Optimization of the Use of Hospital Beds as an Example of Improving the Functioning of Hospitals in Poland on the Basis of the Provincial Clinical Hospital No. 1 in Rzeszow
Abstract
:1. Introduction
2. Materials and Methods
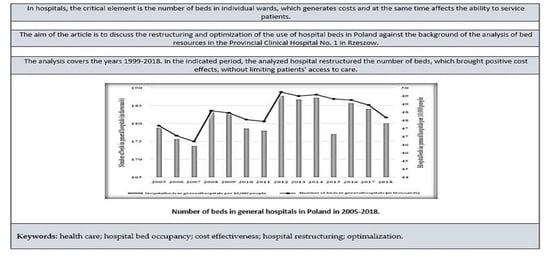
3. Results
4. Discussion
5. Conclusions
6. Limitations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Dubas-Jakóbczyk, K.; Kowalska-Bobko, I.; Sowada, C. The 2017 reform of the hospital sector in Poland—The challenge of consistent design. Health Policy 2019, 123, 538–543. [Google Scholar] [CrossRef] [PubMed]
- Tarnowska, A. Zróżnicowanie infrastruktury społecznej w województwach. (Differentiation of social infrastructure in voivodships.). Bibl. Reg. 2011, 11, 317–336. [Google Scholar]
- Orliński, R. Budżetowanie kosztów na przykładzie oddziału chorób wewnętrznych badanego szpitala (Cost budgeting based on the example of the internal medicine ward of the examined hospital). Zesz. Teor. Rachun. 2011, 119, 141–154. [Google Scholar]
- Moore, K. Hospital restructuring: Impact on nurses mediated by social support and a perception of challenge. J. Health Hum. Serv. Adm. 2001, 4, 490–517. [Google Scholar]
- Malinowski, W.; Nojszewska, E. Uwarunkowania ekonomiczne możliwości komercyjnego świadczenia usług medycznych przez polskie szpitale publiczne (Economic conditions of the possibility of commercial provision of medical services by Polish public hospitals). Nauk. O Zarządzaniu 2017, 3, 4–11. [Google Scholar]
- Dubas-Jakóbczyk, K.; Kozieł, A. Towards Financial Sustainability of the Hospital Sector in Poland—A Post Hoc Evaluation of Policy Approaches. Sustainability 2020, 12, 1–19. [Google Scholar] [CrossRef]
- Rabiej, E. Dostępność świadczeń zdrowotnych w perspektywie założeń i realizacji ustawy “O sieci szpitali”. (Availability of health services in the light of the assumptions and implementation of the Hospital Nerwork Act). Zesz. Nauk. Uniw. Rzeszowskiego. Ser. Prawnicza 2020, 30, 232–245. [Google Scholar] [CrossRef]
- Zu, L. Corporate Social Responsibility, Corporate Restructuring and Firm’s Performance; Springer: Heidelberg, Germany, 2009. [Google Scholar]
- Wiater, K. Restrukturyzacja i Upadłość: Zagadnienia Praktyczne (Restructuring and Bankruptcy: Practical Discussion); Wolters Kluwer: Warszawa, Poland, 2018. [Google Scholar]
- Romanowska, M. Restrukturyzacja jako reakcja na zmiany (na przykładzie grupy kapitałowej Zakładów Chemicznych “Police” SA) (Restructuring as a reaction to changes (on the example of the Zakłady Chemiczne ‘Police’ SA capital group). Studia I Pr. Wydziału Nauk. Ekon. I Zarządzania 2011, 21, 207–214. [Google Scholar]
- Arlbjorn, J.; Haug, A. Business Process Optimization; Academica: Aarhus, Denmark, 2010. [Google Scholar]
- Marciniak, M. Optymalizacja Zatrudnienia: Właściwe Praktyki w Czasie Zmian (Employment Optimization: Appropriate Practices in a Time of Change); Wolters Kluwer: Warszawa, Poland, 2020. [Google Scholar]
