Prognostic and Predictive Biomarkers in Stage III Melanoma: Current Insights and Clinical Implications
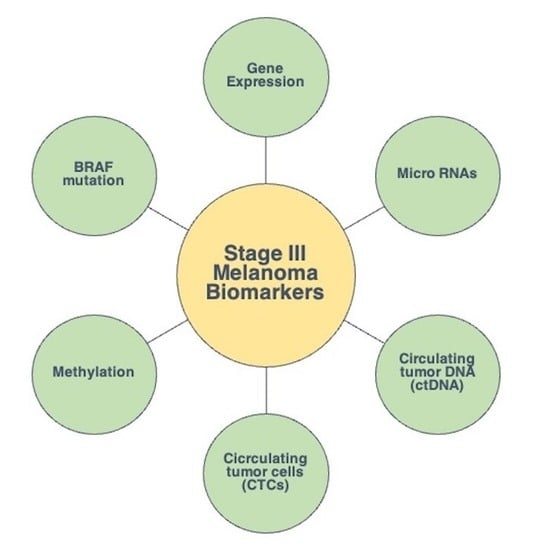
Abstract
:1. Introduction
1.1. Conventional Clinico-Pathologic Markers and Staging
1.2. Gene Expression
1.3. Micro-RNA
1.4. Circulating Tumour DNA
1.5. Circulating Tumour Cells
1.6. Methylation
2. BRAF Mutation
3. Protein Expression
4. Future Perspectives
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Schadendorf, D.; van Akkooi, A.C.J.; Berking, C.; Griewank, K.G.; Gutzmer, R.; Hauschild, A.; Stang, A.; Roesch, A.; Ugurel, S. Melanoma. Lancet 2018, 392, 971–984. [Google Scholar] [CrossRef]
- Ribero, S.; Longo, C.; Glass, D.; Nathan, P.; Bataille, V. What Is New in Melanoma Genetics and Treatment? Dermatology 2016, 232, 259–264. [Google Scholar] [CrossRef] [PubMed]
- Gandini, S.; Sera, F.; Cattaruzza, M.S.; Pasquini, P.; Abeni, D.; Boyle, P.; Melchi, C.F. Meta-Analysis of Risk Factors for Cutaneous Melanoma: I. Common and Atypical Naevi. Eur. J. Cancer 2005, 41, 28–44. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gandini, S.; Sera, F.; Cattaruzza, M.S.; Pasquini, P.; Picconi, O.; Boyle, P.; Melchi, C.F. Meta-Analysis of Risk Factors for Cutaneous Melanoma: II. Sun Exposure. Eur. J. Cancer 2005, 41, 45–60. [Google Scholar] [CrossRef] [PubMed]
- Jiang, A.J.; Rambhatla, P.V.; Eide, M.J. Socioeconomic and Lifestyle Factors and Melanoma: A Systematic Review. Br. J. Dermatol. 2015, 172, 885–915. [Google Scholar] [CrossRef] [PubMed]
- Barreiro-Capurro, A.; Andrés-Lencina, J.J.; Podlipnik, S.; Carrera, C.; Requena, C.; Manrique-Silva, E.; Quaglino, P.; Tonella, L.; Jaka, A.; Richarz, N.; et al. Differences in Cutaneous Melanoma Survival between the 7th and 8th Edition of the American Joint Committee on Cancer (AJCC). A Multicentric Population-Based Study. Eur. J. Cancer 2021, 145, 29–37. [Google Scholar] [CrossRef] [PubMed]
- Gershenwald, J.E.; Scolyer, R.A.; Hess, K.R.; Sondak, V.K.; Long, G.V.; Ross, M.I.; Lazar, A.J.; Faries, M.B.; Kirkwood, J.M.; McArthur, G.A.; et al. Melanoma Staging: Evidence-Based Changes in the American Joint Committee on Cancer Eighth Edition Cancer Staging Manual: Melanoma Staging: AJCC 8th Edition. CA Cancer J. Clin. 2017, 67, 472–492. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kirkwood, J.M.; Strawderman, M.H.; Ernstoff, M.S.; Smith, T.J.; Borden, E.C.; Blum, R.H. Interferon Alfa-2b Adjuvant Therapy of High-Risk Resected Cutaneous Melanoma: The Eastern Cooperative Oncology Group Trial EST 1684. J. Clin. Oncol. 1996, 14, 7–17. [Google Scholar] [CrossRef]
- Eggermont, A.M.M.; Suciu, S.; Rutkowski, P.; Kruit, W.H.; Punt, C.J.; Dummer, R.; Salès, F.; Keilholz, U.; de Schaetzen, G.; Testori, A. Long Term Follow up of the EORTC 18952 Trial of Adjuvant Therapy in Resected Stage IIB–III Cutaneous Melanoma Patients Comparing Intermediate Doses of Interferon-Alpha-2b (IFN) with Observation: Ulceration of Primary Is Key Determinant for IFN-Sensitivity. Eur. J. Cancer 2016, 55, 111–121. [Google Scholar] [CrossRef]
- Sanlorenzo, M.; Vujic, I.; Carnevale-Schianca, F.; Quaglino, P.; Gammaitoni, L.; Fierro, M.T.; Aglietta, M.; Sangiolo, D. Role of Interferon in Melanoma: Old Hopes and New Perspectives. Expert Opin. Biol. Ther. 2017, 17, 475–483. [Google Scholar] [CrossRef]
- Eggermont, A.M.M.; Blank, C.U.; Mandala, M.; Long, G.V.; Atkinson, V.; Dalle, S.; Haydon, A.; Lichinitser, M.; Khattak, A.; Carlino, M.S.; et al. Adjuvant Pembrolizumab versus Placebo in Resected Stage III Melanoma. N. Engl. J. Med. 2018, 378, 1789–1801. [Google Scholar] [CrossRef]
- Ascierto, P.A.; Del Vecchio, M.; Mandalá, M.; Gogas, H.; Arance, A.M.; Dalle, S.; Cowey, C.L.; Schenker, M.; Grob, J.-J.; Chiarion-Sileni, V.; et al. Adjuvant Nivolumab versus Ipilimumab in Resected Stage IIIB–C and Stage IV Melanoma (CheckMate 238): 4-Year Results from a Multicentre, Double-Blind, Randomised, Controlled, Phase 3 Trial. Lancet Oncol. 2020, 21, 1465–1477. [Google Scholar] [CrossRef]
