Microbial Etiology of Pneumonia: Epidemiology, Diagnosis and Resistance Patterns
Abstract
:1. Introduction
2. Microbial Etiology of Community-Acquired Pneumonia (CAP)
2.1. Epidemiology
2.2. Causative Microorganism
2.3. Multidrug-Resistant (MDR) Pathogens in CAP
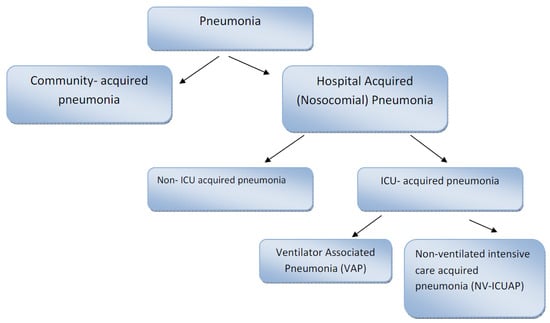
3. Microbial Etiology of Hospital Acquired Pneumonia (HAP)
3.1. Epidemiology
- (i)
- Early onset is defined as case development within the first four days of hospitalization. “Community” microorganisms are the main causes of these cases of pneumonia (methicillin-sensitive Staphylococcus aureus, Streptococcus pneumoniae, Haemophilus influenzae, and anaerobes. This kind of pneumonia is associated with better clinical prognosis.
- (ii)
- Late onset is defined when pneumonia occurs after 5 days of hospitalization. The main pathogens involved in this kind of pneumonia are methicillin-resistant S. aureus, enteric gram negative bacilli, P. aeruginosa and non-fermenting bacteria (e.g., A. baumannii, S. maltophilia). Pneumonia caused by two or more pathogens (polymicrobial) is also frequent [59].
- (iii)
- Early onset HAP tends to have a better prognosis than late onset HAP because of the association of the latter with MDR organisms.
3.2. Causative Microorganism
3.2.1. Gram-Negative Pathogens
- (i)
- Pseudomonas aeruginosa.
- (ii)
- Acinetobacter baumannii.
- (iii)
- Haemophilus influenzae.
- (iv)
- Enterobacteriaceae (Klebsiella pneumoniae, E. coli, Enterobacter species, Serratia species, Proteus species, etc.).
3.2.2. Gram-Positive Pathogens
3.2.3. Polymicrobial Infection
3.2.4. Microbial Etiology of Early- and Late-Onset Pneumonia
3.2.5. Multidrug-Resistant Pathogens (MDR)
- (i)
- Risk factors for MDR HAP: prior intravenous antibiotic treatment within 90 days;
- (ii)
- Risk factors for MDR VAP: prior intravenous antibiotic treatment within 90 days; septic shock at time of VAP; ARDS preceding VAP; five or more days of hospitalization prior to the occurrence of VAP; acute renal replacement therapy prior to VAP onset.
4. Laboratory Diagnosis of Pneumonia
4.1. Clinical Samples to Be Collected
4.1.1. Community-Acquired Pneumonia
- (i)
- Outpatients with failure of antibiotic therapy: sputum culture, urinary antigen test for Legionella pneumophila and Streptococcus pneumoniae.
- (ii)
- Hospitalized patients with positive urinary antigen test for pneumococcus: sputum and blood culture.
- (iii)
- Severe obstructive lung disease: sputum culture.
- (iv)
- Pleural effusion: sputum and blood culture, urinary antigen test for pneumococcus and Legionella, pleural fluid culture.
- (v)
- Cavitary infiltrates: sputum culture (bacteria, fungi and mycobacteria) and blood culture.
- (vi)
- Active alcoholism: sputum and blood culture, urinary antigen test for pneumococcus and Legionella.
- (vii)
- Severe CAP admitted to intensive care unit (ICU): sputum and blood culture, urinary antigen test for pneumococcus and Legionella, tracheal aspirate or bronchoalveolar lavage culture and viral studies also need to be performed.
- (viii)
- Epidemiological factor or specific risk factors suggesting pathogen: urinary antigen test for Legionella (Legionnaires disease), influenza test during influenza season.