- Elias, A.; Davies, D. Analysing public sector continuous improvement: A systems approach. Int. J. Public Sect. Manag. 2017, 2, 2–13. [Google Scholar] [CrossRef]
- Jagodziński, J.; Ostrowski, D. Optymalizacja wybranego procesu produkcyjnego w oparciu o zasadę ciągłego doskonalenia na przykładzie przedsiębiorstwa X. (Optimization of the selected production process based on the principle of continuous improvement on the example of company X). Zesz. Nauk. Politech. Częstochowskiej. Zarządzanie 2016, 24, 201–214. [Google Scholar] [CrossRef]
- Bardhan, A.; Kumar, K. Restructuring Primary Health Care Network to Maximize Utilization and Reduce Patient Out-of-pocket Expenses. Asian J. Innov. Pol. 2019, 8, 122–140. [Google Scholar] [CrossRef]
- Polakowski, M.; Golinowska, S.; Balicki, M. Ochrona Zdrowia w Polsce (Healthcare in Poland); Friedrich-Ebert-Stiftung: Warszawa, Poland, 2019. [Google Scholar]
- Mikos, M.; Barczentewicz, P. Kwalifikacje kadry zarządzającej podmiotami leczniczymi (Qualifications of the management staff of medical entities.). In Zarządzanie Podmiotami Leczniczymi–Bezpieczeństwo Pacjentów i Sposoby Ograniczania Ryzyka Szpitali (Management of Medical Entities-Patient Safety and Methods of Limiting the Risk for Hospitals); Pasowicz, M., Ed.; Krakowskie Towarzystwo Edukacyjne–Oficyna Wydawnicza AFM: Kraków, Poland, 2012. [Google Scholar]
- Chamberland-Rowe, C.; Chiocchio, F.; Bourgeault, I. Harnessing instability as an opportunity for health system strengthening: A review of health system resilience. Healthc. Manag. Forum 2019, 3, 28–135. [Google Scholar] [CrossRef]
- Bułhaka, E. Restrukturyzacja zakładów opieki zdrowotnej w Polsce (Restructuring of Health Care Institutions in Poland). In Zarządzanie Restrukturyzacją w Procesach Integracji i Rozwoju Nowej Gospodarki (Restructuring Management in the Processes of Integration and Development of the New Economy); Wydawnictwo Uniwersytetu Ekonomicznego w Krakowie: Kraków, Poland, 2008. [Google Scholar]
- Klich, J. Health Care Systems’ Evolvement and the Changing Role of the State Inselected CEEC in Institute of Economic Research Working. In Proceedings of the VIIIth International Conference on Applied Economics Contemporary Issues in Economy, Toruń, Poland, 18–19 June 2015; Institute of Economic Research and Polish Economic Society Branch in Toruń: Toruń, Poland, 2015. Abstract Number 61. Available online: http://www.badania-gospodarcze.pl/images/WorkingPapers/2015No61.pdf (accessed on 22 January 2022).
- Fijałkowska, B. Meandry restrukturyzacji samodzielnych publicznych zakładów opieki zdrowotnej (Meanders of restructuring of independent public healthcare institutions). Zesz. Nauk. WSOWL 2013, 1, 209–223. [Google Scholar]
- The European Hospital and Healthcare Federation—HOPE: Hospitals in Europe. 2018. Available online: http://www.hope.be/wpcontent/uploads/2018/07/2018Hospitals-in-EU-28-Synthesis-final-for-publication-002.pdf (accessed on 5 February 2022).