- Dummer, R.; Brase, J.C.; Garrett, J.; Campbell, C.D.; Gasal, E.; Squires, M.; Gusenleitner, D.; Santinami, M.; Atkinson, V.; Mandalà, M.; et al. Adjuvant Dabrafenib plus Trametinib versus Placebo in Patients with Resected, BRAFV600-Mutant, Stage III Melanoma (COMBI-AD): Exploratory Biomarker Analyses from a Randomised, Phase 3 Trial. Lancet Oncol. 2020, 21, 358–372. [Google Scholar] [CrossRef]
- Long, G.V.; Hauschild, A.; Santinami, M.; Atkinson, V.; Mandalà, M.; Chiarion-Sileni, V.; Larkin, J.; Nyakas, M.; Dutriaux, C.; Haydon, A.; et al. Adjuvant Dabrafenib plus Trametinib in Stage III BRAF-Mutated Melanoma. N. Engl. J. Med. 2017, 377, 1813–1823. [Google Scholar] [CrossRef] [Green Version]
- Weber, J.; Mandala, M.; Del Vecchio, M.; Gogas, H.J.; Arance, A.M.; Cowey, C.L.; Dalle, S.; Schenker, M.; Chiarion-Sileni, V.; Marquez-Rodas, I.; et al. Adjuvant Nivolumab versus Ipilimumab in Resected Stage III or IV Melanoma. N. Engl. J. Med. 2017, 377, 1824–1835. [Google Scholar] [CrossRef]
- Oldenhuis, C.N.A.M.; Oosting, S.F.; Gietema, J.A.; de Vries, E.G.E. Prognostic versus Predictive Value of Biomarkers in Oncology. Eur. J. Cancer 2008, 44, 946–953. [Google Scholar] [CrossRef]
- Pasquali, S.; Mocellin, S.; Mozzillo, N.; Maurichi, A.; Quaglino, P.; Borgognoni, L.; Solari, N.; Piazzalunga, D.; Mascheroni, L.; Giudice, G.; et al. Nonsentinel Lymph Node Status in Patients with Cutaneous Melanoma: Results from a Multi-Institution Prognostic Study. J. Clin. Oncol. 2014, 32, 935–941. [Google Scholar] [CrossRef]
- Keung, E.Z.; Gershenwald, J.E. The Eighth Edition American Joint Committee on Cancer (AJCC) Melanoma Staging System: Implications for Melanoma Treatment and Care. Expert Rev. Anticancer Ther. 2018, 18, 775–784. [Google Scholar] [CrossRef]
- Ribero, S.; Torres-Navarro, I.; Botella-Estrada, R. Tumour-Infiltrating Lymphocyte and Histological Regression in Primary Melanoma. Arch. Dermatol. Res. 2021, 313, 63–64. [Google Scholar] [CrossRef]
- Gualano, M.R.; Osella-Abate, S.; Scaioli, G.; Marra, E.; Bert, F.; Faure, E.; Baduel, E.S.; Balagna, E.; Quaglino, P.; Fierro, M.T.; et al. Prognostic Role of Histological Regression in Primary Cutaneous Melanoma: A Systematic Review and Meta-Analysis. Br. J. Dermatol. 2018, 178, 357–362. [Google Scholar] [CrossRef]
- Osella-Abate, S.; Conti, L.; Annaratone, L.; Senetta, R.; Bertero, L.; Licciardello, M.; Caliendo, V.; Picciotto, F.; Quaglino, P.; Cassoni, P.; et al. Phenotypic Characterisation of Immune Cells Associated with Histological Regression in Cutaneous Melanoma. Pathology 2019, 51, 487–493. [Google Scholar] [CrossRef] [Green Version]
- Osella-Abate, S.; Vignale, C.; Annaratone, L.; Nocifora, A.; Bertero, L.; Castellano, I.; Avallone, G.; Conti, L.; Quaglino, P.; Picciotto, F.; et al. Microenvironment in Cutaneous Melanomas: A Gene Expression Profile Study May Explain the Role of Histological Regression. J. Eur. Acad. Dermatol. Venereol. 2021, 35. [Google Scholar] [CrossRef] [PubMed]
- Mann, G.J.; Pupo, G.M.; Campain, A.E.; Carter, C.D.; Schramm, S.-J.; Pianova, S.; Gerega, S.K.; De Silva, C.; Lai, K.; Wilmott, J.S.; et al. BRAF Mutation, NRAS Mutation, and the Absence of an Immune-Related Expressed Gene Profile Predict Poor Outcome in Patients with Stage III Melanoma. J. Investig. Dermatol. 2013, 133, 509–517. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- John, T.; Black, M.A.; Toro, T.T.; Leader, D.; Gedye, C.A.; Davis, I.D.; Guilford, P.J.; Cebon, J.S. Predicting Clinical Outcome through Molecular Profiling in Stage III Melanoma. Clin. Cancer Res. 2008, 14, 5173–5180. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bogunovic, D.; O’Neill, D.W.; Belitskaya-Levy, I.; Vacic, V.; Yu, Y.-L.; Adams, S.; Darvishian, F.; Berman, R.; Shapiro, R.; Pavlick, A.C.; et al. Immune Profile and Mitotic Index of Metastatic Melanoma Lesions Enhance Clinical Staging in Predicting Patient Survival. Proc. Natl. Acad. Sci. USA 2009, 106, 20429–20434. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zager, J.S.; Gastman, B.R.; Leachman, S.; Gonzalez, R.C.; Fleming, M.D.; Ferris, L.K.; Ho, J.; Miller, A.R.; Cook, R.W.; Covington, K.R.; et al. Performance of a Prognostic 31-Gene Expression Profile in an Independent Cohort of 523 Cutaneous Melanoma Patients. BMC Cancer 2018, 18, 130. [Google Scholar] [CrossRef] [PubMed]
