1. Introduction
The Severe Acute Respiratory Syndrome CoronaVirus 2 (SARS-CoV-2) pneumonia—also known as COronaVIrus Disease 19 (COVID-19)—allegedly broke out in a wet market of the city of Wuhan, the capital city of the Hubei Province, in Central China (30.60° N–114.05° E), where also the Wuhan Institute of Virology is located. The first case of hospital admission was reported on 12 December 2019 [
1]. Since January 2020 the pandemic rapidly spread throughout the whole province of Hubei, in other regions of China and, further, began to spread all over the world. The COVID-19 pandemic is being monitored by the World Health Organization (WHO). (Web Page:
https://www.who.int/emergencies/diseases/novel-coronavirus-2019, accessed on 15 April 2020. Coronavirus disease (COVID-19) Pandemic).
The high lethality rate of this virus requires the development of epidemic control strategies such as lock-down of the infected region and others [
2], which, however, in time can negatively affect the economy of a society. Thus, it is a priority to forecast how the COVID-19 pandemic could geographically propagate and affect society for optimizing these strategies.
As of the date—15 April 2020—there are about 2 million people confirmed infected worldwide with about 130 thousand deaths versus only about 500,000 people recovered. China, where the infection first broke out in December 2019, officially had about 82,295 cases infected with 3342 total deaths, of which 3222 came from the province of Hubei alone. The Chinese authorities have declared that there have been very few cases of new infections since the first weeks of March and claim that since then in China the pandemic is under control (cf. Report of the WHO-China Joint Mission on Coronavirus Disease 2019. (Source:
https://www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf, accessed on 15 April 2020.) However, on 17 April, China acknowledged significant reporting errors regarding the total deaths, which were corrected from 3342 to 4632.
However, at the beginning of February, the pandemic began to show up outside of China spreading all over the world. South Korea was the first country severely affected by the pandemic (10,591 cases confirmed and 225 deaths), where since late March the pandemic has appeared mostly under control although in April the rate increased slightly. Later, many other countries were affected such as Iran, Turkey, several European countries (mostly Italy, Spain, France, Germany and the United Kingdom). In Europe, the situation is monitored also by the European Centre for Disease Prevention and Control. (Web page:
https://www.ecdc.europa.eu/en/geographical-distribution-2019-ncov-cases, accessed on 15 April 2020.) Since the 15th of March the COVID-19 pandemic has been rapidly spreading in the United States of America, where, as of April 15, there have been more than 600,000 cases with more than 26,000 deaths.
Italy has been one of the countries most severely affected by the COVID-19 induced pneumonia. (The situation in Italy:
http://www.salute.gov.it/portale/nuovocoronavirus/homeNuovoCoronavirus.jsp?lingua=english, accessed on 15 April 2020.) The first three cases were identified on 20 February and, on 15 April there were more than 162 thousand confirmed infected people with more than 21 thousand deaths and only 38 thousand recoveries. The most affected Italian regions were the northern ones, those located in the Po Valley: Lombardia, 62,153 cases and 11,377 deaths; Emilia Romagna, 21,029 cases and 2788 deaths; Piemonte, 18,229 cases with 2015 deaths; Veneto, 14,624 cases and 940 deaths. (Source:
http://www.salute.gov.it/imgs/C_17_notizie_4482_0_file.pdf, accessed on 15 April 2020.) In Lombardia, the most affected provinces were Milan (14,600 cases), Bergamo (10,472 cases) and Brescia (11,187). (Source:
http://www.salute.gov.it/imgs/C_17_notizie_4482_1_file.pdf, accessed on 15 April 2020.) See
Figure 3. (COVID-19 Italy situation:
http://opendatadpc.maps.arcgis.com/apps/opsdashboard/index.html#/b0c68bce2cce478eaac82fe38d4138b1, accessed on 15 April 2020.)
