Biomechanical Analysis of Stoop and Free-Style Squat Lifting and Lowering with a Generic Back-Support Exoskeleton Model
Abstract
:1. Introduction
2. Methods
2.1. Experimental Setup
2.2. Collection and Processing of the Motion Data
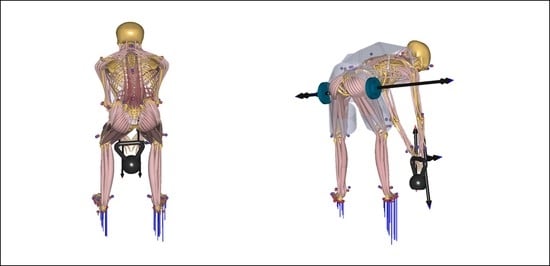
2.3. Human Musculoskeletal Model and Model of the External Load
2.4. Generic BSE Model
2.5. Biomechanical and Ergonomic Parameter Investigation
3. Results
3.1. Biomechanical Analysis without Exoskeleton
3.2. Analysis with Generic Exoskeleton Support
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- De Kok, J.; Vroonhof, P.; Snjiders, J.; Roullis, G.; Clarke, M.; Peereboom, K.; van Dorst, P.; Isusi, I. Work-Related Musculoskeletal Disorders: Prevalence, Costs and Demographics in the EU; European Risk Observatory Report; European Agency for Safety and Health at Work: Luxembourg, 2019. [Google Scholar]
- Luttmann, A.; Jäger, M.; Griefahn, B.; Caffier, G.; Liebers, F. Preventing Musculoskeletal Disorders in the Workplace; World Health Organization: Geneva, Switzerland, 2003. [Google Scholar]
- Monica, L.; Sara Anastasi, S.; Francesco Draicchio, F. Occupational Exoskeletons: Wearable Robotic Devices to Prevent Work-Related Musculoskeletal Disorders in the Workplace of the Future; European Agency for Safety and Health at Work: Luxembourg, 2020. [Google Scholar]
- Theurel, J.; Desbrosses, K. Occupational Exoskeletons: Overview of Their Benefits and Limitations in Preventing Work-Related Musculoskeletal Disorders. IISE Trans. Occup. Ergon. Hum. Factors 2019, 7, 264–280. [Google Scholar] [CrossRef]
- Agrawal, A.; Dube, A.N.; Kansara, D.; Shah, S.; Sheth, S. Exoskeleton: The Friend of Mankind in context of Rehabilitation and Enhancement. Indian J. Sci. Technol. 2016, 9, 1–8. [Google Scholar] [CrossRef]
- Bogue, R. Robotic exoskeletons: A review of recent progress. Ind. Robot. Int. J. 2015, 42, 5–10. [Google Scholar] [CrossRef]
- Gopura, R.A.R.C.; Bandara, D.S.V.; Kiguchi, K.; Mann, G.K.I. Developments in hardware systems of active upper-limb exoskeleton robots: A review. Robot. Auton. Syst. 2016, 75, 203–220. [Google Scholar] [CrossRef]
- Rupal, B.S.; Rafique, S.; Singla, A.; Singla, E.; Isaksson, M.; Virk, G.S. Lower-limb exoskeletons. Int. J. Adv. Robot. Syst. 2017, 14, 172988141774355. [Google Scholar] [CrossRef]
- Yang, C.-J.; Zhang, J.-F.; Chen, Y.; Dong, Y.-M.; Zhang, Y. A Review of exoskeleton-type systems and their key technologies. Proc. Inst. Mech. Eng. Part C J. Mech. Eng. Sci. 2008, 222, 1599–1612. [Google Scholar] [CrossRef]
- Young, A.J.; Ferris, D.P. State of the Art and Future Directions for Lower Limb Robotic Exoskeletons. IEEE Trans. Neural Syst. Rehabil. Eng. 2017, 25, 171–182. [Google Scholar] [CrossRef]
- Gull, M.A.; Bai, S.; Bak, T. A Review on Design of Upper Limb Exoskeletons. Robotics 2020, 9, 16. [Google Scholar] [CrossRef] [Green Version]
- Ottobock SE & Co. KGaA. Paexo Back: Innovative Back Relief for Logistics. Available online: https://paexo.com/paexo-back/?lang=en (accessed on 9 January 2021).
