Photodegradation of Anti-Inflammatory Drugs: Stability Tests and Lipid Nanocarriers for Their Photoprotection
Abstract
:1. Introduction
2. Photodegradation Studies of NSAIDs
2.1. ICH Quality Guidelines
2.2. Analytical Techniques for Drug Determination
2.3. Application of the Photodegradation Test
3. Characteristics of Lipid Nanocarriers
3.1. NSAIDs in Liposomes
3.2. NSAIDs in Niosomes
3.3. NSAIDs in Solid Lipid Nanoparticles
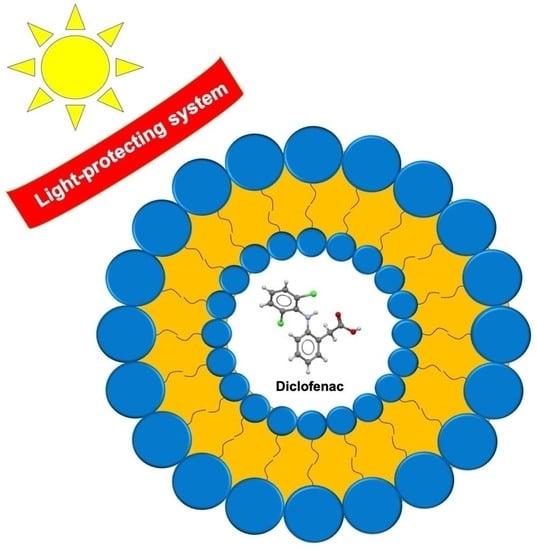
4. Lipid Nanocarriers for Photoprotection of NSAIDs
4.1. Photoprotection of NSAIDs in Liposomes
4.2. Photoprotection of NSAIDs in Niosomes
4.3. Photoprotection of NSAIDs in Solid Lipid Nanoparticles
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Machado, G.C.; Maher, C.G.; Ferreira, P.H.; Day, R.O.; Pinheiro, M.B.; Ferreira, M.L. Non-steroidal anti-inflammatory drugs for spinal pain: A systematic review and meta-analysis. Ann. Rheum. Dis. 2017, 76, 1269–1278. [Google Scholar] [CrossRef] [PubMed]
- Basha, R.; Baker, C.T.; Sankpal, U.T.; Ahmad, S.; Safe, S.; Abbruzzese, J.L.; Abdelrahim, M. Therapeutic applications of NSAIDS in cancer: Special emphasis on tolfenamic acid. Front. Biosci. 2011, 3, 797–805. [Google Scholar] [CrossRef] [Green Version]
- Flattery, M.P.; Hylton Gravatt, L.A. COX-2 inhibitors and cardiovascular risk. Prog. Cardiovasc. Dis. 2005, 20, 123–125. [Google Scholar] [CrossRef] [PubMed]
- Park, J.; Lee, S.H.; You, S.C.; Kim, J.; Yang, K. Non-steroidal anti-inflammatory agent use may not be associated with mortality of coronavirus disease 19. Sci. Rep. 2021, 11, 5087. [Google Scholar] [CrossRef]
- Grande, F.; Giordano, F.; Occhiuzzi, M.A.; Rocca, C.; Ioele, G.; de Luca, M.; Ragno, G.; Panno, M.L.; Rizzuti, B.; Garofalo, A. Toward multitasking pharmacological cox-targeting agents: Non-steroidal anti-inflammatory prodrugs with antiproliferative effects. Molecules 2021, 26, 3940. [Google Scholar] [CrossRef] [PubMed]
- Kowalski, M.L.; Stevenson, D.D. Classification of reactions to nonsteroidal antiinflammatory drugs. Immunol. Allergy Clin. N. Am. 2013, 33, 135–145. [Google Scholar] [CrossRef]
- Ioele, G.; de Luca, M.; Tavano, L.; Ragno, G. The difficulties for a photolabile drug in topical formulations: The case of diclofenac. Int. J. Pharm. 2014, 465, 284–290. [Google Scholar] [CrossRef]
- Takara, A.; Kobayashi, K.; Watanabe, S.; Okuyama, K.; Shimada, Y.; Goto, S. Dibucaine inhibits ketoprofen photodegradation via a mechanism different from that of antioxidants. J. Photochem. Photobiol. A 2017, 333, 208–212. [Google Scholar] [CrossRef]
- Zhang, N.; Li, J.M.; Liu, G.G.; Chen, X.L.; Jiang, K. Photodegradation of diclofenac in seawater by simulated sunlight irradiation: The comprehensive effect of nitrate, Fe(III) and chloride. Mar. Pollut. Bull. 2017, 117, 366–370. [Google Scholar] [CrossRef]
- Cacciari, R.D.; Menis, F.; Biondi, M.A.; Reynoso, E.; Sabini, C.; Montejano, H.A.; Biasutti, M.A. Mechanistic analysis on the photochemistry of the anti-inflammatory drug etoricoxib in aqueous solution. Cytotoxicity of photoproducts. J. Photochem. Photobiol. A 2020, 390, 112331. [Google Scholar] [CrossRef]
- Tu, N.; Liu, Y.; Li, R.; Lv, W.; Liu, G.; Ma, D. Experimental and theoretical investigation on photodegradation mechanisms of naproxen and its photoproducts. Chemosphere 2019, 227, 142–150. [Google Scholar] [CrossRef]
