Indoor Air Pollution, Related Human Diseases, and Recent Trends in the Control and Improvement of Indoor Air Quality
Abstract
:1. Introduction
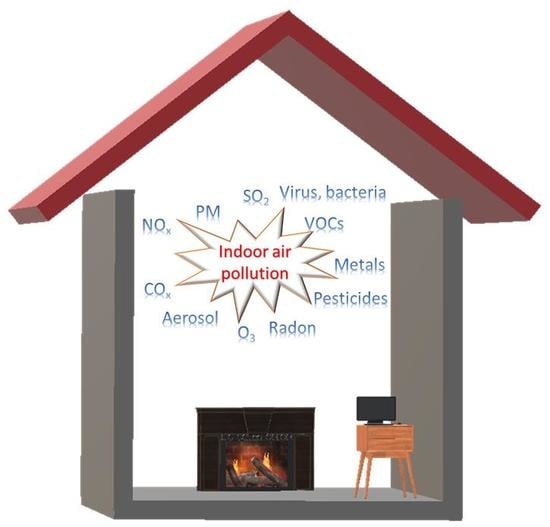
2. Indoor Air Quality (IAQ) and Indoor Air Pollution (IAP)
3. Main Pollutants in Indoor Air Environment
3.1. Particulate Matters
3.2. VOCs
3.3. NOX
3.4. Ozone
3.5. SO2
3.6. COx
3.7. Toxic Metals
3.8. Aerosols
3.9. Radon
3.10. Pesticides
3.11. Biological Pollutants
4. IAQ Guidelines and Standards
5. The Oxidative Capacity of Indoor Environment
6. The Effects of Indoor Air Pollution to Human Health
6.1. Building-Associated Illness
6.1.1. Sick Building Syndrome (SBS)
6.1.2. Building-Related Illness (BRI)
6.2. Acute Respiratory Infection
6.3. Pulmonary Diseases
6.4. Cardiovascular Diseases (CVDs)
7. Current Strategies for Monitoring and Control of IAQ
7.1. Development of Materials for IAQ Sensors
7.2. Advanced Technologies for Monitoring of IAQ
7.2.1. Internet of Thing (IoT)-Based Systems
7.2.2. Wireless Sensor Network (WSN)-Based Systems
7.3. Air Purification Technologies for IAQ Improvement
7.4. Smart Home for IAQ Control
8. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Leech, J.A.; Nelson, W.C.; Burnett, R.T.; Aaron, S.; Raizenne, A.M.E. It’s about time: A comparison of canadian and american time–activity patterns. J. Expo. Sci. Environ. Epidemiol. 2002, 12, 427–432. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- WHO. Household Air Pollution and Health. Available online: https://www.who.int/en/news-room/fact-sheets/detail/household-air-pollution-and-health (accessed on 28 January 2020).
- Kumar, P.; Imam, B. Footprints of air pollution and changing environment on the sustainability of built infrastructure. Sci. Total Environ. 2013, 444, 85–101. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ekmekcioglu, D.; Keskin, S.S. Characterization of indoor air particulate matter in selected elementary schools in istanbul, turkey. Indoor Built Environ. 2007, 16, 169–176. [Google Scholar] [CrossRef]
- Hromadka, J.; Korposh, S.; Partridge, M.C.; James, S.W.; Davis, F.; Crump, D.; Tatam, R.P. Multi-parameter measurements using optical fibre long period gratings for indoor air quality monitoring. Sens. Actuat. B Chem. 2017, 244, 217–225. [Google Scholar] [CrossRef]
- Koivisto, A.J.; Kling, K.I.; Hänninen, O.; Jayjock, M.; Löndahl, J.; Wierzbicka, A.; Fonseca, A.S.; Uhrbrand, K.; Boor, B.E.; Jiménez, A.S.; et al. Source specific exposure and risk assessment for indoor aerosols. Sci. Total Environ. 2019, 668, 13–24. [Google Scholar] [CrossRef] [PubMed]
- Hamanaka, R.B.; Mutlu, G.M. Particulate matter air pollution: Effects on the cardiovascular system. Front. Endocrinol. 2018, 9, 680. [Google Scholar] [CrossRef] [Green Version]
- USEPA. Introduction to Indoor Air Quality. Available online: https://www.epa.gov/indoor-air-quality-iaq/introduction-indoor-air-quality (accessed on 28 January 2020).
- Argunhan, Z.; Avci, A.S. Statistical evaluation of indoor air quality parameters in classrooms of a university. Adv. Merteorol. 2018, 2018, 4391579. [Google Scholar] [CrossRef]
- USEPA. Fundamentals of Indoor Air Quality in Buildings. Available online: https://www.epa.gov/indoor-air-quality-iaq/fundamentals-indoor-air-quality-buildings (accessed on 28 January 2020).
- Fang, L.; Clausen, G.; Fanger, P.O. Impact of temperature and humidity on the perception of indoor air quality. Indoor Air 2004, 8, 80–90. [Google Scholar] [CrossRef]
- Marć, M.; Śmiełowska, M.; Namieśnik, J.; Zabiegała, B. Indoor air quality of everyday use spaces dedicated to specific purposes—A review. Environ. Sci. Pollut. Res. 2018, 25, 2065–2082. [Google Scholar] [CrossRef] [Green Version]
- Peng, Z.; Deng, W.; Tenorio, R. Investigation of indoor air quality and the identification of influential factors at primary schools in the north of china. Sustainability 2017, 9, 1180. [Google Scholar] [CrossRef]
- Poupard, O.; Blondeau, P.; Iordache, V.; Allard, A. Statistical analysis of parameters influencing the relationshipbetween outdoor and indoor air quality in schools. Atmos. Environ. 2005, 39, 2071–2080. [Google Scholar] [CrossRef]
- Liang, J. Other toxins in the air. In Chemical Modeling for Air Resources: Fundamentals, Applications and Corroborative Analysis; Elsevier: Amsterdam, The Netherlands, 2013; pp. 221–237. [Google Scholar]
- Micallef, A.; Caldwell, J.; Colls, J.J. The influence of human activity on the vertical distribution of airborne particle concentration in confined environments: Preliminary results. Indoor Air 1998, 8, 131–136. [Google Scholar] [CrossRef]
- Linaker, C.H.; Chauhan, A.J.; Inskip, H.; Frew, A.J.; Sillence, A.; Coggon, D.; Holgate, S.T. Distribution and determinants of personal exposure to nitrogen dioxide in school children. Occup. Environ. Med. 1996, 53, 200–203. [Google Scholar] [CrossRef] [PubMed]
- Ström, J.; Alfredsson, L.; Malmfors, T.; Selroos, O. Nitrogen dioxide: Causation and aggravation of lung diseases. Indoor Environ. 1994, 3, 58–68. [Google Scholar]
- Awbi, H.B. Ventilation of Buildings; Spon Press: London, UK, 2003. [Google Scholar]
- Op’t Veld, P. Introduction to ec reshyvent–eu cluster project on demandcontrolled hybrid ventilation for residential buildings. Build. Environ. 2008, 43, 1342–1349. [Google Scholar] [CrossRef]
- Chenari, B.; Carrilho, J.D.; Silva, M.G. Towards sustainable, energy-efficient and healthy ventilationstrategies in buildings: A review. Renew. Sustain. Energy Rev. 2016, 59, 1426–1447. [Google Scholar] [CrossRef]
- Vornanen-Winqvist, C.; Salonen, H.; Järvi, K.; Andersson, M.A.; Mikkola, R.; Marik, T.; Kredics, L.; Kurnitski, J. Effects of ventilation improvement on measured and perceived indoor air quality in a school building with a hybrid ventilation system. Int. J. Environ. Res. Public Health 2018, 15, 1414. [Google Scholar] [CrossRef] [Green Version]
- OSHA. Technical Manual: Indoor air Quality Investigation. Available online: https://www.osha.gov/dts/osta/otm/otm_iii/otm_iii_2.html (accessed on 28 January 2020).
