Evaluation of New Antimicrobial Agents Based on tris(1H-Indol-3-yl)methylium Salts: Activity, Toxicity, Suppression of Experimental Sepsis in Mice
Abstract
:1. Introduction
2. Results
2.1. Chemistry
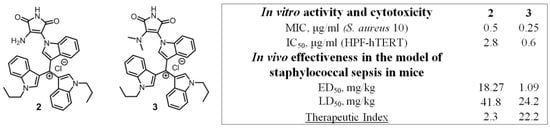
2.2. Biological Evaluation In Vitro: Detection of Antimicrobial Activity and Cytotoxicity
2.3. Biological Evaluation In Vivo
2.3.1. Toxicity Studies in Animals (Mice)
2.3.2. Efficiency in the Model of Staphylococcal Sepsis in Mice
3. Discussion
4. Materials and Methods
4.1. Preparation and Purification of New Compounds, Their Physical and Chemical Characteristics, Preparation of Solutions
4.2. Microbial Strains, Nutrient Media, Cultivation Conditions
4.3. Estimation of the Antibacterial and Antifungal Activities In Vitro
4.4. The Cytotoxic Activity
4.5. Determination of the Acute Toxicity and Antimicrobial Activity of the Tested Compounds In Vivo
4.6. Preparations for Intravenous Administration
4.7. Acute Toxicity Study
4.8. Study of the Drug Efficacy in the Treatment of Staphylococcal Sepsis in Mice
4.9. Experiment Protocol
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gillespie, D.E.; Brady, S.F.; Bettermann, A.D.; Cianciotto, N.P.; Liles, M.R.; Rondon, M.R.; Clardy, J.; Goodman, R.M.; Handelsman, J. Isolation of Antibiotics Turbomycin A and B from a Metagenomic Library of Soil Microbial DNA. Appl. Environ. Microbiol. 2002, 8, 4301–4306. [Google Scholar] [CrossRef] [Green Version]
- Dothager, R.S.; Putt, K.S.; Allen, B.J.; Leslie, B.J.; Nesterenko, V.; Hergenrother, P.J. Synthesis and Identification of Small Molecules that Potently Induce Apoptosis in Melanoma Cells through G1 Cell Cycle Arrest. J. Am. Chem. Soc. 2005, 127, 8686. [Google Scholar] [CrossRef] [PubMed]
- Palchaudhuri, R.; Nesterenko, V.; Hergenrother, P.J. The Complex Role of the Triphenylmethyl Motif in Anticancer Compounds. J. Am. Chem. Soc. 2008, 130, 10274. [Google Scholar] [CrossRef] [PubMed]
- Palchaudhuri, R.; Hergenrother, P.J. Triphenylmethylamides (TPMAs): Structure–activity relationship of compounds that induce apoptosis in melanoma cells. Bioorg. Med. Chem. Lett. 2008, 18, 5888. [Google Scholar] [CrossRef]
- Al-Qawasmeh, R.A.; Lee, Y.; Cao, M.-Y.; Gu, X.; Vassilakos, A.; Wright, J.A.; Young, A. Triaryl methane derivatives as antiproliferative agents. Bioorg. Med. Chem. Lett. 2004, 14, 347. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Guang, B.; Wang, L.; Li, B.; Zhang, G. Synthesis and cytotoxic activity of N-acetylated triindolylmethanes. Heterocycles 2003, 60, 1307–1315. [Google Scholar] [CrossRef]
- El Sayed, M.T.; Sabry, N.M.; Hamdy, N.A.; Voronkov, A.; Ogungbe, I.; Balakin, K.; Abdel-Aziz, M.S. Synthesis, Anti-Methicillin-resistant S. aureus (MRSA) Evaluation, Quantitative Structure-Activity Relationship and Molecular Modeling Studies of Some Novel Bis-indoles as Prospective MRSA Pyruvate Kinase Inhibitors. Lett. Drug. Des. Discov. 2018, 15, 336–346. [Google Scholar] [CrossRef]
- Tu, X.; Chen, X.; Zhang, D.; Guo, M.; Liang, J.; Bao, G.; Zhang, J.; Peng, S.; Zhang, X.; Zeng, Z.; et al. Optimization of novel oxidative DIMs as Nur77 modulators of the Nur77-Bcl-2 apoptotic pathway. Eur. J. Med. Chem. 2021, 211, 113020. [Google Scholar] [CrossRef]
- Ciulla, M.G.; Kumar, K. The natural and synthetic indole weaponry against bacteria. Tetrahedron Lett. 2018, 59, 3223–3233. [Google Scholar] [CrossRef]