- ATOUN Inc. Powered Wear ATOUN Model Y. Available online: https://atoun.co.jp/en/products/atoun-model-y/ (accessed on 11 November 2021).
- German Bionic Systems GmbH. Cray X, 5. Generation. Available online: https://www.germanbionic.com/german-bionic-praesentiert-die-5-generation-seines-ki-gesteuerten-exoskeletts/ (accessed on 17 July 2022).
- Innophys Co., Ltd. Muscle Suit. Available online: https://innophys.jp/en/product/standard/ (accessed on 9 January 2021).
- Kinetic Edge. Flex Lift: A Comfortable Solutionto Injury and Fatigue. Available online: https://kineticedgeinc.com/ (accessed on 9 January 2020).
- Laevo. The Laevo V2. Available online: https://www.laevo-exoskeletons.com/en/laevo-v2 (accessed on 9 January 2020).
- U.S. Bionics, Inc. backX. Available online: https://www.suitx.com/backx (accessed on 9 January 2020).
- RB3D. exoBack: Descriptif Produit. Available online: https://www.rb3d.com/exosquelettes/exoback#description (accessed on 9 January 2021).
- Crea, S.; Beckerle, P.; De Looze, M.; De Pauw, K.; Grazi, L.; Kermavnar, T.; Masood, J.; O’Sullivan, L.W.; Pacifico, I.; Rodriguez-Guerrero, C. Occupational exoskeletons: A roadmap toward large-scale adoption. Methodology and challenges of bringing exoskeletons to workplaces. Wearable Technol. 2021, 2, e11. [Google Scholar] [CrossRef]
- Fondazione Ergo-MTM Italia, Exoskeleton Certification. Available online: https://www.eaws.it/exoskeleton-certification/ (accessed on 2 November 2021).
- Zelik, K.E.; Nurse, C.A.; Schall, M.C.; Sesek, R.F.; Marino, M.C.; Gallagher, S. An ergonomic assessment tool for evaluating the effect of back exoskeletons on injury risk. medRxiv 2021. [Google Scholar] [CrossRef]
- Tröster, M.; Schneider, U.; Bauernhansl, T.; Rasmussen, J.; Andersen, M. Simulation Framework for Active Upper Limb Exoskeleton Design Optimization Based on Musculoskeletal Modeling. In Technische Unterstützungssysteme, die die Menschen Wirklich Wollen: Dritte Transdisziplinäre Konferenz: Hamburg 2018; Weidner, R., Karafillidis, A., Eds.; Helmut-Schmidt-Universität: Hamburg, Germany, 2018; ISBN 978-3-86818-245-3. [Google Scholar]
- Agarwal, P.; Narayanan, M.S.; Lee, L.-F.; Mendel, F.; Krovi, V.N. Simulation-based Design of Exoskeletons Using Musculoskeletal Analysis. In Volume 3: 30th Computers and Information in Engineering Conference, Parts A and B, Proceedings of the ASME 2010 International Design Engineering Technical Conferences and Computers and Information in Engineering Conference, Montreal, QC, Canada, 15–18 August 2010; ASME: New York, NY, USA, 2010; pp. 1357–1364. ISBN 978-0-7918-4411-3. [Google Scholar]
- Zhou, L.; Li, Y.; Bai, S. A human-centered design optimization approach for robotic exoskeletons through biomechanical simulation. Robot. Auton. Syst. 2017, 91, 337–347. [Google Scholar] [CrossRef]
- Tröster, M.; Wagner, D.; Müller-Graf, F.; Maufroy, C.; Schneider, U.; Bauernhansl, T. Biomechanical Model-Based Development of an Active Occupational Upper-Limb Exoskeleton to Support Healthcare Workers in the Surgery Waiting Room. Int. J. Environ. Res. Public Health 2020, 17, 5140. [Google Scholar] [CrossRef] [PubMed]
