Single and Multitarget Systems for Drug Delivery and Detection: Up-to-Date Strategies for Brain Disorders
Abstract
:1. Introduction
2. Materials and Methods
3. Blood–Brain Barrier and Delivery Routes
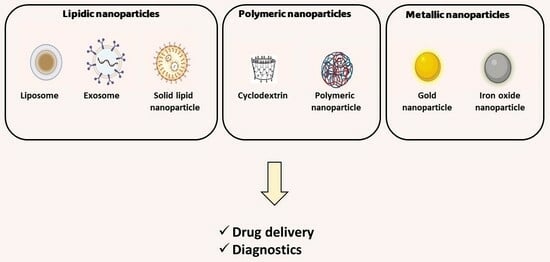
4. Types of Nanoparticles
4.1. Lipid-Based Nanoparticles
| Target/Disease | Drug(s) | Nanoparticle Type | Composition | Functionalization | Diameter of the Optimized Formulation(s) (nm) | Observations | Ref. |
|---|---|---|---|---|---|---|---|
| AD | Anti-amyloid single-domain antibody fragment (VHH-pa2H) | Liposome | 1,2-dimyristoyl-sn-glycero-3-phosphocholine or egg-yolk phosphatidylcholine | Glutathione-DSPE-PEG2000 (PEG) | 108, 110 | Liposomes were injected into APPswe/PS1dE9 double transgenic mice, a mouse model of AD. GSH-PEG liposomes increased VHH-pa2H uptake in the brain. | [53] |
| AD | ApoE2-encoding plasmid DNA/chitosan | Liposome | Dioleoyl-3-trimethylammonium-propane chloride (DOTAP), dioleoyl-sn-glycero-3phosphoethanolamine (DOPE) | DSPE-PEG2000, Glucose transporter-1 (Glut-1) targeting ligand mannose (MAN)+ cell penetrating peptides (CPP) (rabies virus glycoprotein peptide (RVG) or penetratin (Pen)) | 168, 172 | Significantly higher expression of ApoE2 in bEnd.3 cells, primary neurons, and astrocytes compared to monofunctionalized and unmodified liposomes. Dual-modified liposomes (RVG-MAN and Pen-MAN) also showed ∼2 times higher protein expression than single-targeted formulation (MAN or Pen) in neurons cultured below an in vitro BBB model. | [42] |
| AD | Rivastigmine | Liposome | Cholesterol and dipalmitoylphosphatidyl choline (DPPC) methylcellulose dimethyl-β-cyclodextrin or sodium taurocholate | Absorption enhancers (dimethyl-β-cyclodextrin or sodium taurocholate) | 3.4 *, 4.8 * | Rivastigmine liposomes and solutions were also administered to mice orally and intraperitoneally. The highest AChE inhibition was observed for rivastigmine-sodium-taurocholate liposomes. | [54] |
| AD | Rivastigmine | Liposome | Egg phosphatidylcholine, cholesterol | DSPE-PEG2000-CPP | 179 | Intranasal administration of rivastigmine liposomes to rats demonstrated the capacity to improve rivastigmine distribution and adequate retention in CNS regions (hippocampus and cortex) and affected acetylcholinesterase (AChE) and butyrylcholinesterase (BuChE) activities. The effects were more pronounced that those induced by free rivastigmine and uncoated liposomes. | [55] |
| AD | Rivastigmine | Liposome | 1,2-diacyl-sn-glycero-3-phosphocholine, dihexadecyl phosphate, cholesterol | - | 68, 529 | Liposomes resulted in faster memory regain and the amelioration of metabolic disturbances in AlCl3-treated rats than free rivastigmine solution. | [56] |
| AD | α-tocopherol + donepezil hydrochloride | Liposome | L-α-phosphatidylcholine and cholesterol | Tetradecyltriphenylphosphonium bromide | 105–115 | Intranasal administration to APP/PS1 mice resulted in enhanced learning abilities and a reduction in the formation rate of amyloid beta (Aβ) plaques in the entorhinal cortex and hippocampus of the brain. | [6] |
| AD | Galantamine hydrobromide | Liposome | Soya phosphatidylcholine and cholesterol | - | 112 | Intranasal administration of the liposomes could readily transport galantamine into rat brain tissues where it could inhibit cholinesterase. | [57] |
| AD | Quercetin | Liposome | Egg L-α-phosphatidylcholine, cholesterol | - | - | Effect of nasal administration of quercetin liposomes on neurodegeneration in an animal model of AD. Quercetin liposomes attenuated the degeneration of neurons and cholinergic neurons in the hippocampus, promoted the elevation of superoxide dismutase, catalase, and glutathione peroxidase activities and induced the reduction in malondialdehyde in the hippocampus. | [58] |
| PD | Levodopa | Liposome | Hydrogenated soybean phosphatidylcholine, cholesterol | DSPE-PEG2000-Chlorotoxin | 107 | After intraperitoneal injection to mice, liposomes loaded with levodopa significantly increased the distribution of dopamine (DA) and dihydroxyphenyl acetic acid in the substantia nigra and striata. In a 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP)-induced PD mice model, levodopa-loaded chlorotoxin liposomes significantly attenuated the serious behavioral disorders and diminished the MPTP-induced loss of tyrosine hydroxylase-positive dopaminergic neurons. | [59] |
| PD | Glial-cell-derived neurotrophic factor (GDNF) | Liposome | Dioleoylphosphatidylcholine (DOPC), cholesterol, and stearylamine | - | 149 | Rats were nasally administered with GDNF solution or with cationic liposomes containing GDNF before the injection of 6-hydroxydopamine (6-OHDA). Both intranasal GDNF treatments induced a neurotrophic effect in the substantia nigra since the number of tyrosine hydroxylase (TH)-positive neurons was significantly higher than in controls given intranasal PBS liposomes. | [60] |
| PD | Dopamine | Liposome | Cholesterol, 1,2-dioleyl-sn-glycero-3-phosphocholine (DOPC), L-α-phosphatidic acid | APP-derived peptide | 100 | Intraperitoneal injection of the APP-targeted liposomes loaded with dopamine resulted in a significant increase in striatal DA in amphetamine-treated mice. | [61] |
| PD | Resveratrol | Liposome | Soybean lecithin and cholesterol | - | 146–585 | Resveratrol liposomes could significantly enhance the activity of mitochondrial electron transfer chain complex I in the substantia nigra cells of 6-hydroxydopamine-treated rats, promote the expression of complex I subcomponent MT-ND1-37kD, improve mitochondrial membrane potential, inhibit the release of mitochondrial cytochrome C and apoptotic inducible factor, enhance the expression of mitochondrial functional protein PINK1, increase the phosphorylated TRAP1 level, and elevate the phosphorylated TRAP1/TRAP1 levels. | [62] |
| PD | Polyphenol-rich grape pomace extracts | Liposome | Brain lipids, 1,2-distearoylsn-glycero-3-phosphoethanolamine-N-(PEG)5000 | anti-transferrin receptor antibody | 133 | The antioxidant nanoplatform was successfully tested in a rotenone-induced in vitro PD model, where it completely regulated the reactive oxygen species (ROS) levels, prevented the aggregation of α-synuclein fibrils, and restored cell viability. | [63] |
| Anxiety | Nimodipine | Liposome | Soybean phosphatidylcholine and cholesterol | - | 107 | The results suggest that the administration of nimodipine liposomes has no sedative or muscle relaxant effect in animals but displayed anxiolytic-like activity in bright-field test. The results obtained in the open arms test suggest that the new formulation acts on benzodiazepine receptors. | [64] |
| Anxiety | Eugenol | Liposome | Lecithin, cholesterol | - | 91 | The mRNA expression of glyoxylase-1 (GLO-1) and GLO-1 protein expression were measured in 42 BALB/c mice submitted to stress using a conventional restraint model. The mRNA and protein expressions were found to be increased in animals given anxiety as compared to the normal control. Eugenol and its liposome-based nanocarriers counteracted this behavior, with liposomal eugenol behaving better than the compound alone. | [65] |
| Anxiety | Eugenol | Liposome | Lecithin, cholesterol | - | 91 | Stress was induced in 42 BALB/c mice using a conventional restraint model. The mRNA expression of neurokinin 1 receptor (NK1R) and the NK1R protein expression were increased in animals given anxiety as compared to the normal control. Both parameters decreased in animals treated with eugenol and its liposome-based nanocarriers, the results being better for nanocarriers. | [66] |
| Anxiety/Depression | Quercetin | Liposome | Egg L-α phosphatidylcholine, cholesterol | - | - | Wistar rats were intranasally administered quercetin liposomes. These nanocarriers possessed anxiolytic and anti-depression like activity and a cognitive-enhancing effect, which were assessed using the elevated plus maze test, forced swimming test, and Morris water maze test | [67] |
| Depression | Plasmid-harboring brain-derived neurotrophic factor (BDNF) | Liposome | 1,2-Dioleoyl-sn-glycero-3-phosphoethanolamine (DOPE), and 1,2-dioleoyl-3-trimethylammonium-propane chloride (DOTAP), cholesterol | DSPE-PEG2000, transferrin, and arginine | 125 | Physicochemical characterization of the nanoparticles produced. | [68] |
| Depression | Nimodipine | Liposome | Soybean phosphatidylcholine and cholesterol | - | 107 | Tail suspension test, forced swimming test, and MAO-B activity assay suggested that nimodipine-liposomes displayed more antidepressant activity than imipramine and paroxetine but with a lower effect than that observed in the group receiving liposomes + reserpine. | [69] |
| Depression | Sertraline hydrochloride | Liposome | Hydrogenated soya phosphatidylcholine-L-α-phosphatidylcholine (HSPC), distearoyl phosphatidyl glycerol sodium (DSPG) and cholesterol | - | 152 | The use of liposomes increased drug transport to the brain compared with administration with free sertraline | [70] |
| Depression | Piperine | Liposome | Egg L-α-phosphatidylcholine, cholesterol | Polyethylene glycol 1000 | 100 | Piperine-encapsulated liposomes displayed antidepressant-like activity in Wistar rats submitted to forced swimming, Morris water maze, and spontaneous motor behavior tests. | [71] |
4.2. Polymeric Nanoparticles
4.3. Metallic Nanoparticles
5. Comparison between Different Types of Nanoparticles for Brain Delivery
6. Emerging Trends in Nanomedicine: Challenges and Future Directions
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- WHO Dementia—Key Facts. Available online: https://www.who.int/news-room/fact-sheets/detail/dementia (accessed on 15 October 2023).
- WHO Parkinson Disease—Key Facts. Available online: https://www.who.int/news-room/fact-sheets/detail/parkinson-disease (accessed on 15 October 2023).
