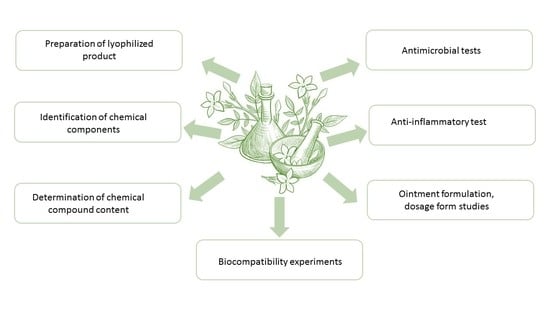
Topical Dosage Formulation of Lyophilized Philadelphus coronarius L. Leaf and Flower: Antimicrobial, Antioxidant and Anti-Inflammatory Assessment of the Plant
Abstract
:1. Introduction
2. Results
2.1. Bioactive Content
2.2. Antioxidant Activity of Philadelphus coronarius, Total Polyphenol and Flavonoid Content
2.3. In Vitro Microdilution
2.4. In Vitro Time-Kill Antimicrobial Test
2.5. Investigation of IL-4 Level, Enzyme-Linked Immunosorbent Assay (ELISA)
2.6. Ointment Formulation
2.7. In Vitro Release
2.8. Results of Texture-Analysis Studies
2.9. MTT Test
3. Discussion
4. Materials and Methods
4.1. Materials
4.2. Preparation of Lyophilized Products
4.3. Physicochemical Characterisation by HPLC-PDA Method
4.4. Phytochemical Investigation of the Lyophilized Extract
4.5. Evaluation of Antioxidant Activity
4.5.1. Evaluation of Antioxidant Activity by DPPH
4.5.2. Evaluation of Antioxidant Activity by FRAP Method (Ferric-Reducing Antioxidant Power)
4.5.3. Evaluation of Antioxidant Activity by CUPRAC Assay
4.5.4. Evaluation of Antioxidant Activity by ABTS Assay
4.6. Antimicrobial Testing by Microdilution Method
4.7. In Vitro Time-Kill Antimicrobial Tests
4.8. Investigation of IL-4, Enzyme-Linked Immunosorbent Assay (ELISA)
4.9. Formulation of Ointments
4.10. In Vitro Release
| Model | Equations [46,47] | Graphic | |
|---|---|---|---|
| Zero-order | (5) | The graphic of the drug-dissolved fraction versus time is linear. | |
| First-order | (6) | The graphic of the decimal logarithm of the released amount of drug versus time is linear. | |
4.11. Biocompatibility Experiments
4.12. Texture-Analysis Experiments
4.13. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ekor, M. The growing use of herbal medicines: Issues relating to adverse reactions and challenges in monitoring safety. Front. Neurol. 2014, 4, 1–10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ali, K.; Majlesi, M.; Rafieian-Kopaei, M. Herbal versus synthetic drugs; beliefs and facts. J. Nephropharmacol. 2015, 4, 27–30. [Google Scholar]
- Hufford, L. Hydrangeaceae; Springer: Berlin/Heidelberg, Germany, 2004; Volume 38, pp. 202–215. [Google Scholar] [CrossRef]
- Myung, D.-B.; Lee, J.-H.; Han, H.-S.; Lee, K.-Y.; Ahn, H.S.; Shin, Y.-K.; Song, E.; Kim, B.-H.; Lee, K.H.; Lee, S.H.; et al. Oral Intake of Hydrangea serrata (Thunb.) Ser. Leaves Extract Improves Wrinkles, Hydration, Elasticity, Texture, and Roughness in Human Skin: A Randomized, Double-Blind, Placebo-Controlled Study. Nutrients 2020, 12, 1588. [Google Scholar] [CrossRef] [PubMed]
- Shi, J.; Li, C.J.; Yang, J.Z.; Ma, J.; Li, Y.; Chen, H.; Zhang, D.M. Monoterpenes from the leaves of Hydrangea paniculata and their hepatoprotective activities. J. Asian Nat. Prod. Res. 2015, 17, 512–518. [Google Scholar] [CrossRef]
- Nakamura, S.; Matsuda, H.; Yoshikawa, M. Search for antidiabetic constituents of medicinal food. Yakugaku Zasshi 2011, 131, 909–915. [Google Scholar] [CrossRef] [Green Version]
- Klecáková, J.; Chobot, V.; Jahodár, L.; Laakso, I.; Víchová, P. Antiradical activity of petals of Philadelphus coronarius L. Cent. Eur. J. Public Health 2004, 12, S39–S40. [Google Scholar]
- Egészségtér, H. A Jezsámennek (Phyladelphus coronarius) Nyár Elején Nyílnak Krémfehér Virágai, Intenzív Illatot Árasztva. Ne tévesszük Össze az Általában Kisebb Termetű és Csak Igen Ritkán Látható Valódi Jázminnal. Available online: https://egeszsegter.hu/cikk/1453/a-jezsamen-nem-jazmin#gsc.tab=0 (accessed on 2 February 2022).