- Leung, D.Y.C. Outdoor-indoor air pollution in urban environment: Challenges and opportunity. Front. Environ. Sci. 2015, 2, 69. [Google Scholar] [CrossRef]
- USEPA. Indoor Particulate Matter. Available online: https://www.epa.gov/indoor-air-quality-iaq/indoor-particulate-matter (accessed on 28 January 2020).
- Miller, M.R.; Shaw, C.A.; Langrish, J.P. From particles to patients: Oxidative stress and the cardiovascular effects of air pollution. Future Cardiol. 2012, 8, 577–602. [Google Scholar] [CrossRef] [Green Version]
- Brook, R.D.; Rajagopalan, S.; PopeIII, C.A.; Brook, J.R.; Bhatnagar, A.; Diez-Roux, A.V.; Holguin, F.; Hong, Y.; Luepker, R.V.; Mittleman, M.A.; et al. Particulate matter air pollution and cardiovascular disease: An update to the scientific statement from the american heart association. Circulation 2010, 121, 2331–2378. [Google Scholar] [CrossRef] [Green Version]
- Ferro, A.R.; Kopperud, R.J.; Hildemann, L.M. Elevated personal exposure to particulate matter from human activities in a residence. J. Expo. Sci. Environ. Epid. 2004, 14, S34–S40. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wallace, L. Indoor particles: A review. J. Air Waste Manag. Assoc. 1996, 46, 98–126. [Google Scholar] [CrossRef] [PubMed]
- Dennekamp, M.; Howarth, S.; Dick, C.A.J.; Cherrie, J.W.; Donaldson, K.; Seaton, A. Ultrafine particles and nitrogen oxides generated by gas and electric cooking. Occup. Environ. Med. 2001, 58, 511–516. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yu, K.-P.; Yang, K.R.; Chen, Y.C.; Gong, J.Y.; Chen, Y.P.; Shih, H.-C.; Lung, S.-C.C. Indoor air pollution from gas cooking infive taiwanese families. Build. Environ. 2015, 93, 258–266. [Google Scholar] [CrossRef]
- Kim, H.; Kang, K.; Kim, T. Measurement of particulate matter (pm2.5) and health risk assessment of cooking-generated particles in the kitchen and living rooms of apartment houses. Sustainability 2018, 10, 843. [Google Scholar] [CrossRef] [Green Version]
- Ferro, A.R.; Kopperud, R.J.; Hildemann, L.M. Source strengths for indoor human activities that resuspend particulate matter. Environ. Sci. Technol. 2004, 38, 1759–1764. [Google Scholar] [CrossRef]
- USEPA. Volatile Organic Compounds’ Impact on Indoor Air Quality. Available online: https://www.epa.gov/indoor-air-quality-iaq/volatile-organic-compounds-impact-indoor-air-quality (accessed on 28 January 2020).
- Huang, Y.; Ho, S.S.H.; Ho, K.F.; Lee, S.C.; Yu, J.Z.; Louie, P.K.K. Characteristics and health impacts of vocs and carbonyls associated withresidential cooking activities in hong kong. J. Hazard. Mater. 2011, 186, 344–351. [Google Scholar] [CrossRef]
- Liu, S.; Li, R.; Wild, R.J.; Warneke, C.; Gouw, J.A.d.; Brown, S.S.; Miller, S.L.; Luongo, J.C.; Jimenez, J.L.; Ziemann, P.J. Contribution of human-related sources to indoor volatile organiccompounds in a university classroom. Indoor Air 2016, 26, 925–938. [Google Scholar] [CrossRef]
- Lee, K.; Choi, J.-H.; Lee, S.; Park, H.-J.; Oh, Y.-J.; Kim, G.; Lee, W.-S.; Son, B.-S. Indoor levels of volatile organic compounds and formaldehyde from emission sources at elderly care centers in korea. PLoS ONE 2018, 13, e0197495. [Google Scholar] [CrossRef]
- Dunagan, S.C.; Dodson, R.E.; Rudel, R.A.; Brody, J.G. Toxics use reduction in the home: Lessons learned from household exposure studies. J. Clean Prod. 2011, 19, 438–444. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tang, X.; Misztal, P.K.; Nazaroff, W.W.; Goldstein, A.H. Siloxanes are the most abundant volatile organic compound emitted from engineering students in a classroom. Environ. Sci. Technol. Lett. 2015, 2, 303–307. [Google Scholar] [CrossRef] [Green Version]
- Chin, J.-Y.; Godwin, C.; Parker, E.; Robins, T.; Lewis, T.; Harbin, P.; Batterman, S. Levels and sources of volatile organic compounds in homes of children with asthma. Indoor Air 2014, 24, 403–415. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lucattini, L.; Poma, G.; Covaci, A.; Boer, J.d.; Lamoree, M.H.; Leonards, P.E.G. A review of semi-volatile organic compounds (svocs) in the indoorenvironment: Occurrence in consumer products, indoor air and dust. Chemosphere 2018, 201, 466–482. [Google Scholar] [CrossRef] [PubMed]
- Okubo, M.; Kuwahara, T. Chapter 5-prospects for marine diesel engine emission control. In New Technologies for Emission Control in Marine Diesel Engines; Elsevier: Amsterdam, The Netherlands, 2020; pp. 211–266. [Google Scholar]
- Brickus, L.R.; Cardoso, J.; Neto, F.R.D.A. Distributions of indoor and outdoor air pollutants in rio de janeiro, brazil: Implications to indoor air quality in bayside offices. Environ. Sci. Technol. 1998, 32, 3485–3490. [Google Scholar] [CrossRef]
- Weschler, C.J.; Nazaroff, W.W. Svoc exposure indoors: Fresh look at dermal pathways. Indoor Air 2012, 22, 356–377. [Google Scholar] [CrossRef]
- Weschler, C.J.; Nazaroff, W.W. Dermal uptake of organic vapors commonly found in indoor air. Environ. Sci. Technol. 2014, 48, 1230–1237. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bernstein, J.A.; Alexis, N.; Bacchus, H.; Bernstein, I.L.; Fritz, P.; Horner, E.; Li, N.; Mason, S.; Nel, A.; Oullette, J.; et al. The health effects of nonindustrial indoor air pollution. J. Allergy Clin. Immunol. 2008, 121, 585–591. [Google Scholar] [CrossRef] [PubMed]
- WHO. Guidelines for Indoor Air Quality: Selected Pollutants; World Health Organization Regional Office for Europe: Bonn, Germany, 2010. [Google Scholar]
- Kodama, Y.; Arashidani, K.; Tokui, N.; Kawamoto, T.; Matsuno, K.; Kunugita, N.; Minakawa, N. Environmental NO2 concentration and exposure in daily life along main roads in tokyo. Environ. Res. 2002, 89, 236–244. [Google Scholar] [CrossRef]
- Spengler, J.; Samet, J.; McCarthy, J.F. Indoor Air Quality Handbook; McGraw-Hill Professional: New York, NY, USA, 2001. [Google Scholar]
- Weschler, C.J. Ozone in indoor environments: Concentration and chemistry. Indoor Air 2000, 10, 269–288. [Google Scholar] [CrossRef] [Green Version]
- Salonen, H.; Salthammer, T.; Morawska, L. Human exposure to ozone in school and office indoor environments. Environ. Int. 2018, 119, 503–514. [Google Scholar] [CrossRef]
- Huang, Y.; Yang, Z.; Gao, Z. Contributions of indoor and outdoor sources to ozone in residential buildings in nanjing. Int. J. Environ. Res. Public Health 2019, 16, 2587. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brown, S.K. Assessment of pollutant emissions from dry-process photocopiers. Indoor Air 1999, 9, 259–267. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.C.; Lam, S.; Fai, H.K. Characterization of vocs, ozone, and pm10 emissions from office equipment in an environmental chamber. Build. Environ. 2001, 36, 837–842. [Google Scholar] [CrossRef]
