Low Prostate Concentration of Lycopene Is Associated with Development of Prostate Cancer in Patients with High-Grade Prostatic Intraepithelial Neoplasia
Abstract
:1. Introduction
2. Results and Discussion
3. Experimental Section
3.1. Patients and Study Design
3.2. Determination of PSA and Plasma Lycopene
3.3. Determination of Prostate Lycopene
3.4. Statistical Analysis
4. Conclusions
Acknowledgments
Conflicts of Interest
References
- Ozten-Kandaş, N.; Bosland, M.C. Chemoprevention of prostate cancer: Natural compounds, antiandrogens, and antioxidants—In vivo evidence. J. Carcinog 2011, 10, 27. [Google Scholar] [CrossRef]
- Thapa, D.; Ghosh, R. Antioxidants for prostate cancer chemoprevention: Challenges and opportunities. Biochem. Pharmacol 2012, 83, 1319–1330. [Google Scholar]
- Shiota, M.; Yokomizo, A.; Naito, S. Pro-survival and anti-apoptotic properties of androgen receptor signaling by oxidative stress promote treatment resistance in prostate cancer. Endocr. Relat. Cancer 2012, 19, R243–R253. [Google Scholar]
- Krinsky, N.I. The antioxidant and biological properties of the carotenoids. Ann. N.Y. Acad. Sci 1998, 854, 443–447. [Google Scholar]
- Park, Y.O.; Hwang, E.S.; Moon, T.W. The effect of lycopene on cell growth and oxidative DNA damage of Hep3B human hepatoma cells. Biofactors 2005, 23, 129–139. [Google Scholar]
- Ivanov, N.I.; Cowell, S.P.; Brown, P.; Rennie, P.S.; Guns, E.S.; Cox, M.E. Lycopene differentially induces quiescence and apoptosis in androgen-responsive and -independent prostate cancer cell lines. Clin. Nutr 2007, 26, 252–263. [Google Scholar]
- da Soares, N. C.; Teodoro, A.J.; Oliveira, F.L.; Santos, C.A.; Takiya, C.M.; Junior, O.S.; Bianco, M.; Junior, A.P.; Nasciutti, L.E.; Ferreira, L.B.; et al. Influence of lycopene on cell viability, cell cycle, and apoptosis of human prostate cancer and benign hyperplastic cells. Nutr. Cancer 2013, 65, 1076–1085. [Google Scholar]
- Trejo-Solís, C.; Pedraza-Chaverrí, J.; Torres-Ramos, M.; Jiménez-Farfán, D.; Cruz Salgado, A.; Serrano-García, N.; Osorio-Rico, L.; Sotelo, J. Multiple molecular and cellular mechanisms of action of lycopene in cancer inhibition. Evid. Complement Alternat. Med 2013, 2013, 705121. [Google Scholar]
- Hantz, H.L.; Young, L.F.; Martin, K.R. Physiologically attainable concentrations of lycopene induce mitochondrial apoptosis in LNCaP human prostate cancer cells. Exp. Biol. Med 2005, 230, 171–179. [Google Scholar]
- Haseen, F.; Cantwell, M.M.; O’Sullivan, J.M.; Murray, L.J. Is there a benefit from lycopene supplementation in men with prostate cancer? A systematic review. Prostate Cancer Prostatic Dis 2009, 12, 325–332. [Google Scholar]
- Chen, L.; Stacewicz-Sapuntzakis, M.; Duncan, C.; Sharifi, R.; Ghosh, L.; van Breemen, R.; Ashton, D.; Bowen, P.E. Oxidative DNA damage in prostate cancer patients consuming tomato sauce-based entrees as a whole-food intervention. J. Natl. Cancer Inst 2001, 93, 1872–1879. [Google Scholar]
- Bowen, P.; Chen, L.; Stacewicz-Sapuntzakis, M.; Duncan, C.; Sharifi, R.; Ghosh, L.; Kim, H.S.; Christov-Tzelkov, K.; van Breemen, R. Tomato sauce supplementation and prostate cancer: Lycopene accumulation and modulation of biomarkers of carcinogenesis. Exp. Biol. Med. (Maywood) 2002, 227, 886–893. [Google Scholar]
- Ilic, D.; Misso, M. Lycopene for the prevention and treatment of benign prostatic hyperplasia and prostate cancer: A systematic review. Maturitas 2012, 72, 269–276. [Google Scholar]
- Wei, M.Y.; Giovannucci, E.L. Lycopene Tomato products, and prostate cancer incidence: A review and reassessment in the PSA screening era. J. Oncol 2012. [Google Scholar] [CrossRef]
- Taneja, S.S. Drug therapies for eradicating high-grade prostatic intraepithelial neoplasia in the prevention of prostate cancer. Rev. Urol 2005, 7, S19–S29. [Google Scholar]
- Hsing, A.W.; Comstock, G.W.; Abbey, H.; Polk, B.F. Serologic precursor of cancer. Retinol, carotenoids and tocopherol and risk of prostate cancer. J. Natl. Cancer Inst 1990, 82, 941–946. [Google Scholar]
