1. Introduction
Hyperglycemia, hyperlipidemia, and hypertension are currently the top three major chronic diseases in Taiwan. According to the Nutrition and Health Survey in Taiwan (NAHSIT) data from 2005 to 2008, the prevalence of hyperuricemia (HUA) in Taiwan has increased each year. Further, hyperuricemia has gradually become the fourth most prevalent chronic disease [
1]. High uric acid (UA) concentrations in the body that persist for a long time can increase the risk of gout, cardiovascular disease, kidney-related diseases, diabetes, hypertension, and hyperlipidemia. The current treatment of hyperuricemia is based on pharmaceutical intervention, which is supplemented by changes in diet and lifestyle. However, long-term use of medication to lower uric acid levels may cause severe allergic reactions, kidney injury, and even death [
2].
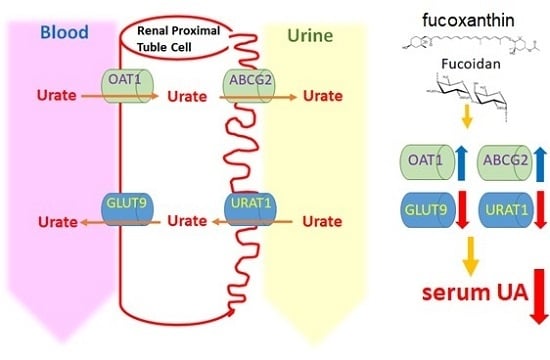
In the kidney, there are millions of renal tubular cells with different uric acid-related transporter proteins on either their apical or basolateral membrane [
3]. Different proteins are responsible for regulating the concentration of uric acid in the body. Urate transporter protein 1 (UTAT1), a protein on the apical membrane in the proximal tubular epithelial cells, is responsible for regulating the reabsorption of uric acid into renal proximal tubule epithelial cells. Glucose transporter protein 9 (GLUT9) is located on the outside of the basolateral membrane of the renal tubules, and it regulates the reabsorption of urate into the blood to control the amount of uric acid that enters the bloodstream. The organic anion transporter (OAT1) is present on the basolateral membrane of the renal tubule, and its major function is to uptake urate anions from the circulatory system and secrete them into tubular cells. The human ATP-binding cassette (subfamily G2, ABCG2) is a protein that exists on the apical membrane of the proximal convoluted tubule of the kidney, and it is responsible for regulating urate and secreting it into the collecting duct for excretion.
Many recent studies have investigated the effects of ingesting natural extracts to prevent or ameliorate hyperuricemia. Fucoidan (Fc) is a sulfated fucose-rich polysaccharide that is present in high levels in brown seaweed and has been shown to have anticancer and antioxidant effects in animal experiments [
4]. Fucoxanthin (Fx) is a red-orange carotenoid that is extracted from natural seaweed. It has been reported to have a potential in improving obesity [
5] and having anti-cancer effects [
6]. Moreover, the combination of Fc and Fx treatment has been reported to have a role in improving the glucose homeostasis and lipid metabolism in the type II diabetes mouse model [
7], as well as in improving the ventricular rhythm and muscular function of the aging mouse model [
8]. However, the effect of combining Fc and Fx to prevent hyperuricemia is still unclear. Therefore, the purpose of this study was to investigate whether fucoidan and fucoxanthin have a preventive effect on hyperuricemia.
