Dengue Surveillance System in Brazil: A Qualitative Study in the Federal District
Abstract
:1. Introduction
1.1. Dengue, Dengue Surveillance, and Relevance in Global Public Health
1.2. Dengue Surveillance in Brazil
1.3. Aim of the Study
2. Materials and Methods
3. Results
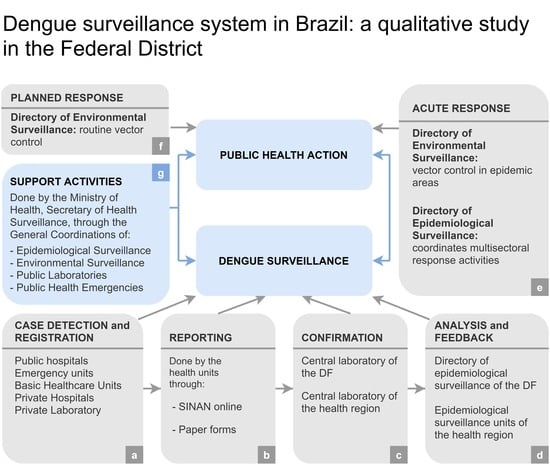
3.1. General Overview of Dengue Surveillance in the DF
3.2. Case Detection
A4: Good sensitivity, completeness, is what we perceive in practice. Since 2014, the circulation of other viruses in our country (Zika and Chikungunja) has hindered this sensitivity […]. But in terms of capturing information on what we thought dengue was, by 2014, sensitivity was good.
C: we can’t get those cases who cannot get medical attention in one moment and they end up not seeking again… Because they know all the recommendations for dengue, resting, hydration, they prefer to go back and self-treat at home.
3.3. Registration and Reporting of the Cases
A4: ...it is an easy-to-operate system, has a certain stability, so you can download databases, do analysis easily. As it’s online, allows the managers of the 3 federative entities to make quick decisions.
A1: (a part is) underreported because the professional doesn’t really notify: it makes the diagnosis, but he does not incorporate the habit of taking a form and informing the surveillance system […] The professional finds it difficult to notify as well [...]. Another issue is that the health service really doesn’t understand the importance of notifying.
A5: ...and has a lower than expected number of completeness of these important variables, […] because it is so complex, because the fields in the notification form are very large and it ends up being complex to fill. This individual is notified and then it takes time for the investigation…
3.3.1. Public Hospitals and Emergency Care Units
A1: Inside hospitals, there are Epidemiological Surveillance Units that work with an active surveillance type. [...] So, as a nurse in these centers, I will go through the pediatric emergency, the clinical emergency… […] and I go looking for cases that were suspected for dengue…
3.3.2. Basic Healthcare Units (Unidades Básicas de Saúde (UBS))
C: ...and when the case is more serious and he goes to the hospital, theoretically he has already been treated and notified in a UBS, but in reality in these places, especially in the epidemic period, there is a lot of work, so often the professionals don’t have time to fill in all those forms with so many items and the forms accumulate there... often when they go to notify […] it’s been a week or longer.
B1: In addition to technological issues, that not all units have a computer [...] we have issues related to the amount of staff that is insufficient. Depending on the volume of cases that arrive at the unit, they can’t do everything, they have to choose: either make the notification, or attend to the patient.
3.3.3. Private Healthcare Units
A1: Public and private should come closer. It should be understood as a single health. The private works a lot with a profit logic. So, for the private sector to put a nurse to do only… not only, but in addition […] she will also notify… if it’s costly for the private sector…. it is of no importance to them, because they don’t see the results either.
B1: This is a major concern for us, because the population that seeks the private sector […] has a different socioeconomic profile, and this may compromise the implementation of responses, the adoption of measures... it is in certain places that the government cannot see the problem…
3.4. Laboratory Testing and Case Confirmation
F: We have very sensitive case definitions, because it favors the entry of many patients in the system
D: The surveillance model needs to be adjusted in the epidemic and inter-epidemic phase. From a laboratory point of view, we are really compromised when we do not define it and use the same model in these two different scenarios. So, you end up overloading the laboratory at certain times [...] we have limited human resources, [...] and we often overburden the surveillance service as much as the laboratory when you do not have this very clear definition regarding the models.
3.5. Data Analysis and Feedback
B1: Although we have minimal human costs, what we see is the knowledge of each professional.
F: Piles of forms accumulate and sometimes there is one person to type hundreds... and if the notification is delayed, the vector control action later, and everything else, is also delayed.