- Nokhodchi, A.; Shokri, J.; Dashbolaghi, A.; Hassan-Zadeh, D.; Ghafourian, T.; Barzegar-Jalali, M. The Enhancement Effect of Surfactants on the Penetration of Lorazepam through Rat Skin. Int. J. Pharm. 2003, 250, 359–369. [Google Scholar] [CrossRef]
- Hagen, M.; Baker, M. Skin penetration and tissue permeation after topical administration of diclofenac. Curr. Med. Res. Opin. 2017, 33, 1623–1634. [Google Scholar] [CrossRef] [Green Version]
- Pető, Á.; Kósa, D.; Haimhoffer, Á.; Fehér, P.; Ujhelyi, Z.; Sinka, D.; Fenyvesi, F.; Váradi, J.; Vecsernyés, M.; Gyöngyösi, A.; et al. Nicotinic Amidoxime Derivate BGP-15, Topical Dosage Formulation and Anti-Inflammatory Effect. Pharmaceutics 2021, 13, 2037. [Google Scholar] [CrossRef]
- Som, I.; Bhatia, K.; Yasir, M. Status of surfactants as penetration enhancers in transdermal drug delivery. J. Pharm. Bioallied Sci. 2012, 4, 2–9. [Google Scholar] [CrossRef]
- Korhonen, O.; Pajula, K.; Laitinen, R. Rational excipient selection for co-amorphous formulations. Expert Opin. Drug Deliv. 2017, 14, 551–569. [Google Scholar] [CrossRef] [PubMed]
- Valko, V.; Fickova, M.; Pravdova, E.; Nagy, M.; Grancai, D.; Czigle, S. Cytotoxicity of water extracts from leaves and branches of Philadelphus coronarius L. Biomed. Pap. Med. Fac. Univ. Palacky. Olomouc. Czech. Repub. 2006, 150, 71–73. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dilshara, M.G.; Jayasooriya, R.G.P.T.; Lee, S.; Jeong, J.B.; Seo, Y.T.; Choi, Y.H.; Jeong, J.W.; Jang, Y.P.; Jeong, Y.K.; Kim, G.Y. Water extract of processed Hydrangea macrophylla (Thunb.) Ser. leaf attenuates the expression of pro-inflammatory mediators by suppressing Akt-mediated NF-κB activation. Environ. Toxicol. Pharmacol. 2013, 35, 311–319. [Google Scholar] [CrossRef] [PubMed]
- Nagy, M.; Grancai, D.; Jantova, S.; Ruzekova, L. Antibacterial Activity of Plant Extracts from the Families Fabaceae, Oleaceae, Philadelphaceae, Rosaceae and Staphyleaceae. Phyther. Res. 2000, 14, 601–603. [Google Scholar]
- Hano, C.; Tungmunnithum, D. Plant Polyphenols, More than Just Simple Natural Antioxidants: Oxidative Stress, Aging and Age-Related Diseases. Medicines 2020, 7, 26. [Google Scholar] [CrossRef]
- Pandey, K.B.; Rizvi, S.I. Plant polyphenols as dietary antioxidants in human health and disease. Oxid. Med. Cell. Longev. 2009, 2, 270–278. [Google Scholar] [CrossRef] [Green Version]
- Pietta, P.G. Flavonoids as antioxidants. J. Nat. Prod. 2000, 63, 1035–1042. [Google Scholar] [CrossRef]
- Panche, A.N.; Diwan, A.D.; Chandra, S.R. Flavonoids: An overview. J. Nutr. Sci. 2016, 5, 47. [Google Scholar] [CrossRef] [Green Version]
- Choubey, S.; Goyal, S.; Varughese, L.R.; Kumar, V.; Sharma, A.K.; Beniwal, V. Probing Gallic Acid for Its Broad Spectrum Applications. Mini-Reviews Med. Chem. 2018, 18, 1283–1293. [Google Scholar] [CrossRef]
- de Cristo Soares Alves, A.; Mainardes, R.M.; Khalil, N.M. Nanoencapsulation of gallic acid and evaluation of its cytotoxicity and antioxidant activity. Mater. Sci. Eng. C 2016, 60, 126–134. [Google Scholar] [CrossRef]