4.1.2. Hospital Acquired Pneumonia
4.2. Diagnostic Testing for Pneumonia
4.2.1. Conventional Microbiological Diagnosis
4.2.2. Molecular Microbiological Diagnosis
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
Abbreviation
| CAP | Community-acquired pneumonia |
| EPIC | Etiology of Pneumonia in the Community |
| ARP | Antibiotic resistant pathogen |
| ICU | Intensive care unit |
| RSV | Respiratory syncitial virus |
| MDR | Multidrug-resistant |
| MRSA | Methicillin-resistant S. aureus |
| MSSA | Methicillin-sensitive S. aureus |
| CA-MRSA | Community-acquired methicillin-resistant S. aureus |
| PVL | Panton-Valentine leukocidin |
| PBPs | Penicillin-binding proteins |
| MIC | Minimum inhibitory concentration |
| HAP | Hospital Acquired Pneumonia |
| VAP | Ventilator associated pneumonia |
| NV-ICUAP | Non-ventilated intensive care acquired pneumonia |
| VE-VAP | Very early-onset VAP |
| HABP | Hospital acquired bacterial pneumonia |
| VABP | Ventilated acquired bacterial pneumonia |
| ESBL | Extended spectrum β-lactamases |
| CFU | Colony-forming units |
References
- Murphy, S.L.; Kochanek, K.D.; Xu, J.; Arias, E. Mortality in the United States, 2014. NCHS Data Brief 2015, 229, 1–8. [Google Scholar]
- World Health Organization (WHO). Pneumonia Fact Sheet; World Health Organization Report 2016; WHO: Geneva, Switzerland, 2016. [Google Scholar]
- World Health Organization (WHO). Antimicrobial Resistance: Global Report on Surveillance 2014; Antimicrobial Resistance Global Surveillance Report; WHO: Geneva, Switzerland, 2014. [Google Scholar]
- GBD 2013 Mortality and Causes of Death Collaborators. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015, 385, 117–171. [Google Scholar]
- Welte, T.; Torres, A.; Nathwani, D. Clinical and economic burden of community-acquired pneumonia among adults in Europe. Thorax 2012, 67, 71–79. [Google Scholar] [CrossRef] [PubMed]
- Jain, S.; Self, W.H.; Wunderink, R.G.; Fakhran, S.; Balk, R.; Bramley, A.M.; Reed, C.; Grijalva, C.G.; Anderson, E.J.; Courtney, D.M.; et al. Community-Acquired pneumonia requiring hospitalization among U.S. adults. N. Engl. J. Med. 2015, 373, 415–427. [Google Scholar] [CrossRef] [PubMed]
- Rozenbaum, M.H.; Mangen, M.J.; Huijts, S.M.; van der Werf, T.S.; Postma, M.J. Incidence, direct costs and duration of hospitalization of patients hospitalized with community acquired pneumonia: A nationwide retrospective claims database analysis. Vaccine 2015, 33, 3193–3199. [Google Scholar] [CrossRef] [PubMed]
- Cilloniz, C.; Ewig, S.; Polverino, E.; Marcos, M.A.; Esquinas, C.; Gabarrus, A.; Mensa, J.; Torres, A. Microbial aetiology of community-acquired pneumonia and its relation to severity. Thorax 2011, 66, 340–346. [Google Scholar] [CrossRef] [PubMed]
- Cilloniz, C.; Ewig, S.; Polverino, E.; Marcos, M.A.; Prina, E.; Sellares, J.; Ferrer, M.; Ortega, M.; Gabarrus, A.; Mensa, J.; et al. Community-acquired pneumonia in outpatients: Aetiology and outcomes. Eur. Respir. J. 2012, 40, 931–938. [Google Scholar] [CrossRef] [PubMed]
- Garau, J.; Baquero, F.; Perez-Trallero, E.; Perez, J.L.; Martin-Sanchez, A.M.; Garcia-Rey, C.; Martin-Herrero, J.E.; Dal-Re, R. Factors impacting on length of stay and mortality of community-acquired pneumonia. Clin. Microbiol. Infect. 2008, 14, 322–329. [Google Scholar] [CrossRef] [PubMed]
- Barlow, G.; Nathwani, D.; Williams, F.; Ogston, S.; Winter, J.; Jones, M.; Slane, P.; Myers, E.; Sullivan, F.; Stevens, N.; et al. Reducing door-to-antibiotic time in community-acquired pneumonia: Controlled before-and-after evaluation and cost-effectiveness analysis. Thorax 2007, 62, 67–74. [Google Scholar] [CrossRef] [PubMed]
- Yu, K.T.; Wyer, P.C. Evidence-based emergency medicine/critically appraised topic. Evidence behind the 4-hour rule for initiation of antibiotic therapy in community-acquired pneumonia. Ann. Emerg. Med. 2008, 51, 651–662. [Google Scholar] [CrossRef] [PubMed]