- Wielicka, K.; Dźwigoł, H.; Męczyńska, A. Skuteczność procesu restrukturyzacji szpitali zlokalizowanych w województwie śląskim—koncepcja badań (Effectiveness of the restructuring process of hospitals located in the Silesian voivodeship—research concept). Organizacja i Zarządzanie. Zesz. Nauk. Politech. Śląskiej 2013, 63, 455–466. [Google Scholar]
- Oliviera, S. Predictive Models for Hospital Bed Management Using Data Mining Techniques. In New Perspectives in Information Systems and Technologies; Volume 2: Advances in Intelligent Systems and Computing; Rocha, A., Ed.; Springer International Publishing: Cham, Switzerland, 2020; pp. 407–416. [Google Scholar]
- Bójko, M.; Maślankiewicz, R. Sytuacja w polskiej psychiatrii dziecięcej na przełomie lat 2018 i 2019 na podstawie danych zebranych w trybie dostępu do informacji publicznej. (The situation in Polish child psychiatry at the turn of 2018 and 2019 based on data collected through access to public information). Dziecko Krzywdzone. Teor. Bad. Prakt. 2020, 19, 116–154. [Google Scholar]
- Krasowska-Marczyk, M.; Marciniak, E. Lecznictwo szpitalne w Polsce w okresie transformacji. Próba oceny działalności szpitali publicznych i niepublicznych w sferze organizacyjno-ekonomicznej w oparciu o model kartydokonań(Hospital treatment in Poland in the period of transformation. An attempt to assess the activities of public and private hospitals in the organizational and economic sphere based on the achievement card model). Studia Adm. 2017, 9, 17–28. [Google Scholar]
- Bank Danych Lokalnych. Poland. Available online: https://bdl.stat.gov.pl/bdl/dane/podgrup/temat (accessed on 15 February 2022).
- Rój, J. Efektywność usługowa jako kryterium wyboru mechanizmu finansowania szpitali (Service efficiency as a criterion for selecting a hospital financing mechanism.). Ruch Praw. Ekon. I Socjol. 2003, 4, 153–171. [Google Scholar]
- Devereaux, P.J.; Heels-Ansdell, D.; Lacchetti, C.; Haines, T.; Burns, E.A.; Cook, D.J. Payments for care at private for-profit and private not-for-profit hospitals: Asystematic review and meta-analysis. CMAJ Can. Med. Assoc. J.-J. L’association Med. Can. 2004, 170, 1817–1824. [Google Scholar] [CrossRef] [Green Version]
- Porębski, D. Pomiar Efektywności Ekonomicznej Szpitala z Wykorzystaniem Zrównoważonej Karty Wyników (Measurement of the Economic Efficiency of a Hospital with the Use of a Balanced Scorecard); Uniwersytet. Ekonomiczny we Wrocławiu: Wrocław, Poland, 2016. [Google Scholar]
- Goldwasser, R. Difficulties in access and estimates of public beds in intensive care units in the state of Rio de Janeiro. Rev. Saude Publica 2016, 50, 1–9. [Google Scholar] [CrossRef] [Green Version]
- Szewieczek, A. Rachunek kosztów szpitala–analiza i ewolucja regulacji prawnych (Hospital cost calculation - analysis and evolution of legal regulations.) Studia Ekonomiczne. Zesz. Nauk. Uniw. Ekon. W Katowicach 2019, 386, 108–121. [Google Scholar]
- Ustawa z Dnia 23 Marca 2017 r. o Zmianie Ustawy o świadczeniach Opieki Zdrowotnej Finansowanych Ze środków Publicznych (Act of 23 March 2017 Amending the Acton Health Care Benefits Financed from Public Funds). Dz. U. 2017 poz. 844. Available online: https://isap.sejm.gov.pl/isap.nsf/download.xsp/WDU20170000844/T/D20170844L.pdf (accessed on 15 February 2022).