- Jiménez, J.J.; Pardo, R.; Sánchez, M.I.; Muñoz, B.E. Photochemical, thermal, biological and long-term degradation of celecoxib in river water. Degradation products and adsorption to sediment. J. Hazard. Mater. 2018, 342, 252–259. [Google Scholar] [CrossRef]
- El-Yazbi, A.F.; Guirguis, K.M.; Belal, T.S.; Bedair, M.M. Sensitive spectrofluorimetric and mass spectroscopic methods for the determination of nucleic acid damage induced by photosensitized anti-inflammatory drugs: Comparative study. J. Pharm. Biomed. Anal. 2020, 187, 113326. [Google Scholar] [CrossRef]
- Zuba, E.B.; Koronowska, S.; Osmola-Mańkowska, A.; Jenerowicz, D. Drug-Induced Photosensitivity. Acta Dermatovenerol. Croat. 2016, 24, 55. [Google Scholar]
- Kaur, A.; Umar, A.; Kansal, S.K. Sunlight-Driven Photocatalytic Degradation of Non-Steroidal Anti-Inflammatory Drug Based on TiO2 Quantum Dots. J. Colloid Interface Sci. 2015, 459, 257–263. [Google Scholar] [CrossRef] [PubMed]
- Ioele, G.; Tavano, L.; de Luca, M.; Ragno, G.; Picci, N.; Muzzalupo, R. Photostability and ex-vivo permeation studies on diclofenac in topical niosomal formulations. Int. J. Pharm. 2015, 494, 490–497. [Google Scholar] [CrossRef] [PubMed]
- Nakama, K.A.; dos Santos, R.B.; da Rosa Silva, C.E.; Izoton, J.C.; Savall, A.S.P.; Gutirrez, M.E.Z.; Roman, S.S.; Luchese, C.; Pinton, S.; Haas, S.E. Establishment of analytical method for quantification of anti-inflammatory agents co-nanoencapsulated and its application to physicochemical development and characterization of lipid-core nanocapsules. Arab. J. Chem. 2020, 13, 2456–2469. [Google Scholar] [CrossRef]
- Ramos, P.T.; Pedra, N.S.; Soares, M.S.P.; da Silveira, E.F.; Oliveira, P.S.; Grecco, F.B.; da Silva, L.M.C.; Ferreira, L.M.; Ribas, D.A.; Gehrcke, M.; et al. Ketoprofen-Loaded rose hip oil nanocapsules attenuate chronic inflammatory response in a pre-clinical trial in mice. Mater. Sci. Eng. C 2019, 103, 109742. [Google Scholar] [CrossRef]
- Atarashi, K.; Takano, M.; Kato, S.; Kuma, H.; Nakanishi, M.; Tokura, Y. Addition of UVA-absorber butyl methoxy dibenzoylmethane to topical ketoprofen formulation reduces ketoprofen-photoallergic reaction. J. Photochem. Photobiol. B 2012, 113, 56–62. [Google Scholar] [CrossRef]
- León, C.; Henríquez, C.; López, N.; Sanchez, G.; Pastén, B.; Baeza, P.; Ojeda, J. Inhibitory effect of the ascorbic acid on photodegradation of pharmaceuticals compounds exposed to UV-B radiation. J. Photochem. Photobiol. 2021, 7, 314–322. [Google Scholar] [CrossRef]
- Iqbal, Z.; Arafa, E.S.A.; Kanwal, Z.; Murtaza, G. Smart solution of severe problems: Radiolabeled nanocarriers for cancer imaging and therapy. J. Drug Deliv. Sci. Technol. 2021, 61, 102205. [Google Scholar] [CrossRef]
- Pimentel-Moral, S.; Teixeira, M.C.; Fernandes, A.R.; Arráez-Román, D.; Martínez-Férez, A.; Segura-Carretero, A.; Souto, E.B. Lipid nanocarriers for the loading of polyphenols—A comprehensive review. Adv. Colloid Interface Sci. 2018, 260, 85–94. [Google Scholar] [CrossRef]
- Severino, P.; Andreani, T.; Macedo, A.S.; Fangueiro, J.F.; Santana, M.H.A.; Silva, A.M.; Souto, E.B. Current state-of-art and new trends on lipid nanoparticles (SLN and NLC) for oral drug delivery. J. Drug Deliv. 2012, 2012, 750891. [Google Scholar] [CrossRef]
