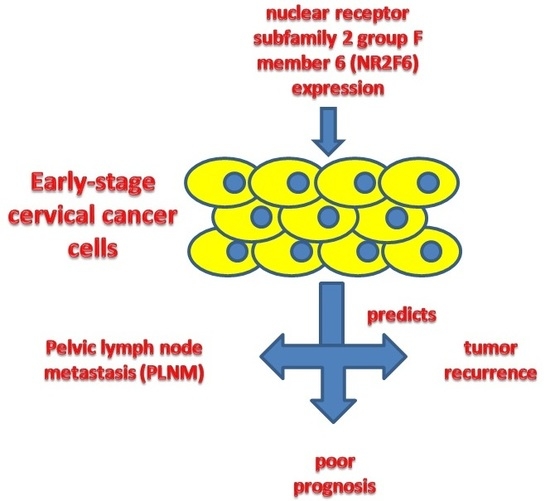
NR2F6 Expression Correlates with Pelvic Lymph Node Metastasis and Poor Prognosis in Early-Stage Cervical Cancer
Abstract
:1. Introduction
2. Results
2.1. Nuclear Receptor Subfamily 2 Group F Member 6 (NR2F6) Is Upregulated in Cervical Cancer Cell Lines
2.2. NR2F6 Is Upregulated in Cervical Cancer Tissues
2.3. Correlation between NR2F6 Overexpression and Cervical Cancer Clinical Features
2.4. High NR2F6 Expression Is Correlated with Poor Prognosis in Early-Stage Cervical Cancer
3. Discussion
4. Materials and Methods
4.1. Patient Information and Tissue Specimens
4.2. Cell Lines
4.3. Real-Time PCR
4.4. Western Blotting
4.5. Immunohistochemical (IHC) Analysis
4.6. Statistical Analysis
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Torre, L.A.; Bray, F.; Siegel, R.L.; Ferlay, J.; Lortet-Tieulent, J.; Jemal, A. Global cancer statistics 2012. CA Cancer J. Clin. 2015, 65, 87–108. [Google Scholar] [CrossRef] [PubMed]
- Piersma, S.J.; Jordanova, E.S.; van Poelgeest, M.I.; Kwappenberg, K.M.; van der Hulst, J.M.; Drijfhout, J.W.; Melief, C.J.; Kenter, G.G.; Fleuren, G.J.; Offringa, R.; et al. High number of intraepithelial CD8+ tumor-infiltrating lymphocytes is associated with the absence of lymph node metastases in patients with large early-stage cervical cancer. Cancer Res. 2007, 67, 354–361. [Google Scholar] [CrossRef] [PubMed]
- Iida, M.; Banno, K.; Yanokura, M.; Nakamura, K.; Adachi, M.; Nogami, Y.; Umene, K.; Masuda, K.; Kisu, I.; Iwata, T.; et al. Candidate biomarkers for cervical cancer treatment: Potential for clinical practice (Review). Mol. Clin. Oncol. 2014, 2, 647–655. [Google Scholar] [CrossRef] [PubMed]
- Bermudez, A.; Bhatla, N.; Leung, E. Cancer of the cervix uteri. Int. J. Gynaecol. Obstet. 2015, 131, S88–S95. [Google Scholar] [CrossRef] [PubMed]
- Asano, H.; Todo, Y.; Watari, H. Adjuvant chemotherapy for early-stage cervical cancer. Chin. J. Cancer Res. 2016, 28, 228–234. [Google Scholar] [CrossRef] [PubMed]
- Hou, T.; Liang, D.; Xu, L.; Huang, X.; Huang, Y.; Zhang, Y. Atypical chemokine receptors predict lymph node metastasis and prognosis in patients with cervical squamous cell cancer. Gynecol. Oncol. 2013, 130, 181–187. [Google Scholar] [CrossRef] [PubMed]
- Noordhuis, M.G.; Fehrmann, R.S.; Wisman, G.B.; Nijhuis, E.R.; van Zanden, J.J.; Moerland, P.D.; ver Loren van Themaat, E.; Volders, H.H.; Kok, M.; Ten Hoor, K.A.; et al. Involvement of the TGF-β and β-catenin pathways in pelvic lymph node metastasis in early-stage cervical cancer. Clin. Cancer Res. 2011, 17, 1317–1330. [Google Scholar] [CrossRef] [PubMed]
- Safe, S.; Jin, U.H.; Hedrick, E.; Reeder, A.; Lee, S.O. Minireview: Role of orphan nuclear receptors in cancer and potential as drug targets. Mol. Endocrinol. 2014, 28, 157–172. [Google Scholar] [CrossRef] [PubMed]