- Robakowski, P.; Pogorzelczyk, K. Rola i zadania sieci szpitali publicznych w procesie kształtowania bezpieczeństwa zdrowotnego (The role and tasks of the public hospital network in the process of shaping health safety). Rocz. Bezpieczeństwa Międzynarodowego 2020, 14, 67–85. [Google Scholar]
- Wielicka-Gańczarczyk, K. Przyczyny restrukturyzacji samodzielnych publicznych zakładów opieki zdrowotnej (Reasons for restructuring independent public health care facilities). Organizacja i Zarządzanie. Zesz. Nauk. Politech. Śląskiej 2016, 89, 539–550. [Google Scholar]
- Cholewa-Wiktor, M. Efektywność w szpitalachpublicznych (Efficiency in public hospitals). Studia Ekonomiczne. Zesz. Nauk. Uniw. Ekon. W Katowicach 2014, 180, 44–54. [Google Scholar]
- OECD. Health at a Glance 2015: OECD Indicators, OECD Publishing, Paris. 2015. Available online: https://doi.org/10.1787/health_glance-2015-en (accessed on 15 February 2022).
- OECD. OECD. Fiscal Sustainability of Health Systems: Bridging Health and Finance Perspectives, OECD Publishing, Paris. 2015. Available online: https://doi.org/10.1787/9789264233386-en (accessed on 15 February 2022).
- Bai, G.; Zare, H. Hospital Cost Structure and the Implications on Cost Management During COVID-19. J. Gen. Intern. Med. 2020, 9, 2807–2809. [Google Scholar] [CrossRef]
- Olkiewicz, M. Elastyczne formy zatrudnienia pielęgniarek i położnych determinantem jakości kapitału ludzkiego szpitali (Flexible forms of employment of nurses and midwives as a determinant of the quality of human capital in hospitals.). Probl. Profesjologii 2018, 2, 149–161. [Google Scholar]
- Wielicka-Gańczarczyk, K. Restrukturyzacja szpitala publicznego–studium przypadku (Restructuring of a public hospital–a case study.) Organizacja i Zarządzanie. Zeszyty Naukowe Politechniki Śląskiej 2018, 121, 557–569. [Google Scholar]
- Gu, Y.; Luo, Q. Optimization model for allocation of hospital beds under the trend of aging population. In Proceedings of the 2019 International Conference on Economic Management and Cultural Industry, Shenzhen, China, 15–17 November 2019; pp. 289–305. [Google Scholar] [CrossRef] [Green Version]
- Nguyen, J. A simple method to optimize hospital beds capacity. Int. J. Med. Inform. 2005, 74, 39–49. [Google Scholar] [CrossRef]
- Furmankiewicz, M.; Sołtysik-Piorunkiewicz, A.; Ziuziański, P. Artificial intelligence and multi-agent software for e-health knowledge management system. Inform. Ekon. 2014, 2, 51–63. [Google Scholar] [CrossRef] [Green Version]
- Matos, J.; Pereira, P. Modeling decisions for hospital bed management. In Proceedings of the HEALTHINF 2011—International Conference on Health Informatics, Rome, Italy, 26–29 January 2011; Volume 1, pp. 504–507. [Google Scholar]
- Pecoraro, F.; Luzi, D.; Clemente, F. The efficiency in the ordinary hospital bed management: A comparative analysis in four European countries before the COVID-19 outbreak. PLoS ONE 2021, 16, e0248867. [Google Scholar] [CrossRef]
- Pecoraro, F.; Clemente, F.; Luzi, D. The efficiency in the ordinary hospital bed management in Italy: An in-depth analysis of intensive care unit in the areas affected by COVID-19 before the outbreak. PLoS ONE 2020, 15, e0239249. [Google Scholar] [CrossRef] [PubMed]