3.6. Role of the Federal Government and Support Activities
3.7. Public Health Action
B2: Inside the SDCC, is also important to highlight all the communication work that is done. Because, as there are several undersecretaries, each secretariat has its communication core […]. Within the epidemiological surveillance only, we would not have this strength. And what is important in this context is the integration…
E: there is a high discontinuity of professionals in the field. So, you capacitate, but you have no guarantee that these professional will remain […]. When there is a management change, also a big part of the agents changes.
A6: And dengue in Brazil is very targeted, because it has much... it affects politically [...] When there was an epidemic, the population complained, complained, and the major ordered the ULV, a machine that goes in the car and fogs Ultra Low Volume. But [...] for dengue control program, the ULV is recommended only in extreme cases, and in many places we saw that ULV use was triggered by policy. To say that they were doing something.
3.8. Vector Surveillance
H2: First, I think we would need an exact number of people, a right number to cover the entire region, and to work better on environmental education.
H1: Residents always accumulate a lot of water from day to day, 80% of the breeding sites in the DF are inside the homes.
H2: I think if we worked in community, schools, I think we would cover a larger number, because we would even need fewer people to work with.
A2: We have different laboratory and entomological systems, and they don’t talk. So, we have to take, almost manually, the base of these two systems and integrate. This, I think, is a very bad factor.
3.9. Active Surveillance
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A
| Outline of the Semi-Structured Interviews |
|---|
| How does the dengue surveillance system work? What are the existing national policies on dengue surveillance? How does data collection for dengue surveillance work? |
| In addition to passive surveillance, are there forms of active dengue surveillance? If so, what types of active surveillance are there and how do they work? |
| How does laboratory surveillance work? |
| How are data integrated at the municipal, state, and federal levels? |
| How are epidemiological and environmental data integrated? Are there any systems in place to integrate other types of data (for example: socioeconomic data, urban environment, weather)? |
| What is the role of the private health system in dengue surveillance? |
| What are the response activities based on dengue surveillance? |
| What are the strengths and weaknesses of the dengue surveillance system? |
| What are the reasons for the low sensitivity of the surveillance system? |
| Do you have any suggestions for improving the dengue surveillance system? |
| English Translation | Original Name | Abbreviation |
|---|---|---|
| national health system | Sistema Único de Saúde | SUS |
| Federal District | Distrito Federal | DF |
| Secretary of health surveillance | Secretária de Vigilância á Saúde | SVS |
| General Coordination of Arbovirosis Surveillance | Coordinação Geral de Vigilância das Arboviroses | CGARB |
| General Coordination of Public Laboratories | Coordinação Geral de Laboratórios em Saúde Pública | CGLAB |
| General Coordination of Public Health Emergencies | Coordinação Geral de Emergência em Saúde Pública | CGEMPS |
| General Coordination of Environmental Surveillance | Coordinação Geral de Vigilância em Saúde Ambiental | CGVAM |
| Central Laboratory of the State | Laboratório Central do Estado | LACEN |
| Undersecretary of Health Surveillance | Subsecretaria de Vigilância á Saude | SVS |
| Directory of Epidemiological Surveillance | Diretoria de Vigilância Epidemiológica | DIVEP |
| Directory of Environmental Surveillance | Diretoria de Vigilância Ambiental | DIVAL |
| Directory of Central Laboratory of Public Health of the DF | Diretoria de Laboratório Central de Saúde Pública do DF | LACEN-DF |
| Regional Superintendencies of Health | Superintendências Regionais de Saúde | SRS |
| Regional Directory of Primary Healthcare | Diretoria Regional de Atenção Primária á Saúde | DIRAPS |