- Journe, F.; Boufker, H.I.; Van Kempen, L.; Galibert, M.-D.; Wiedig, M.; Salès, F.; Theunis, A.; Nonclercq, D.; Frau, A.; Laurent, G.; et al. TYRP1 MRNA Expression in Melanoma Metastases Correlates with Clinical Outcome. Br. J. Cancer 2011, 105, 1726–1732. [Google Scholar] [CrossRef] [Green Version]
- El Hajj, P.; Journe, F.; Wiedig, M.; Laios, I.; Salès, F.; Galibert, M.-D.; Van Kempen, L.C.; Spatz, A.; Badran, B.; Larsimont, D.; et al. Tyrosinase-Related Protein 1 MRNA Expression in Lymph Node Metastases Predicts Overall Survival in High-Risk Melanoma Patients. Br. J. Cancer 2013, 108, 1641–1647. [Google Scholar] [CrossRef] [Green Version]
- Segura, M.F.; Belitskaya-Lévy, I.; Rose, A.E.; Zakrzewski, J.; Gaziel, A.; Hanniford, D.; Darvishian, F.; Berman, R.S.; Shapiro, R.L.; Pavlick, A.C.; et al. Melanoma MicroRNA Signature Predicts Post-Recurrence Survival. Clin. Cancer Res. 2010, 16, 1577–1586. [Google Scholar] [CrossRef] [Green Version]
- Sánchez-Sendra, B.; García-Giménez, J.L.; González-Muñoz, J.F.; Navarro, L.; Murgui, A.; Terrádez, L.; Pinazo, I.; Martin, J.M.; Monteagudo, C. Circulating Mi RNA Expression Analysis Reveals New Potential Biomarkers for Human Cutaneous Melanoma Staging. J. Eur. Acad. Dermatol. Venereol. 2020, 34. [Google Scholar] [CrossRef]
- Huber, V.; Vallacchi, V.; Fleming, V.; Hu, X.; Cova, A.; Dugo, M.; Shahaj, E.; Sulsenti, R.; Vergani, E.; Filipazzi, P.; et al. Tumor-Derived MicroRNAs Induce Myeloid Suppressor Cells and Predict Immunotherapy Resistance in Melanoma. J. Clin. Investig. 2018, 128, 5505–5516. [Google Scholar] [CrossRef] [Green Version]
- Fattore, L.; Mancini, R.; Acunzo, M.; Romano, G.; Laganà, A.; Pisanu, M.E.; Malpicci, D.; Madonna, G.; Mallardo, D.; Capone, M.; et al. MiR-579-3p Controls Melanoma Progression and Resistance to Target Therapy. Proc. Natl. Acad. Sci. USA 2016, 113, E5005–E5013. [Google Scholar] [CrossRef] [Green Version]
- Marczynski, G.T.; Laus, A.C.; dos Reis, M.B.; Reis, R.M.; De Vazquez, V.L. Circulating Tumor DNA (CtDNA) Detection Is Associated with Shorter Progression-Free Survival in Advanced Melanoma Patients. Sci. Rep. 2020, 10, 18682. [Google Scholar] [CrossRef]
- Lee, J.H.; Saw, R.P.; Thompson, J.F.; Lo, S.; Spillane, A.J.; Shannon, K.F.; Stretch, J.R.; Howle, J.; Menzies, A.M.; Carlino, M.S.; et al. Pre-Operative CtDNA Predicts Survival in High-Risk Stage III Cutaneous Melanoma Patients. Ann. Oncol. 2019, 30, 815–822. [Google Scholar] [CrossRef]
- Tan, L.; Sandhu, S.; Lee, R.J.; Li, J.; Callahan, J.; Ftouni, S.; Dhomen, N.; Middlehurst, P.; Wallace, A.; Raleigh, J.; et al. Prediction and Monitoring of Relapse in Stage III Melanoma Using Circulating Tumor DNA. Ann. Oncol. 2019, 30, 804–814. [Google Scholar] [CrossRef]
- Lee, R.J.; Gremel, G.; Marshall, A.; Myers, K.A.; Fisher, N.; Dunn, J.A.; Dhomen, N.; Corrie, P.G.; Middleton, M.R.; Lorigan, P.; et al. Circulating Tumor DNA Predicts Survival in Patients with Resected High-Risk Stage II/III Melanoma. Ann. Oncol. 2018, 29, 490–496. [Google Scholar] [CrossRef] [Green Version]
- Gandini, S.; Zanna, I.; De Angelis, S.P.; Cocorocchio, E.; Queirolo, P.; Lee, J.H.; Carlino, M.S.; Mazzarella, L.; Achutti Duso, B.; Palli, D.; et al. Circulating Tumour DNA and Melanoma Survival: A Systematic Literature Review and Meta-Analysis. Crit. Rev. Oncol. Hematol. 2021, 157, 103187. [Google Scholar] [CrossRef]