- Rhodes, A.; Ferdinande, P.; Flaatten, H.; Guidet, B.; Metnitz, P.G.; Moreno, R.P. The variability of critical care bed numbers in Europe. Intensive Care Med. 2020, 38, 1647–1653. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sielska, A. Determinants of hospital inefficiency. The case of Polish county hospitals. PLoS ONE 2021, 16, e0256267, Erratum in: PLoS ONE 2021, 16, e0260461. [Google Scholar] [CrossRef] [PubMed]
- Sielska, A. Costs of polish county hospitals—A behavioral panel function. PLoS ONE 2022, 17, e0262646. [Google Scholar] [CrossRef] [PubMed]
- Boyle, P. Global public health–challenges and leadership. J. Health Inequalities 2018, 4, 55–61. [Google Scholar] [CrossRef]






| Clinic | Number of Beds | % of Beds |
|---|---|---|
| Anesthesiology and Intensive Care | 8 | 1.08% |
| Clinical Oncology | 25 | 3.36% |
| General and Oncological Surgery | 50 | 6.73% |
| Maxillofacial Surgery | 17 | 2.29% |
| Gastroenterology and Hepatology | 43 | 5.79% |
| Dermatology | 24 | 3.23% |
| Gynecology and Obstetrics | 86 | 11.57% |
| Oncological Gynecology | 35 | 4.71% |
| Hepatology | 24 | 3.23% |
| Nephrology | 18 | 2.42% |
| Ophthalmology | 35 | 4.71% |
| Otolaryngology | 38 | 5.11% |
| General Psychiatry | 30 | 4.04% |
| Radiotherapy | 50 | 6.73% |
| Urology | 42 | 5.65% |
| Neurology | 23 | 3.10% |
| Newborns with Intensive Care Unit | 40 | 5.38% |
| Pulmonology with Allergology * | 30 | 4.04% |
| Pulmonology and Chemotherapy * | 26 | 3.50% |
| Thoracic Surgery * | 27 | 3.63% |
| Tuberculosis and Lung Disease * | 68 | 9.15% |
| Anesthesiology and Intensive Care Unit * | 4 | 0.54% |
| Voivodeship | Years | ||||
|---|---|---|---|---|---|
| 2005 | 2010 | 2015 | 2018 | 2005/2018 | |
| Lower Silesia | 48.98 | 48.42 | 51.10 | 50.53 | +1.55 |
| Kuyavian-Pomeranian | 43.59 | 42.97 | 47.20 | 46.16 | +2.57 |
| Lubelskie | 50.80 | 51.82 | 52.84 | 51.89 | +1.09 |
| Lubuskie | 42.90 | 40.96 | 43.24 | 42.18 | −0.72 |
| Lodzkie | 53.20 | 53.23 | 52.07 | 50.79 | −2.41 |
| Lesser Poland | 42.56 | 42.78 | 44.06 | 43.68 | +1.12 |
| Masovian | 45.59 | 45.92 | 48.47 | 47.69 | +2.10 |
| Opolskie | 39.76 | 43.13 | 46.22 | 44.78 | +5.02 |
| Podkarpackie | 42.27 | 44.91 | 48.17 | 46.66 | +4.39 |
| Podlaskie | 50.92 | 49.61 | 49.91 | 49.83 | −1.09 |
| Pomeranian | 38.89 | 38.27 | 41.19 | 39.00 | +0.11 |
| Silesian | 57.12 | 56.07 | 55.85 | 54.46 | −2.66 |
| Świętokrzyskie | 44.96 | 50.25 | 50.22 | 46.08 | +1.12 |
| Warmian-Masurian | 42.24 | 41.17 | 46.32 | 44.86 | +2.62 |
| Greater Poland | 46.55 | 45.36 | 45.34 | 43.11 | −3.44 |
| West Pomeranian | 46.23 | 45.17 | 48.34 | 46.10 | −0.13 |
| Clinic | Analyzed Hospital | Poland |
|---|---|---|
| Anesthesiology and Intensive Care | 60.8% | 68.9% |
| Clinical Oncology | 96.9% | 71.4% |
| General and Oncological Surgery | 71.7% | no data |
| Maxillofacial Surgery | 83.9% | 46.9% |
| Gastroenterology and Hepatology | 78.2% | no data |
| Dermatology | 80.1% | 63.7% |
| Gynecology and Obstetrics | 90.6% | 58.0% |