- Ioele, G.; de Luca, M.; Garofalo, A.; Ragno, G. Photosensitive drugs: A Review on their photoprotection by liposomes and cyclodextrins. Drug Deliv. 2017, 24, 33–44. [Google Scholar] [CrossRef] [Green Version]
- Kaliamurthi, S.; Selvaraj, G.; Hou, L.; Li, Z.; Wei, Y.; Gu, K.; Wei, D. Synergism of essential oils with lipid based nanocarriers: Emerging trends in preservation of grains and related food products. Grain Oil Sci. Technol. 2019, 2, 21–26. [Google Scholar] [CrossRef]
- European Medicines Agency. ICH guideline Q1A(R2) ICH Harmonised Tripartite Guideline, Stability Testing of New Drug Substances and Products; Current Step 4; European Medicines Agency: Amsterdam, The Netherlands, 2003. [Google Scholar]
- Dai, Q.; Xia, Y.; Jiang, L.; Li, W.; Wang, J.; Chen, J. Enhanced degradation of aspirin by electrochemical oxidation with modified PbO2 electrode and hydrogen peroxide. Int. J. Electrochem. Sci. 2012, 7, 12895–12906. [Google Scholar]
- Mukherjee, D.; Ray, A.K.; Barghi, S. Mechanism of acetyl salicylic acid (aspirin) degradation under solar light in presence of a TiO2-polymeric film photocatalyst. Processes 2016, 4, 13. [Google Scholar] [CrossRef]
- Gugulothu, D.B.; Patravale, V.B. A new stability-indicating HPLC method for simultaneous determination of curcumin and celecoxib at single wavelength: An application to nanoparticulate formulation. Pharm. Anal. Acta 2012, 3, 157. [Google Scholar] [CrossRef] [Green Version]
- Kawabata, K.; Sugihara, K.; Sanoh, S.; Kitamura, S.; Ohta, S. Ultraviolet-photoproduct of acetaminophen: Structure determination and evaluation of ecotoxicological effect. J. Photochem. Photobiol. A 2012, 249, 29–35. [Google Scholar] [CrossRef]
- Iovino, P.; Chianese, S.; Canzano, S.; Prisciandaro, M.; Musmarra, D. Ibuprofen photodegradation in aqueous solutions. Environ. Sci. Pollut. Res. 2016, 23, 22993–23004. [Google Scholar] [CrossRef]
- Marotta, R.; Spasiano, D.; di Somma, I.; Andreozzi, R. Photodegradation of naproxen and its photoproducts in aqueous solution at 254 Nm: A kinetic investigation. Water Res. 2013, 47, 373–383. [Google Scholar] [CrossRef] [Green Version]
- Zhang, N.; Li, J.M.; Liu, G.G.; Chen, X.L.; Jiang, K. Photodegradation of diclofenac in aqueous solution by simulated sunlight irradiation: Kinetics, thermodynamics and pathways. Water Sci. Technol. 2017, 75, 2163–2170. [Google Scholar] [CrossRef]
- Szabó, R.K.; Megyeri, C.S.; Illés, E.; Gajda-Schrantz, K.; Mazellier, P.; Dombi, A. Phototransformation of ibuprofen and ketoprofen in aqueous solutions. Chemosphere 2011, 84, 1658–1663. [Google Scholar] [CrossRef]
- Grande, F.; Ragno, G.; Muzzalupo, R.; Occhiuzzi, M.A.; Mazzotta, E.; de Luca, M.; Garofalo, A.; Ioele, G. Gel formulation of nabumetone and a newly synthesized analog: Microemulsion as a photoprotective topical delivery system. Pharmaceutics 2020, 12, 423. [Google Scholar] [CrossRef]
- Nikolic, V.; Ilic-Stojanovic, S.; Nikolic, L.; Cakic, M.; Zdravkovic, A.; Kapor, A.; Popsavin, M. Photostability of piroxicam in the inclusion complex with 2-hydroxypropyl-β-cyclodextrin. Hem. Ind. 2014, 68, 107–116. [Google Scholar] [CrossRef] [Green Version]
- Mishra, D.K.; Shandilya, R.; Mishra, P.K. Lipid based nanocarriers: A translational perspective. Nanomedicine 2018, 14, 2023–2050. [Google Scholar] [CrossRef]
