV1 | [124] |
| 21 | Prunus dulcis | Rosaceae | Almond skin | Methanol/Hcl | Block virus entry | [125] |
| 22 | Equisetum giganteum | Equisetaceae | Root and stem | Ethanol/water | Inhibition of viral cell attachment and entry/HSV2 | [126] |
| 23 | Schinus terebinthifolia | Anacardiaceae | Bark | Ethanol/water | Inhibition of viral attachment and penetration/HSV1 | [127] |
| 24 | Nepeta nuda | Lamiaceae | Aerial | Aqueous | Inhibition of viral absorption and replication/HSV1 | [128] |
| 25 | Cornus canadensis | Cornaceae | Leaf | Aqueous | Virus absorption inhibition/HSV1 | [129] |
| 26 | Strychnos pseudoquina | Loganiaceae | Stem | Ethyl acetate | Interference with various steps of virus cycle/HSV1 | [130] |
| 27 | Tillandsia usneoides | Bromeliaceae | Fruits | Ethanol | Inhibition of viral replication/HSV1 | [123] |
| 28 | Copaifera reticulate | Fabaceae | Leaf | Ethanol/water | Inhibition of viral cell attachment and entry/HSV2 | [126] |
| 29 | Spondias mombin | Anacardiaceae | Leaf | Methanol | Inhibition of viral cell attachment/HSV1 | [131] |
| 30 | Solanum melongena | Solanaceae | Peel | Ethanol | Reduction of viral protein Expression/HSV1 | [132] |
| 31 | Ixeris Sonchifolia | Compositae | Whole plant | Methanol | Inhibition of viral replication/HSV1 | [133] |
| 32 | Eurycoma longifolia | Simaroubaceae | Stem | Methanol | Inhibition of viral replication/HSV1 | [134] |
| 33 | Garcinia mangostana | Guttiferae | Leaf | Methanol | Inhibition of viral replication/HSV1 | [134] |
| 34 | Peganum harmala | Nitrariaceae | Seed | Methanol | Block virus entry/HSV2 | [135] |
| 35 | Erica multiflora | Ericaceae | Ariel | Methanol | Inhibition of viral replication/HSV1 | [136] |
| 36 | Toona sureni | Meliaceae | Leaf | Methanol | Inhibition of viral replication/HSV1 | [134] |
| 37 | Eucalyptus caesia | Myrtaceae | Aerial | Hydro-distillation | Virucidal activity/HSV1 | [137] |
| 38 | Vachellia nilotica | Fabaceae | Bark | Methanol | Block virus attachment/HSV2 | [138] |
| 39 | Stephania cepharantha | Menispermaceae | Root | Methanol | Virucidal effect/HSV1 | [139] |
| 40 | Zygophyllum album | Zygophyllaceae | Whole plant | Acetone | Virucidal effect/HSV1 | [136] |
| 41 | Ficus religiosa | Moraceae | Bark | Methanol | Virucidal effect/HSV1 | [140] |
| 42 | Eucalyptus alba | Myrtaceae | Fruit | Aqueous | Virucidal effect/HSV1 | [134] |
| 43 | Swertia chirata | Renunculaceae | Leaf | Aqueous | Virucidal effect/HSV1 | [141] |
| 44 | Scoparia dulcis | Plantaginaceae | Leaf | Methanol | Inhibit the viral replication/HSV1 | [142] |
| 45 | Pedilanthus tithymaloides | Euphorbiaceae | Leaves | Methanol | inhibition of viral replication/HSV2 | [143] |
| 46 | Melaleuca leucadendron | Myrtaceae | Fruit | Aqueous | Virucidal effect/HSV1 | [134] |
| 47 | Andrographis paniculata | Acanthaceae | Leaf | Ethanol | Virucidal effect/HSV1 | [144] |
| 48 | Artemisia kermanensis | Asteraceae | Aerial | Hydro-distillation | Virucidal activity/HSV1 | [137] |
| 49 | Vigna radiata | Fabaceae | Spout | Methanol | Virucidal activity/HSV1 | [145] |
| 50 | Schleichera oleosa | Sapindaceae | Fruit | Aqueous | Virucidal activity/HSV1 | [134] |
| 51 | Quercus persica | Fagaceae | Fruit | Hydro alcoholic | Viral attachment inhibition/HSV1 | [146] |