- Bloomingdale, P.; Karelina, T.; Ramakrishnan, V.; Bakshi, S.; Véronneau-Veilleux, F.; Moye, M.; Sekiguchi, K.; Meno-Tetang, G.; Mohan, A.; Maithreye, R.; et al. Hallmarks of neurodegenerative disease: A systems pharmacology perspective. CPT Pharmacomet. Syst. Pharmacol. 2022, 11, 1399–1429. [Google Scholar] [CrossRef] [PubMed]
- Mizuno, Y. Definition and Classification of Parkinsonian Drugs. In NeuroPsychopharmacotherapy; Springer International Publishing: Cham, Switzerland, 2022; pp. 2823–2852. [Google Scholar]
- Cheong, S.L.; Tiew, J.K.; Fong, Y.H.; Leong, H.W.; Chan, Y.M.; Chan, Z.L.; Kong, E.W.J. Current Pharmacotherapy and Multi-Target Approaches for Alzheimer’s Disease. Pharmaceuticals 2022, 15, 1560. [Google Scholar] [CrossRef] [PubMed]
- Vasileva, L.; Gaynanova, G.; Valeeva, F.; Belyaev, G.; Zueva, I.; Bushmeleva, K.; Sibgatullina, G.; Samigullin, D.; Vyshtakalyuk, A.; Petrov, K.; et al. Mitochondria-Targeted Delivery Strategy of Dual-Loaded Liposomes for Alzheimer’s Disease Therapy. Int. J. Mol. Sci. 2023, 24, 10494. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; An, S.; Li, J.; Kuang, Y.; He, X.; Guo, Y.; Ma, H.; Zhang, Y.; Ji, B.; Jiang, C. Brain-targeted co-delivery of therapeutic gene and peptide by multifunctional nanoparticles in Alzheimer’s disease mice. Biomaterials 2016, 80, 33–45. [Google Scholar] [CrossRef]
- Guerzoni, L.P.B.; Nicolas, V.; Angelova, A. In Vitro Modulation of TrkB Receptor Signaling upon Sequential Delivery of Curcumin-DHA Loaded Carriers towards Promoting Neuronal Survival. Pharm. Res. 2017, 34, 492–505. [Google Scholar] [CrossRef]
- Glinz, D.; Gloy, V.L.; Monsch, A.U.; Kressig, R.W.; Patel, C.; McCord, K.A.; Ademi, Z.; Tomonaga, Y.; Schwenkglenks, M.; Bucher, H.C.; et al. Acetylcholinesterase inhibitors combined with memantine for moderate to severe Alzheimer’s disease: A meta-analysis. Swiss Med. Wkly. 2019, 149, w20093. [Google Scholar] [CrossRef]
- Kabir, M.T.; Uddin, M.S.; Mamun, A.A.; Jeandet, P.; Aleya, L.; Mansouri, R.A.; Ashraf, G.M.; Mathew, B.; Bin-Jumah, M.N.; Abdel-Daim, M.M. Combination Drug Therapy for the Management of Alzheimer’s Disease. Int. J. Mol. Sci. 2020, 21, 3272. [Google Scholar] [CrossRef]
- Mateev, E.; Kondeva-Burdina, M.; Georgieva, M.; Zlatkov, A. Repurposing of FDA-approved drugs as dual-acting MAO-B and AChE inhibitors against Alzheimer’s disease: An in silico and in vitro study. J. Mol. Graph. Model. 2023, 122, 108471. [Google Scholar] [CrossRef]
- Chaib, S.; Vidal, B.; Bouillot, C.; Depoortere, R.; Newman-Tancredi, A.; Zimmer, L.; Levigoureux, E. Multimodal imaging study of the 5-HT1A receptor biased agonist, NLX-112, in a model of L-DOPA-induced dyskinesia. NeuroImage Clin. 2023, 39, 103497. [Google Scholar] [CrossRef]
- WHO Depressive Disorder (Depression)—Key Facts. Available online: https://www.who.int/news-room/fact-sheets/detail/depression (accessed on 10 October 2023).
- WHO Mental Disorders—Key Facts. Available online: https://www.who.int/news-room/fact-sheets/detail/mental-disorders (accessed on 10 October 2023).
- Paul, S.M.; Potter, W.Z. Finding new and better treatments for psychiatric disorders. Neuropsychopharmacology 2023, 49, 3–9. [Google Scholar] [CrossRef]
- Li, Z.; Ruan, M.; Chen, J.; Fang, Y. Major Depressive Disorder: Advances in Neuroscience Research and Translational Applications. Neurosci. Bull. 2021, 37, 863–880. [Google Scholar] [CrossRef] [PubMed]
- Nikayin, S.; Murphy, E.; Krystal, J.H.; Wilkinson, S.T. Long-term safety of ketamine and esketamine in treatment of depression. Expert Opin. Drug Saf. 2022, 21, 777–787. [Google Scholar] [CrossRef] [PubMed]
- Johnston, J.N.; Henter, I.D.; Zarate, C.A. The antidepressant actions of ketamine and its enantiomers. Pharmacol. Ther. 2023, 246, 108431. [Google Scholar] [CrossRef] [PubMed]
- Henssler, J.; Alexander, D.; Schwarzer, G.; Bschor, T.; Baethge, C. Combining Antidepressants vs Antidepressant Monotherapy for Treatment of Patients with Acute Depression—A Systematic Review and Meta-Analysis. JAMA Psychiatry 2022, 79, 300–312. [Google Scholar] [CrossRef] [PubMed]
- Garakani, A.; Murrough, J.W.; Freire, R.C.; Thom, R.P.; Larkin, K.; Buono, F.D.; Iosifescu, D.V. Pharmacotherapy of Anxiety Disorders: Current and Emerging Treatment Options. Front. Psychiatry 2020, 11, 1412. [Google Scholar] [CrossRef]
- Gupta, P.R.; Prabhavalkar, K. Combination therapy with neuropeptides for the treatment of anxiety disorder. Neuropeptides 2021, 86, 102127. [Google Scholar] [CrossRef]
- Jagaran, K.; Singh, M. Lipid Nanoparticles: Promising Treatment Approach for Parkinson’s Disease. Int. J. Mol. Sci. 2022, 23, 9361. [Google Scholar] [CrossRef]
- Pulgar, V.M. Transcytosis to Cross the Blood Brain Barrier, New Advancements and Challenges. Front. Neurosci. 2019, 12, 1019. [Google Scholar] [CrossRef]
- Puris, E.; Fricker, G.; Gynther, M. Targeting Transporters for Drug Delivery to the Brain: Can We Do Better? Pharm. Res. 2022, 39, 1415–1455. [Google Scholar] [CrossRef]
- Zhang, W.; Liu, Q.Y.; Haqqani, A.S.; Leclerc, S.; Liu, Z.; Fauteux, F.; Baumann, E.; Delaney, C.E.; Ly, D.; Star, A.T.; et al. Differential expression of receptors mediating receptor-mediated transcytosis (RMT) in brain microvessels, brain parenchyma and peripheral tissues of the mouse and the human. Fluids Barriers CNS 2020, 17, 47. [Google Scholar] [CrossRef]
- Wong, A.D.; Ye, M.; Levy, A.F.; Rothstein, J.D.; Bergles, D.E.; Searson, P.C. The blood-brain barrier: An engineering perspective. Front. Neuroeng. 2013, 6, 7. [Google Scholar] [CrossRef]
- Lombardo, S.M.; Schneider, M.; Türeli, A.E.; Günday Türeli, N. Key for crossing the BBB with nanoparticles: The rational design. Beilstein J. Nanotechnol. 2020, 11, 866–883. [Google Scholar] [CrossRef] [PubMed]
- Sanità, G.; Carrese, B.; Lamberti, A. Nanoparticle Surface Functionalization: How to Improve Biocompatibility and Cellular Internalization. Front. Mol. Biosci. 2020, 7, 587012. [Google Scholar] [CrossRef] [PubMed]
- Thambiliyagodage, C. Ligand exchange reactions and PEG stabilization of gold nanoparticles. Curr. Res. Green Sustain. Chem. 2022, 5, 100245. [Google Scholar] [CrossRef]
- Smolensky, E.D.; Park, H.E.; Berquó, T.S.; Pierre, V.C. Surface functionalization of magnetic iron oxide nanoparticles for MRI applications—Effect of anchoring group and ligand exchange protocol. Contrast Media Mol. Imaging 2011, 6, 189–199. [Google Scholar] [CrossRef] [PubMed]
- Dinkel, R.; Braunschweig, B.; Peukert, W. Fast and Slow Ligand Exchange at the Surface of Colloidal Gold Nanoparticles. J. Phys. Chem. C 2016, 120, 1673–1682. [Google Scholar] [CrossRef]
- Wagner, S.; Zensi, A.; Wien, S.L.; Tschickardt, S.E.; Maier, W.; Vogel, T.; Worek, F.; Pietrzik, C.U.; Kreuter, J.; von Briesen, H. Uptake Mechanism of ApoE-Modified Nanoparticles on Brain Capillary Endothelial Cells as a Blood-Brain Barrier Model. PLoS ONE 2012, 7, e32568. [Google Scholar] [CrossRef]
- Rajora, M.A.; Ding, L.; Valic, M.; Jiang, W.; Overchuk, M.; Chen, J.; Zheng, G. Tailored theranostic apolipoprotein E3 porphyrin-lipid nanoparticles target glioblastoma. Chem. Sci. 2017, 8, 5371–5384. [Google Scholar] [CrossRef]
- Nicolle, L.; Journot, C.M.A.; Gerber-Lemaire, S. Chitosan Functionalization: Covalent and Non-Covalent Interactions and Their Characterization. Polymers 2021, 13, 4118. [Google Scholar] [CrossRef]
- Mahajan, G.; Kaur, M.; Gupta, R. Green functionalized nanomaterials: Fundamentals and future opportunities. In Green Functionalized Nanomaterials for Environmental Applications; Elsevier: Amsterdam, The Netherlands, 2022; pp. 21–41. [Google Scholar]
- Ye, Z.; Gastfriend, B.D.; Umlauf, B.J.; Lynn, D.M.; Shusta, E.V. Antibody-Targeted Liposomes for Enhanced Targeting of the Blood-Brain Barrier. Pharm. Res. 2022, 39, 1523–1534. [Google Scholar] [CrossRef]
- Schnyder, A.; Huwyler, J. Drug transport to brain with targeted liposomes. NeuroRX 2005, 2, 99–107. [Google Scholar] [CrossRef]
- Zhang, Y.; He, J.; Shen, L.; Wang, T.; Yang, J.; Li, Y.; Wang, Y.; Quan, D. Brain-targeted delivery of obidoxime, using aptamer-modified liposomes, for detoxification of organophosphorus compounds. J. Control. Release 2021, 329, 1117–1128. [Google Scholar] [CrossRef] [PubMed]