- Alvarez-Malmagro, J.; Jablonowska, E.; Nazaruk, E.; Szwedziak, P.; Bilewicz, R. How do lipid nanocarriers—Cubosomes affect electrochemical properties of DMPC bilayers deposited on gold (111) electrodes? Bioelectrochemistry 2020, 134, 103208. [Google Scholar] [CrossRef]
- Sala, M.; Diab, R.; Elaissari, A.; Fessi, H. Lipid nanocarriers as skin drug delivery systems: Properties, mechanisms of skin interactions and medical applications. Int. J. Pharm. 2018, 535, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Anita, C.; Munira, M.; Mural, Q.; Shaily, L. Topical nanocarriers for management of rheumatoid arthritis: A review. Biomed. Pharmacother. 2021, 141, 111880. [Google Scholar] [CrossRef] [PubMed]
- Puglia, C.; Trombetta, D.; Venuti, V.; Saija, A.; Bonina, F. Evaluation of in-vivo topical anti-inflammatory activity of indometacin from liposomal vesicles. J. Pharm. Pharmacol. 2010, 56, 1225–1232. [Google Scholar] [CrossRef] [PubMed]
- Yasmin Begum, M.; Abbulu, K.; Sudhakar, M. Celecoxib loaded liposomes: Development, characterization and in vitro evaluation. Int. J. Pharm. Sci. Res. 2012, 3, 154. [Google Scholar]
- Ravalika, V.; Sailaja, A.K. Formulation and evaluation of etoricoxib niosomes by thin film hydration technique and ether injection method. Nano Biomed. Eng. 2017, 9, 242–248. [Google Scholar] [CrossRef] [Green Version]
- Subashini Rajaram, A.S.; Dharmalingam, S.R.; Chidambaram, K. Fabrication of non-ionic surfactant vesicular gel for effective treatment of rheumatoid arthritis. J. Evol. Med. Dent. Sci. 2020, 9, 2289–2296. [Google Scholar] [CrossRef]
- Mishra, R.K.; Ahmad, A.; Kumar, A.; Vyawahare, A.; Raza, S.S.; Khan, R. Lipid-based nanocarrier-mediated targeted delivery of celecoxib attenuate severity of ulcerative colitis. Mater. Sci. Eng. C 2020, 116, 111103. [Google Scholar] [CrossRef]
- Jain, S.K.; Chourasia, M.K.; Masuriha, R.; Soni, V.; Jain, A.; Jain, N.K.; Gupta, Y. Solid lipid nanoparticles bearing flurbiprofen for transdermal delivery. Drug Deliv. 2005, 12, 207–215. [Google Scholar] [CrossRef] [Green Version]
- Chantaburanan, T.; Teeranachaideekul, V.; Chantasart, D.; Jintapattanakit, A.; Junyaprasert, V.B. Effect of binary solid lipid matrix of wax and triglyceride on lipid crystallinity, drug-lipid interaction and drug release of ibuprofen-loaded solid lipid nanoparticles (SLN) for dermal delivery. J. Colloid Interface Sci. 2017, 504, 247–256. [Google Scholar] [CrossRef]
- Mohammadi-Samani, S.; Zojaji, S.; Entezar-Almahdi, E. Piroxicam loaded solid lipid nanoparticles for topical delivery: Preparation, characterization and in vitro permeation assessment. J. Drug Deliv. Sci. Technol. 2018, 47, 427–433. [Google Scholar] [CrossRef]
- Ioele, G.; Tavano, L.; Muzzalupo, R.; de Luca, M.; Ragno, G. Stability-indicating methods for nsaids in topical formulations and photoprotection in host-guest matrices. Mini-Rev. Med. Chem. 2016, 16, 676–682. [Google Scholar] [CrossRef] [PubMed]
- Ioele, G.; Tavano, L.; Luca, M.D.; Muzzalupo, R.; Mancuso, A.; Ragno, G. Light-sensitive drugs in topical formulations: Stability indicating methods and photostabilization strategies. Future Med. Chem. 2017, 9, 1795–1808. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, L.M.; Sari, M.H.M.; Cervi, V.F.; Gehrcke, M.; Barbieri, A.V.; Zborowski, V.A.; Beck, R.C.R.; Nogueira, C.W.; Cruz, L. Pomegranate seed oil nanoemulsions improve the photostability and in vivo antinociceptive effect of a non-steroidal anti-inflammatory drug. Colloids Surf. B 2016, 144, 214–221. [Google Scholar] [CrossRef] [PubMed]