- Tsai, S.Y.; Tsai, M.J. Chick ovalbumin upstream promoter-transcription factors (COUP-TFs): Coming of age. Endocr. Rev. 1997, 18, 229–240. [Google Scholar] [CrossRef] [PubMed]
- Germain, P.; Staels, B.; Dacquet, C.; Spedding, M.; Laudet, V. Overview of nomenclature of nuclear receptors. Pharmacol. Rev. 2006, 58, 685–704. [Google Scholar] [CrossRef] [PubMed]
- Takamoto, N.; You, L.R.; Moses, K.; Chiang, C.; Zimmer, W.E.; Schwartz, R.J.; DeMayo, F.J.; Tsai, M.J.; Tsai, S.Y. COUP-TFII is essential for radial and anteroposterior patterning of the stomach. Development 2005, 132, 2179–2189. [Google Scholar] [CrossRef] [PubMed]
- Doerks, T.; Copley, R.R.; Schultz, J.; Ponting, C.P.; Bork, P. Systematic identification of novel protein domain families associated with nuclear functions. Genome Res. 2002, 12, 47–56. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Dufau, M.L. Nuclear orphan receptors regulate transcription of the gene for the human luteinizing hormone receptor. J. Biol. Chem. 2000, 275, 2763–2770. [Google Scholar] [CrossRef] [PubMed]
- Park, J.I.; Tsai, S.Y.; Tsai, M.J. Molecular mechanism of chicken ovalbumin upstream promoter-transcription factor (COUP-TF) actions. Keio J. Med. 2003, 52, 174–181. [Google Scholar] [CrossRef] [PubMed]
- Ichim, C.V.; Dervović, D.D.; Zúñiga-Pflücker, J.C.; Wells, R.A. The orphan nuclear receptor Ear-2 (Nr2f6) is a novel negative regulator of T cell development. Exp. Hematol. 2014, 42, 46–58. [Google Scholar] [CrossRef] [PubMed]
- Ichim, C.V.; Atkins, H.L.; Iscove, N.N.; Wells, R.A. Identification of a role for the nuclear receptor EAR-2 in the maintenance of clonogenic status within the leukemia cell hierarchy. Leukemia 2011, 25, 1687–1696. [Google Scholar] [CrossRef] [PubMed]
- Li, X.B.; Jiao, S.; Sun, H.; Xue, J.; Zhao, W.T.; Fan, L.; Wu, G.H.; Fang, J. The orphan nuclear receptor EAR2 is overexpressed in colorectal cancer and it regulates survivability of colon cancer cells. Cancer Lett. 2011, 309, 137–144. [Google Scholar] [CrossRef] [PubMed]
- Muscat, G.E.; Eriksson, N.A.; Byth, K.; Loi, S.; Graham, D.; Jindal, S.; Davis, M.J.; Clyne, C.; Funder, J.W.; Simpson, E.R.; et al. Research resource: Nuclear receptors as transcriptome: Discriminant and prognostic value in breast cancer. Mol. Endocrinol. 2013, 27, 350–365. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.; Yu, C.P.; Zhong, Y.; Liu, T.J.; Huang, Q.D.; Zhao, X.H.; Huang, H.; Tu, H.; Jiang, S.; Zhang, Y.; et al. Sam68 expression and cytoplasmic localization is correlated with lymph node metastasis as well as prognosis in patients with early-stage cervical cancer. Ann. Oncol. 2012, 23, 638–646. [Google Scholar] [CrossRef] [PubMed]