| Oncological Gynecology | 53.8% | no data |
| Hepatology | 90.7% | 89.2% |
| Nephrology | 70.8% | 75.5% |
| Ophthalmology | 65.8% | 43.0% |
| Otolaryngology | 96.0% | 52.3% |
| General Psychiatry | 122.8% | 92.7% |
| Radiotherapy | 68.7% | no data |
| Urology | 58.3% | 63.1% |
| Neurology | 49.3% | 76.0% |
| Newborns with Intensive Care Unit | 68.0% | 50.2% |
| Pulmonology with Allergology * | 67.3% | no data |
| Pulmonology and Chemotherapy * | 73.1% | no data |
| Thoracic surgery * | 60.9% | no data |
| Tuberculosis and Lung Disease * | 65.6% | 70.9% |
| Anesthesiology and Intensive Care Unit * | 49.3% | 68.9% |
| Clinic | Hospital | Region | Poland |
|---|---|---|---|
| Anesthesiology and Intensive Care | 11.1 | 11.7 | 8.5 |
| Clinical Oncology | 3.6 | 4.0 | 4.3 |
| General and Oncological Surgery | 6.0 | no data | no data |
| Maxillofacial Surgery | 3.4 | 3.4 | 3.6 |
| Gastroenterology and Hepatology | 3.7 | no data | no data |
| Dermatology | 8.3 | 8.0 | 6.1 |
| Gynecology and Obstetrics | 4.6 | 3.3 | 3.5 |
| Oncological Gynecology | 3.9 | no data | no data |
| Hepatology | 12.1 | 6.8 | 6.2 |
| Nephrology | 5.2 | 9.0 | 6.0 |
| Ophthalmology | 1.6 | 1.5 | 1.9 |
| Otolaryngology | 3.1 | 3.0 | 3.0 |
| General Psychiatry | 36.6 | 28.2 | 28.0 |
| Radiotherapy | 14.9 | no data | no data |
| Urology | 5.3 | 3.6 | 3.3 |
| Neurology | 4.1 | 6.0 | 6.8 |
| Newborns | 5.9 | 4.0 | 4.5 |
| Pulmonology with Allergology * | 6.6 | no data | no data |
| Pulmonology and Chemotherapy * | 5.6 | no data | no data |
| Thoracic Surgery * | 7.1 | no data | no data |
| Tuberculosis and Lung Disease * | 10.1 | 9.7 | 8.3 |
| Anesthesiology and Intensive Care * | 11.0 | 11.7 | 8.5 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Porada, S.; Sygit, K.; Hejda, G.; Nagórska, M. Optimization of the Use of Hospital Beds as an Example of Improving the Functioning of Hospitals in Poland on the Basis of the Provincial Clinical Hospital No. 1 in Rzeszow. Int. J. Environ. Res. Public Health 2022, 19, 5349. https://doi.org/10.3390/ijerph19095349
Porada S, Sygit K, Hejda G, Nagórska M. Optimization of the Use of Hospital Beds as an Example of Improving the Functioning of Hospitals in Poland on the Basis of the Provincial Clinical Hospital No. 1 in Rzeszow. International Journal of Environmental Research and Public Health. 2022; 19(9):5349. https://doi.org/10.3390/ijerph19095349
Chicago/Turabian StylePorada, Sławomir, Katarzyna Sygit, Grażyna Hejda, and Małgorzata Nagórska. 2022. "Optimization of the Use of Hospital Beds as an Example of Improving the Functioning of Hospitals in Poland on the Basis of the Provincial Clinical Hospital No. 1 in Rzeszow" International Journal of Environmental Research and Public Health 19, no. 9: 5349. https://doi.org/10.3390/ijerph19095349
APA StylePorada, S., Sygit, K., Hejda, G., & Nagórska, M. (2022). Optimization of the Use of Hospital Beds as an Example of Improving the Functioning of Hospitals in Poland on the Basis of the Provincial Clinical Hospital No. 1 in Rzeszow. International Journal of Environmental Research and Public Health, 19(9), 5349. https://doi.org/10.3390/ijerph19095349