- Juhairiyah, F.; de Lange, E.C.M. Understanding Drug Delivery to the Brain Using Liposome-Based Strategies: Studies that Provide Mechanistic Insights Are Essential. AAPS J. 2021, 23, 114. [Google Scholar] [CrossRef] [PubMed]
- Suk, J.S.; Xu, Q.; Kim, N.; Hanes, J.; Ensign, L.M. PEGylation as a strategy for improving nanoparticle-based drug and gene delivery. Adv. Drug Deliv. Rev. 2016, 99, 28–51. [Google Scholar] [CrossRef]
- Luo, Y.; Yang, H.; Zhou, Y.-F.; Hu, B. Dual and multi-targeted nanoparticles for site-specific brain drug delivery. J. Control. Release 2020, 317, 195–215. [Google Scholar] [CrossRef] [PubMed]
- Arora, S.; Layek, B.; Singh, J. Design and Validation of Liposomal ApoE2 Gene Delivery System to Evade Blood–Brain Barrier for Effective Treatment of Alzheimer’s Disease. Mol. Pharm. 2021, 18, 714–725. [Google Scholar] [CrossRef]
- Stalmans, S.; Bracke, N.; Wynendaele, E.; Gevaert, B.; Peremans, K.; Burvenich, C.; Polis, I.; De Spiegeleer, B. Cell-Penetrating Peptides Selectively Cross the Blood-Brain Barrier In Vivo. PLoS ONE 2015, 10, e0139652. [Google Scholar] [CrossRef]
- Neves, A.R.; van der Putten, L.; Queiroz, J.F.; Pinheiro, M.; Reis, S. Transferrin-functionalized lipid nanoparticles for curcumin brain delivery. J. Biotechnol. 2021, 331, 108–117. [Google Scholar] [CrossRef]
- Neves, A.R.; Queiroz, J.F.; Reis, S. Brain-targeted delivery of resveratrol using solid lipid nanoparticles functionalized with apolipoprotein E. J. Nanobiotechnology 2016, 14, 27. [Google Scholar] [CrossRef]
- Neves, A.R.; Queiroz, J.F.; Lima, S.A.C.; Reis, S. Apo E-Functionalization of Solid Lipid Nanoparticles Enhances Brain Drug Delivery: Uptake Mechanism and Transport Pathways. Bioconjug. Chem. 2017, 28, 995–1004. [Google Scholar] [CrossRef]
- Monge, M.; Fornaguera, C.; Quero, C.; Dols-Perez, A.; Calderó, G.; Grijalvo, S.; García-Celma, M.J.; Rodríguez-Abreu, C.; Solans, C. Functionalized PLGA nanoparticles prepared by nano-emulsion templating interact selectively with proteins involved in the transport through the blood-brain barrier. Eur. J. Pharm. Biopharm. 2020, 156, 155–164. [Google Scholar] [CrossRef]
- Nsairat, H.; Khater, D.; Sayed, U.; Odeh, F.; Al Bawab, A.; Alshaer, W. Liposomes: Structure, composition, types, and clinical applications. Heliyon 2022, 8, e09394. [Google Scholar] [CrossRef] [PubMed]
- Spuch, C.; Navarro, C. Liposomes for Targeted Delivery of Active Agents against Neurodegenerative Diseases (Alzheimer’s Disease and Parkinson’s Disease). J. Drug Deliv. 2011, 2011, 469679. [Google Scholar] [CrossRef] [PubMed]
- Ross, C.; Taylor, M.; Fullwood, N.; Allsop, D. Liposome delivery systems for the treatment of Alzheimer’s disease. Int. J. Nanomed. 2018, 13, 8507–8522. [Google Scholar] [CrossRef]
- Salarpour, S.; Barani, M.; Pardakhty, A.; Khatami, M.; Pal Singh Chauhan, N. The application of exosomes and Exosome-nanoparticle in treating brain disorders. J. Mol. Liq. 2022, 350, 118549. [Google Scholar] [CrossRef]
- Li, X.-H.; Zhang, J.; Li, D.-F.; Wu, W.; Xie, Z.-W.; Liu, Q. Physiological and pathological insights into exosomes in the brain. Zool. Res. 2020, 41, 365–372. [Google Scholar] [CrossRef]
- Rotman, M.; Welling, M.M.; Bunschoten, A.; de Backer, M.E.; Rip, J.; Nabuurs, R.J.A.; Gaillard, P.J.; van Buchem, M.A.; van der Maarel, S.M.; van der Weerd, L. Enhanced glutathione PEGylated liposomal brain delivery of an anti-amyloid single domain antibody fragment in a mouse model for Alzheimer’s disease. J. Control. Release 2015, 203, 40–50. [Google Scholar] [CrossRef] [PubMed]
- Mutlu, N.B.; Değim, Z.; Yılmaz, Ş.; Eşsiz, D.; Nacar, A. New perspective for the treatment of Alzheimer diseases: Liposomal rivastigmine formulations. Drug Dev. Ind. Pharm. 2011, 37, 775–789. [Google Scholar] [CrossRef]
- Yang, Z.-Z.; Zhang, Y.-Q.; Wang, Z.-Z.; Wu, K.; Lou, J.-N.; Qi, X.-R. Enhanced brain distribution and pharmacodynamics of rivastigmine by liposomes following intranasal administration. Int. J. Pharm. 2013, 452, 344–354. [Google Scholar] [CrossRef]
- Ismail, M.F.; ElMeshad, A.N.; Salem, N.A.H. Potential therapeutic effect of nanobased formulation of rivastigmine on rat model of Alzheimer’s disease. Int. J. Nanomed. 2013, 8, 393–406. [Google Scholar] [CrossRef]
- Li, W.; Zhou, Y.; Zhao, N.; Hao, B.; Wang, X.; Kong, P. Pharmacokinetic behavior and efficiency of acetylcholinesterase inhibition in rat brain after intranasal administration of galanthamine hydrobromide loaded flexible liposomes. Environ. Toxicol. Pharmacol. 2012, 34, 272–279. [Google Scholar] [CrossRef]
- Phachonpai, W.; Wattanathorn, J.; Muchimapura, S.; Tong-Un, T.; Preechagoon, D. Neuroprotective Effect of Quercetin Encapsulated Liposomes: A Novel Therapeutic Strategy against Alzheimer’s Disease. Am. J. Appl. Sci. 2010, 7, 480–485. [Google Scholar] [CrossRef]
- Xiang, Y.; Wu, Q.; Liang, L.; Wang, X.; Wang, J.; Zhang, X.; Pu, X.; Zhang, Q. Chlorotoxin-modified stealth liposomes encapsulating levodopa for the targeting delivery against the Parkinson’s disease in the MPTP-induced mice model. J. Drug Target. 2012, 20, 67–75. [Google Scholar] [CrossRef] [PubMed]
- Migliore, M.M.; Ortiz, R.; Dye, S.; Campbell, R.B.; Amiji, M.M.; Waszczak, B.L. Neurotrophic and neuroprotective efficacy of intranasal GDNF in a rat model of Parkinson’s disease. Neuroscience 2014, 274, 11–23. [Google Scholar] [CrossRef]
- Kahana, M.; Weizman, A.; Gabay, M.; Loboda, Y.; Segal-Gavish, H.; Gavish, A.; Barhum, Y.; Offen, D.; Finberg, J.; Allon, N.; et al. Liposome-based targeting of dopamine to the brain: A novel approach for the treatment of Parkinson’s disease. Mol. Psychiatry 2021, 26, 2626–2632. [Google Scholar] [CrossRef]
- Chen, J.; Liu, Q.; Wang, Y.; Guo, Y.; Xu, X.; Huang, P.; Lian, B.; Zhang, R.; Chen, Y.; Ha, Y. Protective effects of resveratrol liposomes on mitochondria in substantia nigra cells of parkinsonized rats. Ann. Palliat. Med. 2021, 10, 2458–2468. [Google Scholar] [CrossRef] [PubMed]
- Marino, A.; Battaglini, M.; Desii, A.; Lavarello, C.; Genchi, G.; Petretto, A.; Ciofani, G. Liposomes loaded with polyphenol-rich grape pomace extracts protect from neurodegeneration in a rotenone-based in vitro model of Parkinson’s disease. Biomater. Sci. 2021, 9, 8171–8188. [Google Scholar] [CrossRef] [PubMed]
- Moreno, L.C.; da Silva Oliveira, G.Z.; Cavalcanti, I.M.F.; Santos-Magalhães, N.S.; Rolim, H.M.L.; de Freitas, R.M. Development and evaluation of liposomal formulation containing nimodipine on anxiolytic activity in mice. Pharmacol. Biochem. Behav. 2014, 116, 64–68. [Google Scholar] [CrossRef] [PubMed]
- Siyal, F.J.; Siddiqui, R.A.; Memon, Z.; Aslam, Z.; Nisar, U.; Imad, R.; Shah, M.R. Eugenol and its liposome-based nano carrier reduce anxiety by inhibiting glyoxylase-1 expression in mice. Brazilian J. Biol. 2023, 83, e251219. [Google Scholar] [CrossRef] [PubMed]
- Siyal, F.J.; Memon, Z.; Siddiqui, R.A.; Aslam, Z.; Nisar, U.; Imad, R.; Shah, M.R. Eugenol and liposome-based nanocarriers loaded with eugenol protect against anxiolytic disorder via down regulation of neurokinin-1 receptors in mice. Pak. J. Pharm. Sci. 2020, 33, 2275–2284. [Google Scholar] [CrossRef]
- Tong-Un, T.; Wannanon, P.; Wattanatho, J.; Phachonpai, W. Quercetin Liposomes via Nasal Administration Reduce Anxiety and Depression-like Behaviors and Enhance Cognitive Performances in Rats. Am. J. Pharmacol. Toxicol. 2010, 5, 80–88. [Google Scholar] [CrossRef]
- Diniz, D.M.; Franze, S.; Homberg, J.R. Crossing the Blood-Brain-Barrier: A bifunctional liposome for BDNF gene delivery—A Pilot Study. bioRxiv 2020. [Google Scholar] [CrossRef]
- Moreno, L.C.; Rolim, H.M.L.; Freitas, R.M.; Santos-Magalhães, N.S. Antidepressant-like activity of liposomal formulation containing nimodipine treatment in the tail suspension test, forced swim test and MAOB activity in mice. Brain Res. 2016, 1646, 235–240. [Google Scholar] [CrossRef] [PubMed]
- Chauhan, T.; Rani, V.; Sahu, B.; Sharma, A.; Chand Kheruka, S.; Gambhir, S.; Dube, V.; Aggarwal, L.M.; Chawla, R. Negatively charged liposomes of sertraline hydrochloride: Formulation, characterization and pharmacokinetic studies. J. Drug Deliv. Sci. Technol. 2020, 58, 101780. [Google Scholar] [CrossRef]