- Koyanagi, K.; O’Day, S.J.; Gonzalez, R.; Lewis, K.; Robinson, W.A.; Amatruda, T.T.; Wang, H.-J.; Elashoff, R.M.; Takeuchi, H.; Umetani, N.; et al. Serial Monitoring of Circulating Melanoma Cells During Neoadjuvant Biochemotherapy for Stage III Melanoma: Outcome Prediction in a Multicenter Trial. J. Clin. Oncol. 2005, 23, 8057–8064. [Google Scholar] [CrossRef] [Green Version]
- Hoshimoto, S.; Shingai, T.; Morton, D.L.; Kuo, C.; Faries, M.B.; Chong, K.; Elashoff, D.; Wang, H.-J.; Elashoff, R.M.; Hoon, D.S.B. Association Between Circulating Tumor Cells and Prognosis in Patients With Stage III Melanoma With Sentinel Lymph Node Metastasis in a Phase III International Multicenter Trial. J. Clin. Oncol. 2012, 30, 3819–3826. [Google Scholar] [CrossRef] [Green Version]
- Lucci, A.; Hall, C.S.; Patel, S.P.; Narendran, B.; Bauldry, J.B.; Royal, R.E.; Karhade, M.; Upshaw, J.R.; Wargo, J.A.; Glitza, I.C.; et al. Circulating Tumor Cells and Early Relapse in Node-Positive Melanoma. Clin. Cancer Res. 2020, 26, 1886–1895. [Google Scholar] [CrossRef]
- Lin, S.Y.; Chang, S.-C.; Lam, S.; Irene Ramos, R.; Tran, K.; Ohe, S.; Salomon, M.P.; Bhagat, A.A.S.; Teck Lim, C.; Fischer, T.D.; et al. Prospective Molecular Profiling of Circulating Tumor Cells from Patients with Melanoma Receiving Combinatorial Immunotherapy. Clin. Chem. 2020, 66, 169–177. [Google Scholar] [CrossRef] [PubMed]
- Sigalotti, L.; Fratta, E.; Bidoli, E.; Covre, A.; Parisi, G.; Colizzi, F.; Coral, S.; Massarut, S.; Kirkwood, J.M.; Maio, M. Methylation Levels of the “Long Interspersed Nucleotide Element-1” Repetitive Sequences Predict Survival of Melanoma Patients. J. Transl. Med. 2011, 9, 78. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sigalotti, L.; Covre, A.; Fratta, E.; Parisi, G.; Sonego, P.; Colizzi, F.; Coral, S.; Massarut, S.; Kirkwood, J.M.; Maio, M. Whole Genome Methylation Profiles as Independent Markers of Survival in Stage IIIC Melanoma Patients. J. Transl. Med. 2012, 10, 185. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hoshimoto, S.; Kuo, C.T.; Chong, K.K.; Takeshima, T.-L.; Takei, Y.; Li, M.W.; Huang, S.K.; Sim, M.-S.; Morton, D.L.; Hoon, D.S.B. AIM1 and LINE-1 Epigenetic Aberrations in Tumor and Serum Relate to Melanoma Progression and Disease Outcome. J. Investig. Dermatol. 2012, 132, 1689–1697. [Google Scholar] [CrossRef] [Green Version]
- Tanemura, A.; Terando, A.M.; Sim, M.-S.; van Hoesel, A.Q.; de Maat, M.F.G.; Morton, D.L.; Hoon, D.S.B. CpG Island Methylator Phenotype Predicts Progression of Malignant Melanoma. Clin. Cancer Res. 2009, 15, 1801–1807. [Google Scholar] [CrossRef] [Green Version]
- Guadagni, S.; Fiorentini, G.; Clementi, M.; Palumbo, G.; Masedu, F.; Deraco, M.; De Manzoni, G.; Chiominto, A.; Valenti, M.; Pellegrini, C. MGMT Methylation Correlates with Melphalan Pelvic Perfusion Survival in Stage III Melanoma Patients: A Pilot Study. Melanoma Res. 2017, 27, 439–447. [Google Scholar] [CrossRef] [Green Version]
- Barbour, A.P.; Tang, Y.H.; Armour, N.; Dutton-Regester, K.; Krause, L.; Loffler, K.A.; Lambie, D.; Burmeister, B.; Thomas, J.; Smithers, B.M.; et al. BRAF Mutation Status Is an Independent Prognostic Factor for Resected Stage IIIB and IIIC Melanoma: Implications for Melanoma Staging and Adjuvant Therapy. Eur. J. Cancer 2014, 50, 2668–2676. [Google Scholar] [CrossRef]
- Picard, M.; Pham Dang, N.; D’Incan, M.; Mansard, S.; Dechelotte, P.; Pereira, B.; Mondie, J.M.; Barthelemy, I. Is BRAF a Prognostic Factor in Stage III Skin Melanoma? A Retrospective Study of 72 Patients after Positive Sentinel Lymph Node Dissection. Br. J. Dermatol. 2014, 171, 108–114. [Google Scholar] [CrossRef]
- Moreau, S.; Saiag, P.; Aegerter, P.; Bosset, D.; Longvert, C.; Hélias-Rodzewicz, Z.; Marin, C.; Peschaud, F.; Chagnon, S.; Zimmermann, U.; et al. Prognostic Value of BRAF V600 Mutations in Melanoma Patients After Resection of Metastatic Lymph Nodes. Ann. Surg. Oncol. 2012, 19, 4314–4321. [Google Scholar] [CrossRef]