- Norman, R.; Wells, R.; Neumann, P.; Frank, J.; Shannon, H.; Kerr, M.; Ontario Universities Back Pain Study (OUBPS) Group. A comparison of peak vs. cumulative physical work exposure risk factors for the reporting of low back pain in the automotive industry. Clin. Biomech. 1998, 13, 561–573. [Google Scholar] [CrossRef]
- Toxiri, S.; Verstraten, T.; Calanca, A.; Caldwell, D.G.; Ortiz, J. Using parallel elasticity in back-support exoskeletons: A study on energy consumption during industrial lifting tasks. In Proceedings of the 2019 Wearable Robotics Association Conference (WearRAcon), Scottsdale, AZ, USA, 25–27 March 2019. [Google Scholar] [CrossRef]
- Toxiri, S.; Näf, M.B.; Lazzaroni, M.; Fernández, J.; Sposito, M.; Poliero, T.; Monica, L.; Anastasi, S.; Caldwell, D.G.; Ortiz, J. Back-Support Exoskeletons for Occupational Use: An Overview of Technological Advances and Trends. IISE Trans. Occup. Ergon. Hum. Factors 2019, 7, 237–249. [Google Scholar] [CrossRef] [Green Version]
- Glitsch, U.; Bäuerle, I.; Hertrich, L.; Heinrich, K.; Liedtke, M. Biomechanische Beurteilung der Wirksamkeit von rumpfunterstützenden Exoskeletten für den industriellen Einsatz. Z. Arb. 2020, 74, 294–305. [Google Scholar] [CrossRef]
- Marinou, G.; Millard, M.; Šarabon, N.; Mombaur, K. Comparing the risk of low-back injury using model-based optimization: Improved technique versus exoskeleton assistance. Wearable Technol. 2021, 2, e13. [Google Scholar] [CrossRef]
- Bär, M.; Luger, T.; Seibt, R.; Rieger, M.A.; Steinhilber, B. Using a Passive Back Exoskeleton During a Simulated Sorting Task: Influence on Muscle Activity, Posture, and Heart Rate. Hum. Factors 2022, 1–16. [Google Scholar] [CrossRef]
- Steinhilber, B.; Luger, T.; Schwenkreis, P.; Middeldorf, S.; Bork, H.; Mann, B.; von Glinski, A.; Schildhauer, T.A.; Weiler, S.; Schmauder, M. The use of exoskeletons in the occupational context for primary, secondary, and tertiary prevention of work-related musculoskeletal complaints. IISE Trans. Occup. Ergon. Hum. Factors 2020, 8, 132–144. [Google Scholar] [CrossRef]
- Van der Have, A.; Rossom, S.; Jonkers, I. Squat Lifting Imposes Higher Peak Joint and Muscle Loading Compared to Stoop Lifting. Appl. Sci. 2019, 9, 3794. [Google Scholar] [CrossRef] [Green Version]
- Baltrusch, S.J.; van Dieën, J.H.; Koopman, A.S.; Näf, M.B.; Rodriguez-Guerrero, C.; Babič, J.; Houdijk, H. SPEXOR passive spinal exoskeleton decreases metabolic cost during symmetric repetitive lifting. Eur. J. Appl. Physiol. 2020, 120, 401–412. [Google Scholar] [CrossRef] [Green Version]
- Shourijeh, M.; Jung, M.M. Metabolic energy consumption in a box-lifting task: A parametric study on the assistive torque. In Wearable Robotics: Challenges and Trends; Springer: Cham, Switzerland, 2017; pp. 143–148. [Google Scholar]
- Kim, Y.; Shin, S.; Kong, K.; Han, D. Optimal Level of Assistance and Weight of Hip-joint Wearable Robot Considering Influences to the Human Body. IFAC-PapersOnLine 2019, 52, 13–18. [Google Scholar] [CrossRef]