| 52 | Pongamia pinnata | Papillionaceae | Seed | Aqueous | Virucidal activity/HSV1 | [147] |
| 53 | Pterocarya stenoptera | Juylandaceae | Bark | Methanol | Viral attachment and penetration inhibition/HSV2 | [148] |
| 54 | Avicennia marina | Avicenniaceae | Leaf | Methanol | Viral replication inhibition/HSV1 | [149] |
| 55 | Nephelium lappaceum | Sapindaceae | Pericarp | Water/methanol | Virucidal activity/HSV1 | [134] |
| 56 | Zataria multiflora | Labiatae | Aerial | Hydro-distillation | Virucidal activity/HSV1 | [137] |
| 57 | Ocimum sanctum | Lamiaceae | Aerial | Methanol | Viral infection inhibition/HSV1 | [150] |
| 58 | Artocarpus lakoocha | Moraceae | Wood | Methanol | Viral infection inhibition/HSV1 | [106] |
| 59 | Scaevola gaudichaudiana | Asteraceae | Aerial | Dichloromethane | Viral absorption inhibition/HSV1 | [151] |
| 60 | Rosmarinus officinalis | Lamiaceae | Aerial | Hydro-distillation | Virucidal activity/HSV1 | [137] |
| 61 | Limonium sinense | Plumbaginaceae | Root | Ethanol | Virucidal activity/HSV1 | [152] |
| 62 | Prunella vulgaris | Lamiaceae | Fruit spikes | Aqueous | Block HSV-1 binding | [153] |
| 63 | Heterophyllaea pustulata | Rubiaceae | Fruit | Dried powder | Viral absorption inhibition/HSV1 | [154] |
| 64 | Filicium decipiens | Sapindaceae | Stem bark | Water/methanol | Virucidal activity/HSV1 | [134] |
| 65 | Punica granatum | Punicaceae | Pericarp | Water/methanol | Virucidal activity/HSV1 | [134] |
| 66 | Satureja hotensis | Lamiaceae | Aerial | Hydrodistillation | Virucidal activity/HSV1 | [137] |
| No. | Compound | Activity | Dose/IC50 | Ref. |
|---|---|---|---|---|
| 1 | 4E-jatrogrossidentadion | Viral inhibition/HSV 1 | 2.05 μg/mL | [159] |
| 2 | 7-galloyl catechin | Viral inhibition/HSV 1 | 43.2 μg/mL | [119] |
| 3 | Gallic acid | Viral inhibition/HSV 1 | 49.8 μg/mL | [119] |
| 4 | Kaempferol 3-O-β-(6″-O-galloyl)-glucopyranoside | Viral inhibition/HSV 1 | 124.1 μg/mL | [119] |
| 5 | Quercetin 3-O-β-(6″-O-galloyl)-glucopyranoside | Viral inhibition/HSV 1 | 175.6 μg/mL | [119] |
| 6 | Curcumin | Viral inhibition/HSV 1 | 49.8 μg/mL | [119] |
| 7 | Quercetin | Viral inhibition/HSV 1 | 78.1 μg/mL | [119] |
| 8 | Kaempferol | Viral inhibition/HSV 1 | 76.1 μg/mL | [119] |
| 9 | 3,4-Dehydrocycleanine | Viral inhibition/HSV 1 | 43.2 μg/mL | [139] |
| 10 | (−)-Cycleanine | Viral inhibition/HSV 1 | 26.3 μg/mL | [139] |
| 11 | (−)-Norcycleanine | Viral inhibition/HSV 1 | 18.1 μg/mL | [139] |
| 12 | 2-Norcepharanoline | Viral inhibition/HSV 1 | 26.3 μg/mL | [139] |
| 13 | Obaberine | Viral inhibition/HSV 1 | 14.8 μg/mL | [139] |
| 14 | Homoaromoline | Viral inhibition/HSV 1 | 15.1 μg/mL | [139] |
| 15 | Aromoline | Viral inhibition/HSV 1 | 20.4 μg/mL | [139] |
| 16 | Isotetrandrine | Viral inhibition/HSV 1 | 17.4 μg/mL | [139] |
| 17 | Berbamine | Viral inhibition/HSV 1 | 17.4 μg/mL | [139] |
| 18 | Thalrugosine | Viral inhibition/HSV 1 | 16.8 μg/mL | [139] |
| 19 | Obamegine | Viral inhibition/HSV 1 | 23.5 μg/mL | [139] |
| 20 | 2-Norberbamine | Viral inhibition/HSV 1 | 16.8 μg/mL | [139] |
| 21 | 3’,4’-Dihydrostephasubine | Viral inhibition/HSV 1 | 27.4 μg/mL | [139] |