3. Discussion
The hyperuricemia rodent model can be induced through different inhibition pathways as follows. (1) Enhancement of the uric acid level in the body by the administration of uric acid directly [
9], high-purine food such as fructose [
10], or uric acid precursors, such as hypoxanthine (Hx) [
11], which can produce uric acid to establish the model. (2) Inhibition of the excretion of uric acid through the kidneys. The treatment of adenine or ethambutol [
12] can prevent uric acid excretion from the kidneys, leading to an increase in the concentration of uric acid in the serum. (3) Inhibition of uricase activity, which is a common model in rodent experiments. Potassium oxonate (PO), an inhibitor of uricase, can be used to suppress uricase activity through competing with uric acid for binding to uricase [
13,
14,
15]. (4) A hyperuricemia animal model can be obtained by knocking down the uricase gene in rodents [
16]. However, for better induction results, some studies have combined two or three methods. In the present study, the treatment with uricase inhibitor potassium oxonate (PO, 300 mg/kg) alone was not satisfactory after 12 h. We found that the uric acid levels in each group were not different from those in the control group (data not shown). Therefore, we modified the strategy, and the treatment of rats with a combination of PO (300 mg/kg) and HX (HX, 300 mg/kg) at 4 h significantly increased the serum uric acid concentration. Therefore, this model was used to perform further experiments in this study.
It has been reported that after the induction of rat hyperuricemia status by treatment with adenine (200 mg/kg) and ethambutol (250 mg/kg) for 10 days, the kidney-to-body weight ratio (kidney weight index) of the hyperuricemia group was significantly increased compared with the control group. The pale, swollen, and coarse morphology of the kidney was observed, which means that the kidney underwent a pathological change in the hyperuricemia [
12]. Researchers have also mentioned that in their experiment on hyperuricemia induced by adenine (0.1 g/kg) with potassium oxonate (1.5 g/kg) for six weeks, the kidney weight index of the hyperuricemia group was significantly increased compared with the control group [
17]. Moreover, rats were administered potassium oxonate (250 mg/kg) daily, along with a subcutaneous injection of hypoxanthine (10 mg/kg) for two weeks. The results showed a significant increase in the kidney weight index in the hyperuricemia group compared with the control group [
18]. In the present study, the acute hyperuricemic rat model was generated by co-treatment with potassium oxonate (300 mg/kg) combined with hypoxanthine (300 mg/kg) for four hours. According to our result, the kidney index was not altered in the hyperuricemic rat group, suggesting that the induction time in our model was shorter than that in the previous study, and a significant difference between the hyperuricemia group and each of the other groups could not be observed.
The level of serum blood urea nitrogen (BUN) and creatinine was used to evaluate the kidney function. Previously, it has been reported that one hour after hyperuricemia was induced by potassium oxonate, interventions comprising different concentrations of astilbin (5, 10, 20 mg/kg) were applied for seven consecutive days. The results showed that the BUN and creatinine in the serum level in the hyperuricemia group were significantly increased compared with those in the control group. After the intervention, both BUN and creatinine significantly decreased in a dose-dependent manner [
19]. In addition, the plasma BUN and serum creatinine levels were increased in the adenine/ethambutol-induced hyperuricemic rat, and this symptom can be rescued by intervention with taurine that was applied for seven days [
12]. In our study, both serum BUN and creatinine were not altered, suggesting that the acute PO/HX-induced hyperuricemic rat model in this study did not cause any kidney damage. However, the BUN level in the allopurinol treatment (as a positive control) group was significantly increased compared with the hyperuricemia group, implying that the kidney function may become impaired by long-term administration of allopurinol. In agreement with our results, patients with allopurinol hypersensitivity has been reported to have a higher risk for renal or cardiovascular disease.
It has been shown that the uric acid level in the urine was increased by seven days of oral gavage with potassium oxonate (250 mg/kg) in rats; however, this status could be rescued by administration with polydatin (25, 50 mg/kg) [
3]. In addition, treatment with liquiritigenin (20 and 40 mg/kg) has been reported to have a potential role in improving the higher urine uric acid level in PO (250 mg/kg)-induced hyperuricemic rats [
14]. In our study, the concentration of uric acid in the urine was increased in the hyperuricemia group. However, the higher urine uric acid level was observed in the high-dose fucoxanthin group and the combination group. The high-dose fucoxanthin group and the combination group also showed a significant increase in the fractional excretion of uric acid (FEUA) compared with the hyperuricemia group, suggesting that a high-dose of fucoxanthin alone or a combination of fucoidan and fucoxanthin treatment could promote the uric acid excretion from the body to the urine. It has been shown that the PO (250 mg/kg)-induced hyperuricemia group had a lower creatinine clearance than the control group. After treatment with liquiritigenin (20, 40 mg/kg), the creatinine clearance was increased compared with that in the hyperuricemia group [
14]. In the present study, the creatinine clearance in the hyperuricemia group was not altered. There was no significant difference between the hyperuricemia group and any intervention group, except for the positive control group. These results cause us to speculate that the difference between the hyperuricemia group and the positive control group is due to the side effects of allopurinol; however, the acute induction model was not long enough to cause renal damage.