- Maestrelli, F.; González-Rodríguez, M.L.; Rabasco, A.M.; Mura, P. Effect of preparation technique on the properties of liposomes encapsulating ketoprofen-cyclodextrin complexes aimed for transdermal delivery. Int. J. Pharm. 2006, 312, R713–R715. [Google Scholar] [CrossRef]
- Tsukamoto, T.; Hironaka, K.; Fujisawa, T.; Yamaguchi, D.; Tahara, K.; Tozuka, Y.; Takeuchi, H. Preparation of bromfenac-loaded liposomes modified with chitosan for ophthalmic drug delivery and evaluation of physicochemical properties and drug release profile. Asian J. Pharm. Sci. 2013, 8, 104–109. [Google Scholar] [CrossRef] [Green Version]
- Tavano, L.; de Cindio, B.; Picci, N.; Ioele, G.; Muzzalupo, R. Drug Compartmentalization as strategy to improve the physico-chemical properties of diclofenac sodium loaded niosomes for topical applications. Biomed. Microdevices 2014, 16, 504–518. [Google Scholar] [CrossRef] [PubMed]
- Balguri, S.P.; Adelli, G.R.; Majumdar, S. Topical ophthalmic lipid nanoparticle formulations (SLN, NLC) of indomethacin for delivery to the posterior segment ocular tissues. Eur. J. Pharm. Biopharm. 2016, 109, 224–235. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dave, V.; Gupta, A.; Singh, P.; Gupta, C.; Sadhu, V.; Reddy, K.R. Synthesis and characterization of celecoxib loaded PEGylated liposome nanoparticles for biomedical applications. Nano Struct. Nano Objects 2019, 18, 100288. [Google Scholar] [CrossRef]
- Lichtenberger, L.M.; Zhou, Y.; Jayaraman, V.; Doyen, J.R.; O’Neil, R.G.; Dial, E.J.; Volk, D.E.; Gorenstein, D.G.; Boggara, M.B.; Krishnamoorti, R. Insight into NSAID-induced membrane alterations, pathogenesis and therapeutics: Characterization of interaction of NSAIDs with phosphatidylcholine. Biochim. Biophys. Acta Mol. Cell. Biol. Lipids 2012, 1821, 994–1002. [Google Scholar] [CrossRef] [Green Version]
- Ioele, G.; de Luca, M.; Ragno, G. Photostability of barnidipine in combined cyclodextrin-in-liposome matrices. Future Med. Chem. 2014, 6, 35–43. [Google Scholar] [CrossRef]
- Wang, W.X.; Feng, S.S.; Zheng, C.H. A comparison between conventional liposome and drug-cyclodextrin complex in liposome system. Int. J. Pharm. 2016, 513, 387–392. [Google Scholar] [CrossRef]
- Masjedi, M.; Montahaei, T. An illustrated review on nonionic surfactant vesicles (niosomes) as an approach in modern drug delivery: Fabrication, characterization, pharmaceutical, and cosmetic applications. J. Drug Deliv. Sci. Technol. 2021, 61, 102234. [Google Scholar] [CrossRef]
- Puglia, C.; Bonina, F.; Rizza, L.; Blasi, P.; Schoubben, A.; Perrotta, R.; Tarico, M.S.; Damiani, E. Lipid nanoparticles as carrier for octyl-methoxycinnamate: In vitro percutaneous absorption and photostability studies. J. Pharm. Sci. 2012, 101, 301–311. [Google Scholar] [CrossRef]
- Puglia, C.; Damiani, E.; Offerta, A.; Rizza, L.; Tirendi, G.G.; Tarico, M.S.; Curreri, S.; Bonina, F.; Perrotta, R.E. Evaluation of nanostructured lipid carriers (NLC) and nanoemulsions as carriers for UV-filters: Characterization, in vitro penetration and photostability studies. Eur. J. Pharm. Sci. 2014, 51, 211–217. [Google Scholar] [CrossRef] [PubMed]