- De Zee, M.; Hansen, L.; Wong, C.; Rasmussen, J.; Simonsen, E.B. A generic detailed rigid-body lumbar spine model. J. Biomech. 2007, 40, 1219–1227. [Google Scholar] [CrossRef] [PubMed]
- Bassani, T.; Stucovitz, E.; Qian, Z.; Briguglio, M.; Galbusera, F. Validation of the AnyBody full body musculoskeletal model in computing lumbar spine loads at L4L5 level. J. Biomech. 2017, 58, 89–96. [Google Scholar] [CrossRef] [PubMed]
- Damsgaard, M.; Rasmussen, J.; Christensen, S.T.; Surma, E.; de Zee, M. Analysis of musculoskeletal systems in the AnyBody Modeling System. Simul. Model. Pract. Theory 2006, 14, 1100–1111. [Google Scholar] [CrossRef]
- Andersen, M.S.; Damsgaard, M.; MacWilliams, B.; Rasmussen, J. A computationally efficient optimisation-based method for parameter identification of kinematically determinate and over-determinate biomechanical systems. Comput. Methods Biomech. Biomed. Eng. 2010, 13, 171–183. [Google Scholar] [CrossRef]
- Rasmussen, J.; de Zee, M.; Damsgaard, M.; Christensen, S.T.; Marek, C.; Siebertz, K. A general method for scaling musculo-skeletal models. In Proceedings of the 2005 International Symposium on Computer Simulation in Biomechanics, Cherry Hill, NJ, USA, 24–28 July 2005. [Google Scholar]
- Andersen, M.S.; Damsgaard, M.; Rasmussen, J. Kinematic analysis of over-determinate biomechanical systems. Comput. Methods Biomech. Biomed. Eng. 2009, 12, 371–384. [Google Scholar] [CrossRef]
- Fluit, R.; Andersen, M.S.; Kolk, S.; Verdonschot, N.; Koopman, H.F. Prediction of ground reaction forces and moments during various activities of daily living. J. Biomech. 2014, 47, 2321–2329. [Google Scholar] [CrossRef]
- Larsen, F.G.; Svenningsen, F.P.; Andersen, M.S.; de Zee, M.; Skals, S. Estimation of Spinal Loading During Manual Materials Handling Using Inertial Motion Capture. Ann. Biomed. Eng. 2020, 48, 805–821. [Google Scholar] [CrossRef]
- Margaria, R. Positive and negative work performances and their efficiencies in human locomotion. Int. Z. Angew. Physiol. Einschließlich Arb. 1968, 25, 339–351. [Google Scholar] [CrossRef]
- Jäger, M. Die “Revidierten Dortmunder Richtwerte”: Erweiterte Zusammenstellung von Autopsiematerial-Messungen der statischen lumbalen Kompressionsfestigkeit zur Ableitung von Referenzwerten für eine ergonomische Arbeitsgestaltung. Zent. Arb. 2019, 69, 271–289. [Google Scholar] [CrossRef]
- Wang, Z.; Wu, L.; Sun, J.; He, L.; Wang, S.; Yang, L. Squat, stoop or semi-squat: A comparative experiment on lifting technique. J. Huazhong Univ. Sci. Technol. Med. Sci. 2012, 32, 630–636. [Google Scholar] [CrossRef] [PubMed]
- Schmalz, T.; Colienne, A.; Bywater, E.; Fritzsche, l.; Gärtner, C.; Bellmann, M.; Reimer, S.; Ernst, M. A Passive Back-Support Exoskeleton for Manual Materials Handling: Reduction of Low Back Loading and Metabolic Effort during Repetitive Lifting. IISE Trans. Occup. Ergon. Hum. Factors 2021, 10, 7–20. [Google Scholar] [CrossRef] [PubMed]