- Liu, L.; Xia, M.; Wang, J.; Zhang, W.; Zhang, Y.; He, M. CISD2 expression is a novel marker correlating with pelvic lymph node metastasis and prognosis in patients with early-stage cervical cancer. Med. Oncol. 2014, 31, 183. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Hou, T.; Niu, C.; Song, L.; Zhang, Y. B3GNT3 expression is a novel marker correlated with pelvic lymph node metastasis and poor clinical outcome in early-stage cervical cancer. PLoS ONE 2015, 10, e0144360. [Google Scholar] [CrossRef] [PubMed]
- Delgado, G.; Bundy, B.; Zaino, R.; Sevin, B.U.; Creasman, W.T.; Major, F. Prospective surgical-pathological study of disease-free interval in patients with stage IB squamous cell carcinoma of the cervix: A gynecologic oncology group study. Gynecol. Oncol. 1990, 38, 352–357. [Google Scholar] [CrossRef]
- Landoni, F.; Maneo, A.; Colombo, A.; Placa, F.; Milani, R.; Perego, P.; Favini, G.; Ferri, L.; Mangioni, C. Randomised study of radical surgery versus radiotherapy for stage Ib-IIa cervical cancer. Lancet 1997, 350, 535–540. [Google Scholar] [CrossRef]
- Ahn, H.K.; Shin, J.W.; Ahn, H.Y.; Park, C.Y.; Lee, N.W.; Lee, J.K.; Hwang, I.C. Metabolic components and recurrence in early-stage cervical cancer. Tumour Biol. 2015, 36, 2201–2207. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.K.; Jo, H.; Kong, H.J.; Kim, H.C.; Kim, J.W.; Kim, Y.M.; Song, Y.S.; Kang, S.B.; Mok, J.E.; Lee, H.P. Postoperative nomogram predicting risk of recurrence after radical hysterectomy for early-stage cervical cancer. Int. J. Gynecol. Cancer 2010, 20, 1581–1586. [Google Scholar] [PubMed]
- Peters, W.A.; Liu, P.Y.; Barrett, R.J.; Stock, R.J.; Monk, B.J.; Berek, J.S.; Souhami, L.; Grigsby, P.; Gordon, W., Jr.; Alberts, D.S. Concurrent chemotherapy and pelvic radiation therapy compared with pelvic radiation therapy alone as adjuvant therapy after radical surgery in high-risk early-stage cancer of the cervix. J. Clin. Oncol. 2000, 18, 1606–1613. [Google Scholar] [CrossRef] [PubMed]
- Sedlis, A.; Bundy, B.N.; Rotman, M.Z.; Lentz, S.S.; Muderspach, L.I.; Zaino, R.J. A randomized trial of pelvic radiation therapy versus no further therapy in selected patients with stage IB carcinoma of the cervix after radical hysterectomy and pelvic lymphadenectomy: A gynecologic oncology group study. Gynecol. Oncol. 1999, 73, 177–183. [Google Scholar] [CrossRef] [PubMed]
- Frumovitz, M.; Sun, C.C.; Schover, L.R.; Munsell, M.F.; Jhingran, A.; Wharton, J.T.; Eifel, P.; Bevers, T.B.; Levenback, C.F.; Gershenson, D.M.; et al. Quality of life and sexual functioning in cervical cancer survivors. J. Clin. Oncol. 2005, 23, 7428–7436. [Google Scholar] [CrossRef] [PubMed]
- Cervical Cancer Treatment (PDQ). Available online: http://www.cancer.gov/cancertopics/pdq/treatment/cervical/Patient/page5 (accessed on 22 October 2014).
- NCCN Clinical Guideline in Oncology. Cervical Cancer Version 2, 2015. Available online: http://www.nccn.org/professionals/physician_gls/pdf/cervical.pdf (accessed on 23 August 2015).