- Penieres-Carrillo, J.-G.; Ríos-Guerra, H.; Solano-Becerra, J.-D.; Pérez-Flores, F.-J.; Barrera-Téllez, F.-J.; Luna-Mora, R.-A. Synthesis of turbomicin-based alkaloids through infrared light-induced multicomponent reactions and assessment of their cytotoxic and antifungal bioactivity. Mon. Chem. 2021, 152, 1337–1346. [Google Scholar] [CrossRef]
- Shallcross, L.J.; Davies, S.C. The World Health Assembly resolution on antimicrobial resistance. J. Antimicrob. Chemother. 2014, 69, 2883–2885. [Google Scholar] [CrossRef] [PubMed]
- Arias, C.A.; Murray, M.D. Antibiotic-resistant bugs in the 21st century—A clinical super-challenge. N. Engl. J. Med. 2009, 360, 439–443. [Google Scholar] [CrossRef] [Green Version]
- Tsakou, F.; Jersie-Christensen, R.; Jenssen, H.; Mojsoska, B. The Role of Proteomics in Bacterial Response to Antibiotics. Pharmaceuticals 2020, 13, 214. [Google Scholar] [CrossRef]
- MacKenzie, F.M.; Struelens, M.J.; Towner, K.J.; Gould, I.M. Report of the Consensus Conference on Antibiotic Resistance; Prevention and Control (ARPAC). Clin. Microbiol. Infect. 2005, 11, 938–954. [Google Scholar] [CrossRef]
- Stepanova, E.V.; Shtil’, A.A.; Lavrenov, S.N.; Bukhman, V.M.; Inshakov, A.N.; Mirchink, E.P.; Trenin, A.S.; Galatenko, O.A.; Isakova, E.B.; Glazunova, V.A.; et al. Tris(1-alkylindol-3-yl) methylium salts as a novel class of antitumor agents. Russ. Chem. Bull. Int. Ed. 2010, 59, 2259. [Google Scholar] [CrossRef]
- Durandin, N.A.; Tsvetkov, V.B.; Bykov, E.E.; Kaluzhny, D.N.; Lavrenov, S.N.; Tevyashova, A.N.; Preobrazhenskaya, M.N. Quantitative parameters of complexes of tris(1-alkylindol-3-yl)methylium salts with serum albumin: Relevance for the design of drug candidates. J. Photochem. Photobiol. B Biol. 2016, 162, 570–576. [Google Scholar] [CrossRef]
- Lavrenov, S.N.; Isakova, E.B.; Panov, A.A.; Simonov, A.Y.; Tatarsky, V.V.; Trenin, A.S. N-(Hydroxyalkyl) Derivatives of tris(1H-indol-3-yl) methylium salts as promising antibacterial agents: Synthesis and biological evaluation. Pharmaceuticals 2020, 13, 469. [Google Scholar] [CrossRef] [PubMed]
- van Eis, M.J.; Evenou, J.P.; Schuler, W.; Zenke, G.; Vangrevelinghe, E.; Wagner, J.; von Matt, P. Indolyl-naphthyl-maleimides as potent and selective inhibitors of protein kinase C-α/β. Bioorg. Med. Chem. Lett. 2017, 27, 781–786. [Google Scholar] [CrossRef]
- Cohen, P. Protein kinases—The major drug targets of the twenty-first century. Nat. Rev. Drug Discov. 2002, 1, 309–315. [Google Scholar] [CrossRef] [PubMed]
- Simonov, A.Y.; Panov, A.A.; Trenin, A.S.; Korolev, A.M.; Lavrenov, S.N. Optimization of the synthesis technique new antimicrobial substances derivatives of tris(1-alkylindol-3-yl) methilium. Pharm. Chem. J. 2021, 54, 1263–1268. [Google Scholar] [CrossRef]
- NCCLS Reference Method for Broth Dilution Antibacterial Susceptibility Testing; Clinical and Laboratory Standards Institute: Pittsburgh, PA, USA, 2000.
- CLSI M38-A2; Reference Method for Broth Dilution Antifungal Susceptibility Testing of Filamentous Fungi, 2nd ed.; Approved Standart. Clinical and Laboratory Standards Institute: Pittsburgh, PA, USA, 2008.
- CLSI M27-S3; Reference Method for Broth Dilution Antifungal Susceptibility Testing of Yeasts. Clinical and Laboratory Standards Institute: Pittsburgh, PA, USA, 2013.