- Zhang, Q.; Jenkins, P.L. Evaluation of ozone emissions and exposures from consumer products and home appliances. Indoor Air 2016, 27, 386–397. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Guo, C.; Gao, Z.; Shen, J. Emission rates of indoor ozone emission devices: A literature review. Build. Environ. 2019, 158, 302–318. [Google Scholar] [CrossRef]
- Weschler, C.J.; Shields, H.C.; Naik, D.V. Indoor ozone exposures. Air Repair 1989, 39, 1562–1568. [Google Scholar] [CrossRef]
- Weschler, C.J. Roles of the human occupant in indoor chemistry. Indoor Air 2015, 26, 6–24. [Google Scholar] [CrossRef]
- Katsouyanni, K.; Touloumi, G.; Spix, C.; Schwartz, J.; Balducci, F.; Medina, S.; Rossi, G.; Wojtyniak, B.; Sunyer, J.; Bacharova, L.; et al. Short term effects of ambient sulphur dioxide and particulate matter on mortality in 12 european cities: Results from time series data from the aphea project. BMJ 1997, 314, 1658. [Google Scholar] [CrossRef] [Green Version]
- Seow, W.J.; Downward, G.S.; Wei, H.; Rothman, N.; Reiss, B.; Xu, J.; Bassig, B.A.; Li, J.; He, J.; Hosgood, H.D.; et al. Indoor concentrations of nitrogen dioxide and sulfur dioxide from burning solid fuels for cooking and heating in yunnan province, china. Indoor Air 2016, 26, 776–783. [Google Scholar] [CrossRef]
- Hänninen, O.; Goodman, P. Outdoor air as a source of indoor pollution. In Indoor Air Pollution; The Royal Society of Chemistry: London, UK, 2019; pp. 35–65. [Google Scholar]
- WHO. Air Quality Guidelines: Chapter 7.4 Sulfur Dioxide; WHO Regional Office for Europe: Copenhagen, Denmark, 2000. [Google Scholar]
- International Programme on Chemical Safety. Carbon Monoxide; World Health Organization: Geneva, Switzerland, 1999. [Google Scholar]
- Raub, J.A.; Mathieu-Nolf, M.; Hampson, N.B.; Thom, S.R. Carbon monoxide poisoning–A public health perspective. Toxicology 2000, 145, 1–14. [Google Scholar] [CrossRef]
- Zhang, X.; Wargocki, P.; Lian, Z.; Thyregod, C. Effects of exposure to carbon dioxide and bioeffluents on perceivedair quality, self-assessed acute health symptoms and cognitiveperformance. Indoor Air 2017, 27, 47–64. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Persily, A.; de Jonge, L. Carbon dioxide generation rates for building occupants. Indoor Air 2017, 27, 868–879. [Google Scholar] [CrossRef] [PubMed]
- Emmerich, S.J.; Persily, A.K. State-of-the-Art Review of CO2 Demand Controlled Ventilation Technology and Application; Diane Publishing: Darby, PA, USA, 2003; p. 43. [Google Scholar]
- Ramalho, O.; Wyart, G.; Mandin, C.; Blondeau, P.; Cabanes, P.-A.; Leclerc, N.; Mullot, J.-U.; Boulanger, G.; Redaelli, M. Association of carbon dioxide with indoor air pollutants andexceedance of health guideline values. Build. Environ. 2015, 93, 115–124. [Google Scholar] [CrossRef]
- ANSI/ASHRAE Standard 62.1-2013. Ventilation for Acceptable Indoor Air Quality; American Society of Heating, Refrigerating and Air-Conditioning Engineers, Inc.: Atlanta, GA, USA, 2013. [Google Scholar]
- Azuma, K.; Kagi, N.; Yanagi, U.; Osawa, H. Effects of low-level inhalation exposure to carbon dioxide in indoorenvironments: A short review on human health and psychomotorperformance. Environ. Int. 2018, 121, 51–56. [Google Scholar] [CrossRef]
- Komarnicki, G.J.K. Lead and cadmium in indoor air and the urban environment. Environ. Pollut. 2005, 136, 47–61. [Google Scholar] [CrossRef]
- Al-Rajhi, M.A.; Seaward, M.R.D.; Al-Aamer, A.S. Metal levels in indoor and outdoor dust in riyadh, saudi arabia. Environ. Int. 1996, 22, 315–324. [Google Scholar] [CrossRef]
- Kang, Y.; Cheung, K.C.; Wong, M.H. Mutagenicity, genotoxicity and carcinogenic risk assessment of indoor dust from three major cities around the pearl river delta. Environ. Int. 2011, 37, 637–643. [Google Scholar] [CrossRef]
- Tan, S.Y.; Praveena, S.M.; Abidin, E.Z.; Cheema, M.S. A review of heavy metals in indoor dust and its human health-risk implications. Rev. Environ. Health 2016, 31, 447–456. [Google Scholar] [CrossRef] [Green Version]
- Sanborn, M.D.; Abelsohn, A.; Campbell, M.; Weir, E. Identifying and managing adverse environmental health effects: 3. Lead exposure. Can. Med. Assoc. J. 2002, 166, 1287–1292. [Google Scholar]
- Tchounwou, P.B.; Patlolla, A.K.; Centeno, J.A. Carcinogenic and systemic health effects associated with arsenic exposure—A critical review. Toxicol. Pathol. 2003, 31, 575–588. [Google Scholar] [CrossRef]
- Faiz, Y.; Tufail, M.; Javed, M.T.; Chaudhry, M.M.; Naila, S. Road dust pollution of cd, cu, ni, pb and zn along islamabad expressway, pakistan. Microchem. J. 2009, 92, 186–192. [Google Scholar] [CrossRef]
- Turner, A.; Hefzi, B. Levels and bioaccessibilities of metals in dusts from an arid environment. Water Air Soil Pollut. 2009, 210, 483–491. [Google Scholar] [CrossRef]
- Morawska, L.; Afshari, A.; Bae, G.N.; Buonanno, G.; Chao, C.Y.H.; Hänninen, O.; Hofmann, W.; Isaxon, C.; Jayaratne, E.R.; Pasanen, P.; et al. Indoor aerosols: From personal exposure to risk assessment. Indoor Air 2013, 23, 462–487. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Komae, S.; Sekiguchi, K.; Suzuki, M.; Nakayama, R.; Namiki, N.; Kagi, N. Secondary organic aerosol formation from p-dichlorobenzene under indoor environmental conditions. Build. Environ. 2020, 174, 106758. [Google Scholar] [CrossRef]
- Liang, C.-S.; Duan, F.-K.; He, K.-B.; Ma, Y.-L. Review on recent progress in observations, source identifications andcountermeasures of pm2.5. Environ. Int. 2016, 86, 150–170. [Google Scholar] [CrossRef]
- Shiraiwa, M.; Ueda, K.; Pozzer, A.; Lammel, G.; Kampf, C.J.; Fushimi, A.; Enami, S.; Arangio, A.M.; Frohlich-Nowoisky, J.; Fujitani, Y.; et al. Aerosol health effects from molecular to global scales. Environ. Sci. Technol. 2017, 51, 13545–13567. [Google Scholar] [CrossRef]
- Seinfeld, J.H.; Pandis, S.N. Atmospheric Chemistry and Physics: From Air Pollution to Climate Change; Wiley: Hoboken, NJ, USA, 2016. [Google Scholar]
- Vu, T.V.; Ondracek, J.; Zdímal, V.; Schwarz, J.; Delgado-Saborit, J.M.; Harrison, R.M. Physical properties and lung deposition of particles emitted from five major indoor sources. Air Qual. Atmos. Health 2017, 10, 1–14. [Google Scholar] [CrossRef] [Green Version]
- Nazaroff, W.W. Indoor particle dynamics. Indoor Air 2004, 14, 175–183. [Google Scholar] [CrossRef]
- Bruno, R.C. Sources of indoor radon in houses: A review. J. Air Pollut. Control Assoc. 1983, 32, 105–109. [Google Scholar] [CrossRef]
- Stranden, E.; Berteig, L. Radon in dwellings and influencing factors. Health Phys. 1980, 39, 275. [Google Scholar] [CrossRef]
- Gesell, T.F. Background atmospheric radon-222 concentrations outdoors and indoors: A review. Health Phys. 1983, 45, 289–302. [Google Scholar] [CrossRef] [PubMed]
- USEPA. Epa Assessment of Risks From Radon in Homes; United States Environmental Protection Agency: Washington, DC, USA, 2003.