| 22 | Palmatine | Viral inhibition/HSV 1 | 34.0 μg/mL | [139] |
| 23 | Cephakicine | Viral inhibition/HSV 1 | 44.5 μg/mL | [139] |
| 24 | N-Methylcrotsparine | Viral inhibition/HSV 1 | 8.3 μg/mL | [139] |
| 25 | Andrographolide | Viral inhibition/HSV 1 | 8.28 μg/mL | [144] |
| 26 | Neoandrographolide | Viral inhibition/HSV 1 | 7.97 μg/mL | [144] |
| 27 | 14-Deoxy-11,12-didehydroandrographolide | Viral inhibition/HSV 1 | 11.1 μg/mL | [144] |
| 28 | Oxyresveratrol | Inhibitory activity at the early phase and late phase of replication/HSV1 | 24 μg/mL | [106] |
| 29 | Samarangenin B | Inhibition of viral replication/HSV1 | 11.4 μg/mL | [152] |
| 30 | (−)-epigallocatechin 3-O-gallate | Viral inhibition/HSV 1 | 38.6 μg/mL | [152] |
| 31 | Pterocarnin A | Viral attachment inhibition/HSV 1 | 5.4 μM | [148] |
| 32 | Scopadulcic acid B | Viral attachment inhibition/HSV 1 | 0.012 μM | [142] |
| No. | Plant | Family | Part | Extract | Inhibition Target | Ref. |
|---|---|---|---|---|---|---|
| 1 | Cistus incanus | Cistaceae | Whole plant | Polyphenol-rich plant extract | MDCK cell-based assay | [191] |
| 2 | Thuja orientalis | Cupressaceae | Leaves | Methanol | Blockage of attachment to the host cells and inhibition of replication | [192] |
| 3 | Pimpeniella anisum | Apiaceae | Seeds | Aqueous | Direct effect on replication | [193] |
| 4 | Aloe sinana | Xanthorrhoeaceae | Root and leaf latex | Methanol | Induced CPE and increased the cell viability of Vero cells | [194] |
| 5 | Punica granatum L. | Lythraceae | Peel | Ethanol | Inhibit influenza A virus replication | [195] |
| 6 | Geranium thunbergii | Geranii Herba | Dried aerial part | Ethanol | Neuraminidase (NA) inhibitors | [196] |
| 7 | Mussaenda elmeri | Rubiaceae | Whole plant | Dichloromethane and methanol in a 1/1 (v/v) ratio | Inhibition of hemagglutination | [197] |
| 8 | Trigonopleura malayana | Euphorbiaceae | Leaves | Dichloromethane and methanol in a 1/1 (v/v) ratio | Inhibition of hemagglutination | [197] |
| 9 | Mussaenda elmeri | Rubiaceae | Whole plant | Dichloromethane and methanol in a 1/1 (v/v) ratio | Inhibition of hemagglutination | [197] |
| 10 | Santiria apiculata | Burseraceae | Whole plant | Dichloromethane and methanol in a 1/1 (v/v) ratio | Inhibition of hemagglutination | [197] |
| 11 | Anisophyllea disticha | Anisophylleaceae | Stems | Dichloromethane and methanol in a 1/1 (v/v) ratio | Inhibition of hemagglutination | [197] |
| 12 | Trivalvaria macrophylla | Annonaceae | Roots | Dichloromethane and methanol in a 1/1 (v/v) ratio | Inhibition of hemagglutination | [197] |
| 13 | Baccaurea angulata | Euphorbiaceae | Stems | Dichloromethane and methanol in a 1/1 (v/v) ratio | Inhibition of hemagglutination | [197] |
| 14 | Tetracera macrophylla | Dilleniaceae | Leaves | Dichloromethane and methanol in a 1/1 (v/v) ratio | Inhibition of hemagglutination | [197] |
| 15 | Calophyllum lanigerum | Clusiaceae | Whole plant | Dichloromethane and methanol in a 1/1 (v/v) ratio | Inhibition of hemagglutination | [197] |
| 16 | Calophyllum lanigerum | Clusiaceae | Stems | Dichloromethane and methanol in a 1/1 (v/v) ratio | Inhibition of hemagglutination | [197] |