- Muller, P.Y.; Milton, M.N. The determination and interpretation of the therapeutic index in drug development. Nat. Rev. Drug Discov. 2012, 11, 751–761. [Google Scholar] [CrossRef] [PubMed]
- Grant, S.K. Therapeutic protein kinase inhibitors. Cell. Mol. Life Sci. 2009, 66, 1163–1177. [Google Scholar] [CrossRef] [PubMed]
- Council of Europe. European Convention for the Protection of Vertebrate Animals Used for Experimental and Other Purposes; Accessed on 28 August 2018, 18.III.1986, ETS No. 123; Council of Europe: Strasbourg, France, 1986. [Google Scholar]
- The Russian Federation Standard. In National State Standard GOST P 53434-2009; The Principles of Good Laboratory Practice; (Approved and Put into Effect by the Order of the Federal Agency for Technical Regulation and Metrology of 2 December 2009), No 544; Standartinform: Moscow, Russia, 2010.

| Compounds | MIC, μg/mL | ||||
|---|---|---|---|---|---|
| Control | 1 | 2 | 3 | 4 | |
| Bacterial Strains | Gram-Positive Bacteria | ||||
| Staphylococcus aureus ATCC 25923 | 0.25 (Lf) | 2 | 0.5 | 0.13 | 0.25 |
| Staphylococcus aureus ATCC 3798 | 32 (Lf) | 2 | 0.25 | 0.13 | 0.25 |
| Staphylococcus aureus 100KC | 32 (Lf) | 2 | 0.5 | 0.13 | 0.5 |
| Staphylococcus aureus ATCC 700699 | 16 (Lf) | 2 | 0.5 | 0.13 | 0.25 |
| Staphylococcus aureus 10 | 0.13 (Lf) | 1 | 0.5 | 0.25 | 0.25 |
| Staphylococcus aureus 5 | 0.25 (Lf) | 4 | 0.25 | 0.5 | 0.5 |
| Staphylococcus epidermidis 533 | 0.5 (Lf) | 1 | 0.5 | 0.5 | 0.13 |
| Staphylococcus haemoliticus 585 | 0.5 (Lf) | 4 | 2 | >64 | 0.5 |
| Enterococcus faecium 569 | 1 (Lf) | 8 | 8 | >64 | 1 |
| Bacterial Strains | Gram-Negative Bacteria | ||||
| Escherichia coli ATCC 25922 | 0.06 (Lf) | 8 | >64 | 16 | 32 |
| Klebsiella pneumoniae ATCC 13883 | 0.25 (Lf) | 2 | >64 | >64 | >64 |
| Proteus vulgaris ATCC 13315 | 4 (Lf) | 64 | 16 | >64 | 1 |
| Salmonella cholerasuis ATCC 14028 | 0.13 (Lf) | >64 | >64 | >64 | 32 |
| Pseudomonas aeruginosa ATCC 27853 | 1 (Lf) | >64 | 32 | 16 | 64 |
| Fungi Strains | Fungi | ||||
| Candida albicans ATCC 14053 | 1 (Am B) | >64 | 12 | 2 | 1 |
| Aspergillus niger ATCC 16404 | 1 (Am B) | >64 | 8 | 2 | 2 |
| Test Cells | Cytotoxic Activity IC50, μg/mL | ||||
| HPF-hTERT | >50 (Lf); 0.7 (Am B) | 13 | 2.8 | 0.6 | 0.07 |
| Doses, mg/kg | |||
|---|---|---|---|
| Compounds | 1 | 2 | 3 |
| LD50 | 26.2 (24.3 ÷ 28.1) | 41.8 (37.6 ÷ 45.9) | 24.2 (20.2 ÷ 28.2) |
| MTD (LD10) | 22.6 (21.0 ÷ 24.2) | 34.1 (31.0 ÷ 35.8) | 16.9 (15.4 ÷ 17.6) |
| LD16 | 23.4 | 35.8 | 18.5 |
| LD84 | 28.9 | 47.7 | 29.8 |
| LD100 | 30.2 | 50.7 | 32.6 |
| Compound | Dose of the Drug, mg/kg | Death (%) | Survival Rate (%) |
|---|---|---|---|
| 1 | 3.0 | 87.5 | 12.5 |
| 5.0 | 75 | 25 | |
| 7.0 | 75 | 25 | |
| 9.0 | 62.5 | 37.5 | |
| 11.0 | 62.5 | 37.5 | |
| 13.0 | 75 | 25 | |
| 2 | 5.0 | 80 | 20 |
| 10.0 | 70 | 30 | |