- Eggermont, A.M.M.; Blank, C.U.; Mandala, M.; Long, G.V.; Atkinson, V.G.; Dalle, S.; Haydon, A.M.; Meshcheryakov, A.; Khattak, A.; Carlino, M.S.; et al. Longer Follow-Up Confirms Recurrence-Free Survival Benefit of Adjuvant Pembrolizumab in High-Risk Stage III Melanoma: Updated Results From the EORTC 1325-MG/KEYNOTE-054 Trial. J. Clin. Oncol. 2020, 38, 3925–3936. [Google Scholar] [CrossRef]
- Tas, F.; Erturk, K. BRAF V600E Mutation as a Prognostic Factor in Cutaneous Melanoma Patients. Dermatol. Ther. 2020, 33. [Google Scholar] [CrossRef]
- Heppt, M.V.; Siepmann, T.; Engel, J.; Schubert-Fritschle, G.; Eckel, R.; Mirlach, L.; Kirchner, T.; Jung, A.; Gesierich, A.; Ruzicka, T.; et al. Prognostic Significance of BRAF and NRAS Mutations in Melanoma: A German Study from Routine Care. BMC Cancer 2017, 17, 536. [Google Scholar] [CrossRef]
- Mactier, S.; Kaufman, K.L.; Wang, P.; Crossett, B.; Pupo, G.M.; Kohnke, P.L.; Thompson, J.F.; Scolyer, R.A.; Yang, J.Y.; Mann, G.J.; et al. Protein Signatures Correspond to Survival Outcomes of AJCC Stage III Melanoma Patients. Pigment. Cell Melanoma Res. 2014, 27, 1106–1116. [Google Scholar] [CrossRef]
- Karonidis, A.; Mantzourani, M.; Gogas, H.; Tsoutsos, D. Serum S100B Levels Correlate with Stage, N Status, Mitotic Rate and Disease Outcome in Melanoma Patients Independent to LDH. 7. J. BUON 2017, 22, 1296–1302. [Google Scholar]
- Wagner, N.B.; Weide, B.; Gries, M.; Reith, M.; Tarnanidis, K.; Schuermans, V.; Kemper, C.; Kehrel, C.; Funder, A.; Lichtenberger, R.; et al. Tumor Microenvironment-Derived S100A8/A9 Is a Novel Prognostic Biomarker for Advanced Melanoma Patients and during Immunotherapy with Anti-PD-1 Antibodies. J. Immunother. Cancer 2019, 7, 343. [Google Scholar] [CrossRef]
- Madore, J.; Strbenac, D.; Vilain, R.; Menzies, A.M.; Yang, J.Y.H.; Thompson, J.F.; Long, G.V.; Mann, G.J.; Scolyer, R.A.; Wilmott, J.S. PD-L1 Negative Status Is Associated with Lower Mutation Burden, Differential Expression of Immune-Related Genes, and Worse Survival in Stage III Melanoma. Clin. Cancer Res. 2016, 22, 3915–3923. [Google Scholar] [CrossRef] [Green Version]
- Ekmekcioglu, S.; Davies, M.A.; Tanese, K.; Roszik, J.; Shin-Sim, M.; Bassett, R.L.; Milton, D.R.; Woodman, S.E.; Prieto, V.G.; Gershenwald, J.E.; et al. Inflammatory Marker Testing Identifies CD74 Expression in Melanoma Tumor Cells, and Its Expression Associates with Favorable Survival for Stage III Melanoma. Clin. Cancer Res. 2016, 22, 3016–3024. [Google Scholar] [CrossRef] [Green Version]
- Ascierto, P.A.; Lewis, K.D.; Di Giacomo, A.M.; Demidov, L.; Mandalà, M.; Bondarenko, I.; Herbert, C.; Mackiewicz, A.; Rutkowski, P.; Guminski, A.; et al. Prognostic Impact of Baseline Tumour Immune Infiltrate on Disease-Free Survival in Patients with Completely Resected, BRAFv600 Mutation–Positive Melanoma Receiving Adjuvant Vemurafenib. Ann. Oncol. 2020, 31, 153–159. [Google Scholar] [CrossRef] [Green Version]
- Lauwyck, J.; Beckwée, A.; Santens, A.; Schwarze, J.K.; Awada, G.; Vandersleyen, V.; Aspeslagh, S.; Neyns, B. 1131P C-Reactive Protein as Biomarker for Immune-Related Adverse Events in Melanoma Patients Treated with Immune Checkpoint Inhibitors in the Adjuvant Setting. Ann. Oncol. 2020, 31, S759. [Google Scholar] [CrossRef]
- Narrandes, S.; Xu, W. Gene Expression Detection Assay for Cancer Clinical Use. J. Cancer 2018, 9, 2249–2265. [Google Scholar] [CrossRef]
- Gerami, P.; Cook, R.W.; Russell, M.C.; Wilkinson, J.; Amaria, R.N.; Gonzalez, R.; Lyle, S.; Jackson, G.L.; Greisinger, A.J.; Johnson, C.E.; et al. Gene Expression Profiling for Molecular Staging of Cutaneous Melanoma in Patients Undergoing Sentinel Lymph Node Biopsy. J. Am. Acad. Dermatol. 2015, 72, 780–785.e3. [Google Scholar] [CrossRef]