| Unit of Epidemiological Surveillance of the health region | Núcleo De Vigilância Epidemiológica e Imunização | NVEI |
| Emergency care units | Unidades de Pronto Atendimento | UPA |
| Hospital Unit for Epidemiological Surveillance | Núcleo de Vigilância Epidemiólogica | NVE |
| Basic Healthcare Unit | Unidades Básicas de Saúde | UBS |
| Family Health Strategy | Estratégia Saúde da Família | ESF |
| Quick Index Survey for Aedes Aegypti | Levantamento de Índice Rápido para Aedes Aegypti | LIRAa |
| District Committee of Coordination and Control | Sala Distrital permanente de Coordenação e Controle | SDCC |
| Regional management for dengue prevention and control | Gestão do Plano de Prevenção e Controle da Dengue | Geiplan-dengue |
| Unit for social mobilization activities | Núcleo de Mobilização Sociál | NMOBS |
References
- Bhatt, S.; Gething, P.W.; Brady, O.J.; Messina, J.P.; Farlow, A.W.; Moyes, C.L.; Drake, J.M.; Brownstein, J.S.; Hoen, A.G.; Sankoh, O.; et al. The global distribution and burden of dengue. Nature 2013, 496, 504–507. [Google Scholar] [CrossRef]
- Brady, O.J.; Gething, P.W.; Bhatt, S.; Messina, J.P.; Brownstein, J.S.; Hoen, A.G.; Moyes, C.L.; Farlow, A.W.; Scott, T.W.; Hay, S.I. Refining the Global Spatial Limits of Dengue Virus Transmission by Evidence-Based Consensus. PLoS Negl. Trop. Dis. 2012, 6, e1760. [Google Scholar] [CrossRef]
- Böhm, A.W.; Costa, C.D.; Neves, R.G.; Flores, T.R.; Nunes, B.P. Tendência da incidência de dengue no Brasil, 2002–2012. Epidemiol. Ser. Saúde 2016, 25, 725–733. [Google Scholar] [CrossRef] [PubMed]
- Toan, N.T.; Rossi, S.; Prisco, G.; Nante, N.; Viviani, S. Dengue epidemiology in selected endemic countries: Factors influencing expansion factors as estimates of underreporting. Trop. Med. Int. Health 2015, 20, 840–863. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Franklinos, L.H.V.; Jones, K.E.; Redding, D.W.; Abubakar, I. The effect of global change on mosquito-borne disease. Lancet Infect. Dis. 2019, 19, e302–e312. [Google Scholar] [CrossRef]
- WHO. Treatment, Prevention and Control Global Strategy for Dengue Prevention and Control; World Health Organization: Geneve, Switzerland, 2012. [Google Scholar]
- Sarti, E.; L’Azou, M.; Mercado, M.; Kuri, P.; Siqueira Jr, J.B.; Solis, E.; Noriega, F.; Ochiai, R.L. A comparative study on active and passive epidemiological surveillance for dengue in five countries of Latin America. Int. J. Infect. Dis. 2016, 44, 44–49. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kassié, D.; Binot, A.; Peyre, M.; Delabouglise, A.; Hoa, T.T.P.; Roger, F. Geography of Health: Using Territorial Constructions to Better Manage Human and Animal Health. In Living Territories to Transform the World; QUAE: Paris, France, 2017; pp. 91–96. [Google Scholar]
- Modi, A.; Vaishnav, K.; Pandya, R.; Sahu, G.; Naik, A. Urban Dengue Surveillance over Sixteen Years: Integration, Trend Analysis and Participation of Private Medical Sector. J. Commun. Dis. 2018, 50, 52–59. [Google Scholar] [CrossRef]
- Knoema. Brazil Urban Population, 1960–2017; Knoema. 2017. Available online: https://knoema.com/atlas/Brazil/Urban-population (accessed on 10 March 2020).
- Fares, R.C.G.; Souza, K.P.R.; Añez, G.; Rios, M. Epidemiological Scenario of Dengue in Brazil. BioMed Res. Int. 2015, 2015, 321873. [Google Scholar] [CrossRef] [Green Version]
- WHO. National Passive Surveillance; World Health Organization: Geneve, Switzerland, 2014; Available online: https://www.who.int/immunization/monitoring_surveillance/burden/vpd/surveillance_type/passive/en/ (accessed on 10 March 2020).
- Runge-Ranzinger, S.; McCall, P.J.; Kroeger, A.; Horstick, O. Dengue disease surveillance: An updated systematic literature review. Trop. Med. Int. Health 2014, 19, 1116–1160. [Google Scholar] [CrossRef]
- World Health Organisation (WHO), Special Programme for Research and Training in Tropical Diseases (TDR). Technical Handbook for Dengue Surveillance, Dengue Outbreak Prediction/Detection and Outbreak Response [“Model Contingency Plan”]. WHO Libr Cat Data. 2016, pp. 1–92. Available online: http://www.who.int/tdr/news/2016/handbook-dengue-outbreak/en/ (accessed on 10 March 2020).