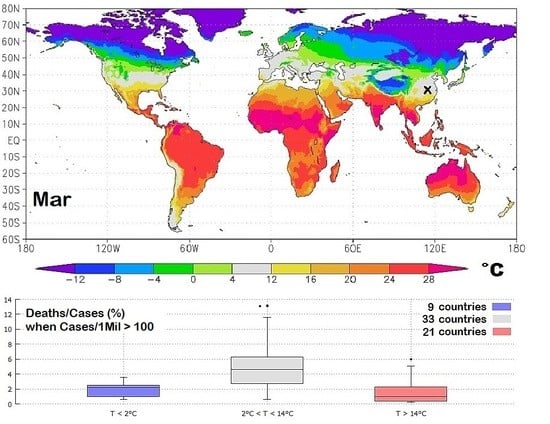
Although the propagation of a pandemic and its health severity may have several causes including people’s network contacts, greater mobility, more concentrated demography, population age and air pollution as it usually happens in large and economically developed zones,
Figure 2 suggests that the spread of the COVID-19 pandemic could also have a main geographical climatic preference. In fact, the pandemic appears to have spread quite fast in moderately cold places where the daily average temperature may have been roughly between 0 °C and 16 °C. On the other hand, up to 15 April, countries with warm climates (e.g., India, Central America, South America, Southern Asia, Africa and Oceania), as well as very cold countries (e.g., Canada, Russia, North-Eastern Europe) appear to have been less affected. It is also noticeable that even when the number of cases is relatively large relative to the population, the number of deaths is usually lower in warm countries, as shown in
Figure 2C. Thus, it is reasonable to ask whether geographical regions within a specific climatic/weather zone could be more vulnerable to this epidemic. Indeed, several studies have established that influenza virus transmission and virulence depend also on meteorological conditions such as temperature, relative humidity and wind speed; besides, in the Northern Hemisphere, influenza is more widely spread during the winter seasons [
3,
4,
5].
Influenza rates are normally seasonal [
6] and, usually, these infections nearly disappear when the weather gets warm. Similar behavior has been observed for other SARS coronaviruses [
7,
8,
9,
10] that belong to the same Coronaviridae family of SARS-CoV-2 [
11]. The finding has always been that these viruses spread mostly within given ranges of meteorological conditions. For example, Yuan et al. [
12] determined that the SARS virus identified in November 2002 in Guangdong Province, China, presents a peak spread at a mean temperature of 16.9 °C (95% CI, 10.7 °C to 23.1 °C), with a mean relative humidity of 52.2% (95% CI, 33.0% to 71.4%) and wind speed of 2.8 m/s (95% CI, 2.0 to 3.6 m/s). Gaunt et al. [
13] found that three coronaviruses showed “marked winter seasonality” and that they seemed to cause infections mainly between December and April. In a preliminary analysis, Bukhari and Jameel [
14] noted that the novel COVID-19 pandemic has affected more seriously countries within a temperature range of 3 °C to 17 °C with absolute humidity between 3 g/m
3 and 9 g/m
3. Thus, also for the COVID-19 it has been proposed that a dry, moderate cold environment could be the most favorable state for the spreading of this virus [
15].
The seasonal influence on the spread or slowdown of a pandemic induced by aerially transmitted viruses can have several biological, physical, solar-light mechanisms that involve both the virus survival and transmission in the air and the susceptibility of the host immune system [
16]. Some of these results came from laboratory-experimental studies on how viral etiology and host susceptibility vary under different environmental conditions, while other findings are from epidemiological studies relating large-scale patterns to various climate signals and atmospheric conditions. In any case, even if viruses could survive at relatively high temperatures in lab experiments (indeed, they live in a human body at 37 °C or more) their ability to propagate from person to person and to overcome their immune system may strongly depend on seasonal weather conditions.
In this paper, geographical data describing the COVID-19 diffusion and lethality are correlated against weather-climatic conditions of various countries, their median population age and air pollution levels to determine the main possible factors affecting the pandemic. The study starts with a detailed comparison of the weather conditions from January to March 2020 between Wuhan and the Italian provinces of Milan, Brescia and Bergamo that were the first most affected regions. The striking similarity between the weather conditions of these two regions leads us to reason that there could be an optimal weather condition (dry and moderate cold weather) that could favor the spreading of the COVID-19 epidemic. This hypothesis is also supported by physical considerations related to the transmission in the air of viruses through respiratory droplets, as explained in the discussion section. The testing is then completed by analyzing the situation in the United States of America and finally of the entire world. Finally, the median population age of the countries and their air pollution levels are analyzed to evaluate their possible contribution to the pandemic. Based on this reasoning and the analysis results, it is suggested that weather-climatic conditions are the main factor regulating the development of the pandemic. Consequently, a set of optimized monthly isotherm world maps from January to December 2020 are proposed to forecast its course and timeline evolution by identifying the geographical regions that are likely to experience similar weather conditions as in Wuhan and Milan during the high peak of the COVID-19 infection. For each country and region, weather predictions could later be further convoluted with the median population age of the specific place since the COVID-19 affects mostly the elderly. The online
supplementary files provide the same maps as Google-Earth-Pro interactive files and the full data files. (
Appendix A).