- Gilot, D.; Migault, M.; Bachelot, L.; Journé, F.; Rogiers, A.; Donnou-Fournet, E.; Mogha, A.; Mouchet, N.; Pinel-Marie, M.-L.; Mari, B.; et al. A Non-Coding Function of TYRP1 MRNA Promotes Melanoma Growth. Nat. Cell Biol. 2017, 19, 1348–1357. [Google Scholar] [CrossRef]
- Rad, H.H.; Yamashita, T.; Jin, H.-Y.; Hirosaki, K.; Wakamatsu, K.; Ito, S.; Jimbow, K. Tyrosinase-Related Proteins Suppress Tyrosinase-Mediated Cell Death of Melanocytes and Melanoma Cells. Exp. Cell Res. 2004, 298, 317–328. [Google Scholar] [CrossRef]
- Kobayashi, T.; Imokawa, G.; Bennett, D.C.; Hearing, V.J. Tyrosinase Stabilization by Tyrp1 (the Brown Locus Protein). J. Biol. Chem. 1998, 273, 31801–31805. [Google Scholar] [CrossRef] [Green Version]
- Rozeman, E.A.; Hoefsmit, E.P.; Reijers, I.L.M.; Saw, R.P.M.; Versluis, J.M.; Krijgsman, O.; Dimitriadis, P.; Sikorska, K.; van de Wiel, B.A.; Eriksson, H.; et al. Survival and Biomarker Analyses from the OpACIN-Neo and OpACIN Neoadjuvant Immunotherapy Trials in Stage III Melanoma. Nat. Med. 2021, 27, 256–263. [Google Scholar] [CrossRef]
- Dika, E.; Riefolo, M.; Porcellini, E.; Broseghini, E.; Ribero, S.; Senetta, R.; Osella-Abate, S.; Scarfì, F.; Lambertini, M.; Veronesi, G.; et al. Defining the Prognostic Role of MicroRNAs in Cutaneous Melanoma. J. Investig. Dermatol. 2020, 140, 2260–2267. [Google Scholar] [CrossRef]
- Latchana, N.; Ganju, A.; Howard, J.H.; Carson, W.E. MicroRNA Dysregulation in Melanoma. Surg. Oncol. 2016, 25, 184–189. [Google Scholar] [CrossRef]
- Boyer, M.; Cayrefourcq, L.; Dereure, O.; Meunier, L.; Becquart, O.; Alix-Panabières, C. Clinical Relevance of Liquid Biopsy in Melanoma and Merkel Cell Carcinoma. Cancers 2020, 12, 960. [Google Scholar] [CrossRef] [Green Version]
- Aya-Bonilla, C.A.; Morici, M.; Hong, X.; McEvoy, A.C.; Sullivan, R.J.; Freeman, J.; Calapre, L.; Khattak, M.A.; Meniawy, T.; Millward, M.; et al. Detection and Prognostic Role of Heterogeneous Populations of Melanoma Circulating Tumour Cells. Br. J. Cancer 2020, 122, 1059–1067. [Google Scholar] [CrossRef]
- Marsavela, G.; Aya-Bonilla, C.A.; Warkiani, M.E.; Gray, E.S.; Ziman, M. Melanoma Circulating Tumor Cells: Benefits and Challenges Required for Clinical Application. Cancer Lett. 2018, 424, 1–8. [Google Scholar] [CrossRef]
- Micevic, G.; Theodosakis, N.; Bosenberg, M. Aberrant DNA Methylation in Melanoma: Biomarker and Therapeutic Opportunities. Clin. Epigenetics 2017, 9, 34. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ascierto, P.A.; Kirkwood, J.M.; Grob, J.-J.; Simeone, E.; Grimaldi, A.M.; Maio, M.; Palmieri, G.; Testori, A.; Marincola, F.M.; Mozzillo, N. The Role of BRAF V600 Mutation in Melanoma. J. Transl. Med. 2012, 10, 85. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Maurer, G.; Tarkowski, B.; Baccarini, M. Raf Kinases in Cancer–Roles and Therapeutic Opportunities. Oncogene 2011, 30, 3477–3488. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zocco, D.; Bernardi, S.; Novelli, M.; Astrua, C.; Fava, P.; Zarovni, N.; Carpi, F.M.; Bianciardi, L.; Malavenda, O.; Quaglino, P.; et al. Isolation of Extracellular Vesicles Improves the Detection of Mutant DNA from Plasma of Metastatic Melanoma Patients. Sci. Rep. 2020, 10, 15745. [Google Scholar] [CrossRef]
- García-Silva, S.; Benito-Martín, A.; Sánchez-Redondo, S.; Hernández-Barranco, A.; Ximénez-Embún, P.; Nogués, L.; Mazariegos, M.S.; Brinkmann, K.; Amor López, A.; Meyer, L.; et al. Use of Extracellular Vesicles from Lymphatic Drainage as Surrogate Markers of Melanoma Progression and BRAFV600E Mutation. J. Exp. Med. 2019, 216, 1061–1070. [Google Scholar] [CrossRef] [Green Version]
- Kleffel, S.; Posch, C.; Barthel, S.R.; Mueller, H.; Schlapbach, C.; Guenova, E.; Elco, C.P.; Lee, N.; Juneja, V.R.; Zhan, Q.; et al. Melanoma Cell-Intrinsic PD-1 Receptor Functions Promote Tumor Growth. Cell 2015, 162, 1242–1256. [Google Scholar] [CrossRef] [Green Version]