- Rozenbaum, M.H.; Pechlivanoglou, P.; van der Werf, T.S.; Lo-Ten-Foe, J.R.; Postma, M.J.; Hak, E. The role of Streptococcus pneumoniae in community-acquired pneumonia among adults in Europe: A meta-analysis. Eur. J. Clin. Microbiol. Infect. Dis. 2013, 32, 305–316. [Google Scholar] [CrossRef] [PubMed]
- Simonetti, A.F.; Garcia-Vidal, C.; Viasus, D.; Garcia-Somoza, D.; Dorca, J.; Gudiol, F.; Carratala, J. Declining mortality among hospitalized patients with community-acquired pneumonia. Clin. Microbiol. Infect. 2016. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention (CDC). Current cigarette smoking among adults—United States, 2011. MMWR Morb. Mortal. Wkly. Rep. 2012, 61, 889–894. [Google Scholar]
- Garcia-Vidal, C.; Ardanuy, C.; Tubau, F.; Viasus, D.; Dorca, J.; Linares, J.; Gudiol, F.; Carratala, J. Pneumococcal pneumonia presenting with septic shock: Host- and pathogen-related factors and outcomes. Thorax 2010, 65, 77–81. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Blasi, F. Atypical pathogens and respiratory tract infections. Eur. Respir. J. 2004, 24, 171–181. [Google Scholar] [CrossRef] [PubMed]
- Marrie, T.J.; Costain, N.; La, S.B.; Patrick, W.; Forgie, S.; Xu, Z.; McNeil, S.A. The role of atypical pathogens in community-acquired pneumonia. Semin. Respir. Crit. Care Med. 2012, 33, 244–256. [Google Scholar] [CrossRef] [PubMed]
- Cilloniz, C.; Torres, A.; Niederman, M.; van der, E.M.; Chalmers, J.; Welte, T.; Blasi, F. Community-acquired pneumonia related to intracellular pathogens. Intensive Care Med. 2016. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Basarab, M.; Macrae, M.B.; Curtis, C.M. Atypical pneumonia. Curr. Opin. Pulm. Med. 2014, 20, 247–251. [Google Scholar] [CrossRef] [PubMed]
- Capelastegui, A.; Espana, P.P.; Bilbao, A.; Gamazo, J.; Medel, F.; Salgado, J.; Gorostiaga, I.; Lopez de Goicoechea, M.J.; Gorordo, I.; Esteban, C.; et al. Etiology of community-acquired pneumonia in a population-based study: Link between etiology and patients characteristics, process-of-care, clinical evolution and outcomes. BMC Infect. Dis. 2012, 12, 134. [Google Scholar] [CrossRef] [PubMed]
- Cilloniz, C.; Ewig, S.; Ferrer, M.; Polverino, E.; Gabarrus, A.; Puig de la, B.J.; Mensa, J.; Torres, A. Community-acquired polymicrobial pneumonia in the intensive care unit: Aetiology and prognosis. Crit. Care 2011, 15, R209. [Google Scholar] [CrossRef] [PubMed]
- Ruuskanen, O.; Lahti, E.; Jennings, L.C.; Murdoch, D.R. Viral pneumonia. Lancet 2011, 377, 1264–1275. [Google Scholar] [CrossRef]
- Archer, B.; Cohen, C.; Naidoo, D.; Thomas, J.; Makunga, C.; Blumberg, L.; Venter, M.; Timothy, G.; Puren, A.; McAnerney, J.; et al. Interim report on pandemic H1N1 influenza virus infections in South Africa, April to October 2009: Epidemiology and factors associated with fatal cases. Euro Surveill 2009, 14. [Google Scholar]
- Crovari, P.; Gasparini, R. Influenza (AH1N1v) pandemic 2009: An update. J. Prev. Med. Hyg. 2009, 50, 129–130. [Google Scholar] [PubMed]
- Dowell, S.F.; Anderson, L.J.; Gary, H.E., Jr.; Erdman, D.D.; Plouffe, J.F.; File, T.M., Jr.; Marston, B.J.; Breiman, R.F. Respiratory syncytial virus is an important cause of community-acquired lower respiratory infection among hospitalized adults. J. Infect. Dis. 1996, 174, 456–462. [Google Scholar] [CrossRef] [PubMed]
- Zambon, M.C.; Stockton, J.D.; Clewley, J.P.; Fleming, D.M. Contribution of influenza and respiratory syncytial virus to community cases of influenza-like illness: An observational study. Lancet 2001, 358, 1410–1416. [Google Scholar] [CrossRef]
- Griffin, M.R.; Coffey, C.S.; Neuzil, K.M.; Mitchel, E.F., Jr.; Wright, P.F.; Edwards, K.M. Winter viruses: Influenza- and respiratory syncytial virus-related morbidity in chronic lung disease. Arch. Intern. Med. 2002, 162, 1229–1236. [Google Scholar] [CrossRef] [PubMed]
- Ellis, S.E.; Coffey, C.S.; Mitchel, E.F., Jr.; Dittus, R.S.; Griffin, M.R. Influenza- and respiratory syncytial virus-associated morbidity and mortality in the nursing home population. J. Am. Geriatr. Soc. 2003, 51, 761–767. [Google Scholar] [CrossRef] [PubMed]
- Walsh, E.E.; Falsey, A.R. Respiratory syncytial virus infection in adult populations. Infect. Disord. Drug Targets 2012, 12, 98–102. [Google Scholar] [CrossRef] [PubMed]