5. Discussion and Conclusions
Respiratory virus infection rate is usually seasonal [
7,
8,
9,
10]. This applies also to the coronaviridae family of COVID-19 [
11]. In general, there are likely several biological, physical and sunlight mechanisms that can seasonally influence the survival and transmission of viruses in the air, as well as the susceptibility of the host immune system [
16]. The weather conditions that facilitate this type of diseases include moderate cold and dry weather, high pressure, low-speed wind and modest rain, as it happened from January to March 2020 both in Wuhan and in Northern Italy. Similar weather conditions occurred in other countries where the pandemic has been significant, for example in Western Europe and the United States of America.
The COVID-19 infection primary transmission route from person to person is through contact with respiratory water droplets exhaled by infected persons. Contacts with surfaces contaminated by secretions or oral nose pharyngeal emissions could be a secondary transmission route. In fact, a person can also catch the virus if he or she touches a surface or object that has the virus on it and then touches his or her mouth, nose, or eyes.
Exhaled water droplets floating in the air could be as small as 0.5 to 10 micron and carry around coronaviruses, which have a size of about 120 nm. Such droplets are generated when, for example, people blow their nose, cough or sneeze, or just breathe. The warm and humid lungs add moisture to the breath. Thus, when people exhale on a cold day, the water vapor contained in their breath partially condenses as the air cools down. Therefore, when the air temperature is low, but not freezing, and the relative humidity is neither too low nor too high, as it happens in the winter in the most affected regions, water-based small droplets, which could carry viruses, more easily form and remain floating in the air for a longer time because they do not evaporate easily nor fall fast on the ground by further capturing additional water vapor. Thus, viruses could survive floating in the air protected by a small respiratory droplet long enough to infect somebody else who could pass by and then breathe in those droplets.
High temperature and dry air prevent the formation of such small condensation droplets or make them evaporate fast exposing the virus directly to the air which should induce a rapid destruction of its capsid. Larger droplets emitted with the cough fall rapidly to the ground and evaporate fast if the air is warm or very dry inducing again a rapid death of the virus. Freezing weather favors the formation of large droplets that fall fast on the ground. Rain facilitates the removal of virus-carrying droplets and virions because it captures them in the air and makes them fall on the ground. High atmospheric relative humidity would also facilitate the fall of such droplets by preventing them to become sufficiently small to float in the air for a time long enough to reach and, therefore, contaminate far distances. High atmospheric pressure reduces the wind speed, and virus-carrying droplet density could increase in the urban area. Northern Hemisphere winters also have fewer hours of sunlight and UV exposure that have a sterilizing effect [
23]. In addition, cold weather usually increases the susceptibility of people to virus attacks, whereas summer warmer temperatures, more abundant UVB sunlight, and vitamin-rich food strengthen the immune system.
Cold weather also forces people to gather more likely in closed warm environments. Here it is easier to get infected because of poorer air exchange. In fact, in indoor environments—such as apartments, offices, shops, schools, restaurants, cruise ships, etc.—although the water of the infected droplets could evaporate faster exposing the virus to an inhospitable environment, the air concentration of floating virions, which could still remain active for a while, could increase so much to easily infect other people [
22]. Indoor environments are also not protected nor sterilized by UV solar radiation: a fact that prolongs the life of the virus in such environments.
Thus, there are numerous direct and indirect mechanisms supporting the hypothesis that seasonal weather conditions affect the diffusion of SARS-CoV-2, as it has been observed for many other respiratory viral infections.