- Gambichler, T.; Schröter, U.; Höxtermann, S.; Susok, L.; Stockfleth, E.; Becker, J.C. A Brief Communication on Circulating PD-1-Positive T-Regulatory Lymphocytes in Melanoma Patients Undergoing Adjuvant Immunotherapy with Nivolumab. J. Immunother. 2019, 42, 265–268. [Google Scholar] [CrossRef]
- Pantel, K.; Alix-Panabières, C. Liquid Biopsy: Potential and Challenges. Mol. Oncol. 2016, 10, 371–373. [Google Scholar] [CrossRef] [Green Version]
- Yancovitz, M.; Litterman, A.; Yoon, J.; Ng, E.; Shapiro, R.L.; Berman, R.S.; Pavlick, A.C.; Darvishian, F.; Christos, P.; Mazumdar, M.; et al. Intra- and Inter-Tumor Heterogeneity of BRAFV600EMutations in Primary and Metastatic Melanoma. PLoS ONE 2012, 7, e29336. [Google Scholar] [CrossRef]
- Diaz, L.A.; Bardelli, A. Liquid Biopsies: Genotyping Circulating Tumor DNA. J. Clin. Oncol. 2014, 32, 579–586. [Google Scholar] [CrossRef]
- Postel, M.; Roosen, A.; Laurent-Puig, P.; Taly, V.; Wang-Renault, S.-F. Droplet-Based Digital PCR and next Generation Sequencing for Monitoring Circulating Tumor DNA: A Cancer Diagnostic Perspective. Expert Rev. Mol. Diagn. 2018, 18, 7–17. [Google Scholar] [CrossRef]
- Valenti, F.; Falcone, I.; Ungania, S.; Desiderio, F.; Giacomini, P.; Bazzichetto, C.; Conciatori, F.; Gallo, E.; Cognetti, F.; Ciliberto, G.; et al. Precision Medicine and Melanoma: Multi-Omics Approaches to Monitoring the Immunotherapy Response. Int. J. Mol. Sci. 2021, 22, 3837. [Google Scholar] [CrossRef]
- Basler, L.; Gabryś, H.S.; Hogan, S.A.; Pavic, M.; Bogowicz, M.; Vuong, D.; Tanadini-Lang, S.; Förster, R.; Kudura, K.; Huellner, M.W.; et al. Radiomics, Tumor Volume, and Blood Biomarkers for Early Prediction of Pseudoprogression in Patients with Metastatic Melanoma Treated with Immune Checkpoint Inhibition. Clin. Cancer Res. 2020, 26, 4414–4425. [Google Scholar] [CrossRef] [Green Version]
- Shofty, B.; Artzi, M.; Shtrozberg, S.; Fanizzi, C.; DiMeco, F.; Haim, O.; Peleg Hason, S.; Ram, Z.; Bashat, D.B.; Grossman, R. Virtual Biopsy Using MRI Radiomics for Prediction of BRAF Status in Melanoma Brain Metastasis. Sci. Rep. 2020, 10, 6623. [Google Scholar] [CrossRef] [Green Version]
- Gill, A.B.; Rundo, L.; Wan, J.C.M.; Lau, D.; Zawaideh, J.P.; Woitek, R.; Zaccagna, F.; Beer, L.; Gale, D.; Sala, E.; et al. Correlating Radiomic Features of Heterogeneity on CT with Circulating Tumor DNA in Metastatic Melanoma. Cancers 2020, 12, 3493. [Google Scholar] [CrossRef]
- Sun, Y.; Guo, J. Pilot Study of CT-Based Radiomics Model for Early Evaluation of Response to Immunotherapy in Patients with Metastatic Melanoma. Front. Oncol. 2020, 10, 8. [Google Scholar]

| Type of BM | Author | Findings/Study | Utility OF BMs | Techniques | No. of Patients | Samples |
|---|---|---|---|---|---|---|
| Gene expression | Mann et al. [23] | 46 gene expression signature | Prognostic | GEP | 79 | T + LN |
| John et al. [24] | 21 gene expression signature | Prognostic | GEP | 29 | LN | |
| Bogunovic et al. [25] | 266 gene expression signature | Prognostic | Microarray | 38 | MTS | |
| Zager et al. [26] | 31 gene expression signature | Predictive of metastatic risk | GEP | 523 | T | |
| Journe et al. [27] | Expression of TYRP1 | Prognostic | Microarray + qPCR | 111 | T + LN | |
| El Hajj et al. [28] | Expression of TYRP1 | Prognostic | RT-qPCR | 104 | LN | |
| Dummer et al. [13] | Expression of IFNG, CXCL9, CXCL10, CXCL11, GBP1 | Prognostic and predictive | Nanostring + NGS | 875 | - | |
| miRNAs | Segura et al. [29] | 6 miRNA signature | Prognostic | Microarray | 59 | LB |
| Sanchez-Sendra et al. [30] | 5 miRNA signature | Prognostic | RT-qPCR | 132 | T + LN + MTS | |
| Huber et al. [31] | MiRNA signature | Predictive of immunotherapy resistance | RT-qPCR | 87 | LB + T | |
| Fattore et al. [32] | Expression of miR-579-3p | Predictive of MAPKi resistance | RT-qPCR | 23 | T | |
| ctDNA | Marczynski et al. [33] | ctDNA (BRAF, NRAS, TERT) | Prognostic | ddPCR | 19 | LB |