- WHO. Who Handbook on Indoor Radon: A Public Health Perspective; World Health Organization: Geneva, Switzerland, 2009. [Google Scholar]
- Unger, A.; Schniewind, A.; Unger, W. Conservation of Wood Artifacts; Sringer: Berlin, Germany, 2001. [Google Scholar]
- Holt, E.; Audy, O.; Booij, P.; Melymuk, L.; Prokes, R.; Klánová, J. Organochlorine pesticides in the indoor air of a theatre and museum inthe czech republic: Inhalation exposure and cancer risk. Sci. Total Environ. 2017, 609, 598–606. [Google Scholar] [CrossRef] [PubMed]
- USEPA. Pesticides’ Impact on Indoor Air Quality. Available online: https://www.epa.gov/indoor-air-quality-iaq/pesticides-impact-indoor-air-quality (accessed on 28 January 2020).
- Gallart-Mateu, D.; Armenta, S.; Guardia, M.d.l. Indoor and outdoor determination of pesticides in air by ion mobilityspectrometry. Talanta 2016, 161, 632–639. [Google Scholar] [CrossRef] [PubMed]
- Colt, J.S.; Severson, R.K.; Lubin, J.; Rothman, N.; Camann, D.; Davis, S.; Cerhan, J.R.; Cozen, W.; Hartge, P. Organochlorines in carpet dust and non-hodgkin lymphoma. Epidemiology 2005, 16, 516–525. [Google Scholar] [CrossRef] [PubMed]
- Abb, M.; Breuer, J.V.; Zeitz, C.; Lorenz, W. Analysis of pesticides and pcbs in waste wood and house dust. Chemosphere 2010, 81, 488–493. [Google Scholar] [CrossRef]
- Colt, J.S.; Lubin, J.; Camann, D.; Davis, S.; Cerhan, J.; Severson, R.K.; Cozen, W.; Hartge, P. Comparison of pesticide levels in carpet dust and self-reported pest treatment practices in four us sites. J. Expo. Anal. Environ. Epidemiol. 2004, 14, 74–83. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hwang, H.-M.; Park, E.-K.; Young, T.M.; Hammock, B.D. Occurrence of endocrine-disrupting chemicals in indoor dust. Sci. Total Environ. 2008, 404, 26–35. [Google Scholar] [CrossRef] [Green Version]
- Kim, K.-H.; Kabir, E.; Jahan, S.A. Exposure to pesticides and the associated human health effects. Sci. Total Environ. 2017, 575, 525–535. [Google Scholar] [CrossRef] [PubMed]
- WHO. Indoor Air Quality: Biological Contaminants: Report on a Who Meeting, Rautavaara; World Health Organization Regional Office for Europe: Copenhagen, Denmark, 1988; Volume 31. [Google Scholar]
- Bousquet, J.; Khaltaev, N.; Cruz, A.A.; Denburg, J.; Fokkens, W.J.; Togias, A.; Zuberbier, T.; Baena-Cagnani, C.E.; Canonica, G.W.; Weel, C.V.; et al. Allergic rhinitis and its impact on asthma (aria) 2008. Allergy 2008, 63, 8–160. [Google Scholar] [CrossRef] [PubMed]
- Hulin, M.; Simoni, M.; Viegi, G.; Annesi-Maesano, I. Respiratory health and indoor air pollutants based on quantitative exposure assessments. Eur. Respir. J. 2012, 40, 1033–1045. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Baldacci, S.; Maio, S.; Cerrai, S.; Sarno, G.; Baız, N.; Simoni, M.; Annesi-Maesano, I.; Viegi, G. Allergy and asthma: Effects of the exposureto particulate matter and biological allergens. Respir. Med. 2015, 109, 1089–1104. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hospodsky, D.; Qian, J.; Nazaroff, W.W.; Yamamoto, N.; Bibby, K.; Rismani-Yazdi, H.; Peccia, J. Human occupancy as a source of indoor airborne bacteria. PLoS ONE 2012, 7, e34867. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- USEPA. Carbon Monoxide’s Impact on Indoor Air Quality. Available online: https://www.epa.gov/indoor-air-quality-iaq/carbon-monoxides-impact-indoor-air-quality (accessed on 28 January 2020).
- Rashed, M.N. Total and extractable heavy metals in indoor, outdoor and street dust from aswan city, Egypt. Clean 2008, 36, 850–857. [Google Scholar] [CrossRef]
- Madany, I.M. The correlations between heavy metals in residential indoor dust and outdoor street dust in bahrain. Environ. Int. 1994, 20, 483–492. [Google Scholar] [CrossRef]
- Oh, H.-J.; Jeong, N.-N.; Sohn, J.-R.; Kim, J. Personal exposure to indoor aerosols as actual concern: Perceived indoorand outdoor air quality, and health performances. Build. Environ. 2019, 165, 106403. [Google Scholar] [CrossRef]
- Kulmala, M.; Asmi, A.; Pirjola, L. Indoor air aerosol model: The effect of outdoor air, filtration and ventilation on indoor concentrations. Atmos. Environ. 1999, 33, 2133–2144. [Google Scholar] [CrossRef]
- Avgelis, A.; Papadopoulos, A.M. Indoor air quality guidelines and standards–A state of the art review. Int. J. Vent. 2004, 3, 267–278. [Google Scholar] [CrossRef]
- WHO. Air Quality Guidelines for Europe, 2nd ed.; The World Health Organization: Geneva, Switzerland, 2000. [Google Scholar]
- Al-Hemoud, A.; Al-Awadi, L.; Al-Khayat, A.; Behbehani, W. Streamlining IAQ guidelines and investigating the effect of door opening/closing on concentrations of VOCs, formaldehyde, and NO2 in office buildings. Build. Environ. 2018, 137, 127–137. [Google Scholar] [CrossRef]
- Abdul-Wahab, S.A.; En, S.C.F.; Elkamel, A.; Ahmadi, L.; Yetilmezsoy, K. A review of standards and guidelines set by international bodies for the parameters of indoor air quality. Atmos. Pollut. Res. 2015, 6, 751–767. [Google Scholar] [CrossRef]
- Mandin, C.; Bonvallot, N.; Kirchner, S.; Keirsbulck, M.; Alary, R.; Cabanes, P.A.; Dor, F.; Moullec, Y.L.; Mullot, J.-U.; Peel, A.E.; et al. Development of french indoor air quality guidelines. Clean Soil Air Water 2009, 37, 494–499. [Google Scholar] [CrossRef]
- Becher, R.; Hongslo, J.K.; Dybing, E. Guidelines for indoor air in norway–a practicalapproach. Pollut. Atmos. 2000, 166, 245–246. [Google Scholar]
- Husman, T.M. The health protection act, national guidelines for indoor air quality and development of the national indoor air programs in finland. Environ. Health Perspect. 1999, 107, 515–517. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Young, C.J.; Zhou, S.; Siegel, J.A.; Kahan, T.F. Illuminating the dark side of indoor oxidants. Environ. Sci. Process. Impacts 2019, 21, 1229. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gligorovski, S.; Weschler, C.J. The oxidative capacity of indoor atmospheres. Environ. Sci. Technol. 2013, 47, 13905–13906. [Google Scholar] [CrossRef] [PubMed]