- Colombo, N.; Carinelli, S.; Colombo, A.; Marini, C.; Rollo, D.; Sessa, C. Cervical cancer: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 2012, 23, vii27–vii32. [Google Scholar] [CrossRef] [PubMed]
- Takeshima, N.; Umayahara, K.; Fujiwara, K.; Hirai, Y.; Takizawa, K.; Hasumi, K. Treatment results of adjuvant chemotherapy after radical hysterectomy for intermediate- and high-risk stage IB-IIA cervical cancer. Gynecol. Oncol. 2006, 103, 618–622. [Google Scholar] [CrossRef] [PubMed]
- Hosaka, M.; Watari, H.; Takeda, M.; Moriwaki, M.; Hara, Y.; Todo, Y.; Ebina, Y.; Sakuragi, N. Treatment of cervical cancer with adjuvant chemotherapy versus adjuvant radiotherapy after radical hysterectomy and systematic lymphadenectomy. J. Obstet. Gynaecol. Res. 2008, 34, 552–556. [Google Scholar] [CrossRef] [PubMed]
- Angioli, R.; Plotti, F.; Montera, R.; Aloisi, A.; Luvero, D.; Capriglione, S.; Terranova, C.; de Cicco Nardone, C.; Muzii, L.; Benedetti-Panici, P. Neoadjuvant chemotherapy plus radical surgery followed by chemotherapy in locally advanced cervical cancer. Gynecol. Oncol. 2012, 127, 290–296. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.B.; Lee, J.M.; Ki, K.D.; Lee, S.K.; Park, C.Y.; Ha, S.Y. Comparison of adjuvant chemotherapy and radiation in patients with intermediate risk factors after radical surgery in FIGO stage IB-IIA cervical cancer. Int. J. Gynecol. Cancer 2008, 18, 1027–1031. [Google Scholar] [CrossRef] [PubMed]
- Lee, T.Y.; Jeung, Y.J.; Lee, C.J.; Kim, H.Y.; Kim, S.H.; Kim, W.G. Promising treatment results of adjuvant chemotherapy following radical hysterectomy for intermediate risk stage 1B cervical cancer. Obstet. Gynecol. Sci. 2013, 56, 15–21. [Google Scholar] [CrossRef] [PubMed]
- Li, S.; Hu, T.; Chen, Y.; Zhou, H.; Li, X.; Cheng, X.; Yang, R.; Wang, S.; Xie, X.; Ma, D. Adjuvant chemotherapy, a valuable alternative option in selected patients with cervical cancer. PLoS ONE 2013, 8, e73837. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.D.; Li, H.Y.; Li, B.H.; Xie, T.; Zhu, T.; Sun, L.L.; Ren, H.Y.; Ye, Z.M. The role of CTLA-4 and PD-1 in anti-tumor immune response and their potential efficacy against osteosarcoma. Int. Immunopharmacol. 2016, 38, 81–89. [Google Scholar] [CrossRef] [PubMed]
- Hermann-Kleiter, N.; Klepsch, V.; Wallner, S.; Siegmund, K.; Klepsch, S.; Tuzlak, S.; Villunger, A.; Kaminski, S.; Pfeifhofer-Obermair, C.; Gruber, T.; et al. The nuclear orphan receptor NR2F6 is a central checkpoint for cancer immune surveillance. Cell Rep. 2015, 12, 2072–2085. [Google Scholar] [CrossRef] [PubMed]





| Characteristic | Number of Cases (%) | |
|---|---|---|
| Age (years) | ≤46 | 95 (50.3) |
| >46 | 94 (49.7) | |
| FIGO (International Federation of Gynecology and Obstetrics) Stage | Ib1 | 72 (38.1) |
| Ib2 | 37 (19.6) | |
| IIa1 | 54 (28.6) | |
| IIa2 | 26 (13.8) | |
| Histological Type | Squamous carcinoma | 179 (94.7) |
| Adenocarcinoma | 10 (5.3) | |
| Tumor Size, cm | <4 cm | 154(81.5) |
| ≥4 cm | 35 (18.5) | |
| Squamous Cell Carcinoma Antigen, ng/mL | ≤1.5 | 110 (65.5) |
| >1.5 | 58 (34.5) | |