- Azeredo, E.L.; Dos Santos, F.B.; Barbosa, L.S.; Souza, T.M.; Badolato-Corrêa, J.; Sánchez-Arcila, J.C.; Nunes, P.C.; de-Oliveira-Pinto, L.M.; de Filippis, A.M.; Dal Fabbro, M.; et al. Clinical and Laboratory Profile of Zika and Dengue Infected Patients: Lessons Learned From the Co-circulation of Dengue, Zika and Chikungunya in Brazil. PLoS Curr. 2018, 10. [Google Scholar] [CrossRef]
- Bosch, I.; De Puig, H.; Hiley, M.; Carré-Camps, M.; Perdomo-Celis, F.; Narváez, C.F.; Salgado, D.M.; Senthoor, D.; O’Grady, M.; Phillips, E.; et al. Rapid antigen tests for dengue virus serotypes and Zika virus in patient serum. Sci. Transl. Med. 2017, 9, eaan1589. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Teoh, B.T.; Sam, S.S.; Tan, K.K.; Johari, J.; Abd-Jamil, J.; Hooi, P.S.; AbuBakar, S. The Use of NS1 Rapid Diagnostic Test and qRT-PCR to Complement IgM ELISA for Improved Dengue Diagnosis from Single Specimen. Sci. Rep. 2016, 6, 27663. [Google Scholar] [CrossRef] [PubMed]
- Hassan, S.; Khare, V.; Singh, M.; Asghar, S.A. Comparison of rapid immuno-chromatographic card test with elisa in diagnosis of dengue fever at tertiary care centre. Indian J. Microbiol. Res. 2018, 5, 284–287. [Google Scholar]
- World Health Organization. WHO Guidance for the Use of Annex 2 of the International Health Regulations (2005); World Health Organization: Geneva, Switzerland, 2008. [Google Scholar]
- Stone, K.; Horney, J.A. Methods: Surveillance. In Disaster Epidemiology; Academic Press: London, UK, 2018. [Google Scholar]
- Johansen, I.C.; do Carmo, R.L.; Correia Alves, L.; Bueno, M.D. Environmental and demographic determinants of dengue incidence in Brazil. Rev. Salud. Públ. 2018, 20, 346–353. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pliego Pliego, E.; Velázquez-Castro, J.; Eichhorn, M.P.; Fraguela Collar, A. Increased efficiency in the second-hand tire trade provides opportunity for dengue control. J. Theor. Biol. 2018, 437, 126–136. [Google Scholar] [CrossRef] [Green Version]
- Sobral, M.F.F.; Sobral, A.I.G.D.P. Casos de dengue e coleta de lixo urbano: Um estudo na Cidade do Recife, Brasil. Cien. Saude Colet. 2019, 24, 1075–1082. [Google Scholar] [CrossRef]
- Barreto, M.L.; Teixeira, M.G.; Bastos, F.I.; Ximenes, R.A.A.; Barata, R.B.; Rodrigues, L.C. Successes and failures in the control of infectious diseases in Brazil: Social and environmental context, policies, interventions, and research needs. Lancet 2011, 377, 1877–1889. [Google Scholar] [CrossRef]
- Teixeira, M.G.; Costa, M.C.; Souza, L.P.; Nascimento, E.M.; Barreto, M.L.; Barbosa, N.; Carmo, E.H. Evaluation of Brazil’s public health surveillance system within the context of the International Health Regulations (2005). Rev. Panam. Salud Públ. 2012, 32, 49–55. [Google Scholar] [CrossRef] [Green Version]
- Brady, O.J.; Smith, D.L.; Scott, T.W.; Hay, S.I. Dengue disease outbreak definitions are implicitly variable. Epidemics 2015, 11, 92–102. [Google Scholar] [CrossRef] [Green Version]
- Cortes, F.; Martelli, C.M.; de Alencar Ximenes, R.A.; Montarroyos, U.R.; Junior, J.B.; Cruz, O.G.; Alexander, N.; de Souza, W.V. Time series analysis of dengue surveillance data in two Brazilian cities. Acta Trop. 2018, 182, 190–197. [Google Scholar] [CrossRef]
- Duarte, H.H.P.; França, E.B. Qualidade dos dados da vigilância epidemiológica da dengue em Belo Horizonte, MG. Rev. Saude Publ. 2006, 40, 134–142. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- SINANWEB. Sinan Dengue/Chikungunya. Portalsinan.Saude.Gov. 2016. Available online: http://www.portalsinan.saude.gov.br/sinan-dengue-chikungunya (accessed on 10 March 2020).