- Xu, D.; Hu, M.-J.; Wang, Y.-Q.; Cui, Y.-L. Antioxidant Activities of Quercetin and Its Complexes for Medicinal Application. Molecules 2019, 24, 1123. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Song, X.; Wang, Y.; Gao, L. Mechanism of antioxidant properties of quercetin and quercetin-DNA complex. J. Mol. Model. 2020, 26, 133. [Google Scholar] [CrossRef] [PubMed]
- Cazón, P.; Antoniewska, A.; Rutkowska, J.; Vázquez, M. Evaluation of easy-removing antioxidant films of chitosan with Melaleuca alternifolia essential oil. Int. J. Biol. Macromol. 2021, 186, 365–376. [Google Scholar] [CrossRef]
- Bener, M.; Şen, F.B.; Apak, R. Heparin-stabilized gold nanoparticles-based CUPRAC colorimetric sensor for antioxidant capacity measurement. Talanta 2018, 187, 148–155. [Google Scholar] [CrossRef] [PubMed]
- Kalasz, H.; Antal, I. Drug Excipients. Curr. Med. Chem. 2006, 13, 2535–2563. [Google Scholar] [CrossRef] [PubMed]
- López-Lluch, G.; del Pozo-Cruz, J.; Sánchez-Cuesta, A.; Cortés-Rodríguez, A.B.; Navas, P. Bioavailability of coenzyme Q10 supplements depends on carrier lipids and solubilization. Nutrition 2019, 57, 133–140. [Google Scholar] [CrossRef]
- Csizmazia, E.; Eros, G.; Berkesi, O.; Berkó, S.; Szabó-Révész, P.; Csányi, E. Penetration enhancer effect of sucrose laurate and Transcutol on ibuprofen. J. Drug Deliv. Sci. Technol. 2011, 21, 411–415. [Google Scholar] [CrossRef]
- Abd-Elsalam, W.H.; Nagy, Y.I.; Abouelatta, S.M. Tailoring thixotropic mixed-lipid nanoconstructs of voriconazole for the management of Vulvovaginal candidiasis: Formulation, statistical optimization, in vitro characterization and in vivo assessment. Drug Deliv. 2021, 28, 1877–1889. [Google Scholar] [CrossRef]
- Morris, L.S.; Schulz, R.M. Patient compliance—An overview. J. Clin. Pharm. Ther. 1992, 17, 283–295. [Google Scholar] [CrossRef]
- Thatai, P.; Khan, A.B. Management of nail psoriasis by topical drug delivery: A pharmaceutical perspective. Int. J. Dermatol. 2020, 59, 915–925. [Google Scholar] [CrossRef]
- Jurca, T.; Marian, E.; Tita, B.; Vicas, S.; Pallag, A.; Toth, I.; Krusper, L.; Braun, M.; Vicas, L. Determination of oligoelements content of plant material and assessment of bioactive compounds from calendula officinalis lyophilized extract. Rev. Chim. 2017, 68, 1786–1789. [Google Scholar] [CrossRef]
- Mensor, L.L.; Menezes, F.S.; Leitão, G.G.; Reis, A.S.; dos Santos, T.C.; Coube, C.S.; Leitão, S.G. Screening of Brazilian plant extracts for antioxidant activity by the use of DPPH free radical method. Phyther. Res. 2001, 15, 127–130. [Google Scholar] [CrossRef] [PubMed]
- Vicaş, L.; Teuşdea, A.; Vicaş, S.; Marian, E.; Tunde, J.; Mureşan, M.; Gligor, F. Assessment of antioxidant capacity of some extracts for further use in therapy. Farmacia 2015, 63, 267–274. [Google Scholar]