- Priprem, A.; Chonpathompikunlert, P.; Sutthiparinyanont, S.; Wattanathorn, J. Antidepressant and cognitive activities of intranasal piperine-encapsulated liposomes. Adv. Biosci. Biotechnol. 2011, 02, 108–116. [Google Scholar] [CrossRef]
- Zhang, Y.; Liu, Y.; Liu, H.; Tang, W.H. Exosomes: Biogenesis, biologic function and clinical potential. Cell Biosci. 2019, 9, 19. [Google Scholar] [CrossRef] [PubMed]
- Saeedi, S.; Israel, S.; Nagy, C.; Turecki, G. The emerging role of exosomes in mental disorders. Transl. Psychiatry 2019, 9, 122. [Google Scholar] [CrossRef]
- Hornung, S.; Dutta, S.; Bitan, G. CNS-Derived Blood Exosomes as a Promising Source of Biomarkers: Opportunities and Challenges. Front. Mol. Neurosci. 2020, 13, 38. [Google Scholar] [CrossRef]
- Xia, X.; Wang, Y.; Huang, Y.; Zhang, H.; Lu, H.; Zheng, J.C. Exosomal miRNAs in central nervous system diseases: Biomarkers, pathological mediators, protective factors and therapeutic agents. Prog. Neurobiol. 2019, 183, 101694. [Google Scholar] [CrossRef]
- Satapathy, M.K.; Yen, T.-L.; Jan, J.-S.; Tang, R.-D.; Wang, J.-Y.; Taliyan, R.; Yang, C.-H. Solid Lipid Nanoparticles (SLNs): An Advanced Drug Delivery System Targeting Brain through BBB. Pharmaceutics 2021, 13, 1183. [Google Scholar] [CrossRef]
- Wang, H.; Sui, H.; Zheng, Y.; Jiang, Y.; Shi, Y.; Liang, J.; Zhao, L. Curcumin-primed exosomes potently ameliorate cognitive function in AD mice by inhibiting hyperphosphorylation of the Tau protein through the AKT/GSK-3β pathway. Nanoscale 2019, 11, 7481–7496. [Google Scholar] [CrossRef] [PubMed]
- Qi, Y.; Guo, L.; Jiang, Y.; Shi, Y.; Sui, H.; Zhao, L. Brain delivery of quercetin-loaded exosomes improved cognitive function in AD mice by inhibiting phosphorylated tau-mediated neurofibrillary tangles. Drug Deliv. 2020, 27, 745–755. [Google Scholar] [CrossRef] [PubMed]
- Alvarez-Erviti, L.; Seow, Y.; Yin, H.; Betts, C.; Lakhal, S.; Wood, M.J.A. Delivery of siRNA to the mouse brain by systemic injection of targeted exosomes. Nat. Biotechnol. 2011, 29, 341–345. [Google Scholar] [CrossRef]
- Qu, M.; Lin, Q.; Huang, L.; Fu, Y.; Wang, L.; He, S.; Fu, Y.; Yang, S.; Zhang, Z.; Zhang, L.; et al. Dopamine-loaded blood exosomes targeted to brain for better treatment of Parkinson’s disease. J. Control. Release 2018, 287, 156–166. [Google Scholar] [CrossRef] [PubMed]
- Haney, M.J.; Klyachko, N.L.; Zhao, Y.; Gupta, R.; Plotnikova, E.G.; He, Z.; Patel, T.; Piroyan, A.; Sokolsky, M.; Kabanov, A.V.; et al. Exosomes as drug delivery vehicles for Parkinson’s disease therapy. J. Control. Release 2015, 207, 18–30. [Google Scholar] [CrossRef]
- Cooper, J.M.; Wiklander, P.B.O.; Nordin, J.Z.; Al-Shawi, R.; Wood, M.J.; Vithlani, M.; Schapira, A.H.V.; Simons, J.P.; El-Andaloussi, S.; Alvarez-Erviti, L. Systemic exosomal siRNA delivery reduced alpha-synuclein aggregates in brains of transgenic mice. Mov. Disord. 2014, 29, 1476–1485. [Google Scholar] [CrossRef] [PubMed]
- Ren, X.; Zhao, Y.; Xue, F.; Zheng, Y.; Huang, H.; Wang, W.; Chang, Y.; Yang, H.; Zhang, J. Exosomal DNA Aptamer Targeting α-Synuclein Aggregates Reduced Neuropathological Deficits in a Mouse Parkinson’s Disease Model. Mol. Ther. Nucleic Acids 2019, 17, 726–740. [Google Scholar] [CrossRef]
- Vakilinezhad, M.A.; Amini, A.; Akbari Javar, H.; Baha’addini Beigi Zarandi, B.F.; Montaseri, H.; Dinarvand, R. Nicotinamide loaded functionalized solid lipid nanoparticles improves cognition in Alzheimer’s disease animal model by reducing Tau hyperphosphorylation. DARU J. Pharm. Sci. 2018, 26, 165–177. [Google Scholar] [CrossRef]
- Misra, S.; Chopra, K.; Sinha, V.R.; Medhi, B. Galantamine-loaded solid–lipid nanoparticles for enhanced brain delivery: Preparation, characterization, in vitro and in vivo evaluations. Drug Deliv. 2016, 23, 1434–1443. [Google Scholar] [CrossRef]
- Dhawan, S.; Kapil, R.; Singh, B. Formulation development and systematic optimization of solid lipid nanoparticles of quercetin for improved brain delivery. J. Pharm. Pharmacol. 2011, 63, 342–351. [Google Scholar] [CrossRef]
- Yusuf, M.; Khan, M.; Khan, R.A.; Ahmed, B. Preparation, characterization, in vivo and biochemical evaluation of brain targeted Piperine solid lipid nanoparticles in an experimentally induced Alzheimer’s disease model. J. Drug Target. 2013, 21, 300–311. [Google Scholar] [CrossRef] [PubMed]
- Smith, A.; Giunta, B.; Bickford, P.C.; Fountain, M.; Tan, J.; Shytle, R.D. Nanolipidic particles improve the bioavailability and α-secretase inducing ability of epigallocatechin-3-gallate (EGCG) for the treatment of Alzheimer’s disease. Int. J. Pharm. 2010, 389, 207–212. [Google Scholar] [CrossRef]
- Kakkar, V.; Kaur, I.P. Evaluating potential of curcumin loaded solid lipid nanoparticles in aluminium induced behavioural, biochemical and histopathological alterations in mice brain. Food Chem. Toxicol. 2011, 49, 2906–2913. [Google Scholar] [CrossRef] [PubMed]
- Tsai, M.-J.; Huang, Y.-B.; Wu, P.-C.; Fu, Y.-S.; Kao, Y.-R.; Fang, J.-Y.; Tsai, Y.-H. Oral Apomorphine Delivery from Solid Lipid Nanoparticles with Different Monostearate Emulsifiers: Pharmacokinetic and Behavioral Evaluations. J. Pharm. Sci. 2011, 100, 547–557. [Google Scholar] [CrossRef] [PubMed]
- Pardeshi, C.V.; Rajput, P.V.; Belgamwar, V.S.; Tekade, A.R.; Surana, S.J. Novel surface modified solid lipid nanoparticles as intranasal carriers for ropinirole hydrochloride: Application of factorial design approach. Drug Deliv. 2013, 20, 47–56. [Google Scholar] [CrossRef] [PubMed]
- Megala, M.; Shivaramakrishnan, B.; Kishore, R.M.; Balashanmugam, K. Neuroprotective potential of Naringenin-loaded solid-lipid nanoparticles against rotenone-induced Parkinson’s disease model. J. Appl. Pharm. Sci. 2020, 11, 19–28. [Google Scholar] [CrossRef]
- Vitorino, C.; Silva, S.; Gouveia, F.; Bicker, J.; Falcão, A.; Fortuna, A. QbD-driven development of intranasal lipid nanoparticles for depression treatment. Eur. J. Pharm. Biopharm. 2020, 153, 106–120. [Google Scholar] [CrossRef]
- Nirale, P.; Paul, A.; Yadav, K.S. Nanoemulsions for targeting the neurodegenerative diseases: Alzheimer’s, Parkinson’s and Prion’s. Life Sci. 2020, 245, 117394. [Google Scholar] [CrossRef]
- Misra, S.K.; Pathak, K. Nose-to-Brain Targeting via Nanoemulsion: Significance and Evidence. Colloids Interfaces 2023, 7, 23. [Google Scholar] [CrossRef]
- Singh, Y.; Meher, J.G.; Raval, K.; Khan, F.A.; Chaurasia, M.; Jain, N.K.; Chourasia, M.K. Nanoemulsion: Concepts, development and applications in drug delivery. J. Control. Release 2017, 252, 28–49. [Google Scholar] [CrossRef]
- Kaur, A.; Nigam, K.; Srivastava, S.; Tyagi, A.; Dang, S. Memantine nanoemulsion: A new approach to treat Alzheimer’s disease. J. Microencapsul. 2020, 37, 355–365. [Google Scholar] [CrossRef] [PubMed]
- Kaur, A.; Nigam, K.; Bhatnagar, I.; Sukhpal, H.; Awasthy, S.; Shankar, S.; Tyagi, A.; Dang, S. Treatment of Alzheimer’s diseases using donepezil nanoemulsion: An intranasal approach. Drug Deliv. Transl. Res. 2020, 10, 1862–1875. [Google Scholar] [CrossRef]
- Jiang, Y.; Liu, C.; Zhai, W.; Zhuang, N.; Han, T.; Ding, Z. The Optimization Design of Lactoferrin Loaded HupA Nanoemulsion for Targeted Drug Transport via Intranasal Route. Int. J. Nanomed. 2019, 14, 9217–9234. [Google Scholar] [CrossRef] [PubMed]
- Kotta, S.; Mubarak Aldawsari, H.; Badr-Eldin, S.M.; Alhakamy, N.A.; Md, S. Coconut oil-based resveratrol nanoemulsion: Optimization using response surface methodology, stability assessment and pharmacokinetic evaluation. Food Chem. 2021, 357, 129721. [Google Scholar] [CrossRef] [PubMed]
- Nasr, M. Development of an optimized hyaluronic acid-based lipidic nanoemulsion co-encapsulating two polyphenols for nose to brain delivery. Drug Deliv. 2016, 23, 1444–1452. [Google Scholar] [CrossRef]
- Kumar, S.; Ali, J.; Baboota, S. Design Expert ® supported optimization and predictive analysis of selegiline nanoemulsion via the olfactory region with enhanced behavioural performance in Parkinson’s disease. Nanotechnology 2016, 27, 435101. [Google Scholar] [CrossRef] [PubMed]