- Silva, M.M.; Rodrigues, M.S.; Paploski, I.A.; Kikuti, M.; Kasper, A.M.; Cruz, J.S.; Queiroz, T.L.; Tavares, A.S.; Santana, P.M.; Araújo, J.M.; et al. Accuracy of Dengue Reporting by National Surveillance System, Brazil. Emerg. Infect. Dis. 2016, 22, 336–339. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Coelho, G.E.; Leal, P.L.; de Cerroni, M.P.; Simplicio, A.C.R.; Siqueira, J.B. Sensitivity of the Dengue Surveillance System in Brazil for Detecting Hospitalized Cases. PLoS Negl. Trop. Dis. 2016, 10, e0004705. [Google Scholar] [CrossRef] [PubMed]
- Costa, N.D. Austeridade, predominância privada e falha de governo na saúde. Cien. Saude Colet. 2017, 22, 1065–1074. [Google Scholar] [CrossRef] [Green Version]
- Garrafa, V.; Cunha, T.; Rocha Da Manchola, C. Access to Healthcare: A Central Question within Brazilian Bioethics. Camb. Q. Healthc. Ethics 2018, 27, 431–439. [Google Scholar] [CrossRef]
- Santos, A.D.O.; Campos Alves, S.M. Public Health System in Brazil nowadays: Challenges for its operation and funding. Cad Ibero Americanos Direito Sanitário 2016, 5, 65. [Google Scholar] [CrossRef] [Green Version]
- Castiglione, D.; Lovasi, G.S.; Carvalho, M.S. Perceptions and Uses of Public and Private Health Care in a Brazilian Favela. Qual. Health Res. 2018, 28, 159–172. [Google Scholar] [CrossRef]
- Silva, A.C.; Pereira, J.L.; Martins, T.C. Situação epidemiológica da coqueluche e dengue no Centro-Oeste e no Distrito Federal no período de 2001 a 2012. Available online: http://www.bdm.unb.br/handle/10483/15514 (accessed on 10 March 2020).
- Ramalho, W.M.; Silveira, B.D.; Catão, R.D.C.; Bitar, R.; de Araújo, W.N.; Gurgel, H.C. A Dengue: Contextos Temporal e Social no Distrito Federal. 2017. Available online: http://www.codeplan.df.gov.br/wp-content/uploads/2018/03/Brasília-em-Debate-17.pdf (accessed on 10 March 2020).
- Subsecretaria de Vigilância à Saúde. Informativo no26, Setembro de 2019. Brasilia. 2019. Available online: http://www.saude.df.gov.br/informes-dengue/ (accessed on 10 March 2020).
- Finkbeiner, P. Qualitative Research: Semi-structured Expert Interview. In Social Media for Knowledge Sharing in Automotive Repair; Springer International Publishing: Cham, Switzerland, 2017; pp. 141–181. [Google Scholar]
- Adams, W.C. Conducting Semi-Structured Interviews. In Handbook of Practical Program Evaluation; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2015; pp. 492–505. [Google Scholar]
- Bogner, A.; Littig, B.; Menz, W. Introduction: Expert Interviews—An Introduction to a New Methodological Debate. In Interviewing Experts; Palgrave Macmillan: London, UK, 2009; pp. 157–183. [Google Scholar]
- Glaser, B.G.; Strauss, A.L. The Discovery of Grounded Theory: Strategies for Qualitative Research. 2012. Available online: https://books.google.co.th/books/about/The_Discovery_of_Grounded_Theory.html?id=rtiNK68Xt08C&redir_esc=y (accessed on 10 March 2020).
- Teddlie, C.; Yu, F. Mixed Methods Sampling. J. Mix. Methods Res. 2007, 1, 77–100. [Google Scholar] [CrossRef]
- McNabb, S.J.; Chungong, S.; Ryan, M.; Wuhib, T.; Nsubuga, P.; Alemu, W.; Carande-Kulis, V.; Rodier, G. Conceptual framework of public health surveillance and action and its application in health sector reform. BMC Public Health 2002, 2, 2. [Google Scholar] [CrossRef] [Green Version]
- Bradley, E.H.; Curry, L.A.; Devers, K.J. Qualitative Data Analysis for Health Services Research: Developing Taxonomy, Themes, and Theory. Health Serv. Res. 2007, 42, 1758–1772. [Google Scholar] [CrossRef] [Green Version]
- Mangen, S. Qualitative research methods in cross-national settings. Int. J. Soc. Res. Methodol. 1999, 2, 109–124. [Google Scholar] [CrossRef]
- Stoop, A.P.; Berg, M. Integrating Quantitative and Qualitative Methods in Patient Care Information System Evaluation. Methods Inf. Med. 2003, 42, 458–462. [Google Scholar] [PubMed]
- Ministério da Saúde. Guia de Vigilância em Saúde: Volume único. 2019. Available online: http://bvsms.saude.gov.br/bvs/publicacoes/guia_vigilancia_saude_3ed.pdf (accessed on 10 March 2020).