- Ebbert, J.O.; Limper, A.H. Respiratory syncytial virus pneumonitis in immunocompromised adults: Clinical features and outcome. Respiration 2005, 72, 263–269. [Google Scholar] [CrossRef] [PubMed]
- Teramoto, S.; Yoshida, K.; Hizawa, N. Update on the pathogenesis and management of pneumonia in the elderly-roles of aspiration pneumonia. Respir. Investig. 2015, 53, 178–184. [Google Scholar] [CrossRef] [PubMed]
- Aliberti, S.; Cilloniz, C.; Chalmers, J.D.; Zanaboni, A.M.; Cosentini, R.; Tarsia, P.; Pesci, A.; Blasi, F.; Torres, A. Multidrug-resistant pathogens in hospitalised patients coming from the community with pneumonia: A European perspective. Thorax 2013, 68, 997–999. [Google Scholar] [CrossRef] [PubMed]
- Obed, M.; Garcia-Vidal, C.; Pessacq, P.; Mykietiuk, A.; Viasus, D.; Cazzola, L.; Dominguez, M.; Calmaggi, A.; Carratala, J. Características clínicas y pronóstico de la neumonía adquirida en la comunidad causada por Staphylococcus aureus resistente a meticilina. Enfermedades Infecciosas y Microbiología Clínica 2014, 32, 23–27. (In Spanish) [Google Scholar] [CrossRef] [PubMed]
- Mandell, L.A.; Wunderink, R.G.; Anzueto, A.; Bartlett, J.G.; Campbell, G.D.; Dean, N.C.; Dowell, S.F.; File, T.M., Jr.; Musher, D.M.; Niederman, M.S.; et al. Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin. Infect. Dis. 2007, 44, S27–S72. [Google Scholar] [CrossRef] [PubMed]
- Ruiz, L.A.; Gomez, A.; Jaca, C.; Martinez, L.; Gomez, B.; Zalacain, R. Bacteraemic community-acquired pneumonia due to Gram-negative bacteria: Incidence, clinical presentation and factors associated with severity during hospital stay. Infection 2010, 38, 453–458. [Google Scholar] [CrossRef] [PubMed]
- Von Baum, H.; Welte, T.; Marre, R.; Suttorp, N.; Ewig, S. Community-acquired pneumonia through Enterobacteriaceae and Pseudomonas aeruginosa: Diagnosis, incidence and predictors. Eur. Respir. J. 2010, 35, 598–605. [Google Scholar] [CrossRef] [PubMed]
- Arancibia, F.; Bauer, T.T.; Torres, A.; Sanchez, F.; Mensa, J.; Maldonado, A.; Rodriguez, M.J.; Ewig, S. Community-acquired Pneumonia caused by Gram-negative bacteria: Incidence and risk and prognosis. Eur. Respir. J. 2016, in press. [Google Scholar]
- Torres, A.; Serra, B.J.; Ferrer, A.; Jimenez, P.; Celis, R.; Cobo, E.; Rodriguez, R.R. Severe community-acquired pneumonia. Epidemiology and prognostic factors. Am. Rev. Respir. Dis. 1991, 144, 312–318. [Google Scholar] [CrossRef] [PubMed]
- Cilloniz, C.; Polverino, E.; Ewig, S.; Aliberti, S.; Gabarrus, A.; Menendez, R.; Mensa, J.; Blasi, F.; Torres, A. Impact of age and comorbidity on cause and outcome in community-acquired pneumonia. Chest 2013, 144, 999–1007. [Google Scholar] [CrossRef] [PubMed]
- Rello, J.; Bodi, M.; Mariscal, D.; Navarro, M.; Diaz, E.; Gallego, M.; Valles, J. Microbiological testing and outcome of patients with severe community-acquired pneumonia. Chest 2003, 123, 174–180. [Google Scholar] [CrossRef] [PubMed]
- Paganin, F.; Lilienthal, F.; Bourdin, A.; Lugagne, N.; Tixier, F.; Genin, R.; Yvin, J.L. Severe community-acquired pneumonia: Assessment of microbial aetiology as mortality factor. Eur. Respir. J. 2004, 24, 779–785. [Google Scholar] [CrossRef] [PubMed]
- Yoshimoto, A.; Nakamura, H.; Fujimura, M.; Nakao, S. Severe community-acquired pneumonia in an intensive care unit: Risk factors for mortality. Intern. Med. 2005, 44, 710–716. [Google Scholar] [CrossRef] [PubMed]
- Cilloniz, C.; Gabarrus, A.; Ferrer, M.; Puig de la, B.J.; Rinaudo, M.; Mensa, J.; Niederman, M.S.; Torres, A. Community-Acquired Pneumonia due to Multidrug and non-Multidrug resistant Pseudomonas aeruginosa. Chest 2016, 150, 415–425. [Google Scholar] [CrossRef] [PubMed]
- Lynch, J.P., III; Zhanel, G.G. Streptococcus pneumoniae: Does antimicrobial resistance matter? Semin. Respir. Crit. Care Med. 2009, 30, 210–238. [Google Scholar] [PubMed]
- Song, J.H.; Chung, D.R. Respiratory infections due to drug-resistant bacteria. Infect. Dis. Clin. N. Am. 2010, 24, 639–653. [Google Scholar] [CrossRef] [PubMed]