| 17 | Albizia corniculata | Fabaceae | Stems | Dichloromethane and methanol in a 1/1 (v/v) ratio | Inhibition of hemagglutination | [197] |
| 18 | Mussaenda elmeri | Rubiaceae | Whole plant | Dichloromethane and methanol in a 1/1 (v/v) ratio | Inhibition of hemagglutination | [197] |
| 19 | Polygonum chinense | Polygonaceae | Whole plant | Methanol | Inhibited viral replication viral neuraminidase | [198] |
| 20 | Bletilla striata | Orchidaceae | Rhizomes | Ethanol | Viability assay | [199] |
| 21 | Jatropha multifida Linn | Euphorbiaceae | Stems | 70% aqueous ethanol | Virus-infected MDCK cells-based assay | [200] |
| 22 | Dandelion | Asteraceae | Whole plant | Aqueous | Inhibit polymerase activity and reduce virus nucleoprotein (NP) RNA level. | [201] |
| 23 | Radix Paeoniae Alba | Paeoniaceae | Roots | Aqueous | Inhibit the replication | [202] |
| 24 | Balanites aegyptiaca, | Zygophyllaceae | Leaves | Aqueous or 70% methanol | Inhibited the virus-induced hemagglutination of chicken RBCs | [203] |
| 25 | Cordia africana, | Boraginaceae | Bark | Aqueous or 70% methanol | Inhibited the virus-induced hemagglutination of chicken RBCs | [203] |
| 26 | Aristolochia bracteolata | Aristolochiaceae | Whole plant | Aqueous or 70% methanol | Inhibited the virus-induced hemagglutination of chicken RBCs | [203] |
| 27 | Boscia senegalensis | Capparaceae | Leaves | Aqueous or 70% methanol | Inhibited the virus-induced hemagglutination of chicken RBCs | [203] |
| 28 | Leptadenia arborea | Apocynaceae | Roots | Aqueous or 70% methanol | Inhibited the virus-induced hemagglutination of chicken RBCs | [203] |
| 29 | Punica granatumL. | Lythraceae | Peel | Ethyl alcohol extract | Inhibition of viral adsorption and viral RNA transcription | [204] |
| 30 | Caesalpinia decapetala | Fabaceae | Leaves | 75% aqueous ethanol | Inhibit replication | [205] |
| No. | Compound | Activity | Dose/IC50 | Ref. |
|---|---|---|---|---|
| 1 | Pentagalloylglucose | Inhibited the virus-induced hemagglutination of chicken RBCs | 11.3 µg/mL | [211] |
| 2 | Quercetin | Inhibit the entry of the H5N1 virus | 7.75 µg/mL | [212] |
| 3 | Apigenin | Inhibited viral replication viral neuraminidase | 21.54 µM | [213] |
| 4 | Baicalein | Inhibited H5N1 viral replication viral neuraminidase | 18.79 µM | [213] |
| 5 | Biochanin A | Inhibited H5N1 viral replication viral neuraminidase | 8.92 µM | [213] |
| 6 | Hispidulin | Inhibition against H1N1 neuraminidase | 11.18 µM | [214] |
| 7 | Nepetin | Inhibition against H1N1 neuraminidase | 12.54 µM | [214] |
| 8 | Rosmarinic acid methyl ester | Inhibition against H1N1 neuraminidase | 15.47 µM | [214] |
| 9 | Luteolin | Inhibition against H1N1 neuraminidase | 19.83 µM | [214] |
| 10 | Homonojirimycin | Inhibition against H1N1 neuraminidase | 10.4 µg/mL | [215] |
| 11 | Dendrobine | Inhibited early steps in the H1N1 viral replication cycle | 3.39 µg/mL | [216] |
| No. | Plant | Family | Part | Extract | Inhibition Target | Ref. |
|---|---|---|---|---|---|---|
| 1 | Ajuga bracteosa | Lamiaceae | Leaves | Methanol | HCV infection Replication | [224] |
| 2 | Ajuga parviflora | Lamiaceae | Leaves | Methanol | HCV infection Replication | [224] |
| 3 | Berberis lycium | Lamiaceae | Roots | Methanol | HCV infection Replication | [224] |