- Gann, P.; Ma, J.; Giovannucci, E.; Willett, W.; Sacks, F.M.; Hennekens, C.H.; Stampfer, M.J. Lower prostate cancer risk in men with elevated plasma lycopene: Results of a prospective analysis. Cancer Res 1999, 59, 1225–1230. [Google Scholar]
- Rao, A.V. Serum and tissue lycopene and biomarkers of oxidation in prostate cancer patients: A case-control study. Nutr. Cancer 1999, 33, 159–164. [Google Scholar]
- Ros, M.M.; Bueno-de-Mesquita, H.B.; Kampman, E.; Aben, K.K.; Büchner, F.L.; Jansen, E.H.; van Gils, C.H.; Egevad, L.; Overvad, K.; Tjønneland, A.; et al. Plasma carotenoids and vitamin C concentrations and risk of urothelial cell carcinoma in the European Prospective Investigation into Cancer and Nutrition. Am. J. Clin. Nutr 2012, 96, 902–910. [Google Scholar]
- Hughes, K.J.; Mayne, S.T.; Blumberg, J.B.; Ribaya-Mercado, J.D.; Johnson, E.J.; Cartmel, B. Plasma carotenoids and biomarkers of oxidative stress in patients with prior head and neck cancer. Biomark Insights 2009, 23, 17–26. [Google Scholar]
- Stahl, W.; Sies, H. Uptake of lycopene and its geometrical isomers is greater from heat-processed than from unprocessed tomato juice in humans. J. Nutr 1992, 122, 2161–2166. [Google Scholar]

| All Subjects (n = 32) | Prostatitis (n = 7) | HGPIN (n = 16) | Prostate Cancer (n = 9) | p | |
|---|---|---|---|---|---|
| Age (years) | 66.22 ± 6.53 | 66.57 ± 7.50 | 64.44 ± 6.67 | 69.50 ± 4.41 | 0.37 |
| PSA (ng/dL) | |||||
| Pre | 8.40 ± 4.85 | 10.26 ± 7.68 | 7.51 ± 2.50 | 8.43 ± 5.36 | 0.99 |
| Post | 7.93 ± 4.77 | 9.6 ± 6.3 | 6.87 ± 2.6 | 8.42 ± 5.67 | 0.86 |
| Plasmatic Lycopene (μmol/L) | |||||
| Pre | 1.17 ± 0.92 | 1.42 ± 1.29 | 1.27 ± 0.89 | 0.68 ± 0.31 | 0.06 |
| Post | 1.38 ± 0.57 | 1.23 ± 0.50 | 1.52 ± 0.65 | 1.26 ± 0.46 | 0.58 |
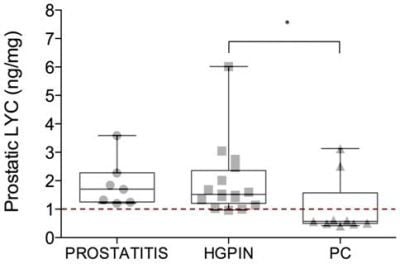
| Prostatic Lycopene (ng/mg) | |||||
| Post | 1.67 ± 1.15 | 1.89 ± 0.84 | 1.94 ± 1.25 | 1.04 ± 1.02 | 0.03 |
| Prostatitis | HGPIN | Prostate Cancer | Total | |
|---|---|---|---|---|
| Prostatic Lycopene < 1 ng/mg | 0 (0%) | 1 (6.3%) | 7 (77.8%) | 8 |
| Prostatic Lycopene > 1 ng/mg | 7 (100%) | 15 (93.7%) | 2 (22.2%) | 24 |
| Total | 7 | 16 | 9 | 32 |
| Chi-Squared p-value | 0.003 | |||
| Sensitivity | 77.8% | |||
| Specificity | 95.6% | |||
| Positive Predictive Value | 87.5% | |||
| Negative Predictive Value | 91.7% |
© 2014 by the authors; licensee MDPI, Basel, Switzerland This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Mariani, S.; Lionetto, L.; Cavallari, M.; Tubaro, A.; Rasio, D.; De Nunzio, C.; Hong, G.M.; Borro, M.; Simmaco, M. Low Prostate Concentration of Lycopene Is Associated with Development of Prostate Cancer in Patients with High-Grade Prostatic Intraepithelial Neoplasia. Int. J. Mol. Sci. 2014, 15, 1433-1440. https://doi.org/10.3390/ijms15011433
Mariani S, Lionetto L, Cavallari M, Tubaro A, Rasio D, De Nunzio C, Hong GM, Borro M, Simmaco M. Low Prostate Concentration of Lycopene Is Associated with Development of Prostate Cancer in Patients with High-Grade Prostatic Intraepithelial Neoplasia. International Journal of Molecular Sciences. 2014; 15(1):1433-1440. https://doi.org/10.3390/ijms15011433
Chicago/Turabian StyleMariani, Simone, Luana Lionetto, Michele Cavallari, Andrea Tubaro, Debora Rasio, Cosimo De Nunzio, Gena M. Hong, Marina Borro, and Maurizio Simmaco. 2014. "Low Prostate Concentration of Lycopene Is Associated with Development of Prostate Cancer in Patients with High-Grade Prostatic Intraepithelial Neoplasia" International Journal of Molecular Sciences 15, no. 1: 1433-1440. https://doi.org/10.3390/ijms15011433
APA StyleMariani, S., Lionetto, L., Cavallari, M., Tubaro, A., Rasio, D., De Nunzio, C., Hong, G. M., Borro, M., & Simmaco, M. (2014). Low Prostate Concentration of Lycopene Is Associated with Development of Prostate Cancer in Patients with High-Grade Prostatic Intraepithelial Neoplasia. International Journal of Molecular Sciences, 15(1), 1433-1440. https://doi.org/10.3390/ijms15011433