- Van, B.F.; Reinert, R.R.; Appelbaum, P.C.; Tulkens, P.M.; Peetermans, W.E. Multidrug-resistant Streptococcus pneumoniae infections: Current and future therapeutic options. Drugs 2007, 67, 2355–2382. [Google Scholar]
- Draghi, D.C.; Jones, M.E.; Sahm, D.F.; Tillotson, G.S. Geographically-based evaluation of multidrug resistance trends among Streptococcus pneumoniae in the USA: Findings of the FAST surveillance initiative (2003–2004). Int. J. Antimicrob. Agents 2006, 28, 525–531. [Google Scholar] [CrossRef] [PubMed]
- Whitney, C.G.; Farley, M.M.; Hadler, J.; Harrison, L.H.; Lexau, C.; Reingold, A.; Lefkowitz, L.; Cieslak, P.; Cetron, M.; Zell, E.R.; et al. Increasing prevalence of multidrug-resistant Streptococcus pneumoniae in the United States. N. Engl. J. Med. 2000, 343, 1917–1924. [Google Scholar] [CrossRef] [PubMed]
- Cilloniz, C.; Albert, R.K.; Liapikou, A.; Gabarrus, A.; Rangel, E.; Bello, S.; Marco, F.; Mensa, J.; Torres, A. The Effect of Macrolide-Resistance on the Presentation and Outcome of Patients Hospitalized for Streptococcus pneumoniae Pneumonia. Am. J. Respir. Crit. Care Med. 2015, 191, 1265–1272. [Google Scholar] [CrossRef] [PubMed]
- Kalil, A.C.; Metersky, M.L.; Klompas, M.; Muscedere, J.; Sweeney, D.A.; Palmer, L.B.; Napolitano, L.M.; O’Grady, N.P.; Bartlett, J.G.; Carratala, J.; et al. Management of Adults With Hospital-acquired and Ventilator-associated Pneumonia: 2016 Clinical Practice Guidelines by the Infectious Diseases Society of America and the American Thoracic Society. Clin. Infect. Dis. 2016, 63, e61–e111. [Google Scholar] [CrossRef] [PubMed]
- Chastre, J.; Fagon, J.Y. Ventilator-associated pneumonia. Am. J. Respir. Crit. Care Med. 2002, 165, 867–903. [Google Scholar] [CrossRef] [PubMed]
- Kollef, M.H.; Hamilton, C.W.; Ernst, F.R. Economic impact of ventilator-associated pneumonia in a large matched cohort. Infect. Control Hosp. Epidemiol. 2012, 33, 250–256. [Google Scholar] [CrossRef] [PubMed]
- Restrepo, M.I.; Anzueto, A.; Arroliga, A.C.; Afessa, B.; Atkinson, M.J.; Ho, N.J.; Schinner, R.; Bracken, R.L.; Kollef, M.H. Economic burden of ventilator-associated pneumonia based on total resource utilization. Infect. Control Hosp. Epidemiol. 2010, 31, 509–515. [Google Scholar] [CrossRef] [PubMed]
- Rello, J.; Ollendorf, D.A.; Oster, G.; Vera-Llonch, M.; Bellm, L.; Redman, R.; Kollef, M.H. Epidemiology and outcomes of ventilator-associated pneumonia in a large US database. Chest 2002, 122, 2115–2121. [Google Scholar] [CrossRef] [PubMed]
- Richards, M.J.; Edwards, J.R.; Culver, D.H.; Gaynes, R.P. Nosocomial infections in combined medical-surgical intensive care units in the United States. Infect. Control Hosp. Epidemiol. 2000, 21, 510–515. [Google Scholar] [CrossRef] [PubMed]
- Esperatti, M.; Ferrer, M.; Theessen, A.; Liapikou, A.; Valencia, M.; Saucedo, L.M.; Zavala, E.; Welte, T.; Torres, A. Nosocomial Pneumonia in the Intensive Care Unit Acquired during Mechanical Ventilation or Not. Am. J. Respir. Crit. Care Med. 2010, 182, 1533–1539. [Google Scholar] [CrossRef] [PubMed]
- Vincent, J.L.; Rello, J.; Marshall, J.; Silva, E.; Anzueto, A.; Martin, C.D.; Moreno, R.; Lipman, J.; Gomersall, C.; Sakr, Y.; et al. International study of the prevalence and outcomes of infection in intensive care units. JAMA 2009, 302, 2323–2329. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- American Thoracic Society, Infectious Diseases Society of America. Guidelines for the Management of Adults with Hospital-acquired, Ventilator-associated, and Healthcare-associated Pneumonia. Am. J. Respir. Crit. Care Med. 2005, 171, 388–416. [Google Scholar]
- Ewig, S.; Torres, A.; El-Ebiary, M.; Fabregas, N.; Hernández, C.; González, J.; Nicolas, J.M.; Soto, L. Bacterial colonization patterns in mechanically ventilated patients with traumatic and medical head injury. Am. J. Respir. Crit. Care Med. 1999, 159, 188–198. [Google Scholar] [CrossRef] [PubMed]