| 4 | Toona sureni | Meliaceae | Leaves | 80% Ethanol | HCV infection Replication | [225] |
| 5 | Melicope latifolia | Rutaceae | Leaves | 80% Ethanol | HCV infection Replication | [225] |
| 6 | Melanolepis multiglandulosa | Euphorbiaceae | Stems | 80% Ethanol | HCV infection Replication | [225] |
| 7 | Ficus fistulosa | Moraceae | Leaves | 80% Ethanol | HCV infection Replication | [225] |
| 8 | Phyllanthus amarus | Phyllanthaceae | Whole plant | Methanol | Inhibition of HCV RNA replication | [226] |
| 9 | Acacia nilotica | Mimosaceae | Bark | Methanol | Hepatitis C virus (HCV) protease inhibition | [227] |
| 10 | Boswellia carterii | Burseraceae | Root | Methanol | Hepatitis C virus (HCV) protease inhibition | [227] |
| 11 | Embelia schimperi | Myrsinaceae | Fruit | Methanol | Hepatitis C virus (HCV) protease inhibition | [227] |
| 12 | Piper cubeba | Piperaceae | Fruit | Aqueous | Hepatitis C virus (HCV) protease inhibition | [227] |
| 13 | Quercus infectoria | Fagaceae | Gall | Methanol | Hepatitis C virus (HCV) protease inhibition | [227] |
| 14 | Syzygium aromaticum | Myrtaceae | Fruit | Aqueous | Hepatitis C virus (HCV) protease inhibition | [227] |
| 15 | Trachyspermum ammi | Apiaceae | Fruit | Methanol | Hepatitis C virus (HCV) protease inhibition | [227] |
| 16 | Morinda citrifolia | Rubioideae | Leaves | Methanol | Hepatitis C virus (HCV) protease inhibition | [228] |
| 17 | Silybum marianum | Asteraceae | Flower | Methanol | Hepatitis C virus (HCV) protease inhibition | [229] |
| 18 | Limonium sinense | Plumbaginaceae | Flower | Aqueous | HCV infection Replication | [230] |
| 19 | Bupleurum kaoi | Apiaceae | Root | Methanol | Inhibit HCV entry | [231] |
| 20 | Rhizoma coptidis | Ranunculaceae | Whole | Methanol | Inhibit HCV entry | [232] |
| 21 | Schisandra sphenanthera | Schisandraceae | Rhizome | Methanol | Inhibit HCV entry | [232] |
| 22 | Solanum nigrum | Solanaceae | Seed | Chloroform | NS3 protease inhibition | [233] |
| 23 | Terminalia arjuna | Combretaceae | Bark | Methanol | NS3 protease inhibition | [226] |
| 24 | Embelia ribes | Myrsinaceae | Leaf | Aqueous | NS3 protease inhibition | [234] |
| 25 | Aeginetia indica | Orobanchaceae | Whole | Aqueous | NS5B polymerase inhibition | [235] |
| 26 | Rhodiola kirilowii | Crassulaceae | Flower | Ethanol | NS3 protease inhibition | [236] |
| 27 | Schisandra sphenanthera | Schisandraceae | Fruit | Ethanol | Inhibition of HCV entry | [237] |
| 28 | Spatholobus suberectus | Fabaceae | Leaf | Ethanol | NS3 protease inhibition | [238] |
| 29 | Vitis vinifera | Vitaceae | Root | Ethanol | NS3 helicase inhibition | [239] |
| 30 | Cinnamomi cortex | Lauraceae | Bark | Methanol | Inhibition of HCV replication and RNA synthesis | [240] |
| No. | Compound | Activity | Dose/IC50 | Ref. |
|---|---|---|---|---|
| 1 | Embelin | Hepatitis C virus (HCV) protease inhibition | 21 µM | [227] |
| 2 | Silymarin | NS5B polymerase inhibition | 40 µM | [242] |
| 3 | 5-O-Methylembelin | Hepatitis C virus (HCV) protease inhibition | 46 µM | [227] |
| 4 | Pheophorbide a | Hepatitis C virus (HCV) protease inhibition | 0.3 μg/mL | [228] |
| 5 | Pentagalloylglucose | Inhibit viral attachment | 2.2 µM | [243] |