A previous study has reported that the hepatic xanthine oxidase activity did not cause any alteration in the PO (250 mg/kg)- and HX (300 mg/kg)-induced hyperuricemic rat model [
11]. In addition, there was no significant difference in the positive control group, which was given a dose of 3.5 mg/kg allopurinol, compared with the hyperuricemia group [
11]. However, according to our results, the PO (300 mg/kg)- and HX (300 mg/kg)-induced hyperuricemic rats had a significantly increased xanthine oxidase activity in the liver, and this stimulatory effect was rescued by intervention with fucoxanthin alone or combined with fucoxanthin and fucoidan. Moreover, the combination group had the best efficiency of xanthine oxidase inhibition.
Previous studies have shown that the expression levels of the two transporters, GLUT9 and URAT1, in the kidney were significantly increased in the PO (300 mg/kg)-induced hyperuricemia group, but the higher GLUT9 and URAT1 protein levels in the hyperuricemia group were reduced by intervention with luteolin (20, 40, 100 mg/kg) [
20]. In the hyperuricemia mouse model, the hyperuricemia-induced high renal GLUT9 protein expression was reduced by treatment with nuciferin. In addition, the expression of the ABCG2 and OAT1 transporter proteins in the hyperuricemia group was significantly lower than that of the control group, whereas treatment of hyperuricemia mice with nuciferin significantly increased the expression of ABCG2 and OAT1 proteins [
21]. In the present study, the results showed that the expression levels of GLUT9 and URAT1 were significantly increased in the hyperuricemia group, whereas the expression levels of ABCG2 and OAT1 were significantly decreased. Among the intervention groups, those receiving fucoxanthin alone and a combination of fucoxanthin and fucoidan had a significantly reduced expression level of GLUT9 and URAT1 proteins. The protein expression of ABCG2 was significantly increased in the low-dose fucoxanthin group and the combination group compared with the hyperuricemia group. Finally, the protein expression of OAT1 was only significantly increased in the combination group compared with the hyperuricemia group. These results suggested that only the combination group (fucoidan and low dose fucoxanthin) significantly regulated all uric acid-related transporters in the kidney compared with the hyperuricemia group. The mechanism by which fucoxanthin and fucoidan modulate hyperuricemia is proposed in
Figure 7.
It has been reported that hyperuricemia patients with a higher level of uric acid in the serum are exposed to a higher risk of cardiovascular disease [
22]. Uric acid has been reported to inhibit nitric oxide (NO) production and induce inflammation cytokine interleukin (IL)-6, IL-8, and tumor necrosis factor (TNF)-α release from human umbilical vein endothelial cells, which are associated with endothelium injury and vascular dysfunction [
23]. In addition, uric acid can pass through the blood–brain barrier and induce hypothalamic inflammation through activation of the NFκB-mediated inflammation pathway [
24]. However, fucoidan and fucoxanthin have been reported to have a potential role in improving inflammation via suppressing inflammatory cytokine production [
25]. Treatment with fucoidan has also been reported to improve renal tubulointerstitial fibrosis in a chronic kidney disease mouse model via reducing the β-catenin and TGF-β1 expression [
26]. According to our findings in this study, we propose that a combined treatment with fucoidan and fucoxanthin reducing the uric acid level may improve the inflammatory signaling in the hyperuricemic rat.