- Dżugan, M.; Tomczyk, M.; Sowa, P.; Grabek-Lejko, D. Antioxidant Activity as Biomarker of Honey Variety. Molecules 2018, 23, 2069. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Campos, C.; Guzmán, R.; López-Fernández, E.; Casado, Á. Evaluation of the copper(II) reduction assay using bathocuproinedisulfonic acid disodium salt for the total antioxidant capacity assessment: The CUPRAC–BCS assay. Anal. Biochem. 2009, 392, 37–44. [Google Scholar] [CrossRef]
- Re, R.; Pellegrini, N.; Proteggente, A.; Pannala, A.; Yang, M.; Rice-Evans, C. Antioxidant activity applying an improved ABTS radical cation decolorization assay. Free Radic. Biol. Med. 1999, 26, 1231–1237. [Google Scholar] [CrossRef]
- Nemes, D.; Kovács, R.; Nagy, F.; Mező, M.; Poczok, N.; Ujhelyi, Z.; Pető, Á.; Fehér, P.; Fenyvesi, F.; Váradi, J.; et al. Interaction between different pharmaceutical excipients in liquid dosage forms—Assessment of cytotoxicity and antimicrobial activity. Molecules 2018, 23, 1827. [Google Scholar] [CrossRef] [Green Version]
- Nemes, D.; Kovács, R.; Nagy, F.; Tóth, Z.; Herczegh, P.; Borbás, A.; Kelemen, V.; Pfliegler, W.P.; Rebenku, I.; Hajdu, P.B.; et al. Comparative biocompatibility and antimicrobial studies of sorbic acid derivates. Eur. J. Pharm. Sci. 2020, 143, 105162. [Google Scholar] [CrossRef]
- Tavakolpour, S.; Tavakolpour, V. Interleukin 4 inhibition as a potential therapeutic in pemphigus. Cytokine 2016, 77, 189–195. [Google Scholar] [CrossRef]
- Qiu, Y.Y.; Zhu, J.X.; Bian, T.; Gao, F.; Qian, X.F.; Du, Q.; Yuan, M.Y.; Sun, H.; Shi, L.Z.; Yu, M.H. Protective effects of astragaloside IV against ovalbumin-induced lung inflammation are regulated/mediated by T-bet/GATA-3. Pharmacology 2014, 94, 51–59. [Google Scholar] [CrossRef]
- Fehér, P.; Ujhelyi, Z.; Váradi, J.; Fenyvesi, F.; Róka, E.; Juhász, B.; Varga, B.; Bombicz, M.; Priksz, D.; Bácskay, I.; et al. Efficacy of pre- and post-treatment by topical formulations containing dissolved and suspended Silybum marianum against UVB-induced oxidative stress in guinea pig and on HaCaT keratinocytes. Molecules 2016, 21, 1269. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Suarato, G.; Spanò, R.; Bertorelli, R.; Diaspro, A.; Athanassiou, A.; Surdo, S. 3D-Printed, Pocket-Size Diffusion Cells for Skin Permeation Investigation. Proceedings 2018, 2, 945. [Google Scholar] [CrossRef] [Green Version]
- Franz, T.J. Percutaneous Absorption. on the Relevance of In Vitro Data. J. Investig. Dermatol. 1975, 64, 190–195. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Samaha, D.; Shehayeb, R.; Kyriacos, S. Modeling and comparison of dissolution profiles of diltiazem modified-release formulations. Dissolution Technol. 2009, 16, 41–46. [Google Scholar] [CrossRef]
- Dash, S.; Murthy, P.N.; Nath, L.; Chowdhury, P. Kinetic modeling on drug release from controlled drug delivery systems. Acta Pol. Pharm. Drug Res. 2010, 67, 217–223. [Google Scholar]
- Costa, P. José Manuel Sousa Lobo Modeling and comparison of dissolution profiles. Eur. J. Pharm. Sci. 2001, 13, 123–133. [Google Scholar] [CrossRef]
- Kumar, P.; Nagarajan, A.; Uchil, P.D. Analysis of Cell Viability by the MTT Assay. Cold Spring Harb. Protoc. 2018, 6, 469–471. [Google Scholar] [CrossRef]