| 6 | Quercetin | inhibitory effect of NS3 catalytic activity | 10 µg/mL | [234] |
| 7 | Naringenin | Hepatitis C virus (HCV) protease inhibition | 200 μM | [244] |
| 8 | (+)-Epicatechin | Inhibition of HCV replication | 75 μM | [245] |
| 9 | (−)-Epicatechin | Inhibition of HCV replication | 75 μM | [245] |
| 10 | Ladanein | inhibition of the post attachment entry step of HCV | 2.5 μM | [246] |
| 11 | Luteolin | Inhibition of HCV infection Replication in NS5B polymerase | 7.9 μM | [247] |
| 12 | Honokiol | Inhibition of HCV infection Replication in NS5B polymerase | 4.5 μM | [248] |
| 13 | 3-Hydroxy caruilignan C | Inhibition of HCV replication | 37.5 μM | [249] |
| 14 | Gallic acid | Inhibition of viral entry | 24.31 μM | [230] |
| 15 | Saikosaponin b2 | Inhibition of viral entry | 16.13 μM | [231] |
| 16 | Delphinidin | Inhibition of viral entry | 3.7 µM | [250] |
| 17 | Amentoflavone | Inhibition of viral entry | 42 µM | [251] |
| 18 | 7,40-Dihydroxyflavanone | Inhibition of viral entry | 42 µM | [251] |
| 19 | Orobol | Inhibition of viral entry | 42 µM | [251] |
| 20 | 3,3′-Digalloylproprodelphinidin | NS3 protease inhibition | 0.77 μM | [236] |
| 21 | B2, 3,3′-Digalloylprocyanidin | NS3 protease inhibition | 0.91 μM | [236] |
| 22 | B2, (−)-Epigallocatechin-3-O-gallate, (−)-Epicatechin- | NS3 protease inhibition | 8.51 μM | [236] |
| 23 | 3-O-gallate | NS3 protease inhibition | 18.55 μM | [236] |
| 24 | Schizandronic acid | Inhibition of HCV entry | 5.27 μg/mL | [237] |
| 25 | Vitisin B | NS3 helicase inhibition | 0.006 μM | [239] |
| 26 | Procyanidin B1 | Inhibition of HCV replication and RNA synthesis | 29 μM | [240] |
| 27 | Plumbagin | Inhibition of HCV infection Replication in NS5B polymerase | 0.57 μM | [252] |
| 28 | Caffeine | Inhibition of HCV infection Replication in NS5B polymerase | 0.726 mM | [253] |
| 29 | Ursolic acid | Inhibition of HCV infection Replication in NS5B polymerase | 16 μg/mL | [254] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mohan, S.; Elhassan Taha, M.M.; Makeen, H.A.; Alhazmi, H.A.; Al Bratty, M.; Sultana, S.; Ahsan, W.; Najmi, A.; Khalid, A. Bioactive Natural Antivirals: An Updated Review of the Available Plants and Isolated Molecules. Molecules 2020, 25, 4878. https://doi.org/10.3390/molecules25214878
Mohan S, Elhassan Taha MM, Makeen HA, Alhazmi HA, Al Bratty M, Sultana S, Ahsan W, Najmi A, Khalid A. Bioactive Natural Antivirals: An Updated Review of the Available Plants and Isolated Molecules. Molecules. 2020; 25(21):4878. https://doi.org/10.3390/molecules25214878
Chicago/Turabian StyleMohan, Syam, Manal Mohamed Elhassan Taha, Hafiz A. Makeen, Hassan A. Alhazmi, Mohammed Al Bratty, Shahnaz Sultana, Waquar Ahsan, Asim Najmi, and Asaad Khalid. 2020. "Bioactive Natural Antivirals: An Updated Review of the Available Plants and Isolated Molecules" Molecules 25, no. 21: 4878. https://doi.org/10.3390/molecules25214878
APA StyleMohan, S., Elhassan Taha, M. M., Makeen, H. A., Alhazmi, H. A., Al Bratty, M., Sultana, S., Ahsan, W., Najmi, A., & Khalid, A. (2020). Bioactive Natural Antivirals: An Updated Review of the Available Plants and Isolated Molecules. Molecules, 25(21), 4878. https://doi.org/10.3390/molecules25214878