- Giantsou, E.; Liratzopoulos, N.; Efraimidou, E.; Panopoulou, M.; Alepopoulou, E.; Kartali-Ktenidou, S.; Minopoulos, G.I.; Zakynthinos, S.; Manolas, K.I. Both early-onset and late-onset ventilator-associated pneumonia are caused mainly by potentially multiresistant bacteria. Intensive Care Med. 2005, 31, 1488–1494. [Google Scholar] [CrossRef] [PubMed]
- Ibrahim, E.H.; Ward, S.; Sherman, G.; Kollef, M.H. A comparative analysis of patients with early-onset vs. late-onset nosocomial pneumonia in the ICU setting. Chest. 2000, 117, 1434–1442. [Google Scholar] [CrossRef] [PubMed]
- Koulenti, D.; Tsigou, E.; Rello, J. Nosocomial pneumonia in 27 ICUs in Europe: Perspectives from the EU-VAP/CAP study. Eur. J. Clin. Microbiol. Infect. Dis. 2016. [Google Scholar] [CrossRef] [PubMed]
- Jones, R.N. Microbial etiologies of hospital-acquired bacterial pneumonia and ventilator-associated bacterial pneumonia. Clin. Infect. Dis. 2010, 51, S81–S87. [Google Scholar] [CrossRef] [PubMed]
- Torres, A.; Aznar, R.; Gatell, J.M.; Jiménez, P.; González, J.; Ferrer, A.; Celis, R.; Rodriguez-Roisin, R. Incidence, risk, and prognosis factors of nosocomial pneumonia in mechanically ventilated patients. Am. Rev. Respir. Dis. 1990, 142, 523–528. [Google Scholar] [CrossRef] [PubMed]
- Micek, S.T.; Kollef, M.H.; Torres, A.; Chen, C.; Rello, J.; Chastre, J.; Antonelli, M.; Welte, T.; Clair, B.; Ostermann, H.; et al. Pseudomonas aeruginosa nosocomial pneumonia: Impact of pneumonia classification. Infect. Control Hosp. Epidemiol. 2015, 36, 1190–1197. [Google Scholar] [CrossRef] [PubMed]
- Nair, G.B.; Niederman, M.S. Nosocomial pneumonia: Lessons learned. Crit. Care Clin. 2013, 29, 521–546. [Google Scholar] [CrossRef] [PubMed]
- Torres, A.; Carlet, J. Ventilator-associated pneumonia. European Task Force on ventilator-associated pneumonia. Eur. Respir. J. 2001, 17, 1034–1045. [Google Scholar] [PubMed]
- Combes, A.; Figliolini, C.; Trouillet, J.L.; Kassis, N.; Wolff, M.; Gibert, C.; Chastre, J. Incidence and outcome of polymicrobial ventilator-associated pneumonia. Chest 2002, 121, 1618–1623. [Google Scholar] [CrossRef] [PubMed]
- Ferrer, M.; Difrancesco, L.F.; Liapikou, A.; Rinaudo, M.; Carbonara, M.; Li, B.G.; Gabarrus, A.; Torres, A. Polymicrobial intensive care unit-acquired pneumonia: Prevalence, microbiology and outcome. Crit. Care 2015, 19, 450. [Google Scholar] [CrossRef] [PubMed]
- Martin-Loeches, I.; Torres, A.; Rinaudo, M.; Terraneo, S.; de, R.F.; Ramirez, P.; Diaz, E.; Fernandez-Barat, L.; Li Bassi, G.L.; Ferrer, M. Resistance patterns and outcomes in intensive care unit (ICU)-acquired pneumonia. Validation of European Centre for Disease Prevention and Control (ECDC) and the Centers for Disease Control and Prevention (CDC) classification of multidrug resistant organisms. J. Infect. 2015, 70, 213–222. [Google Scholar] [PubMed]
- Hohenthal, U.; Sipila, J.; Vainionpaa, R.; Meurman, O.; Rantakokko-Jalava, K.; Nikoskelainen, J.; Kotilainen, P. Diagnostic value of bronchoalveolar lavage in community-acquired pneumonia in a routine setting: A study on patients treated in a Finnish university hospital. Scand. J. Infect. Dis. 2004, 36, 198–203. [Google Scholar] [CrossRef] [PubMed]
- Resti, M.; Micheli, A.; Moriondo, M.; Becciolini, L.; Cortimiglia, M.; Canessa, C.; Indolfi, G.; Bartolini, E.; de, M.M.; Azzari, C. Comparison of the effect of antibiotic treatment on the possibility of diagnosing invasive pneumococcal disease by culture or molecular methods: A prospective, observational study of children and adolescents with proven pneumococcal infection. Clin. Ther. 2009, 31, 1266–1273. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.F.; Gao, Y.; Chen, M.F.; Cao, B.; Yang, X.H.; Wei, L. Etiological analysis and predictive diagnostic model building of community-acquired pneumonia in adult outpatients in Beijing, China. BMC Infect. Dis. 2013, 13, 309. [Google Scholar] [CrossRef] [PubMed]
- Waterer, G.W.; Wunderink, R.G. The influence of the severity of community-acquired pneumonia on the usefulness of blood cultures. Respir. Med. 2001, 95, 78–82. [Google Scholar] [CrossRef] [PubMed]