- Finlayson-Pitts, B.J.; Pitts, J.N. Tropospheric air pollution: Ozone, airborne toxics, polycyclic aromatic hydrocarbons, and particles. Science 1997, 276, 1045–1052. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alvarez, E.G.; Afif, D.A.; Gligorovski, S.; Schoemaecker, C.; Fittschen, C.; Doussin, J.-F.; Wortham, H. Unexpectedly high indoor hydroxyl radical concentrations associated with nitrous acid. Proc. Natl. Acad. Sci. USA 2013, 110, 13294–13299. [Google Scholar] [CrossRef] [Green Version]
- Salthammer, T.; Mentese, S.; Marutsky, R. Formaldehyde in the indoor environment. Chem. Rev. 2010, 110, 2536–2572. [Google Scholar] [CrossRef]
- Hult, E.; Willem, H.; Price, P.N.; Hotchi, T.; Russell, M.; Singer, B.C. Formaldehyde and acetaldehyde exposure mitigation in us residences: In-home measurements of ventilation control and source control. Indoor Air 2015, 25, 523–535. [Google Scholar] [CrossRef] [Green Version]
- Destaillats, H.; Maddalena, R.L.; Singer, B.C.; Hodgson, A.T.; McKone, T.E. Indoor pollutants emitted by office equipment: A review of reported data and information needs. Atmos. Environ. 2008, 42, 1371–1388. [Google Scholar] [CrossRef] [Green Version]
- Stonner, C.; Edtbauer, A.; Williams, J. Real-world volatile organic compound emission rates from seated adults and children for use in indoor air studies. Indoor Air 2018, 28, 164–172. [Google Scholar] [CrossRef]
- Misztal, P.K.; Lymperopoulou, D.S.; Adams, R.I.; Scott, R.A.; Lindow, S.E.; Bruns, T.; Taylor, J.W.; Uehling, J.; Bonito, G.; Vilgalys, R. Emission factors of microbial volatile organic compounds from environmental bacteria and fungi. Environ. Sci. Technol. 2018, 52, 8272–8282. [Google Scholar] [CrossRef]
- Marmot, A.F.; Eley, J.; Stafford, M.; Stansfeld, S.A.; Warwick, E.; Marmot, M.G. Building health: An epidemiological study of "sick building syndrome" in the whitehall ii study. Occup. Environ. Med. 2006, 63, 283–289. [Google Scholar] [CrossRef] [PubMed]
- Joshi, S.M. The sick building syndrome. Indian J. Occup. Environ. Med. 2008, 12, 61–64. [Google Scholar] [CrossRef] [PubMed]
- Redlich, C.A.; Sparer, J.; Cullen, M.R. Sick-building syndrome. Lancet 1997, 349, 1013–1016. [Google Scholar] [CrossRef]
- Guo, P.; Yokoyama, K.; Piao, F.; Sakai, K.; Khalequzzaman, M.; Kamijima, M.; Nakajima, T.; Kitamura, F. Sick building syndrome by indoor air pollution in dalian, China. Int. J. Environ. Res. Public Health 2013, 10, 1489–1504. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kreiss, K. The epidemiology of building-related complaints and illness. Occup. Med. 1989, 4, 575–592. [Google Scholar]
- USEPA. Sick Building Syndrome; United States Environmental Protection Agency: Washington, DC, USA, 1991; Volume 4.
- International Labour Organisation (ILO). Encyclopedia of Accupational Safety and Health-Sick Building Syndrome; International Labour Organisation (ILO): Geneva, Switzerland, 2011. [Google Scholar]
- Zhang, X.; Li, F.; Zhang, L.; Zhao, Z.; Norback, D. A longitudinal study of sick building syndrome (SBS) among pupils in relation to SO2, NO2, O3 and PM10 in schools in china. PLoS ONE 2014, 9, e112933. [Google Scholar] [CrossRef] [Green Version]
- Li, L.; Adamkiewicz, G.; Zhang, Y.; Spengler, J.D.; Qu, F.; Sundell, J. Effect of traffic exposure on sick building syndrome symptoms among parents/ grandparents of preschool children in beijing, China. PLoS ONE 2015, 10, e0128767. [Google Scholar] [CrossRef]
- Seltzer, J.M. Building-related illnesses. J. Allergy Clin. Immunol. 1994, 94, 351–361. [Google Scholar] [CrossRef]
- Gerardi, D.A. Building-related illness. Clin. Pulm. Med. 2010, 17, 276–281. [Google Scholar] [CrossRef]
- Simkovich, S.M.; Goodman, D.; Roa, C.; Crocker, M.E.; Gianella, G.E.; Kirenga, B.J.; Wise, R.A.; Checkley, W. The health and social implications of household air pollution and respiratory diseases. NPJ Prim. Care Respir. Med. 2019, 29, 12. [Google Scholar] [CrossRef] [PubMed]
- Grief, S.N. Upper respiratory infections. Prim. Care 2013, 40, 757–770. [Google Scholar] [CrossRef] [PubMed]
- Jary, H.; Simpson, H.; Havens, D.; Manda, G.; Pope, D.; Bruce, N.; Mortimer, K. Household air pollution and acute lower respiratory infections in adults: A systematic review. PLoS ONE 2016, 11, e0167656. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, D.; Chen, Z.; Zhou, L.-F.; Huang, S.-X. Air pollutants and early origins of respiratory diseases. Chronic Dis. Transl. Med. 2018, 4, 75–94. [Google Scholar] [CrossRef]
- Kim, K.-H.; Jahan, S.A.; Kabir, E. A review of diseases associated with household air pollution due to the use o fbiomass fuels. J. Hazard. Mater. 2011, 192, 425–431. [Google Scholar] [CrossRef] [PubMed]
- Smith, K.R.; Samet, J.M.; Romieu, I.; Bruce, N. Indoor air pollution in developing countries and acute lower respiratory infections in children. Thorax 2000, 55, 518–532. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Raaschou-Nielsen, O.; Beelen, R.; Wang, M.; Hoek, G.; Andersen, Z.J.; Hoffmann, B.; Stafoggia, M.; Samoli, E.; Weinmayr, G.; Dimakopoulou, K.; et al. Particulate matter air pollution components and risk for lung cancer. Environ. Int. 2016, 87, 66–73. [Google Scholar] [CrossRef]
- Kirkby, J.; Bountziouka, V.; Lum, S.; Wade, A.; Stocks, J. Natural variability of lung function in young healthy school children. Eur. Respir. J. 2016, 48, 411–419. [Google Scholar] [CrossRef]
- Smith-Sivertsen, T.; Dı´az, E.; Pope, D.; Lie, R.T.; Dı´az, A.; McCracken, J.; Bakke, P.; Arana, B.; Smith, K.R.; Bruce, N. Effect of reducing indoor air pollution on women’s respiratory symptoms and lung function: The respire randomized trial, guatemala. Am. J. Epidemiol. 2009, 170, 211–220. [Google Scholar] [CrossRef]
- Regalado, J.; Pe´rez-Padilla, R.; Sansores, R.l.; Ramirez, J.I.P.r.; Brauer, M.; Pare´, P.; Vedal, S. The effect of biomass burning on respiratory symptoms and lung function in rural mexican women. Am. J. Respir. Crit. Care Med. 2006, 174, 901–905. [Google Scholar] [CrossRef]
- Ceylan, E.; Kocyigit, A.; Gencer, M.; Aksoy, N.; Selek, S. Increased DNA damage in patients with chronic obstructive pulmonary disease who had oncesmoked or been exposed to biomass. Respir. Med. 2006, 100, 1270–1276. [Google Scholar] [CrossRef] [Green Version]