- Das, S.S.; Sarkar, A.; Chabattula, S.C.; Verma, P.R.P.; Nazir, A.; Gupta, P.K.; Ruokolainen, J.; Kesari, K.K.; Singh, S.K. Food-Grade Quercetin-Loaded Nanoemulsion Ameliorates Effects Associated with Parkinson’s Disease and Cancer: Studies Employing a Transgenic C. elegans Model and Human Cancer Cell Lines. Antioxidants 2022, 11, 1378. [Google Scholar] [CrossRef]
- Gaba, B.; Khan, T.; Haider, M.F.; Alam, T.; Baboota, S.; Parvez, S.; Ali, J. Vitamin E Loaded Naringenin Nanoemulsion via Intranasal Delivery for the Management of Oxidative Stress in a 6-OHDA Parkinson’s Disease Model. Biomed Res. Int. 2019, 2019, 2382563. [Google Scholar] [CrossRef]
- da Silva Campelo, M.; Câmara Neto, J.F.; de Souza, Á.L.; Ferreira, M.K.A.; dos Santos, H.S.; Gramosa, N.V.; de Aguiar Soares, S.; Ricardo, N.M.P.S.; de Menezes, J.E.S.A.; Ribeiro, M.E.N.P. Clove volatile oil-loaded nanoemulsion reduces the anxious-like behavior in adult zebrafish. DARU J. Pharm. Sci. 2023, 31, 183–192. [Google Scholar] [CrossRef]
- Kumar, A.; Jain, S.K. Preliminary studies for the development of intranasal nanoemulsion containing CNS agent: Emphasizing the utilization of cut and weigh method. Artif. Cells Nanomed. Biotechnol. 2017, 45, 515–521. [Google Scholar] [CrossRef]
- Boche, M.; Pokharkar, V. Quetiapine Nanoemulsion for Intranasal Drug Delivery: Evaluation of Brain-Targeting Efficiency. AAPS PharmSciTech 2017, 18, 686–696. [Google Scholar] [CrossRef]
- Pandey, Y.R.; Kumar, S.; Gupta, B.K.; Ali, J.; Baboota, S. Intranasal delivery of paroxetine nanoemulsion via the olfactory region for the management of depression: Formulation, behavioural and biochemical estimation. Nanotechnology 2016, 27, 025102. [Google Scholar] [CrossRef] [PubMed]
- Zielińska, A.; Carreiró, F.; Oliveira, A.M.; Neves, A.; Pires, B.; Venkatesh, D.N.; Durazzo, A.; Lucarini, M.; Eder, P.; Silva, A.M.; et al. Polymeric Nanoparticles: Production, Characterization, Toxicology and Ecotoxicology. Molecules 2020, 25, 3731. [Google Scholar] [CrossRef] [PubMed]
- Elmowafy, M.; Shalaby, K.; Elkomy, M.H.; Alsaidan, O.A.; Gomaa, H.A.M.; Abdelgawad, M.A.; Mostafa, E.M. Polymeric Nanoparticles for Delivery of Natural Bioactive Agents: Recent Advances and Challenges. Polymers 2023, 15, 1123. [Google Scholar] [CrossRef]
- Wüpper, S.; Lüersen, K.; Rimbach, G. Cyclodextrins, Natural Compounds, and Plant Bioactives—A Nutritional Perspective. Biomolecules 2021, 11, 401. [Google Scholar] [CrossRef] [PubMed]
- Xu, W.; Li, X.; Wang, L.; Li, S.; Chu, S.; Wang, J.; Li, Y.; Hou, J.; Luo, Q.; Liu, J. Design of Cyclodextrin-Based Functional Systems for Biomedical Applications. Front. Chem. 2021, 9, 635507. [Google Scholar] [CrossRef]
- Ghitman, J.; Voicu, S.I. Controlled drug delivery mediated by cyclodextrin-based supramolecular self-assembled carriers: From design to clinical performances. Carbohydr. Polym. Technol. Appl. 2023, 5, 100266. [Google Scholar] [CrossRef]
- La Barbera, L.; Mauri, E.; D’Amelio, M.; Gori, M. Functionalization strategies of polymeric nanoparticles for drug delivery in Alzheimer’s disease: Current trends and future perspectives. Front. Neurosci. 2022, 16, 939855. [Google Scholar] [CrossRef] [PubMed]
- Nagpal, K.; Singh, S.K.; Mishra, D.N. Optimization of brain targeted chitosan nanoparticles of Rivastigmine for improved efficacy and safety. Int. J. Biol. Macromol. 2013, 59, 72–83. [Google Scholar] [CrossRef]
- Fazil, M.; Md, S.; Haque, S.; Kumar, M.; Baboota, S.; kaur Sahni, J.; Ali, J. Development and evaluation of rivastigmine loaded chitosan nanoparticles for brain targeting. Eur. J. Pharm. Sci. 2012, 47, 6–15. [Google Scholar] [CrossRef]
- Hanafy, A.S.; Farid, R.M.; Helmy, M.W.; ElGamal, S.S. Pharmacological, toxicological and neuronal localization assessment of galantamine/chitosan complex nanoparticles in rats: Future potential contribution in Alzheimer’s disease management. Drug Deliv. 2016, 23, 3111–3122. [Google Scholar] [CrossRef]
- Hassanzadeh, G.; Fallahi, Z.; Khanmohammadi, M.; Elmizadeh, H.; Sharifzadeh, M.; Nouri, K.; Heydarian, Z.; Mahakizadeh, S.; Zendedel, A.; Beyer, C.; et al. Effect of Magnetic Tacrine-Loaded Chitosan Nanoparticles on Spatial Learning, Memory, Amyloid Precursor Protein and Seladin-1 Expression in the Hippocampus of Streptozotocin-Exposed Rats. Int. Clin. Neurosci. J. 2016, 3, 25–31. [Google Scholar] [CrossRef]
- Yang, R.; Zheng, Y.; Wang, Q.; Zhao, L. Curcumin-loaded chitosan–bovine serum albumin nanoparticles potentially enhanced Aβ 42 phagocytosis and modulated macrophage polarization in Alzheimer’s disease. Nanoscale Res. Lett. 2018, 13, 330. [Google Scholar] [CrossRef]
- Elnaggar, Y.S.R.; Etman, S.M.; Abdelmonsif, D.A.; Abdallah, O.Y. Intranasal Piperine-Loaded Chitosan Nanoparticles as Brain-Targeted Therapy in Alzheimer’s Disease: Optimization, Biological Efficacy, and Potential Toxicity. J. Pharm. Sci. 2015, 104, 3544–3556. [Google Scholar] [CrossRef]
- Alam, S.; Mustafa, G.; Khan, Z.I.; Islam, F.; Bhatnagar, A.; Ahmad, F.J.; Kumar, M. Development and evaluation of thymoquinone-encapsulated chitosan nanoparticles for nose-to-brain targeting: A pharmacoscintigraphic study. Int. J. Nanomed. 2012, 7, 5705–5718. [Google Scholar] [CrossRef] [PubMed]
- Sánchez-López, E.; Ettcheto, M.; Egea, M.A.; Espina, M.; Cano, A.; Calpena, A.C.; Camins, A.; Carmona, N.; Silva, A.M.; Souto, E.B.; et al. Memantine loaded PLGA PEGylated nanoparticles for Alzheimer’s disease: In vitro and in vivo characterization. J. Nanobiotechnology 2018, 16, 32. [Google Scholar] [CrossRef]
- Quitschke, W.W.; Steinhauff, N.; Rooney, J. The effect of cyclodextrin-solubilized curcuminoids on amyloid plaques in Alzheimer transgenic mice: Brain uptake and metabolism after intravenous and subcutaneous injection. Alzheimer’s Res. Ther. 2013, 5, 16. [Google Scholar] [CrossRef]
- Wong, K.H.; Xie, Y.; Huang, X.; Kadota, K.; Yao, X.-S.; Yu, Y.; Chen, X.; Lu, A.; Yang, Z. Delivering Crocetin across the Blood-Brain Barrier by Using γ-Cyclodextrin to Treat Alzheimer’s Disease. Sci. Rep. 2020, 10, 3654. [Google Scholar] [CrossRef] [PubMed]
- Bi, C.; Wang, A.; Chu, Y.; Liu, S.; Mu, H.; Liu, W.; Wu, Z.; Sun, K.; Li, Y. Intranasal delivery of rotigotine to the brain with lactoferrin-modified PEG-PLGA nanoparticles for Parkinson’s disease treatment. Int. J. Nanomed. 2016, 11, 6547–6559. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, N. Rasagiline-encapsulated chitosan-coated PLGA nanoparticles targeted to the brain in the treatment of parkinson’s disease. J. Liq. Chromatogr. Relat. Technol. 2017, 40, 677–690. [Google Scholar] [CrossRef]
- Chen, T.; Liu, W.; Xiong, S.; Li, D.; Fang, S.; Wu, Z.; Wang, Q.; Chen, X. Nanoparticles Mediating the Sustained Puerarin Release Facilitate Improved Brain Delivery to Treat Parkinson’s Disease. ACS Appl. Mater. Interfaces 2019, 11, 45276–45289. [Google Scholar] [CrossRef] [PubMed]
- Barros, M.C.F.; Ribeiro, A.C.F.; Esteso, M.A. Cyclodextrins in Parkinson’s Disease. Biomolecules 2018, 9, 3. [Google Scholar] [CrossRef] [PubMed]
- Bari, N.K.; Fazil, M.; Hassan, M.Q.; Haider, M.R.; Gaba, B.; Narang, J.K.; Baboota, S.; Ali, J. Brain delivery of buspirone hydrochloride chitosan nanoparticles for the treatment of general anxiety disorder. Int. J. Biol. Macromol. 2015, 81, 49–59. [Google Scholar] [CrossRef] [PubMed]
- Mahmoud, K.Y.; Elhesaisy, N.A.; Rashed, A.R.; Mikhael, E.S.; Fadl, M.I.; Elsadek, M.S.; Mohamed, M.A.; Mostafa, M.A.; Hassan, M.A.; Halema, O.M.; et al. Exploring the potential of intranasally administered naturally occurring quercetin loaded into polymeric nanocapsules as a novel platform for the treatment of anxiety. Sci. Rep. 2023, 13, 510. [Google Scholar] [CrossRef] [PubMed]
- Jani, P.; Vanza, J.; Pandya, N.; Tandel, H. Formulation of polymeric nanoparticles of antidepressant drug for intranasal delivery. Ther. Deliv. 2019, 10, 683–696. [Google Scholar] [CrossRef]
- Cayero-Otero, M.D.; Gomes, M.J.; Martins, C.; Álvarez-Fuentes, J.; Fernández-Arévalo, M.; Sarmento, B.; Martín-Banderas, L. In vivo biodistribution of venlafaxine-PLGA nanoparticles for brain delivery: Plain vs. functionalized nanoparticles. Expert Opin. Drug Deliv. 2019, 16, 1413–1427. [Google Scholar] [CrossRef]