- Koopman, A.S.; Näf, M.; Baltrusch, S.J.; Kingma, I.; Rodriguez-Guerrero, C.; Babič, J.; de Looze, M.P.; van Dieën, J.H. Biomechanical evaluation of a new passive back support exoskeleton. J. Biomech. 2020, 105, 109795. [Google Scholar] [CrossRef] [PubMed]
- Negrini, S.; Piovanelli, B.; Amici, C.; Cappellini, V.; Bovi, G.; Ferrarin, M.; Zaina, F.; Borboni, A. Trunk motion analysis: A systematic review from a clinical and methodological perspective. Eur. J. Phys. Rehabil. Med. 2016, 52, 583–592. [Google Scholar] [PubMed]
- Simon, A.A.; Alemi, M.M.; Asbeck, A.T. Kinematic effects of a passive lift assistive exoskeleton. J. Biomech. 2021, 120, 110317. [Google Scholar] [CrossRef]
- Koelewijn, A.D.; Heinrich, D.; van den Bogert, A.J. Metabolic cost calculations of gait using musculoskeletal energy models, a comparison study. PLoS ONE 2019, 14, e0222037. [Google Scholar] [CrossRef] [Green Version]
- Arones, M.M.; Shourijeh, M.S.; Patten, C.; Fregly, B.J. Musculoskeletal Model Personalization Affects Metabolic Cost Estimates for Walking. Front. Bioeng. Biotechnol. 2020, 8, 588925. [Google Scholar] [CrossRef]









| Kinetic Interfaces | Interaction Forces (14) | Interaction Moments (12) |
|---|---|---|
| human femur <> exo-thigh segment (2 × (left and right)) | FThigh,CC FThigh,ML FThigh,AP | TThigh,CC TThigh,ML TThigh,AP |
| human pelvis <> exo-hip segment | FHip,CC FHip,ML FHip,AP | THip,AP |
| human thorax <> exo-back segment | FThorax,CC FThorax,AP | - |
| exo-hip segment <> exo-back segment | FExoBack,CC FExoBack,ML FExoBack,AP | TExoBack,CC TExoBack,ML TExoBack,AP |
| exo-hip segment <> exo-thigh segment (2 × (left and right)) | - | TExoActuator,ML |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tröster, M.; Budde, S.; Maufroy, C.; Andersen, M.S.; Rasmussen, J.; Schneider, U.; Bauernhansl, T. Biomechanical Analysis of Stoop and Free-Style Squat Lifting and Lowering with a Generic Back-Support Exoskeleton Model. Int. J. Environ. Res. Public Health 2022, 19, 9040. https://doi.org/10.3390/ijerph19159040
Tröster M, Budde S, Maufroy C, Andersen MS, Rasmussen J, Schneider U, Bauernhansl T. Biomechanical Analysis of Stoop and Free-Style Squat Lifting and Lowering with a Generic Back-Support Exoskeleton Model. International Journal of Environmental Research and Public Health. 2022; 19(15):9040. https://doi.org/10.3390/ijerph19159040
Chicago/Turabian StyleTröster, Mark, Sarah Budde, Christophe Maufroy, Michael Skipper Andersen, John Rasmussen, Urs Schneider, and Thomas Bauernhansl. 2022. "Biomechanical Analysis of Stoop and Free-Style Squat Lifting and Lowering with a Generic Back-Support Exoskeleton Model" International Journal of Environmental Research and Public Health 19, no. 15: 9040. https://doi.org/10.3390/ijerph19159040
APA StyleTröster, M., Budde, S., Maufroy, C., Andersen, M. S., Rasmussen, J., Schneider, U., & Bauernhansl, T. (2022). Biomechanical Analysis of Stoop and Free-Style Squat Lifting and Lowering with a Generic Back-Support Exoskeleton Model. International Journal of Environmental Research and Public Health, 19(15), 9040. https://doi.org/10.3390/ijerph19159040