- Kim, Y.-K.; Oh, S.-Y.; Jeon, S.G.; Park, H.-W.; Lee, S.-Y.; Chun, E.-Y.; Bang, B.; Lee, H.-S.; Oh, M.-H.; Kim, Y.-S.; et al. Airway exposure levels of lipopolysaccharide determine type 1 versus type 2 experimental asthma. J. Allergy Clin. Immunol. 2007, 178, 5375–5382. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Kim, E.K.; Park, H.J.; McDowell, A.; Kim, Y.-K. The impact of bacteria-derived ultrafine dust particles on pulmonary diseases. Exp. Mol. Med. 2020, 52, 338–347. [Google Scholar] [CrossRef] [PubMed]
- Charpin, D.; Birnbaum, J.; Haddi, E.; Genard, G.; Lanteaume, A.; Toumi, M.; Faraj, F.; Brempt, X.V.D.; Vervloet, D. Altitude and allergy to house-dust mites. A paradigm of the influence of environmental exposure on allergic sensitization. Am. Rev. Respir. Dis. 1991, 143, 983–986. [Google Scholar] [CrossRef] [PubMed]
- Kurmi, O.P.; Lam, K.B.H.; Ayres, J.G. Indoor air pollution and the lung in low- and medium-income countries. Eur. Respir. J. 2012, 40, 239–254. [Google Scholar] [CrossRef] [PubMed]
- Torres-Duque, C.; Maldonado, D.; Pe´rez-Padilla, R.; Ezzati, M.; Viegi, G. Biomass fuels and respiratory diseases-A review of the evidence. Proc. Am. Thorac. Soc. 2008, 5, 577–590. [Google Scholar] [CrossRef] [PubMed]
- Jiang, X.-Q.; Mei, X.-D.; Feng, D. Air pollution and chronic airway diseases: What should people know and do? J. Thorac. Dis. 2016, 8, E31–E40. [Google Scholar]
- Kurmi, O.P.; Arya, P.H.; Lam, K.-B.H.; Sorahan, T.; Ayres, J.G. Lung cancer risk and solid fuel smoke exposure: A systematic review and meta-analysis. Eur. Respir. J. 2012, 40, 1228–1237. [Google Scholar] [CrossRef] [Green Version]
- Sun, S.; Schiller, J.H.; Gazdar, A.F. Lung cancer in never smokers-a different disease. Nat. Rev. Cancer 2007, 7, 778–790. [Google Scholar] [CrossRef]
- Mu, L.; Liu, L.; Niu, R.; Zhao, B.; Shi, J.; Li, Y.; Scheider, W.; Su, J.; Chang, S.-C.; Yu, S.; et al. Indoor air pollution and risk of lung cancer among chinese female non-smokers. Cancer Causes Control. 2013, 24, 439–450. [Google Scholar] [CrossRef] [Green Version]
- Zhang, J.; Smith, K.R.; Ma, Y.; Ye, S.; Jiang, F.; Qi, W.; Liu, P.; Khalil, M.A.K.; Rasmussen, R.A.; Thorneloe, S.A. Greenhouse gases and other airborne pollutantsfrom household stoves in china: A databasefor emission factors. Atmos. Environ. 2000, 34, 4537–4549. [Google Scholar] [CrossRef] [Green Version]
- Turner, M.C.; Krewski, D.; Pope, C.A.; Chen, Y.; Gapstur, S.M.; Thun, M.J. Long-term ambient fine particulate matter air pollution and lung cancer in a large cohort of never-smokers. Am. J. Respir. Crit. Care Med. 2011, 184, 1374–1381. [Google Scholar] [CrossRef] [PubMed]
- Uzoigwe, J.C.; Prum, T.; Bresnahan, E.; Garelnabi, M. The emerging role of outdoor and indoor air pollution in cardiovascular disease. N. Am. J. Med. Sci. 2013, 5, 445–453. [Google Scholar] [PubMed]
- Peters, A.; Liu, E.; Verrier, R.; Schwartz, J.; Gold, D.; Mittleman, M.; Baliff, J.; Oh, J.; Allen, G.; Monahan, K.; et al. Air pollution and incidence of cardiac arrhythmia. Epidemiology 2000, 11, 11–17. [Google Scholar] [CrossRef] [PubMed]
- Singh, A.; Kesavachandran, C.N.; Kamal, R.; Bihari, V.; Ansari, A.; Azeez, P.A.; Saxena, P.N.; KS, A.K.; Khan, A.H. Indoor air pollution and its association with poor lung function, microalbuminuria and variations in blood pressure among kitchen workers in india: A cross-sectional study. Environ. Health 2017, 16, 33. [Google Scholar] [CrossRef] [Green Version]
- Kampfrath, T.; Maiseyeu, A.; Ying, Z.; Shah, Z.; Deiuliis, J.A.; Xu, X.; Kherada, N.; Brook, R.D.; Reddy, K.M.; Padture, N.P.; et al. Chronic fine particulate matter exposure induces systemic vascular dysfunction via NADPH oxidase and TLR4 pathways. Circ. Res. 2011, 108, 716–726. [Google Scholar] [CrossRef] [Green Version]
- Pan, C.-H.; Chan, C.-C.; Wu, K.-Y. Effects on chinese restaurant workers of exposure to cooking oil fumes: A cautionary note on urinary 8-hydroxy-2′-deoxyguanosine. Cancer Epidemiol. Biomark. Prev. 2008, 17, 3351–3357. [Google Scholar] [CrossRef] [Green Version]
- Bag, A.; Lee, N.-E. Gas sensing with heterostructures based on twodimensional nanostructured materials: A review. J. Mater. Chem. C 2019, 7, 13367. [Google Scholar] [CrossRef]
- Koziej, D.; Lauria, A.; Niederberger, M. Metal oxide particles in materials science: Addressing all length scales. Adv. Mater. 2014, 26, 235–257. [Google Scholar] [CrossRef]
- Liu, H.; Li, M.; Voznyy, O.; Hu, L.; Fu, Q.; Zhou, D.; Xia, Z.; Sargent, E.H.; Tang, J. Physically flexible, rapid-response gas sensor based on colloidal quantum dot solids. Adv. Mater. 2014, 26, 2718–2724. [Google Scholar] [CrossRef]
- Jariwala, D.; Marks, T.J.; Hersam, M.C. Mixed-dimensional van der waals heterostructures. Nat. Mater. 2017, 16, 170–181. [Google Scholar] [CrossRef] [PubMed]
- Choi, H.K.; Park, J.; Myoung, N.; Kim, H.-J.; Choi, J.S.; Choi, Y.K.; Hwang, C.-Y.; Kim, J.T.; Park, S.; Yi, Y.; et al. Gas molecule sensing of van der waals tunnel field effect transistors. Nanoscale 2017, 9, 18644–18650. [Google Scholar] [CrossRef] [PubMed]
- Cho, B.; Yoon, J.; Lim, S.K.; Kim, A.R.; Kim, D.-H.; Park, S.-G.; Kwon, J.-D.; Lee, Y.-J.; Lee, K.-H.; Lee, B.H.; et al. Chemical sensing of 2d graphene/mos2 heterostructure device. ACS Appl. Mater. Interfaces 2015, 7, 16775–16780. [Google Scholar] [CrossRef] [PubMed]
- Masson, N.; Piedrahita, R.; Hannigan, M. Approach for quantification of metal oxide type semiconductor gassensors used for ambient air quality monitoring. Sens. Actuat. B Chem. 2015, 208, 339–345. [Google Scholar] [CrossRef]
- Kim, B.-Y.; Ahn, J.H.; Yoon, J.-W.; Lee, C.-S.; Kang, Y.C.; Abdel-Hady, F.; Wazzan, A.A.; Lee, J.-H. Highly selective xylene sensor based on nio/nimoo4 nanocomposite hierarchical spheres for indoor air monitoring. ACS Appl. Mater. Interfaces 2016, 8, 34603–34611. [Google Scholar] [CrossRef] [PubMed]
- Baron, R.; Saffell, J. Amperometric gas sensors as a low cost emerging technology platform for air quality monitoring applications: A review. ACS Sens. 2017, 2, 1553–1566. [Google Scholar] [CrossRef] [PubMed]