| 15.0 | 60 | 40 | |
| 20.0 | 40 | 60 | |
| 25.0 | 40 | 60 | |
| 30.0 | 20 | 80 | |
| 35.0 | 30 | 70 | |
| 3 | 0.5 | 70 | 30 |
| 1.0 | 50 | 50 | |
| 1.5 | 40 | 60 | |
| 1.75 | 10 | 90 | |
| 2.0 | 0 | 100 | |
| Levofloxacin | 1.0 | 90 | 10 |
| 2.0 | 60 | 40 | |
| 4.0 | 40 | 60 | |
| 6.0 | 30 | 70 | |
| Control (infected mice without treatment). | - | 100 | 0 |
| Intact Animals | - | 0 | 100 |
| Group Number | Regimen of Drug Administration | Days of Experiment (Numerator—Dead Animals, Denominator—Survivors) | Death (%) | Survival Rate (%) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 0 | 3 | 4 | 6 | 7 | 8 | 9 | 10 | 12 | 14 | ||||
| 1 | One-time | 0/8 | 1/7 | 2/6 | 4/4 | 5/3 | 5/3 | 6/2 | 7/1 | 7/1 | 7/1 | 87.5 | 12.5 |
| 2 | Double | 0/8 | 0/8 | 1/7 | 3/5 | 4/4 | 4/4 | 5/3 | 6/2 | 6/2 | 6/2 | 75 | 25 |
| 3 | Three-fold | 0/8 | 0/8 | 1/7 | 2/6 | 3/5 | 3/5 | 4/4 | 5/3 | 5/3 | 5/3 | 62.5 | 37.5 |
| 4 | Control | 0/8 | 2/6 | 3/5 | 5/3 | 6/2 | 7/1 | 8/0 | 8/0 | 8/0 | 8/0 | 100 | 0 |
| Compound | |||
|---|---|---|---|
| 1 | 2 | 3 | |
| ED50, mg/kg | 7.6 (4.85 ÷ 11/45) | 18.27 (11.9 ÷ 24.95) | 1.09 (0.77 ÷ 1.42) |
| LD50, mg/kg | 26,2 (24.3 ÷ 28.1) | 41.8 (37.6 ÷ 45.9) | 24.2 (20.2 ÷ 28.2) |
| TI | 3.45 | 2.3 | 22.2 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Trenin, A.S.; Isakova, E.B.; Treshchalin, M.I.; Polozkova, V.A.; Mirchink, E.P.; Panov, A.A.; Simonov, A.Y.; Bychkova, O.P.; Tatarskiy, V.V.; Lavrenov, S.N. Evaluation of New Antimicrobial Agents Based on tris(1H-Indol-3-yl)methylium Salts: Activity, Toxicity, Suppression of Experimental Sepsis in Mice. Pharmaceuticals 2022, 15, 118. https://doi.org/10.3390/ph15020118
Trenin AS, Isakova EB, Treshchalin MI, Polozkova VA, Mirchink EP, Panov AA, Simonov AY, Bychkova OP, Tatarskiy VV, Lavrenov SN. Evaluation of New Antimicrobial Agents Based on tris(1H-Indol-3-yl)methylium Salts: Activity, Toxicity, Suppression of Experimental Sepsis in Mice. Pharmaceuticals. 2022; 15(2):118. https://doi.org/10.3390/ph15020118
Chicago/Turabian StyleTrenin, Alexey S., Elena B. Isakova, Michael I. Treshchalin, Vasilisa A. Polozkova, Elena P. Mirchink, Alexey A. Panov, Alexander Y. Simonov, Olga P. Bychkova, Victor V. Tatarskiy, and Sergey N. Lavrenov. 2022. "Evaluation of New Antimicrobial Agents Based on tris(1H-Indol-3-yl)methylium Salts: Activity, Toxicity, Suppression of Experimental Sepsis in Mice" Pharmaceuticals 15, no. 2: 118. https://doi.org/10.3390/ph15020118
APA StyleTrenin, A. S., Isakova, E. B., Treshchalin, M. I., Polozkova, V. A., Mirchink, E. P., Panov, A. A., Simonov, A. Y., Bychkova, O. P., Tatarskiy, V. V., & Lavrenov, S. N. (2022). Evaluation of New Antimicrobial Agents Based on tris(1H-Indol-3-yl)methylium Salts: Activity, Toxicity, Suppression of Experimental Sepsis in Mice. Pharmaceuticals, 15(2), 118. https://doi.org/10.3390/ph15020118