- Haque, S.; Md, S.; Fazil, M.; Kumar, M.; Sahni, J.K.; Ali, J.; Baboota, S. Venlafaxine loaded chitosan NPs for brain targeting: Pharmacokinetic and pharmacodynamic evaluation. Carbohydr. Polym. 2012, 89, 72–79. [Google Scholar] [CrossRef]
- Haque, S.; Md, S.; Sahni, J.K.; Ali, J.; Baboota, S. Development and evaluation of brain targeted intranasal alginate nanoparticles for treatment of depression. J. Psychiatr. Res. 2014, 48, 1–12. [Google Scholar] [CrossRef]
- Tong, G.-F.; Qin, N.; Sun, L.-W. Development and evaluation of Desvenlafaxine loaded PLGA-chitosan nanoparticles for brain delivery. Saudi Pharm. J. 2017, 25, 844–851. [Google Scholar] [CrossRef]
- Singh, D.; Rashid, M.; Hallan, S.S.; Mehra, N.K.; Prakash, A.; Mishra, N. Pharmacological evaluation of nasal delivery of selegiline hydrochloride-loaded thiolated chitosan nanoparticles for the treatment of depression. Artif. Cells Nanomed. Biotechnol. 2015, 44, 865–877. [Google Scholar] [CrossRef]
- Aree, T. Advancing insights on β-cyclodextrin inclusion complexes with SSRIs through lens of X-ray diffraction and DFT calculation. Int. J. Pharm. 2021, 609, 121113. [Google Scholar] [CrossRef] [PubMed]
- Martins, P.M.; Lima, A.C.; Ribeiro, S.; Lanceros-Mendez, S.; Martins, P. Magnetic Nanoparticles for Biomedical Applications: From the Soul of the Earth to the Deep History of Ourselves. ACS Appl. Bio Mater. 2021, 4, 5839–5870. [Google Scholar] [CrossRef] [PubMed]
- Zhao, J.; Xu, N.; Yang, X.; Ling, G.; Zhang, P. The roles of gold nanoparticles in the detection of amyloid-β peptide for Alzheimer’s disease. Colloid Interface Sci. Commun. 2022, 46, 100579. [Google Scholar] [CrossRef]
- Mao, X.; Xu, J.; Cui, H. Functional nanoparticles for magnetic resonance imaging. WIREs Nanomed. Nanobiotechnol. 2016, 8, 814–841. [Google Scholar] [CrossRef]
- Singh, A.V.; Bansod, G.; Mahajan, M.; Dietrich, P.; Singh, S.P.; Rav, K.; Thissen, A.; Bharde, A.M.; Rothenstein, D.; Kulkarni, S.; et al. Digital Transformation in Toxicology: Improving Communication and Efficiency in Risk Assessment. ACS Omega 2023, 8, 21377–21390. [Google Scholar] [CrossRef]
- Wei, H.; Wiśniowska, A.; Fan, J.; Harvey, P.; Li, Y.; Wu, V.; Hansen, E.C.; Zhang, J.; Kaul, M.G.; Frey, A.M.; et al. Single-nanometer iron oxide nanoparticles as tissue-permeable MRI contrast agents. Proc. Natl. Acad. Sci. USA 2021, 118, e2102340118. [Google Scholar] [CrossRef] [PubMed]
- Avasthi, A.; Caro, C.; Pozo-Torres, E.; Leal, M.P.; García-Martín, M.L. Magnetic Nanoparticles as MRI Contrast Agents. Top. Curr. Chem. 2020, 378, 40. [Google Scholar] [CrossRef]
- Yang, H.; Wang, H.; Wen, C.; Bai, S.; Wei, P.; Xu, B.; Xu, Y.; Liang, C.; Zhang, Y.; Zhang, G.; et al. Effects of iron oxide nanoparticles as T2-MRI contrast agents on reproductive system in male mice. J. Nanobiotechnol. 2022, 20, 98. [Google Scholar] [CrossRef]
- Korchinski, D.J.; Taha, M.; Yang, R.; Nathoo, N.; Dunn, J.F. Iron Oxide as an Mri Contrast Agent for Cell Tracking: Supplementary Issue. Magn. Reson. Insights 2015, 8s1, MRI.S23557. [Google Scholar] [CrossRef]
- Oberdick, S.D.; Jordanova, K.V.; Lundstrom, J.T.; Parigi, G.; Poorman, M.E.; Zabow, G.; Keenan, K.E. Iron oxide nanoparticles as positive T1 contrast agents for low-field magnetic resonance imaging at 64 mT. Sci. Rep. 2023, 13, 11520. [Google Scholar] [CrossRef]
- Tang, T.; Valenzuela, A.; Petit, F.; Chow, S.; Leung, K.; Gorin, F.; Louie, A.Y.; Dhenain, M. In Vivo MRI of Functionalized Iron Oxide Nanoparticles for Brain Inflammation. Contrast Media Mol. Imaging 2018, 2018, 3476476. [Google Scholar] [CrossRef] [PubMed]
- Yu, M.; Huang, S.; Yu, K.J.; Clyne, A.M. Dextran and Polymer Polyethylene Glycol (PEG) Coating Reduce Both 5 and 30 nm Iron Oxide Nanoparticle Cytotoxicity in 2D and 3D Cell Culture. Int. J. Mol. Sci. 2012, 13, 5554–5570. [Google Scholar] [CrossRef] [PubMed]
- Cheng, K.K.; Chan, P.S.; Fan, S.; Kwan, S.M.; Yeung, K.L.; Wáng, Y.-X.J.; Chow, A.H.L.; Wu, E.X.; Baum, L. Curcumin-conjugated magnetic nanoparticles for detecting amyloid plaques in Alzheimer’s disease mice using magnetic resonance imaging (MRI). Biomaterials 2015, 44, 155–172. [Google Scholar] [CrossRef] [PubMed]
- Fernández, T.; Martínez-Serrano, A.; Cussó, L.; Desco, M.; Ramos-Gómez, M. Functionalization and Characterization of Magnetic Nanoparticles for the Detection of Ferritin Accumulation in Alzheimer’s Disease. ACS Chem. Neurosci. 2018, 9, 912–924. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.Y.; Chang, K.-A. Therapeutic Potential of Magnetic Nanoparticle-Based Human Adipose-Derived Stem Cells in a Mouse Model of Parkinson’s Disease. Int. J. Mol. Sci. 2021, 22, 654. [Google Scholar] [CrossRef] [PubMed]
- Sivaji, K.; Kannan, R.R. Polysorbate 80 Coated Gold Nanoparticle as a Drug Carrier for Brain Targeting in Zebrafish Model. J. Clust. Sci. 2019, 30, 897–906. [Google Scholar] [CrossRef]
- Sardjono, R.E.; Khoerunnisa, F.; Musthopa, I.; Akasum, N.S.M.M.; Rachmawati, R. Synthesize, characterization, and anti-Parkinson activity of silver-Indonesian velvet beans (Mucuna pruriens) seed extract nanoparticles (AgMPn). J. Phys. Conf. Ser. 2018, 1013, 012195. [Google Scholar] [CrossRef]
- Kim, M.J.; Rehman, S.U.; Amin, F.U.; Kim, M.O. Enhanced neuroprotection of anthocyanin-loaded PEG-gold nanoparticles against Aβ1-42-induced neuroinflammation and neurodegeneration via the NF-KB /JNK/GSK3β signaling pathway. Nanomed. Nanotechnol. Biol. Med. 2017, 13, 2533–2544. [Google Scholar] [CrossRef]
- Khadrawy, Y.A.; Hosny, E.N.; Magdy, M.; Mohammed, H.S. Antidepressant effects of curcumin-coated iron oxide nanoparticles in a rat model of depression. Eur. J. Pharmacol. 2021, 908, 174384. [Google Scholar] [CrossRef]
- Lu, H.; Zhang, S.; Wang, J.; Chen, Q. A Review on Polymer and Lipid-Based Nanocarriers and Its Application to Nano-Pharmaceutical and Food-Based Systems. Front. Nutr. 2021, 8, 783831. [Google Scholar] [CrossRef]
- van der Koog, L.; Gandek, T.B.; Nagelkerke, A. Liposomes and Extracellular Vesicles as Drug Delivery Systems: A Comparison of Composition, Pharmacokinetics, and Functionalization. Adv. Healthc. Mater. 2022, 11, 2100639. [Google Scholar] [CrossRef]
- Akel, H.; Csóka, I.; Ambrus, R.; Bocsik, A.; Gróf, I.; Mészáros, M.; Szecskó, A.; Kozma, G.; Veszelka, S.; Deli, M.A.; et al. In Vitro Comparative Study of Solid Lipid and PLGA Nanoparticles Designed to Facilitate Nose-to-Brain Delivery of Insulin. Int. J. Mol. Sci. 2021, 22, 13258. [Google Scholar] [CrossRef] [PubMed]
- Kasina, V.; Mownn, R.J.; Bahal, R.; Sartor, G.C. Nanoparticle delivery systems for substance use disorder. Neuropsychopharmacology 2022, 47, 1431–1439. [Google Scholar] [CrossRef] [PubMed]
- Ross, A.M.; Kennedy, T.; McNulty, D.; Leahy, C.I.; Walsh, D.R.; Murray, P.; Grabrucker, A.M.; Mulvihill, J.J.E. Comparing nanoparticles for drug delivery: The effect of physiological dispersion media on nanoparticle properties. Mater. Sci. Eng. C 2020, 113, 110985. [Google Scholar] [CrossRef] [PubMed]
- Kaushik, A.; Jayant, R.D.; Bhardwaj, V.; Nair, M. Personalized nanomedicine for CNS diseases. Drug Discov. Today 2018, 23, 1007–1015. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; He, R.; Yan, H.; Leng, Z.; Zhu, S.; Gu, Z. Nanotechnology for the diagnosis and treatment of Alzheimer’s disease: A bibliometric analysis. Nano Today 2022, 47, 101654. [Google Scholar] [CrossRef]
- Alghamdi, M.A.; Fallica, A.N.; Virzì, N.; Kesharwani, P.; Pittalà, V.; Greish, K. The Promise of Nanotechnology in Personalized Medicine. J. Pers. Med. 2022, 12, 673. [Google Scholar] [CrossRef]
- Foulkes, R.; Man, E.; Thind, J.; Yeung, S.; Joy, A.; Hoskins, C. The regulation of nanomaterials and nanomedicines for clinical application: Current and future perspectives. Biomater. Sci. 2020, 8, 4653–4664. [Google Scholar] [CrossRef]
- EMA. Withrawal Assessment Report for Sinerem (EMEA/CHMP/11527/2008); European Medicines Agency: London, UK, 2008. [Google Scholar]
- National Library of Medicine. ClinicalTrials.gov. Available online: https://clinicaltrials.gov/ (accessed on 20 November 2023).