- Oosthuizen, D.N.; Motaung, D.E.; Swart, H.C. Selective detection of co at room temperature with cuo nanoplateletssensor for indoor air quality monitoring manifested by crystallinity. Appl. Surf. Sci. 2019, 466, 545–553. [Google Scholar] [CrossRef]
- Saini, J.; Dutta, M.; Marques, G. A comprehensive review on indoor air quality monitoring systems for enhanced public health. Sustain. Environ. Res. 2020, 30, 6. [Google Scholar] [CrossRef] [Green Version]
- Pitarma, R.; Marques, G.; Caetano, F. Monitoring Indoor Air Quality to Improve Occupational Health; Springer: Basel, Switzerland, 2016. [Google Scholar]
- Persaud, K.; Dodd, G. Analysis of discrimination mechanisms in the mammalian olfactory system using a model nose. Nature 1982, 299, 352–355. [Google Scholar] [CrossRef]
- Freund, M.S.; Lewis, N.S. A chemically diverse conducting polymer-based “electronic nose”. Proc. Natl. Acad. Sci. USA 1995, 92, 2652–2656. [Google Scholar] [CrossRef] [Green Version]
- Scott, S.M.; James, D.; Ali, Z. Data analysis for electronic nose systems. Microchim Acta 2007, 156, 183–207. [Google Scholar] [CrossRef]
- Chen, K.; Gao, W.; Emaminejad, S.; Kiriya, D.; Ota, H.; Nyein, H.Y.Y.; Takei, K.; Javey, A. Printed carbon nanotube electronics and sensor systems. Adv. Mater. 2016, 28, 4397–4414. [Google Scholar] [CrossRef] [PubMed]
- Tastan, M.; Gökozan, H. Real-time monitoring of indoor air quality with internet of things-based e-nose. Appl. Sci. 2019, 9, 3435. [Google Scholar] [CrossRef]
- Chen, J.; Chen, Z.; Boussaid, F.; Zhang, D.; Pan, X.; Zhao, H.; Bermak, A.; Tsui, C.-Y.; Wang, X.; Fan, Z. Ultra-low-power smart electronic nose system based on three-dimensional tin oxide nanotube arrays. ACS Nano 2018, 12, 6079–6088. [Google Scholar] [CrossRef] [PubMed]
- Benammar, M.; Abdaoui, A.; Ahmad, S.H.M.; Touati, F.; Kadri, A. A modular iot platform for real-time indoor air quality monitoring. Sensors 2018, 18, 581. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chiesa, G.; Cesari, S.; Garcia, M.; Issa, M.; Li, S. Multisensor iot platform for optimising iaq levels in buildings through a smart ventilation system. Sustainability 2019, 11, 5777. [Google Scholar] [CrossRef] [Green Version]
- Jo, J.; Jo, B.; Kim, J.; Kim, S.; Han, W. Development of an iot-based indoor air quality monitoring platform. J. Sens. 2020, 2020, 8749764. [Google Scholar] [CrossRef]
- Sun, Z.; Wang, S.; Ma, Z. In-situ implementation and validation of a co2-based adaptive demand-controlled ventilation strategy in a multi-zone office building. Build. Environ. 2011, 46, 124–133. [Google Scholar] [CrossRef]
- Yick, J.; Mukherjee, B.; Ghosal, D. Wireless sensor network survey. Comput. Netw. 2008, 52, 2292–2330. [Google Scholar] [CrossRef]
- Arroyo, P.; Lozano, J.; Suárez, J.I. Evolution of wireless sensor network for air quality measurements. Electronics 2018, 7, 342. [Google Scholar] [CrossRef] [Green Version]
- Guglielmo, D.D.; Brienza, S.; Anastasi, G. Ieee 802.15.4e: A survey. Comput. Commun. 2016, 88, 1–24. [Google Scholar] [CrossRef]
- Yang, C.-T.; Chen, S.-T.; Den, W.; Wang, Y.-T.; Kristian, E. Implementation of an intelligent indoor environmental monitoring and management system in cloud. Future Gener. Comput. Syst. 2019, 96, 731–749. [Google Scholar] [CrossRef]
- Abraham, S.; Li, X. A cost-effective wireless sensor network system for indoor air quality monitoring applications. Proc. Comput. Sci. 2014, 34, 165–171. [Google Scholar] [CrossRef] [Green Version]
- Arroyo, P.; Herrero, J.L.; Suárez, J.I.; Lozano, J. Wireless sensor network combined with cloud computing for air quality monitoring. Sensors 2019, 19, 691. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pitarma, R.; Marques, G.; Ferreira, B.R. Monitoring indoor air quality for enhanced occupational health. J. Med. Syst. 2017, 41, 23. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.; Ho, S.S.H.; Lu, Y.; Niu, R.; Xu, L.; Cao, J.; Lee, S. Removal of indoor volatile organic compounds via photocatalytic oxidation: A short review and prospect. Molecules 2016, 21, 56. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Haghighat, F.; Lee, C.-S.; Pant, B.; Bolourani, G.; Lakdawala, N.; Bastani, A. Evaluation of various activated carbons for air cleaning–Towardsdesign of immune and sustainable buildings. Atmos. Environ. 2008, 42, 8176–8184. [Google Scholar] [CrossRef]
- Zhao, P.; Siegel, J.A.; Corsi, R.L. Ozone removal by hvac filters. Atmos. Environ. 2007, 41, 3151–3160. [Google Scholar] [CrossRef]
- Ligotski, R.; Sager, U.; Schneiderwind, U.; Asbach, C.; Schmidt, F. Prediction of voc adsorption performance for estimation of service life ofactivated carbon basedfilter media for indoor air purification. Build. Environ. 2019, 149, 146–156. [Google Scholar] [CrossRef]
- Carter, E.M.; Katz, L.E.; Speitel, G.E.; Ramirez, D. Gas-phase formaldehyde adsorption isotherm studies on activated carbon: Correlations of adsorption capacity to surface functional group density. Environ. Sci. Technol. 2011, 45, 6498–6503. [Google Scholar] [CrossRef]
- Jung, J.-S.; Kim, J.-G. An indoor air purification technology using a non-thermal plasmareactor with multiple-wire-to-wire type electrodes and afiber airfilter. J. Electrostat. 2017, 86, 12–17. [Google Scholar] [CrossRef]
- Francke, K.-P.; Miessner, H.; Rudolph, R. Plasmacatalytic processes for environmental problems. Catal. Today 2000, 59, 411–416. [Google Scholar] [CrossRef]
- Sathiamoorthy, G.; Kalyana, S.; Finney, W.C.; Clark, R.J.; Locke, B.R. Chemical reaction kinetics and reactor modeling of nox removal in a pulsed streamer corona discharge reactor. Ind. Eng. Chem. Res. 1999, 38, 1844–1855. [Google Scholar] [CrossRef]
- Urashima, K.; Chang, J.-S. Removal of volatile organic compounds from air streams and industrial flue gases by non-thermal plasma technology . IEEE Trans. Dielectr. Electr. Insul. 2000, 7, 602–614. [Google Scholar] [CrossRef]
- Bahri, M.; Haghighat, F. Plasma-based indoor air cleaning technologies: The state of the art-review. Clean Soil Air Water 2014, 42, 1667–1680. [Google Scholar] [CrossRef]