- Ujhelyi, Z.; Fenyvesi, F.; Váradi, J.; Fehér, P.; Kiss, T.; Veszelka, S.; Deli, M.; Vecsernyés, M.; Bácskay, I. Evaluation of cytotoxicity of surfactants used in self-micro emulsifying drug delivery systems and their effects on paracellular transport in Caco-2 cell monolayer. Eur. J. Pharm. Sci. 2012, 47, 564–573. [Google Scholar] [CrossRef]
- Kovács, R.; Tóth, Z.; Locke, J.B.; Forgács, L.; Kardos, G.; Nagy, F.; Borman, A.M.; Majoros, L. Comparison of In Vitro Killing Activity of Rezafungin, Anidulafungin, Caspofungin, and Micafungin against Four Candida auris Clades in RPMI-1640 in the Absence and Presence of Human Serum. Microorganisms 2021, 9, 863. [Google Scholar] [CrossRef]






| P. coronarius Leaf | Bioactive Compound Content (Mg Compound/100 mg) ± SD |
|---|---|
| 7-methoxycoumarin | 0.2061 ± 0.032 |
| Chlorogenic acid | 0.0128 ± 0.0097 |
| Caffeic acid | 0.0740 ± 0.0033 |
| Delphinidin 3-rutinoside chloride | 0.3354 ± 0.047 |
| Hyperoside | 0.0514 ± 0.0071 |
| Luteolin 7-glucoside | 0.2528 ± 0.056 |
| Rutin | 0.0941 ± 0.0045 |
| T-resveratrol | 0.0602 ± 0.0026 |
| P. coronarius Flower | Bioactive-Compound Content (Mg Compound/100 mg) ± SD |
|---|---|
| 7-methoxycoumarin | 1.6725 ± 0.372 |
| Chlorogenic acid | 0.2485 ± 0.098 |
| Ferulic acid | 0.1094 ± 0.020 |
| Gallic acid | 0.1375 ± 0.034 |
| Rosmarinic acid | 0.7674 ± 0.112 |
| Trans p-coumaric acid | 0.4387 ± 0.079 |
| Bergapten | 2.8370 ± 0.432 |
| Caffeic acid | 1.8407 ± 0.087 |
| Delphinidin 3-rutinoside chloride | 1.7928 ± 0.201 |
| Diosmin | 1.1125 ± 0.386 |
| Hyperoside | 0.2428 ± 0.042 |
| Isopimpinellin | 0.4678 ± 0.016 |
| Luteolin 7-glucoside | 0.0585 ± 0.0093 |
| Myricetin | 0.0645 ±0.0021 |
| Quercetin | 0.1449 ± 0.034 |
| Rutin | 0.4077 ± 0.015 |
| T-resveratrol | 0.5262 ± 0.027 |
| P. coronarius Leaf | P. coronarius Flower | |
|---|---|---|
| DPPH (%) | 86.63 ± 6.49 | 92.24 ± 10.09 |
| ABTS (mmol TE/g DW) | 18.37 ± 4.73 | 40.54 ± 9.77 * |
| FRAP (μmol TE/g) | 77.97 ± 46.01 | 164.62 ± 52.75 |
| Cuprac (μmol TE/mL) | 222.42 ± 21.04 | 423.35 ± 71.07 ** |
| P. coronarius Leaf | P. coronarius Flower | |
|---|---|---|
| Polyphenols (mg GAE/100 g) | 59.31 ± 4.36 | 54.83 ± 9.74 |
| Flavonoids (mg QE/100 g) | 1.97 ± 1.49 | 1.91 ± 0.82 |
| Inhibition of Microbial Strains by P. coronarius Flower or Leaf Measured with Microdilution Method at 5% Concentration ± SD | ||||
|---|---|---|---|---|
| C. albicans | S. aureus | E. coli | P. aeruginosa | |
| P. coronarius flower | no inhibition | no inhibition | 46.4% ±3.4% | no inhibition |
| P. coronarius leaf | no inhibition | 68.6% ±5.6% | 41.5% ±2.7% | no inhibition |
| Abbreviation | Leaf or Flower | Emulsifier | |
|---|---|---|---|
| Composition 1. | CMP 1 | leaf | SP70 |
| Composition 2. | CMP 2 | leaf | Tefose 63 |
| Composition 3. | CMP 3 | leaf | Sedefos 75 |
| Composition 4. | CMP 4 | flower | SP70 |
| Composition 5. | CMP 5 | flower | Tefose 63 |
| Composition 6. | CMP 6 | flower | Sedefos 75 |
| Kinetic Model | ||
|---|---|---|
| Composition | Zero | First |
| CMP 1 | 0.03 | 0.37 |