| Drug Class | Drug | Pharmaceutical Formulation | Determination Method | References |
|---|---|---|---|---|
| Salicylates | Aspirin | Aqueous solution | LC/MS | [28] |
| Solid state | FTIR | [28] | ||
| Aqueous solution | GC/MS | [27] | ||
| Propionic acid derivatives | Ibuprofen | Aqueous solution | GC-MS | [31] |
| Naproxen | Aqueous solution | HPLC-DAD | [32] | |
| Ketoprofen | Aqueous solution | HPLC-DAD | [8] | |
| Aqueous solution | HPLC-MS | [34] | ||
| Acetic acid derivatives | Diclofenac | Gel formulation | UV-Vis/MCR | [7,16,33] |
| Aqueous solution | HPLC/MS | [33] | ||
| Nabumetone | Gel formulation | UV-Vis and MCR | [35] | |
| Aniline derivatives | Paracetamol | Aqueous solution | HPLC 7/ESI/TOF/MS/MS | [30] |
| Enolic acid derivatives | Piroxicam | Methanol solution | FTIR | [36] |
| Selective COX-2 inhibitors | Etoricoxib | Aqueous solution | UV-Vis | [10] |
| Celecoxib | Methanol solution | HPLC-DAD | [29] |
| Drug | Pharmaceutical Formulation | Photo-Protective System | References |
|---|---|---|---|
| Ibuprofen | Aqueous solution | Ascorbic acid as UV absorber | [20] |
| Aqueous solution | Methyl-β-cyclodextrins | [49,50] | |
| Naproxen | Aqueous solution | Methyl-β-cyclodextrins | [49,50] |
| Ketoprofen | Gel | Methoxy dibenzoylmethane as UV absorber | [19] |
| Aqueous solution | Ascorbic acid as UV absorber | [20] | |
| Emulsion | Nanoemulsion | [51] | |
| Aqueous solution | β-cyclodextrin and hydroxypropyl-βcyclodextrin in liposomes | [52] | |
| Bromfenac | Aqueous solution | Liposomes with chitosan | [53] |
| Diclofenac | Gel | Octisilate and/or octyl methoxycinnamate as UV absorbers | [7] |
| Aqueous solution | Methyl-β-cyclodextrins | [7,49,50] | |
| Gel | Niosomes | [16,54] | |
| Gel | Niosomes and 5% ascorbic acid | [16,54] | |
| Nabumetone | Gel | Microemulsion | [35] |
| Paracetamol | Aqueous solution | Ascorbic acid as UV absorber | [20] |
| Piroxicam | Aqueous solution | 2-hydroxypropyl-cyclodextrin | [36] |
| Indomethacin | Aqueous solution | SLNs | [55] |
| Aqueous solution | NLCs | [55] | |
| Celecoxib | Aqueous solution | PEGylated liposomes | [56] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ioele, G.; Grande, F.; De Luca, M.; Occhiuzzi, M.A.; Garofalo, A.; Ragno, G. Photodegradation of Anti-Inflammatory Drugs: Stability Tests and Lipid Nanocarriers for Their Photoprotection. Molecules 2021, 26, 5989. https://doi.org/10.3390/molecules26195989
Ioele G, Grande F, De Luca M, Occhiuzzi MA, Garofalo A, Ragno G. Photodegradation of Anti-Inflammatory Drugs: Stability Tests and Lipid Nanocarriers for Their Photoprotection. Molecules. 2021; 26(19):5989. https://doi.org/10.3390/molecules26195989
Chicago/Turabian StyleIoele, Giuseppina, Fedora Grande, Michele De Luca, Maria Antonietta Occhiuzzi, Antonio Garofalo, and Gaetano Ragno. 2021. "Photodegradation of Anti-Inflammatory Drugs: Stability Tests and Lipid Nanocarriers for Their Photoprotection" Molecules 26, no. 19: 5989. https://doi.org/10.3390/molecules26195989
APA StyleIoele, G., Grande, F., De Luca, M., Occhiuzzi, M. A., Garofalo, A., & Ragno, G. (2021). Photodegradation of Anti-Inflammatory Drugs: Stability Tests and Lipid Nanocarriers for Their Photoprotection. Molecules, 26(19), 5989. https://doi.org/10.3390/molecules26195989