| HPV (Human Papillomavirus) Infection | No | 38 (20.1) |
| Yes | 151 (79.9) | |
| Pelvic Lymph Node Metastasis | No | 135 (71.4) |
| Yes | 54 (28.6) | |
| Tumor Recurrence | No | 170 (89.9) |
| Yes | 19 (10.1) | |
| Vital Status (at last follow-up) | Alive | 160 (84.7) |
| Dead | 29 (15.3) | |
| Differentiation Grade | G1 | 73 (49.6) |
| G2 | 41 (27.9) | |
| G3 | 33 (22.5) | |
| Myometrium Invasion | <1/2 | 66 (34.9) |
| ≥1/2 | 122 (64.6) | |
| Property of Surgical Margin | No | 176 (93.1) |
| Yes | 13 (6.9) | |
| Infiltration of Parauterine Organ | No | 179 (94.7) |
| Yes | 10 (5.3) | |
| Lymphovascular Space Involvement | No | 173 (91.5) |
| Yes | 16 (8.0) | |
| Chemotherapy | No | 73 (38.6) |
| Yes | 115 (61.2) | |
| Radiation | No | 169 (89.4) |
| Yes | 20 (10.6) | |
| Concurrent chemotherapy and Radiotherapy | No | 176 (93.1) |
| Yes | 13 (6.9) | |
| Expression of NR2f6 | Low or none | 114 (60.3) |
| High | 75 (39.7) | |
| Characteristic | Total | NR2F6 | Chi-Squared Test p-Value | Fisher’s Exact Test p-Value | ||
|---|---|---|---|---|---|---|
| No or Weak Expression | Moderate or Strong Expression | |||||
| Age (years) | ≤46 | 95 | 58 (30.7) | 37 (19.6) | 0.835 | 0.882 |
| >46 | 94 | 52 (29.6) | 41 (20.1) | |||
| Histological Type | Adenocarcinoma | 10 | 7 (3.7) | 3 (1.6) | 0.520 | 0.742 |
| Squamous cell carcinoma | 179 | 107 (56.6) | 72 (38.1) | |||
| HPV Infection | No | 38 | 26 (13.8) | 12 (6.3) | 0.253 | 0.272 |
| Yes | 151 | 88 (46.6) | 63 (33.3) | |||
| FIGO Stage | Ib1 | 72 | 52 (27.5) | 20 (10.6) | 0.027 | - |
| Ib2 | 37 | 23 (12.2) | 14 (7.4) | |||
| IIa1 | 54 | 25 (13.2) | 29 (15.3) | |||
| IIa2 | 26 | 14 (7.4) | 12 (6.3) | |||
| Pelvic Lymph Node Metastasis | Absent | 135 | 98 (51.9) | 37 (19.6) | 0.000 | 0.000 |
| Present | 54 | 16 (8.5) | 38 (20.1) | |||
| Squamous Cell Carcinoma Antigen, ng/mL | ≤1.5 | 110 | 75 (44.6) | 35 (16.1) | 0.006 | 0.008 |
| >1.5 | 58 | 27(20.8) | 31(18.5) | |||
| Tumor Size | <4 cm | 154 | 93 (49.2) | 61 (32.3) | 0.996 | 1.000 |
| ≥4 cm | 35 | 21 (11.1) | 14 (17.4) | |||
| Tumor Recurrence | No | 170 | 109 (57.7) | 61 (32.3) | 0.001 | 0.002 |
| Yes | 19 | 5 (2.6) | 14 (7.4) | |||
| Vital Status (At Last Follow-up) | Alive | 160 | 107 (56.6) | 53 (28.0) | 0.000 | 0.000 |
| Dead | 29 | 7 (3.7) | 22 (11.6) | |||
| Differentiation Grade | G1 | 73 | 48 (32.7) | 25 (17.0) | 0.113 | - |
| G2 | 41 | 27 (18.4) | 14 (9.5) | |||
| G3 | 33 | 20 (13.6) | 13 (8.8) | |||
| Chemotherapy | No | 73 | 51 (27.1) | 22 (11.7) | 0.039 | 0.047 |
| Yes | 115 | 63 (33.5) | 52 (27.7) | |||
| Radiation | No | 169 | 105 (55.6) | 64 (33.9) | 0.139 | 0.153 |
| Yes | 20 | 9 (4.8) | 11 (5.8) | |||
| Concurrent Chemotherapy and Radiotherapy | No | 176 | 107 (56.6) | 69 (36.5) | 0.621 | 0.770 |
| Yes | 13 | 7 (3.7) | 6 (3.2) | |||
| Myometrium Invasion | <1/2 | 66 | 43 (22.9) | 23 (12.2) | 0.299 | 0.350 |
| ≥1/2 | 122 | 70 (37.2) | 52 (27.7) | |||
| Property of Surgical Margin | No | 176 | 108 (57.1) | 68 (36.0) | 0.279 | 0.379 |
| Yes | 13 | 11 (3.2) | 2 (3.7) | |||