4. Materials and Methods
4.1. Materials
Hi-Q oligo-fucoidans (Fc) and high-stability fucoxanthin (HS Fucoxanthin, HSFUCO) (Fx) were derived from
Laminaria japonica and obtained from Hi-Q Marine Biotech International Ltd. (New Taipei City, Taiwan) [
27]. Oxonic acid (potassium salt), hypoxanthine, and the xanthine oxidase fluorometric assay kit were purchased from Cayman Chemical (Ann Arbor, MI, USA). Allopurinol was purchased from Sigma-Aldrich (St. Louis, MO, USA). Rabbit anti-ABCG2 and anti-OAT1 antibodies were obtained from Abcam (Cambridge, MA, USA). Rabbit anti-GLUT9 antibody was obtained from Millipore (Billerica, MA, USA), and rabbit anti-URAT1 antibody was obtained from Proteintech (Rosemont, IL, USA).
4.2. Animals
For this study, 35 male Sprague Dawley (SD) rats (9 to 10 weeks old, 400 ± 20 g) were purchased from BioLASCO Taiwan Co., Ltd. (Yilan, Taiwan). The experimental animals were quarantined and allowed to acclimate for a week before the experiment. The room temperature was maintained at 21 ± 2 °C, and the relative humidity was kept at 40–60%. Two or three animals were housed per cage under standard laboratory conditions, with a 12/12 h light/dark cycle. During the whole experimental period, food and water were provided ad libitum. All the experiments involving animals were approved by the Institutional Animal Care and Use Committee (IACUC), with approval number LAC-2018-0085 (Approval day: 12th June 2018), Taipei Medical University, Taiwan. The experiment complied with the Guide for the Care and Use of Laboratory Animals published by the National Research Council (revised 2011) and the Guide for the Care and Use of Laboratory Animals—Taiwanese Edition (1996).
4.3. Hyperuricemic (HUA) Rats and Drug Administration
Potassium oxonate (PO), an uricase inhibitor, was used to induce hyperuricemia. Hypoxanthine (HX) is a precursor of uric acid, and allopurinol, a xanthine oxidase inhibitor, is a clinical medication for hyperuricemia. In this study, PO (300 mg/kg) was mixed with 0.5% (w/v) sodium carboxymethyl cellulose solution (CMC, Sigma-Aldrich, St Louis, MO, USA) and HX (300 mg/kg) were dissolved in distilled water. First, nine rats were used to induce the acute hyperuricemia (HUA) rat model by oral gavage of PO and HX. Blood samples were collected through the tail veil in a time-course manner, and then serum uric acid was measured. According to this experiment, treatment of PO/HX for 4 h was selected to design the next experiment.
After a one-week recovery, these nine rats and the other twenty-six rats (total of 35 rats) were randomly divided into seven groups (n = 5 per group): (1) control group (C) rats were treated with 0.5% CMC; (2) vehicle group (V)rats were treated with 0.5% CMC; (3) low-dose fucoxanthin group (LFx) rats were treated with 150 mg/kg of fucoxanthin; (4) high-dose fucoxanthin group (HFx) rats were treated with 300 mg/kg of fucoxanthin; (5) fucoidan group (Fc) rats were treated with 150 mg/kg of fucoidan; (6) combination of low-dose fucoxanthin and fucoidan group (Fxc) rats were co-treated with 150 mg/kg of fucoxanthin and 150 mg/kg of fucoidan; and (7) positive control group (P) rats were treated with 20 mg/kg of allopurinol. These interventions were performed by oral gavage once daily for 21 days.
One hour after the intervention on the 21st day, the hyperuricemia (HUA) model was induced by oral gavage of PO and HX, and then the rats were housed in metabolic cages and the urine was collected for 24 h. The urine sample was centrifuged (3000×
g, 4 °C) for 10 min to obtain urine free of particulate contaminants. The volume of urine was measured using a graduated cylinder. On the next day, a process was performed similar to the one followed above on the 21st day; the hyperuricemia model was induced again (
Figure 8). After 4 h, all animals were sacrificed using a Zoletil (20 mg/kg) + rompun (5 mg/kg) mixed solution (
v/
v = 1:1) anesthesia.