| CMP 2 | 0.14 | 0.44 |
| CMP 3 | 0.59 | 0.70 |
| CMP 4 | 0.58 | 0.71 |
| CMP 5 | 0.65 | 0.75 |
| CMP 6 | 0.392 | 0.384 |
| Composition | Release Rate (k) (μg/cm2 × √min) | Diffusion Coefficient (D × 10−7; cm2/min) |
|---|---|---|
| CMP 1 | 7.47 | 3.30 |
| CMP 2 | 8.05 | 3.97 |
| CMP 3 | 5.31 | 2.36 |
| CMP 4 | 7.45 | 4.32 |
| CMP 5 | 6.57 | 3.97 |
| CMP 6 | 5.29 | 1.40 |
| Composition | f1 |
|---|---|
| CMP 1 vs. CMP 2 | 6.87 |
| CMP 1 vs. CMP 3 | 31.40 |
| CMP 1 vs. CMP 4 | 2.98 |
| CMP 1 vs. CMP 5 | 14.44 |
| CMP 1 vs. CMP 6 | 24.02 |
| CMP 2 vs. CMP 3 | 36.11 |
| CMP 2 vs. CMP 4 | 9.65 |
| CMP 2 vs. CMP 5 | 20.32 |
| CMP 2 vs. CMP 6 | 29.24 |
| CMP 3 vs. CMP 4 | 29.29 |
| CMP 3 vs. CMP 5 | 24.71 |
| CMP 3 vs. CMP 6 | 9.71 |
| CMP 4 vs. CMP 5 | 11.81 |
| CMP 4 vs. CMP 6 | 21.68 |
| CMP 5 vs. CMP 6 | 11.19 |
| CMP 1 | CMP 2 | CMP 3 | CMP 4 | CMP 5 | CMP6 | |
|---|---|---|---|---|---|---|
| Transcutol | + | + | + | + | + | + |
| SP70 Tefose 63 Sedefos 75 | + | − | − | + | − | − |
| − | + | − | − | + | − | |
| − | − | + | − | − | + | |
| P. coronarius leaf P. coronarius flower | + | + | + | − | − | − |
| − | − | − | + | + | + | |
| Cetostearyl alcohol Stearic acid Glycerol IPM | + | + | + | + | + | + |
| + | + | + | + | + | + | |
| + | + | + | + | + | + | |
| + | + | + | + | + | + | |
| Propylene glycol Purified water | + | + | + | + | + | + |
| + | + | + | + | + | + |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pető, Á.; Kósa, D.; Haimhoffer, Á.; Nemes, D.; Fehér, P.; Ujhelyi, Z.; Vecsernyés, M.; Váradi, J.; Fenyvesi, F.; Frum, A.; et al. Topical Dosage Formulation of Lyophilized Philadelphus coronarius L. Leaf and Flower: Antimicrobial, Antioxidant and Anti-Inflammatory Assessment of the Plant. Molecules 2022, 27, 2652. https://doi.org/10.3390/molecules27092652
Pető Á, Kósa D, Haimhoffer Á, Nemes D, Fehér P, Ujhelyi Z, Vecsernyés M, Váradi J, Fenyvesi F, Frum A, et al. Topical Dosage Formulation of Lyophilized Philadelphus coronarius L. Leaf and Flower: Antimicrobial, Antioxidant and Anti-Inflammatory Assessment of the Plant. Molecules. 2022; 27(9):2652. https://doi.org/10.3390/molecules27092652
Chicago/Turabian StylePető, Ágota, Dóra Kósa, Ádám Haimhoffer, Dániel Nemes, Pálma Fehér, Zoltán Ujhelyi, Miklós Vecsernyés, Judit Váradi, Ferenc Fenyvesi, Adina Frum, and et al. 2022. "Topical Dosage Formulation of Lyophilized Philadelphus coronarius L. Leaf and Flower: Antimicrobial, Antioxidant and Anti-Inflammatory Assessment of the Plant" Molecules 27, no. 9: 2652. https://doi.org/10.3390/molecules27092652
APA StylePető, Á., Kósa, D., Haimhoffer, Á., Nemes, D., Fehér, P., Ujhelyi, Z., Vecsernyés, M., Váradi, J., Fenyvesi, F., Frum, A., Gligor, F. G., Vicaș, L. G., Marian, E., Jurca, T., Pallag, A., Muresan, M. E., Tóth, Z., & Bácskay, I. (2022). Topical Dosage Formulation of Lyophilized Philadelphus coronarius L. Leaf and Flower: Antimicrobial, Antioxidant and Anti-Inflammatory Assessment of the Plant. Molecules, 27(9), 2652. https://doi.org/10.3390/molecules27092652