- Herdiana, Y.; Wathoni, N.; Shamsuddin, S.; Muchtaridi, M. Scale-up polymeric-based nanoparticles drug delivery systems: Development and challenges. OpenNano 2022, 7, 100048. [Google Scholar] [CrossRef]


| Target/Disease | Drug(s) | Nanoparticle Type | Composition | Functionalization | Diameter of the Optimized Formulation(s) (nm) | Observations | Ref. |
|---|---|---|---|---|---|---|---|
| AD | Curcumin | Exosome | Macrophage RAW264.7 cells treated with curcumin | Exosome inherited the lymphocyte function-associated antigen 1 from their parental cells, a protein that interacts with the endothelial intercellular adhesion molecule 1 | 117 | Exosome improved the solubility and bioavailability of curcumin and increased drug penetration across the BBB. Exosomes derived from curcumin-treated RAW264.7 cells relieved the symptoms of AD by inhibiting phosphorylation of the tau protein via activating the AKT/GSK-3β pathway. | [77] |
| AD | Quercetin | Exosome | Isolated from whole blood of SD rats | Inherited heat shock protein 70 | 150 | The bioavailability of quercetin was enhanced via loading into the exosome, relieving the symptoms of AD in okadaic-acid-induced AD mice, by inhibiting the cyclin-dependent-kinase-5-mediated phosphorylation of tau and reducing the formation of insoluble neurofibrillary tangles (NFTs). | [78] |
| AD | GAPDH small interfering RNA | Exosome | Bone marrow from inbred C57BL/6 mice. Dendritic cells with granulocyte/macrophage-colony stimulating factor were selected | Three different peptides—RVG peptide, a muscle-specific peptide (MSP), and a FLAG epitope—were cloned into Lamp2b | 80 | Intravenously injected RVG-targeted exosomes delivered glyceraldehyde 3-phosphate dehydrogenase siRNA specifically to neurons, microglia, and oligodendrocytes in the brain, resulting in strong mRNA and protein knockdown of BACE1. | [79] |
| PD | Dopamine (DA) | Exosome | Blood samples from the orbit venous plexus of Kunming mice containing CD9, CD63, and CD81 marker proteins | - | 40–200 (70% in the range of 70–100) | In vitro and in vivo studies demonstrated the successful delivery of DA to the brain using exosomes, including the striatum and substantia nigra. Brain distribution of DA increased >15-fold by using the blood exosomes as a delivery system. DA-loaded exosomes showed much better therapeutic efficacy in 6-OHDA-treated mice and lower systemic toxicity than free DA after intravenous administration. | [80] |
| PD | Catalase | Exosome | Raw 264.7 macrophages | - | 100–200 | Exosomes were readily taken up by neuronal cells in vitro. A considerable number of exosomes was detected in 6-OHDA-treated mice brains following intranasal administration, providing significant neuroprotective effects in in vitro and in vivo models of PD. | [81] |
| PD | Synuclein small interfering RNA | Exosome | Murine dendritic cells harvested from bone marrow | Expressing RVG | 100 | In normal and in S129D α-syn transgenic mice, the authors detected significantly reduced α-synuclein mRNA and protein levels throughout the brain after treatment with RVG exosomes loaded with siRNA for α-synuclein. | [82] |
| PD | DNA aptamer targeting α-synuclein aggregates | Exosome | HEK293T cells | Expressing RVG-Lamp2b | - | The aptamer-loaded RVG exosomes significantly reduced the α-synuclein preformed fibril-induced pathological aggregates and rescued synaptic protein (synapsin II and SNAP25) loss and neuronal death. Additionally, intraperitoneal administration of these exosomes into mice treated intra-striatally with α-synuclein preformed fibrils reduced the pathological α-synuclein aggregates and improved motor impairments. | [83] |
| Target/Disease | Drug(s) | Nanoparticle Type | Composition | Functionalization | Diameter of the Optimized Formulation(s) (nm) | Observations | Ref. |
|---|---|---|---|---|---|---|---|
| AD | Nicotinamide | SLN | Stearic acid and phospholipon® 90 G (as the oil phase) and sodium taurocholate and ultrapure water (as the water phase) | Polysorbate 80, phosphatidylserine or phosphatidic acid | 112, 124, 137 | The results of Morris water maze and also histopathological and biochemical tests demonstrated the effectiveness of intraperitoneal injection of phosphatidylserine-functionalized SLNs in improving cognition, preserving the neuronal cells, and reducing tau hyperphosphorylation in a rat model of AD. | [84] |
| AD | Galantamine hydrobromide | SLN | Compritol (glyceryl behnate), pluronic F-127 (250 mg) as surfactant and Tween 80 as co-surfactant | - | 88–221 | In vivo assays demonstrated a significant memory restoration capability in cognitive deficit rats in comparison with free drug. The developed carriers offered approximately twice the bioavailability of the free drug. | [85] |
| AD | Quercetin | SLN | Compritol and Tween 80 as the surfactant | - | 159 | In all the in vivo behavioral (spatial navigation task, elevated plus maze paradigm, gross behavioral activity) and biochemical (lipid peroxidation, glutathione levels, and nitrite levels) experiments, the rats treated with SLN-encapsulated quercetin showed markedly better memory retention than free quercetin-treated rats. | [86] |
| AD | Piperine | SLN | Glycerol mono stearate, Epikuron 200, Tween 80, Tween 20 | Polysorbate-80 coating | 312 | Ibotenic acid-stimulated lesions of basalis magnacellularis were developed in albino Wister rats. SLNs containing piperine reduced the SOD values, increased the AChE values, reduced immobility in the forced swimming test, and showed superior results than donepezil. Histopathology studies revealed reduced plaques and tangles. | [87] |
| AD | Epigallocatechin-3-O-gallate (EGCG) | SLN | - | - | 50 | Nano-EGCG more than doubled the oral bioavailability of EGCG in rats and also was more effective at promoting α-secretase activity in vitro. | [88] |
| AD | Curcumin | SLN | Soy lecithin and water | Polysorbate 80 | 135 | Young male Lacca mice were treated with AlCl3 to induce alterations in the brain histopathology, loss of cognition, and oxidative damage. Behavioral assessments using a Morris water maze test, biochemical measurements (AChE activity, lipid peroxidation, reduced glutathione, superoxide dismutase, catalase, blood lipid profile), and histopathological analysis were performed. Curcumin SLNs completely reversed the induced alterations. | [89] |
| PD | Apomorphine | SLN | Glyceryl monostearate (GMS) or polyethylene glycol monostearate (PMS) | - | 155, 63 | 6-OHDA-lesioned rats were orally administered with apomorphine. The total number of rotations increased from 20 to 94 and from 20 to 115 when the drug was administered from SLNs containing GMS and PMS, respectively. | [90] |
| PD | Ropinirole hydrochloride | SLN | Pluronic F68, stearylamine | - | 66 | Physicochemical characterization and pharmacodynamic studies. | [91] |
| PD | Naringenin | SLN | Glycerol monostearate, Tween 80, and F68 non-ionic surfactant | - | 135 | Neuroprotective activity of naringenin–SLN was evaluated using a rotenone-induced PD model in Wistar rats. Results of behavioral observations (in the Rota rod test) and biomarkers (reduced gluthatione, SOD, CAT, lipid peroxidation) showed that naringenin loaded SLN can exert neuroprotective effects. | [92] |
| Depression/anxiety | Fluoxetine | SLN | Precirol®, lauroglycol™, tween80 | - | 128–158 | The intranasal delivery of the optimal lipid nanoparticle formulation reduced both depressive and anxiety-like behaviors in adult CD1 mice (assessment using a mice marble-burying test (MBT) and mice forced swimming test (FST)) | [93] |
| Target/Disease | Drug(s) | Nanoparticle Type | Composition | Functionalization | Globule Size of the Optimized Formulation(s) (nm) | Observations | Ref. |
|---|---|---|---|---|---|---|---|
| AD | Memantine hydrochloride | NE | Labrasol, Tween 20, PEG | - | ~11 | NE displayed antioxidant activity (FRAP and DPPH), and 98% cell viability in the Neuro 2a cell line. Biodistribution results showed NE uptake in the brains of rats when administered intranasally. | [97] |
| AD | Donepezil | NE | Labrasol, cetyl pyridinium chloride, glycerol | - | 65 | Cell viability in the Neuro 2a cell line was 76.3% for the NE and 85% for donepezil solution. In vivo assays showed that rats intranasally administered with the NE showed maximum distribution in the brain and it remained in the target site until 24 h, while no brain uptake was seen in the rats orally administered with the NE. The rats intravenously administered with the NE or intranasally administered with donepezil solution showed only trace amounts of drug distribution in the brain. | [98] |
| AD | Huperzine A | NE | Isopropylmyristate, Capryol 90, Cremophor EL + Labrasol | Lactoferrin (Lf) | 15 (without Lf), 17 (with Lf) | Lf–huperzine A-NE showed better uptake for the hCMEC/D3 cell line than unmodified huperzine A-NE. Similar results were found in in vivo assays. | [99] |
| AD | Resveratrol | NE | Coconut oil, pluronic and cremophor EL | - | 111 | In Wistar rats, the brain-targeted efficiency was higher after intranasal administration of resveratrol NE (2 mg/kg) compared with that of resveratrol suspension. | [100] |
| AD | Curcumin + resveratrol | NE | Labrafac lipophile/cremophor 40, with hyaluronic acid | 115 | NEs displayed antioxidant activity (DPPH method). Moreover, the integrity of the lining epithelium of the nasal cavity was maintained after repeated administration of hyaluronic-acid-based NEs co-encapsulating curcumin and resveratrol, with no inflammatory cellular infiltration in the lamina propria of the mucosal lining. NEs successfully increased the amount of both polyphenols in the brain of male Albino rats. | [101] | |
| PD | Selegiline | NE | Grape seed oil, Sefsol 218®, Tween 80, lauroglycol 90 | - | 61 | Behavior studies (FST, locomotor activity test, catalepsy, muscle coordination test, akinesia test, pole test) were undertaken. Rats were treated with haloperidol to induce PD. Selegiline NE (administered intranasally) showed significant improvement in behavioral activities in comparison to the orally administered free drug. | [102] |
| PD | Quercetin | NE | Capmul MCM NF and cremophor RH 40 | - | ~50 | In vivo results show that quercetin-loaded NEs potentially reduced α-synuclein aggregation, increased mitochondrial and fat content, and improved the lifespan in transgenic C. elegans strain NL5901. Moreover, quercetin NEs significantly downregulated the reactive oxygen species (ROS) levels in wild-type C. elegans strain N2 more efficiently than pure quercetin. | [103] |
| PD | Naringenin | NE | Vitamin E: Capryol 90 (1:1), Tween 80, transcutol-HP, and water | - | 39 | Behaviors in 6-OHDA-treated rats were successfully reversed after intranasal administration of naringenin NE along with the levodopa. Naringenin NE + levodopa also induced higher levels of GSH and SOD and lower levels of MDA. | [104] |
| Anxiety | Clove volatile oil (contains eugenol) | NE | Coconut oil, polysaccharides from Agaricus blazei Murill mushroom, Tween 80, and water | - | 227 to 333 | Clove volatile oil (CVO), eugenol, a CVO NE, and an empty NE presented low acute toxicity in zebrafish. The CVO NE reduced the anxious-like behavior of adult zebrafish without affecting their locomotor activity. However, CVO and eugenol displayed anxiolytic activity but reduced animal locomotion similarly to benzodiazepines (diazepam). The observed anxiolytic activity of the CVO, eugenol, and CVO NE is linked to the GABAergic pathway. | [105] |