- Ministério da Saúde. Plano de Contingência Nacional para Epidemias de Dengue. Available online: www.saude.gov.br/bvs (accessed on 10 March 2020).
- Ministério da Saúde. Levantamiento Rápido de Índices Para Aedes Aegypti—LIRAa—Para Vigilancia Entomológica de Aedes Aegypti en Brasil. Brasilia. 2015. Available online: http://bvsms.saude.gov.br/bvs/publicacoes/levantamiento_rapido_indices_aedes_aegypti_liraa.pdf (accessed on 10 March 2020).
- Rollemberg, R. Decreto 37488 de 18 July 2016. Sistema Integrado de Normas Juridicas. 2016. Available online: http://www.sinj.df.gov.br/SINJ/Norma/804947ccf6ab4abab2465f52a515adf5/Decreto_37488_18_07_2016.html (accessed on 10 March 2020).
- Sistema de Nota Técnica do DF. Available online: http://sisaps.saude.gov.br/notatecnica/frmListaMunic.php (accessed on 10 March 2020).
- Dye, C. After 2015: Infectious diseases in a new era of health and development. Philos. Trans. R. Soc. B Biol. Sci. 2014, 369, 20130426. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Heymann, D.L.; Dar, O.A. Prevention is better than cure for emerging infectious diseases. BMJ 2014, 348, g1499. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- WHO Global Strategy on People-Centred and Integrated Health Services Interim Report. 2015. Available online: https://www.who.int/servicedeliverysafety/areas/people-centred-care/global-strategy/en/ (accessed on 10 March 2020).
- Dorussen, H.; Lenz, H.; Blavoukos, S. Assessing the Reliability and Validity of Expert Interviews. Eur. Union Polit. 2005, 6, 315–337. [Google Scholar] [CrossRef]

| Department | N. of Interviewees | ID Code |
|---|---|---|
| General Coordination of Arbovirosis Surveillance, Ministry of Health | 6 | A1–A6 |
| Directory of Epidemiological Surveillance, Federal District | 3 | B1–B2 |
| Unit of Epidemiological Surveillance, health region of the DF | 1 | C |
| General Coordination of Public Laboratories, Ministry of Health | 1 | D |
| General Coordination of Public Health Emergencies, Ministry of Health | 1 | E |
| General Coordination of Environmental Surveillance, Ministry of Health | 1 | F |
| Directory of Environmental Surveillance, Federal District | 2 | G1–G2 |
| Field workers for environmental (vector) surveillance, Federal District | 2 | H1–H2 |
| Type of Notification Unit | % of Notified Cases |
|---|---|
| Public Hospitals | 56.32 |
| Emergency Healthcare Units | 17.65 |
| Basic Healthcare Units | 14.72 |
| Private Hospitals | 4.32 |
| Private Laboratories | 4.08 |
| Non-Governmental Organizations | 1.34 |
| Other Public Units | 0.80 |
| Other Private Units | 0.73 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Angelo, M.; Ramalho, W.M.; Gurgel, H.; Belle, N.; Pilot, E. Dengue Surveillance System in Brazil: A Qualitative Study in the Federal District. Int. J. Environ. Res. Public Health 2020, 17, 2062. https://doi.org/10.3390/ijerph17062062
Angelo M, Ramalho WM, Gurgel H, Belle N, Pilot E. Dengue Surveillance System in Brazil: A Qualitative Study in the Federal District. International Journal of Environmental Research and Public Health. 2020; 17(6):2062. https://doi.org/10.3390/ijerph17062062
Chicago/Turabian StyleAngelo, Marco, Walter Massa Ramalho, Helen Gurgel, Nayara Belle, and Eva Pilot. 2020. "Dengue Surveillance System in Brazil: A Qualitative Study in the Federal District" International Journal of Environmental Research and Public Health 17, no. 6: 2062. https://doi.org/10.3390/ijerph17062062
APA StyleAngelo, M., Ramalho, W. M., Gurgel, H., Belle, N., & Pilot, E. (2020). Dengue Surveillance System in Brazil: A Qualitative Study in the Federal District. International Journal of Environmental Research and Public Health, 17(6), 2062. https://doi.org/10.3390/ijerph17062062