- Roson, B.; Carratala, J.; Fernandez-Sabe, N.; Tubau, F.; Manresa, F.; Gudiol, F. Causes and factors associated with early failure in hospitalized patients with community-acquired pneumonia. Arch. Intern. Med. 2004, 164, 502–508. [Google Scholar] [CrossRef] [PubMed]
- Andreo, F.; Dominguez, J.; Ruiz-Manzano, J.; Prat, C.; Blanco, S.; Lores, L.; Sanchez, M.D.; Latorre, I.; Gimenez, M.; Ausina, V. Usefulness of pneumococcal antigen detection in pleural fluid samples by immunochromatographic assay for diagnosis of pneumococcal pneumonia. Clin. Microbiol. Infect. 2006, 12, 682–684. [Google Scholar] [CrossRef] [PubMed]
- Falguera, M.; Lopez, A.; Nogues, A.; Porcel, J.M.; Rubio-Caballero, M. Evaluation of the polymerase chain reaction method for detection of Streptococcus pneumoniae DNA in pleural fluid samples. Chest 2002, 122, 2212–2216. [Google Scholar] [CrossRef] [PubMed]
- Falguera, M.; Trujillano, J.; Caro, S.; Menendez, R.; Carratala, J.; Ruiz-Gonzalez, A.; Vila, M.; Garcia, M.; Porcel, J.M.; Torres, A. A prediction rule for estimating the risk of bacteremia in patients with community-acquired pneumonia. Clin. Infect. Dis. 2009, 49, 409–416. [Google Scholar] [CrossRef] [PubMed]
- Torres, A.; Cilloniz, C.; Ferrer, M.; Gabarrus, A.; Polverino, E.; Villegas, S.; Marco, F.; Mensa, J.; Menendez, R.; Niederman, M. Bacteraemia and antibiotic-resistant pathogens in community acquired pneumonia: Risk and prognosis. Eur. Respir. J. 2015, 45, 1353–1363. [Google Scholar] [CrossRef] [PubMed]
- Roson, B.; Carratala, J.; Verdaguer, R.; Dorca, J.; Manresa, F.; Gudiol, F. Prospective study of the usefulness of sputum Gram stain in the initial approach to community-acquired pneumonia requiring hospitalization. Clin. Infect. Dis. 2000, 31, 869–874. [Google Scholar] [CrossRef] [PubMed]
- Anevlavis, S.; Petroglou, N.; Tzavaras, A.; Maltezos, E.; Pneumatikos, I.; Froudarakis, M.; Anevlavis, E.; Bouros, D. A prospective study of the diagnostic utility of sputum Gram stain in pneumonia. J. Infect. 2009, 59, 83–89. [Google Scholar] [CrossRef] [PubMed]
- Cook, D.; Mandell, L. Endotracheal aspiration in the diagnosis of ventilator-associated pneumonia. Chest 2000, 117, 195S–197S. [Google Scholar] [CrossRef] [PubMed]
- Saukkoriipi, A.; Pascal, T.; Palmu, A.A. Evaluation of the BinaxNOW(R) Streptococcus pneumoniae antigen test on fresh, frozen and concentrated urine samples in elderly patients with and without community-acquired pneumonia. J. Microbiol. Methods 2016, 121, 24–26. [Google Scholar] [CrossRef] [PubMed]
- Schulte, B.; Eickmeyer, H.; Heininger, A.; Juretzek, S.; Karrasch, M.; Denis, O.; Roisin, S.; Pletz, M.W.; Klein, M.; Barth, S.; et al. Detection of pneumonia associated pathogens using a prototype multiplexed pneumonia test in hospitalized patients with severe pneumonia. PLoS ONE 2014, 9, e110566. [Google Scholar] [CrossRef] [PubMed]
- Scanvic, A.; Courdavault, L.; Sollet, J.P.; Le, T.F. Interest of real-time PCR Xpert MRSA/SA on GeneXpert((R)) DX System in the investigation of staphylococcal bacteremia]. Pathol. Biol. (Paris) 2011, 59, 67–72. [Google Scholar] [CrossRef] [PubMed]
- Wellinghausen, N.; Siegel, D.; Gebert, S.; Winter, J. Rapid detection of Staphylococcus aureus bacteremia and methicillin resistance by real-time PCR in whole blood samples. Eur. J. Clin. Microbiol. Infect. Dis. 2009, 28, 1001–1005. [Google Scholar] [CrossRef] [PubMed]
- Mok, J.H.; Eom, J.S.; Jo, E.J.; Kim, M.H.; Lee, K.; Kim, K.U.; Park, H.K.; Yi, J.; Lee, M.K. Clinical utility of rapid pathogen identification using matrix-assisted laser desorption/ionization time-of-flight mass spectrometry in ventilated patients with pneumonia: A pilot study. Respirology 2016, 21, 321–328. [Google Scholar] [CrossRef] [PubMed]
- Gadsby, N.J.; Russell, C.D.; McHugh, M.P.; Mark, H.; Conway, M.A.; Laurenson, I.F.; Hill, A.T.; Templeton, K.E. Comprehensive Molecular Testing for Respiratory Pathogens in Community-Acquired Pneumonia. Clin. Infect. Dis. 2016, 62, 817–823. [Google Scholar] [CrossRef] [PubMed]




| Condition of Pneumonia | Blood Cultures | Respiratory Samples | Urinary Antigen Test for Legionella/Pneumococcus | Comments |