- Fujishima, A.; Honda, K. Photolysis-decomposition of water at the surface of an irradiated semiconductor. Nature 1972, 238, 37–38. [Google Scholar] [CrossRef]
- Weon, S.; He, F.; Choi, W. Status and challenges in photocatalytic nanotechnology for cleaning air polluted with volatile organic compounds: Visible light utilization and catalyst deactivation. Environ. Sci. Nano 2019, 6, 3185–3214. [Google Scholar] [CrossRef]
- Park, H.; Kim, H.-i.; Moon, G.-h.; Choi, W. Photoinduced charge transfer processes in solar photocatalysis based on modified tio2. Energy Environ. Sci. 2016, 9, 411–433. [Google Scholar] [CrossRef] [Green Version]
- Patil, K.; Laad, M.; Kamble, A.; Laad, S. A consumer-based smart home with indoor air quality monitoring system. IETE J. Res. 2019, 65, 758–770. [Google Scholar] [CrossRef]
- Zhou, B.; Li, W.; Chan, K.W.; Cao, Y.; Kuang, Y.; Liu, X.; Wang, X. Smart home energy management systems: Concept, configurations, and scheduling strategies. Renew. Sustain. Energy Rev. 2016, 61, 30–40. [Google Scholar] [CrossRef]
- Paetz, A.-G.; Dütschke, E.; Fichtner, W. Smart homes as a means to sustainable energy consumption: A study of consumer perceptions. J. Consum. Policy 2012, 35, 23–41. [Google Scholar] [CrossRef]
- Missaoui, R.; Joumaa, H.; Ploix, S.; Bacha, S. Managing energy smart homes according to energy prices: Analysisof a building energy management system. Energy Build. 2014, 71, 155–167. [Google Scholar] [CrossRef]
- Schieweck, A.; Uhde, E.; Salthammer, T.; Salthammer, L.C.; Morawska, L.; Mazaheri, M.; Kumar, P. Smart homes and the control of indoor air quality. Renew. Sustain. Energy Rev. 2018, 94, 705–718. [Google Scholar] [CrossRef]
- Kumar, P.; Skouloudis, A.N.; Bell, M.; Viana, M.; Carotta, M.C.; Biskos, G.; Morawska, L. Real-time sensors for indoor air monitoring and challenges ahead indeploying them to urban buildings. Sci. Total Environ. 2016, 560–561, 150–159. [Google Scholar] [CrossRef] [PubMed] [Green Version]




| Pollutants | Sources | Health Impacts | Refs |
|---|---|---|---|
| PM | Outdoor environment, cooking, combustion activities (burning of candles, use of fireplaces, heaters, stoves, fireplaces and chimneys, cigarette smoking), cleaning activities | Premature death in people with heart or lung disease, nonfatal heart attacks, irregular heartbeat, aggravated asthma, decreased lung function, increased respiratory symptoms | [7,25,26,27] |
| VOCs | Paints, stains, varnishes, solvents, pesticides, adhesives, wood preservatives, waxes, polishes, cleansers, lubricants, sealants, dyes, air fresheners, fuels, plastics, copy machines, printers, tobacco products, perfumes, dry-cleaned clothing, building materials and furnishings |
| [34,39,43,44,45] |
| NO2 | Gas-fueled cooking and heating appliances |
| [46] |
| O3 | Outdoor sources, photocopying, air purifying, disinfecting devices | DNA damage, lung damage, asthma, decreased respiratory functions | [51,52] |
| SO2 | Cooking stoves; fireplaces; outdoor air |
| [60] |
| COx | Cooking stoves; tobacco smoking; fireplaces; generators and other gasoline powered equipment; outdoor air | Fatigue, chest pain, impaired vision, reduced brain function | [64,105] |
| Heavy metals | Pb, Cd, Zn, Cu, Cr, As, Ni, Hg, Mn, Fe Outdoor sources, fuel-consumption products, incense burning, smoking and building materials |
| [71,106,107] |
| Aerosols | Tobacco smoke, building materials, consumer products, incense burning, cleaning and cooking | Cardiovascular diseases, respiratory diseases, allergies, lung cancer, irritation and discomfort | [6,108,109] |
| Radon (Rn) | Soil gas, building materials, and tap water Outdoor air | Lung cancer | [86,89,90] |
| Pesticides |
| Irritation to eye, nose and throat; Damage to central nervous system and kidney; Increased risk of cancer | [92,93,97,98] |
| Biological allergens | House dust, pets, cockroaches, mold/dampness, pollens originating from animals, insects, mites, and plants | Asthma and allergies Respiratory infections, sensitization, respiratory allergic diseases and wheezing | [100,103] |
| Microorganism | Bacteria, viruses, and fungi are carried by people, animals, and soil and plants | Fever, digestive problems, infectious diseases, chronic respiratory illness | [100,104] |
| Pollutants | Concentration Levels (mg/m3) | Exposure Time | Organization |
|---|---|---|---|
| CO | 100 | 15 min | WHO |
| 60 | 30 min | ||
| 30 | 1 h | ||
| 10 | 8 h | ||
| 29 | 1 h | USEPA | |
| 10 | 8 h | ||
| CO2 | 1800 | 1 h | WHO |
| NO2 | 0.4 | 1 h | WHO |
| 0.15 | 24 h | ||
| 0.1 | 1 year | USEPA | |
| PM | 0.15 | 24 h | USEPA |
| 0.05 | 1 year | ||
| O3 | 0.15–0.2 | 1 h | WHO |
| 0.1–0.12 | 8 h | ||
| 0.235 | 1 h | USEPA | |
| SO2 | 0.5 | 10 min | WHO |
| 0.35 | 1 h | ||
| 0.365 | 24 h | USEPA | |
| 0.08 | 1 year | ||
| Pb | 0.0005–0.001 | 1 year | WHO |
| 0.0015 | 3 months | USEPA | |
| Xylene | 8 | 24 h | WHO |
| Formaldehyde | 0.1 | 30 min | WHO |
| Radon | 100 Bq/m3 | 1 year | WHO |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tran, V.V.; Park, D.; Lee, Y.-C. Indoor Air Pollution, Related Human Diseases, and Recent Trends in the Control and Improvement of Indoor Air Quality. Int. J. Environ. Res. Public Health 2020, 17, 2927. https://doi.org/10.3390/ijerph17082927
Tran VV, Park D, Lee Y-C. Indoor Air Pollution, Related Human Diseases, and Recent Trends in the Control and Improvement of Indoor Air Quality. International Journal of Environmental Research and Public Health. 2020; 17(8):2927. https://doi.org/10.3390/ijerph17082927
Chicago/Turabian StyleTran, Vinh Van, Duckshin Park, and Young-Chul Lee. 2020. "Indoor Air Pollution, Related Human Diseases, and Recent Trends in the Control and Improvement of Indoor Air Quality" International Journal of Environmental Research and Public Health 17, no. 8: 2927. https://doi.org/10.3390/ijerph17082927
APA StyleTran, V. V., Park, D., & Lee, Y. -C. (2020). Indoor Air Pollution, Related Human Diseases, and Recent Trends in the Control and Improvement of Indoor Air Quality. International Journal of Environmental Research and Public Health, 17(8), 2927. https://doi.org/10.3390/ijerph17082927