| Depression | Fluoxetine | NE | Capmul MCM, labrasol, transcutol-P | - | - | Nasal ciliotoxicity studies were performed to evaluate any potential toxic effects of excipients used in the NE formulation on the nasal mucosa. The blank NE displayed no damage to nasal mucosa showing their potential for intranasal delivery. | [106] |
| Depression | Quetiapine fumarate | NE | Capmul MCM, Tween 80, transcutol P, PEG, water | - | 144 | In vivo studies were performed in male Wistar rats after intravenous and intranasal administration of quetiapine pure drug and an NE containing quetiapine. Superiority of the NE for intranasal delivery was observed. | [107] |
| Depression | Paroxetine | NE | Capmul MCM, Solutol HS 15, and PEG | - | 59 | Permeation studies revealed increased permeation of the paroxetine NE (2.57-fold) compared to the paroxetine suspension. Behavioral studies (FST and locomotor activity test) in Wistar rats showed that treatment with paroxetine NE (administered intranasally) significantly improved the behavioral activities in comparison to paroxetine suspension (orally administered). The NEs were also effective in counterbalancing oxidative stress. | [108] |
| Target/Disease | Drug(s) | Nanoparticle Type | Composition | Functionalization | Diameter of the Optimized Formulation(s) (nm) | Observations | Ref. |
|---|---|---|---|---|---|---|---|
| AD | Rivastigmine | Chitosan-based polymeric nanoparticles | Chitosan, tri-polyphosphate pentasodium | Tween 80® | 154 | Compared to both pure rivastigmine and uncoated nanoparticles, Tween 80®-coated nanoparticles induced significant reversal of scopolamine-induced effects. Coated nanoparticles also increased the maximum tolerable dose of rivastigmine. | [115] |
| AD | Rivastigmine | Chitosan-based polymeric nanoparticles | Chitosan, sodium tripolyphosphate | - | 164 | Intranasal administration showed higher brain targeting of rivastigmine using chitosan nanoparticles compared to other tested formulations. | [116] |
| AD | Galantamine | Chitosan-based polymeric nanoparticles | Chitosan, sodium tripolyphosphate | Tween 80® | 48–68 | Nasal administration of chitosan nanoparticles exhibited a significant decrease in the AChE protein level and activity in rat brains compared to the oral and nasal free galantamine solutions. | [117] |
| AD | Tacrine | Chitosan-based polymeric nanoparticles | Chitosan | - | - | The application of tacrine-loaded chitosan nanoparticles selectively increased the tacrine concentration in the brain tissue. Tacrine-loaded non-magnetic and tacrine-loaded magnetic chitosan nanoparticles improved spatial learning and memory after streptozotocin treatment in Wistar rats, with magnetic nanoparticles being the most effective. Tacrine-loaded chitosan nanoparticles increased seladin-1 and reduced APP gene expression. | [118] |
| AD | Curcumin | Chitosan-based polymeric nanoparticles | Chitosan | Bovine serum albumin (BSA) | 144 | Curcumin-loaded chitosan/BSA nanoparticles effectively increased drug penetration through the BBB, promoted the activation ofmicroglia, and further accelerated the phagocytosis of the Aβ peptide. They also inhibited the TLR4-MAPK/NF-κB signaling pathway and further downregulated M1 macrophage polarization. | [119] |
| AD | Piperine | Chitosan-based polymeric nanoparticles | Chitosan, sodium tripolyphosphate, poloxamer 188 | - | 249 | Piperine nanoparticles could significantly improve cognitive functions as efficiently as the standard drug (donepezil injection) with additional advantages of a dual mechanism of action (AChE inhibition and antioxidant effect). | [120] |
| AD | Thymoquinone | Chitosan-based polymeric nanoparticles | Chitosan, sodium tripolyphosphate | - | 172–281 | Intranasal thymoquinone-loaded nanoparticles were more effective in brain targeting compared to intravenous and intranasal thymoquinone solutions. | [121] |
| AD | Memantine | PLGA-based polymeric nanoparticles | Poly(lactic-co-glycolic acid) (PLGA) | PEG | 153 | Nanoparticles were able to cross the BBB. Behavioral tests in transgenic APPswe/PS1dE9 mice demonstrated that nanoparticles decreased memory impairment in comparison to the free drug solution. Memantine–PEG–PLGA nanoparticles reduced Aβ plaques and the associated inflammation characteristics of AD. | [122] |
| AD | BACE1-ASshRNA + D-peptide | Dendrigraft poly L-lysines | Dendrigraft poly-l-lysines, α-malemidyl-ω-N-hydroxysuccinimidyl polyethyleneglycol | Two peptides—RVG-29 and D-peptide | 97, 110 | Downregulation of the key enzyme in Aβ formation was achieved by delivering non-coding RNA plasmid. Simultaneous delivery of the therapeutic gene and peptide into the brain led to a reduction in neurofibrillary tangles. Meanwhile, memory loss rescue in AD mice was also observed. | [7] |
| AD | Curcuminoids | Cyclodextrin | 2-hydroxypropyl-cyclodextrin | - | - | Curcuminoids are rapidly metabolized after intravenous injection into APPSWE/PS1dE9 transgenic mice, and their effect on reducing the plaque load associated with AD may be dependent on the frequency of administration. | [123] |
| AD | Crocetin | Cyclodextrin | γ-Cyclodextrin | - | - | A water-soluble crocetin-γ-cyclodextrin inclusion complex was nontoxic to normal neuroblastoma cells (N2a cells and SH-SY5Y cells) and AD model cells (7PA2 cells). Furthermore, it showed a stronger ability to downregulate the expression of C-terminus fragments and the level of Aβ in 7PA2 cells compared to the crocetin free drug. Both the inclusion complex and crocetin were able to prevent SH-SY5Y cell death from H2O2-induced toxicity. | [124] |
| PD | Rotigotine | PLGA-based polymeric nanoparticles | PLGA | PEG, lactoferrin | 122 | Qualitative and quantitative cellular uptake studies demonstrated that accumulation of rotigotine was greater when using lactoferrin coating. In addition, intranasal delivery of rotigotine was much more effective with lactoferrin-coated nanoparticles than with uncoated nanoparticles. Rotigotine concentration was higher in the striatum, the primary region affected in PD. | [125] |
| PD | Rasagiline | Chitosan coated PLGA- polymeric nanoparticles | PLGA | Chitosan | 122 | Intranasal delivery of mucoadhesive nanocarrier showed significant enhancement of bioavailability in brain, after administration of the rasagiline-chitosan-PLGA-nanoparticles which could be a substantial achievement of direct nose to brain targeting in PD therapy and related brain disorders. | [126] |
| PD | Puerarin | PLGA-based polymeric nanoparticles | s-PLGA | D-α-tocopherol poly(ethylene glycol)1000 succinate | 88 | Relative to puerarin alone, encapsulated puerarin exhibited significantly improved cellular internalization, permeation, and neuroprotective effects in zebrafish, rats, and MPTP-treated mice. | [127] |
| PD | L-DOPA | Cyclodextrin | β-cyclodextrin, 2-hydroxypropyl-β-cyclodextrin | - | - | - | [128] |
| Anxiety | Buspirone hydrochloride | Chitosan-based polymeric nanoparticles | thiolated chitosan, chitosan, sodium tripolyphosphate, sodium alginate | - | 227 | The brain concentration achieved after intranasal administration of buspirone/chitosan nanoparticles was higher than that achieved with intravenous or with intranasal administration of free buspirone. | [129] |
| Anxiety | Quercetin | Polycaprolactone-based polymeric nanoparticles | Polycaprolactone, Span 80, Capryol 90, | Tween 80® or poloxamer 188 | 228 | Behavioral tests demonstrated the superiority of quercetin-loaded polymeric nanocapsules administered intranasally compared to quercetin solution administered both orally and intranasally. | [130] |
| Depression | Agomelatine | PLGA-based polymeric nanoparticles | PLGA, poloxamer 407 | - | 116 | Pharmacodynamic studies showed a significant reduction in immobility time in forced swimming tests in rats intranasally treated with the formulation, which indicated the antidepressant activity of the formulation. | [131] |
| Depression | Venlafaxine | PLGA-based polymeric nanoparticles | PLGA | Transferrin or a specific peptide against transferrin receptor | 230 | In vivo studies showed that non-functionalized nanoparticles reached the brain more efficiently than functionalized ones after intranasal administration. Probably, plain NPs travel via the direct nose-to-brain route whereas functionalized NPs reach the brain via receptor-mediated endocytosis. | [132] |
| Depression | Venlafaxine | Chitosan-based polymeric nanoparticles | Chitosan, sodium tripolyphosphate | - | 168 | The higher drug transport efficiency and intranasal direct transport percentage of venlafaxine/chitosan nanoparticles compared to other formulations (non-encapsulated venlafaxine via oral and intranasal route) suggest their better efficacy in the treatment of depression. | [133] |
| Depression | Venlafaxine | Alginate and chitosan-based polymeric nanoparticles | Alginate, chitosan | - | 174 | Intranasal administration of venlafaxine-alginate nanoparticles delivered greater amounts of venlafaxine to the brain in comparison to the free drug solution. | [134] |
| Depression | Desvenlafaxine | PLGA-chitosan polymeric nanoparticles | PLGA, chitosan | - | 173 | The optimized desvenlafaxine-loaded PLGA/chitosan nanoparticles on intranasal administration significantly reduced the symptoms of depression and enhanced the level of monoamines in the brain in Wistar rats in comparison with orally administered desvenlafaxine. Intranasal delivery of desvenlafaxine PLGA/chitosan nanoparticles also enhanced the pharmacokinetic profile of desvenlafaxine in the brain. | [135] |
| Depression | Selegiline hydrochloride | Chitosan-based polymeric nanoparticles | Thiolated chitosan | - | 215 | Forced swimming and tail suspension tests were used to evaluate the antidepressant activity, in which elevated immobility time was found to be reduced upon treatments. Thiolated chitosan nanoparticles seem to be promising candidates for nose-to-brain delivery in the evaluation of antidepressant activity. | [136] |
| Depression | Sertraline hydrochloride | Cyclodextrin | β-Cyclodextrin | - | - | Physicochemical characterization of the nanoparticles. | [137] |
| Depression | Fluoxetine hydrochloride | Cyclodextrin | β-Cyclodextrin | - | - | Physicochemical characterization of the nanoparticles. | [137] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Grosso, C.; Silva, A.; Delerue-Matos, C.; Barroso, M.F. Single and Multitarget Systems for Drug Delivery and Detection: Up-to-Date Strategies for Brain Disorders. Pharmaceuticals 2023, 16, 1721. https://doi.org/10.3390/ph16121721
Grosso C, Silva A, Delerue-Matos C, Barroso MF. Single and Multitarget Systems for Drug Delivery and Detection: Up-to-Date Strategies for Brain Disorders. Pharmaceuticals. 2023; 16(12):1721. https://doi.org/10.3390/ph16121721
Chicago/Turabian StyleGrosso, Clara, Aurora Silva, Cristina Delerue-Matos, and Maria Fátima Barroso. 2023. "Single and Multitarget Systems for Drug Delivery and Detection: Up-to-Date Strategies for Brain Disorders" Pharmaceuticals 16, no. 12: 1721. https://doi.org/10.3390/ph16121721
APA StyleGrosso, C., Silva, A., Delerue-Matos, C., & Barroso, M. F. (2023). Single and Multitarget Systems for Drug Delivery and Detection: Up-to-Date Strategies for Brain Disorders. Pharmaceuticals, 16(12), 1721. https://doi.org/10.3390/ph16121721