4.4. Blood, Urine, and Tissue Sample Collection
After the rats were sacrificed, blood samples were collected by cardiac puncture and allowed to clot for at least 1 h at room temperature and then centrifuged (3000× g, 4 °C) for 10 min, after which the serum was collected. On the day of collection, the serum and urine samples from the metabolic cage collection were delivered to Taipei Medical University Hospital (Taipei, Taiwan) for biochemical examination. Kidneys, livers, hearts, spleens, and testes were quickly excised, weighed, and immediately stored at −80 °C for further analysis.
4.5. Determination of Uric Acid, BUN, and Creatinine Levels in Serum
Twenty-four hours before the sacrifice, all animals were placed in metabolic cages to collect fasting urine. After the urine volume was measured using a graduated cylinder (Sigma-Aldrich, St. Louis, MO, USA), the serum and urine samples were delivered to the Taipei University of Medical Sciences. The uric acid concentration, blood urea nitrogen, and creatinine in the serum and urine were determined by using a chemical analyzer (Roche Diagnostics, Rotkreuz, Switzerland). After the biochemical data were collected, the fractional excretion of uric acid (FEUA) and creatinine clearance rate (CCr) were calculated using the following equations:
4.6. Xanthine Oxidase Assay
After the livers were homogenized and centrifuged, the supernatant was collected. The xanthine oxidase activities were detected using a xanthine oxidase fluorometric assay kit (Cayman Chemical, Ann Arbor, MI, USA). The procedures were followed according to the manufacturer’s instructions.
4.7. Western Blot Analysis
Tissue protein levels were analyzed by Western blot as described previously [
27,
28]. After kidney samples were homogenized at 4 °C, they were separated by protein electrophoresis and Western blot to analyze the expression of kidney-related transporter proteins. Lysis buffer (RIPA/protein inhibitor = 19:1) was added to the kidney homogenization and further homogenized by an organization homogenizer (Qiagen, Chatsworth, CA, USA) (1/20 Hz, 30 s/time). After centrifuging the sample for 30 min at 12,000 rpm and 4 °C, the supernatant was collected, and the protein sample was quantified using a BCA (bicinchoninic acid) assay. A volume equivalent to 80 μg of the sample protein was taken and mixed with 1/5 of the total volume of sample dye (4×). The mixture was left to react at 100 °C for 5 min to facilitate protein denaturation. Then, the protein extraction was added to a 10% SDS gel for protein electrophoresis. When the proteins were adequately separated, the protein was transferred to 0.45 μm PVDF membrane, which was then blocked with blocking buffer for 1 h and washed with TBST three times (10 min/wash). After washing the membrane, the membrane was incubated with primary antibodies at 4 °C overnight; then, the membrane was washed with TBST three times (10 min/wash). Subsequently, the membranes were incubated with anti-rabbit or anti-mouse IgG. The uric acid-related transporter proteins were detected by a chemiluminescence detection system according to the manufacturer’s instructions (ECL, T-Pro Biotechnology, New Taipei City, Taiwan).
4.8. Statistical Analysis
All data were expressed as the mean ± standard error of the mean (SEM). The effect of PO/HX on the induction of the hyperuricemia model was analyzed by paired t-test. The effects of fucoidan and fucoxanthin on biochemical composition and renal function were analyzed by one-way analysis of variance (ANOVA) and unpaired t-test to determine the level of significance. The results of Western blotting were analyzed using the Mann–Whitney test. A value of p < 0.05 was considered statistically significant. Figures were obtained using the Statistical Analysis System (GraphPad Prism 6, GraphPad Software, Inc., San Diego, CA, USA).