|---|---|---|---|---|
| Outpatient | Sputum culture | Serology test when pathogens are suspected through epidemiological evidence | ||
| Hospitalized patients (ward) | × | × | × | Influenza test during influenza season |
| Hospitalized patients admitted to ICU | × | BAL/BAS in intubated patients | × | Serology test when pathogens are suspected through epidemiological evidence |
| Failure of outpatient antibiotic treatment | Sputum culture | × | Serology for intracellular pathogens | |
| CAP cases who do not respond to treatment or suspicion of uncommon pathogens | × | BAL Mycobacterial and mycological culture Nasopharyngeal swab for respiratory viruses | ||
| Hospital acquired pneumonia | × | × | × | Influenza test during influenza season |
| Ventilator associated pneumonia | × | BAS/BAL/mini BAL | × |
| Platform | Pathogens | Technology | Sensibility/Specificity | Time | Sample | Advantages | Disadvantages | Approved |
|---|---|---|---|---|---|---|---|---|
| Curetis Unyvero P50 Pneumonia | 18 bacterial and fungal pathogens 22 antibiotic resistance markers | Multiplex-PCR cartridge system | 81%/99% | 4 h | Sputum, BAL, BAS | Detection of resistant patterns | Test limited to a two samples test per run. A relatively large amount of hands-on time | Under FDA/EC/Under Singapore Registration/Under Chinese Registration |
| GeneXpertMRSA/SA | Methicillin-resistant S. aureus (MRSA) methicillin-sensitive S. aureus (MSSA) | Multiplex-PCR | 99%/72% | 1 h | Blood, Nasal swabs | Minimal technical expertise | Only detects MRSA/SA | FDA/EC |
| MALDI-TOF | 200 microorganisms | Mass spectrometry, identification of microorganisms directly from colonies of bacteria and fungi | 99%–100%/97%–100% | 0.5–1 min | Colonies, positive blood cultures, direct samples such as urine | Rapid and accurate approach to detect microorganism | Lack of standardized assay conditions | |
| GeneXpert Flu Assay | Influenza A/B (A/2009H1) | multiplex-PCR | 97%–100%/100% | 1 h | Nasopharyngeal swabs, nasal aspirates and washes | Minimal technical expertise | Only detects influenza viruses | FDA/EC |
| GeneXpert Flu/RSV Assay | Influenza A/B/RSV | Multiplex-PCR | 97%–100%/100% | 0.5–1 h | Nasopharyngeal swabs, nasal aspirates and washes | Minimal technical expertise | Only detects influenza viruses and RSV | FDA/EC |
| FilmArray Respiratory Panel | Adenovirus; coronaviruses 229E, OC43, NL63, HKU1; metapneumovirus; influenza A, H3, H1, 2009 H1; parainfluenza viruses 1, 2, 3, 4; RSV; rhinovirus/enterovirus B. pertussis, M. pneumoniae, C. pneumoniae | An unprocessed biologic/clinical sample is subjected to nucleic acid purification, reverse transcription, a high-order nested multiplex PCR and DNA melting curve analysis | 84%–100%/98%–100% | 1 h | Nasopharyngeal Swab | Minimal technical expertise required | Test limited to a single patient test per run. Decreased sensitivity for some adenovirus types | FDA/ EC |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cilloniz, C.; Martin-Loeches, I.; Garcia-Vidal, C.; San Jose, A.; Torres, A. Microbial Etiology of Pneumonia: Epidemiology, Diagnosis and Resistance Patterns. Int. J. Mol. Sci. 2016, 17, 2120. https://doi.org/10.3390/ijms17122120
Cilloniz C, Martin-Loeches I, Garcia-Vidal C, San Jose A, Torres A. Microbial Etiology of Pneumonia: Epidemiology, Diagnosis and Resistance Patterns. International Journal of Molecular Sciences. 2016; 17(12):2120. https://doi.org/10.3390/ijms17122120
Chicago/Turabian StyleCilloniz, Catia, Ignacio Martin-Loeches, Carolina Garcia-Vidal, Alicia San Jose, and Antoni Torres. 2016. "Microbial Etiology of Pneumonia: Epidemiology, Diagnosis and Resistance Patterns" International Journal of Molecular Sciences 17, no. 12: 2120. https://doi.org/10.3390/ijms17122120
APA StyleCilloniz, C., Martin-Loeches, I., Garcia-Vidal, C., San Jose, A., & Torres, A. (2016). Microbial Etiology of Pneumonia: Epidemiology, Diagnosis and Resistance Patterns. International Journal of Molecular Sciences, 17(12), 2120. https://doi.org/10.3390/ijms17122120