| Infiltration of Parauterine Organ | No | 179 | 108 (57.1) | 71 (37.6) | 0.983 | 1.000 |
| Yes | 10 | 6 (3.2) | 4 (2.1) | |||
| Lymphovascular Space Involvement | No | 173 | 107 (56.6) | 66 (34.9) | 0.157 | 0.186 |
| Yes | 16 | 7 (3.7) | 9 (4.8) | |||
| Variable | NR2F6 Expression | |
|---|---|---|
| Spearman’s Correlation Coefficient | p-Value | |
| Age | 0.015 | 0.837 |
| Histological type | −0.047 | 0.523 |
| HPV infection | 0.083 | 0.256 |
| FIGO Stage | 0.198 | 0.006 |
| Pelvic lymph node metastasis | 0.397 | <0.001 |
| Squamous cell carcinoma antigen, ng/mL | 0.211 | 0.006 |
| Tumor size | 0.003 | 0.996 |
| Recurrence | 0.232 | 0.001 |
| Vital status | 0.315 | <0.001 |
| Differentiation grade | −0.150 | 0.042 |
| Chemotherapy | 0.150 | 0.039 |
| Radiation | 0.108 | 0.140 |
| Concurrent chemotherapy and radiotherapy | 0.036 | 0.623 |
| Myometrium invasion | 0.076 | 0.301 |
| Property of surgical margin | 0.079 | 0.282 |
| Infiltration of parauterine organ | 0.002 | 0.983 |
| Lymphovascular space involvement | 0.103 | 0.158 |
| Variable | Univariate Analysis | Multivariate Analysis | ||||
|---|---|---|---|---|---|---|
| No. Patients | p | Regression Coefficient (SE) | p | Relative Risk | 95% Confidence Interval | |
| NR2F6 | ||||||
| Low expression | 114 | <0.001 | 7.688 (0.447) | 0.006 | 4.439 | 1.533–12.855 |
| High expression | 75 | |||||
| Pelvic lymph Node Metastasis | ||||||
| Absent | 135 | 0.001 | 3.326 (0.374) | 0.486 | 1.354 | 0.576–3.183 |
| Present | 54 | |||||
| Squamous Cell Carcinoma Antigen, ng/mL | ||||||
| ≤1.5 | 110 | 0.006 | 3.065 (0.408) | 0.449 | 0.689 | 0.262–1.808 |
| >1.5 | 58 | |||||
| FIGO Stage | ||||||
| Ib1 | 72 | 0.010 | 1.551 (0.439) | 0.082 | 1.484 | 0.951–2.315 |
| Ib2 | 37 | |||||
| IIa1 | 54 | |||||
| IIa2 | 26 | |||||
| Recurrence | ||||||
| No | 170 | <0.001 | 30.659 (0.406) | 0.000 | 21.311 | 7.741–58.667 |
| Yes | 19 | |||||
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Niu, C.; Sun, X.; Zhang, W.; Li, H.; Xu, L.; Li, J.; Xu, B.; Zhang, Y. NR2F6 Expression Correlates with Pelvic Lymph Node Metastasis and Poor Prognosis in Early-Stage Cervical Cancer. Int. J. Mol. Sci. 2016, 17, 1694. https://doi.org/10.3390/ijms17101694
Niu C, Sun X, Zhang W, Li H, Xu L, Li J, Xu B, Zhang Y. NR2F6 Expression Correlates with Pelvic Lymph Node Metastasis and Poor Prognosis in Early-Stage Cervical Cancer. International Journal of Molecular Sciences. 2016; 17(10):1694. https://doi.org/10.3390/ijms17101694
Chicago/Turabian StyleNiu, Chunhao, Xiaoying Sun, Weijing Zhang, Han Li, Liqun Xu, Jun Li, Benke Xu, and Yanna Zhang. 2016. "NR2F6 Expression Correlates with Pelvic Lymph Node Metastasis and Poor Prognosis in Early-Stage Cervical Cancer" International Journal of Molecular Sciences 17, no. 10: 1694. https://doi.org/10.3390/ijms17101694
APA StyleNiu, C., Sun, X., Zhang, W., Li, H., Xu, L., Li, J., Xu, B., & Zhang, Y. (2016). NR2F6 Expression Correlates with Pelvic Lymph Node Metastasis and Poor Prognosis in Early-Stage Cervical Cancer. International Journal of Molecular Sciences, 17(10), 1694. https://doi.org/10.3390/ijms17101694