In any case, the virus by itself can survive also high temperatures, as it lives within human bodies and, therefore, people could get infected also in warm places, as it has been observed worldwide. This evidence, however, does not contradict the fact that the COVID-19 pandemic has been worst and developed more rapidly in specific countries which, during winter 2020, shared a common weather condition. The few observed anomalous cases could have simple explanations.
For example, as of the date (15 April 2020), the warm State of Louisiana in the United States of America counted 237 deaths per million people and was the fourth most affected state of the USA. However, this apparent anomaly was likely due to its famous carnival festivals that attracted into the city historic center 1.4 million people from all around the world, making the city the main infection hub. Similarly, the coronavirus outbreak in the city of Daegu in South Korea was induced by a very large service gathering by the Shincheonji religious group in a closed space. (Web Page:
https://edition.cnn.com/2020/02/26/asia/shincheonji-south-korea-hnk-intl/index.html, accessed on 15 April 2020.)
We also checked whether air pollution could have been a relevant co-factor for the SARS-CoV-2 lethality in some countries. Our analysis suggests a poor correlation because heavily polluted countries such as India and the South-Eastern Asian countries (including also Southern China, Hong Kong, and Taiwan) have been modestly affected by the pandemic. For example, as of the date (15 April 2020), despite its close connections with China, Hong Kong (7,392,000 people by 2017) had about one thousand cases with only four deaths. Note that the COVID-19 started earlier in Hong Kong than in Italy because on 02/15/2020 in Hong Kong there were 56 cases while in Italy there were 3 cases. (Source:
https://www.worldometers.info/coronavirus/, accessed on 15 April 2020.) The warm and dry Qatar, Bahrein and the United Arab Emirates (UAE) with their crowded and very polluted capitals (Doha, Manama and Dubai: Source:
https://www.thenational.ae/uae/world-environment-day-middle-eastern-cities-choked-by-air-pollution-1.870540, accessed on 15 April 2020) had a number of COVID-19 cases—1288, 982 and 542 cases/1Mil, respectively—probably due to their international connections, but only 2, 4 and 3 deaths per million people, respectively. This is a mortality rate per infected people nearly 50 times lower than that observed in Italy and other Western European countries. By contrast, the small Republic of San Marino located on hills in Italy between the regions of Emilia-Romagna and Marche was much more affected by the COVID-19 pandemic than the nearby cities despite its cleaner air. This could have happened because San Marino is a few degree colder than the nearby warm cities located in the valley and on the coast.
Indeed, as of the date (15 April 2020), on 151 countries of the world with a population larger than one million people, among the 80 countries that had at least 50 cases/1Mil, those with a mortality rate larger than 10% were seven and from Western Europe: Belgium, Italy, and the United Kingdom, 13%; France, 12%; Netherlands, 11%; Spain and Sweden, 10%. On the contrary, the last seven countries were all from warm zones: the United Arab Emirates (UAE), 0.6%; Oman, Bahrain, Hong Kong, 0.4%; Singapore 0.3%; Kuwait, 0.2%; and Qatar, 0.15%. Note that the latter seven countries are internationally well interconnected, with high densely populated cities and medical technology not superior to that of the European countries. Thus, the different lethality rates, by a factor of 20 and above, observed between the two groups are likely due to their very different winter climatic conditions, with the European countries significantly colder than the latter.
Among the other 72 countries with less than 50 cases per million people, none is from Europe. There are 43 warm African countries except for the colder Marocco (Cases/1Mil = 55; Deaths/1Mil = 3, and Deaths/Cases = 5.5%) and Tunisia (Cases/1Mil = 66; Deaths/1Mil = 3, and Deaths/Cases = 4.5%), with the addition of the Mauritius islands (Cases/1Mil = 255, Deaths/1Mil = 7, and Deaths/Cases = 2.7%; note that these islands are a popular touristic place which could explain the relatively high infection rate). Large but warm countries such as Indonesia and India had just 19 and 9 cases per million people, respectively.