| Lee et al. [34] | ctDNA pre-operative | Prognostic | ddPCR | 174 | LB | |
| Tan et al. [35] | ctDNA pre- and post-operative | Prognostic | ddPCR | 126 | LB | |
| Lee et al. [36] | ctDNA levels | Prognostic | ddPCR | 161 | LB | |
| Gandini et al. [37] | ctDNA levels | Prognostic | Meta-analysis | 2000 | MA | |
| CTCs | Koyanagi et al. [38] | MART-1, GalNAc-T, PAX-3, MAGE-A3 for CTCs detection | Prognostic | RT-qPCR | 92 | LB |
| Hoshimoto et al. [39] | MART1, MAGE-A3, GalNAc-T for CTCs detection | Prognostic | RT-qPCR | 320 | LB | |
| Lucci et al. [40] | Anti-CD146 for CTCs detection | Prognostic | 243 | LB | ||
| Lin et al. [41] | CTNNB1 | Predictive | Microfluidics | 22 | ||
| Methylation | Sigalotti et al. [42] | 17 gene methylation signature | Prognostic | Pyrosequencing | 42 | C |
| Sigalotti et al. [43] | LINE-1 methylation levels | Prognostic | BeadChip essay | 45 | C | |
| Hoshimoto et al. [44] | LINE-1 methylation levels | Prognostic | MALDI-TOF MS MSP | 203 | T + MTS + LN + LB | |
| Tanemura et al. [45] | MINT31 methylation levels | Prognostic | PCR | 107 | T + MTS | |
| Guadagni et al. [46] | MGMT promoter methylation levels | Prognostic | PCR | 27 | MTS | |
| BRAF | Mann et al. [23] | BRAF mutation | Prognostic | GEP | 79 | T + LN |
| Barbour et al. [47] | BRAF mutation | Prognostic | Sequenom MASSarray | 134 | LN | |
| Picard et al. [48] | BRAF mutation | Prognostic | PCR | 72 | T + LN | |
| Moreau et al. [49] | BRAF mutation | Prognostic | Pyrosequencing | 105 | T + LN | |
| Eggermont et al. [50] | BRAF mutation | Prognostic | - | 1019 | T | |
| Tas et al. [51] | BRAF mutation | Prognostic | RT-qPCR | 151 | T | |
| Heppt et al. [52] | BRAF mutation | Prognostic | Pyrosequencing + Sanger | 217 | T + LN + MTS | |
| Protein expression | Mactier et al. [53] | 21 proteins signature | Prognostic | Mass spectrometry | 33 | LN |
| Karonidis et al. [54] | S100B serum levels | Prognostic | Electroluminescence | 107 | LB | |
| Wagner et al. [55] | S100A8/A9 serum levels | Prognostic | ELISA | 354 | LB | |
| Madore et al. [56] | PD-L1 expression | Prognostic | IHC | 52 | LN | |
| Ekmekcioglu et al. [57] | CD74 expression | Prognostic | IHC | 158 | LN | |
| Ascierto et al. [58] | Immune infiltrate | Prognostic | IHC | 498 | T | |
| Lauwyck et al. [59] | C-Reactive protein | Predictive of irAEs | - | 72 | LB |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tonella, L.; Pala, V.; Ponti, R.; Rubatto, M.; Gallo, G.; Mastorino, L.; Avallone, G.; Merli, M.; Agostini, A.; Fava, P.; et al. Prognostic and Predictive Biomarkers in Stage III Melanoma: Current Insights and Clinical Implications. Int. J. Mol. Sci. 2021, 22, 4561. https://doi.org/10.3390/ijms22094561
Tonella L, Pala V, Ponti R, Rubatto M, Gallo G, Mastorino L, Avallone G, Merli M, Agostini A, Fava P, et al. Prognostic and Predictive Biomarkers in Stage III Melanoma: Current Insights and Clinical Implications. International Journal of Molecular Sciences. 2021; 22(9):4561. https://doi.org/10.3390/ijms22094561
Chicago/Turabian StyleTonella, Luca, Valentina Pala, Renata Ponti, Marco Rubatto, Giuseppe Gallo, Luca Mastorino, Gianluca Avallone, Martina Merli, Andrea Agostini, Paolo Fava, and et al. 2021. "Prognostic and Predictive Biomarkers in Stage III Melanoma: Current Insights and Clinical Implications" International Journal of Molecular Sciences 22, no. 9: 4561. https://doi.org/10.3390/ijms22094561
APA StyleTonella, L., Pala, V., Ponti, R., Rubatto, M., Gallo, G., Mastorino, L., Avallone, G., Merli, M., Agostini, A., Fava, P., Bertero, L., Senetta, R., Osella-Abate, S., Ribero, S., Fierro, M. T., & Quaglino, P. (2021). Prognostic and Predictive Biomarkers in Stage III Melanoma: Current Insights and Clinical Implications. International Journal of Molecular Sciences, 22(9), 4561. https://doi.org/10.3390/ijms22094561