Thus, the relatively low COVID-19 diffusion and mortality rates, and the low ratio between mortality and infection rates observed in warm countries (see
Figure 11) relative to the high mortality levels of colder countries such as those in Europe and the United States of America indicate that weather, not air pollution is the main factor for the diffusion and lethality of the COVID-19 pandemic. A correlation between the number of COVID-19 cases and higher polluted areas, such as large cities, could be accidental, and simply due to the higher population density of these places where it happens that more air pollution is also produced. In general, air pollution is not expected to be a major carrier of the coronavirus since the virus is mostly diffused in the air by human breath. The question about whether people living habitually in air polluted areas could be more sensitive to the infection because of a weakened immune system is a different topic, but still, pollution appears to only play a secondary role relative to weather conditions.
Finally, we checked a possible influence on the COVID-19 pandemic of the median population age of the place. The analysis was carried by comparing the regions of Italy, the United States of America, and the countries of the world. We did find a correlation with the COVID-19 but, by considering all local and global evidences, it appears weak relative to the one observed with the weather-climatic patterns. Thus, we conclude that places with a higher median population age could be disadvantaged, but still, the severity of the pandemic is driven mostly by the weather-climatic conditions that regulate both the diffusion of the virus through the air and the susceptibility of the immune system of the people to viral attacks. An additional detailed analysis may need to compare the weather records using age-standardized COVID-19 records divided by age categories, but this operation requires additional detailed data for each countries and regions. Whether this additional analysis could improve the reliability of the results herein presented is left to further research.
With regards to the mortality rates, a role is also played by the different quality of the health system of each country and region, but this analysis goes beyond the purpose of this work. For example, there have been reports of a large number of infections occurred within elderly care housing centers and hospitals, which had to and should be prevented. E.g., Wang et al. [
24] found that in a single-center case series of 138 hospitalized patients with confirmed NCIP in Wuhan, China, presumed hospital-related transmission of 2019-nCoV was suspected in 41% of patients, 26% of patients received ICU care and mortality was 4.3%.
Based on the above considerations, this work explored the possible link between COVID-19 pandemic and weather conditions. We showed that the region of Wuhan in the Hubei Province, in Central China, and the Italian provinces of Milan, Brescia and Bergamo—which to date have been the most affected by the COVID-19 pandemic—presented a striking similarity in weather conditions between January and March. In particular, the weather condition in Wuhan in late January and February—when the COVID-19 infection affected that region most severely—was nearly identical to the weather conditions between February and March experienced in the Italian northern provinces. The same correlation was confirmed by a detailed analysis of the relation between weather conditions and the pandemic situation in the United States of America. These findings suggest that weather temperatures between 4 °C and 12 °C together with low humidity values between 60% and 80% and low-speed winds (about 10 km/h) could be those that mostly favor the spread of COVID-19 and/or aggravate the susceptibility of the population to its secondary pneumonia.
We used this result to create a specific isotherm world map for each month from January to December to highlight the timing and the position of the world regions that could be most affected by the pandemic in the upcoming months. To date—15 April 2020—the model appears to have well described the pandemic evolution as, for example, it has well predicted the pandemic strong development from February to the end of March in Iran, Italy, Spain, France, Germany, the United Kingdom and the United States of America, in order of time. Thus, it is possible that in the absence of adequate prevention policies, as the weather gets warm, the pandemic is likely to move following the seasonal temperature cycle and could migrate toward northern regions of the Northern Hemisphere while weakening in the southern ones such as China and Italy. The Southern Hemisphere appears to be more protected because most of its land, except for a few regions, is always sufficiently warm throughout the year. In addition, also the relatively low median population age of several warm countries, such as the African ones, could contribute to mitigating the effect of the pandemic in those countries.
Furthermore, the weather model suggests that in the Northern Hemisphere there may be a possible second wave of infections in the autumn following the return of the cold season. In general, the pandemic could return to the middle latitude regions (roughly 30°–60° N and 30°–60° S) with a 6-month cycle and in the other regions with an annual cycle. Although the transmission of COVID-19 should go down as weather temperature goes up, the virus may not disappear completely. The infection rate could simply slow down, as suggested by the evidence that people get infected also in warm regions, although in these places the percentage of deaths per million people appears to be significantly lower than in the cold weather regions (
Figure 2). Thus, although the optimized isotherm maps proposed in the present work could be useful to optimize the timing of the required COVID-19 epidemic control policies that each country needs to implement, people and governments should be warned against lowering their guard.