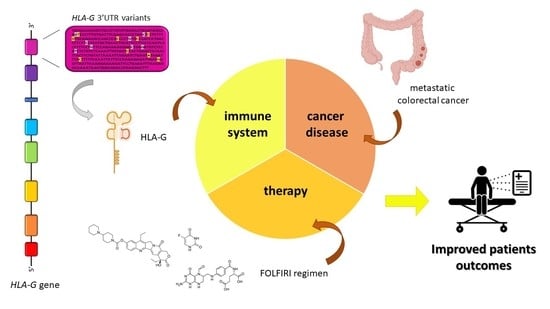
Association of HLA-G 3′UTR Polymorphisms with Response to First-Line FOLFIRI Treatment in Metastatic Colorectal Cancer
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patients Clinical Data and Study Design
2.2. HLA-G Genetic Analyses
2.3. Plasma sHLA-G Analysis
2.4. Statistical Analysis
3. Results
3.1. Patients’ Clinical Data
3.2. HLA-G Genetic Analyses
3.3. Effect of HLA-G 3′UTR Genetic Characteristics on Tumor Response
3.4. Plasma sHLA-G Analysis
3.5. Effect of HLA-G 3′UTR Genetic Characteristics on Survival Outcomes
3.6. Subgroup Survival Analysis: Effect of HLA-G 3′UTR Genetic Characteristics in All Responder Patients
4. Discussion and Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Dyba, T.; Randi, G.; Bray, F.; Martos, C.; Giusti, F.; Nicholson, N.; Gavin, A.; Flego, M.; Neamtiu, L.; Dimitrova, N.; et al. The European Cancer Burden in 2020: Incidence and Mortality Estimates for 40 Countries and 25 Major Cancers. Eur. J. Cancer Oxf. Engl. 1990 2021, 157, 308–347. [Google Scholar] [CrossRef] [PubMed]
- Salvatore, L.; Aprile, G.; Arnoldi, E.; Aschele, C.; Carnaghi, C.; Cosimelli, M.; Maiello, E.; Normanno, N.; Sciallero, S.; Valvo, F.; et al. Management of Metastatic Colorectal Cancer Patients: Guidelines of the Italian Medical Oncology Association (AIOM). ESMO Open 2017, 2, e000147. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van Cutsem, E.; Cervantes, A.; Adam, R.; Sobrero, A.; Van Krieken, J.H.; Aderka, D.; Aranda Aguilar, E.; Bardelli, A.; Benson, A.; Bodoky, G.; et al. ESMO Consensus Guidelines for the Management of Patients with Metastatic Colorectal Cancer. Ann. Oncol. Off. J. Eur. Soc. Med. Oncol. 2016, 27, 1386–1422. [Google Scholar] [CrossRef] [PubMed]
- Vento, S.; Cainelli, F. Infections in Patients with Cancer Undergoing Chemotherapy: Aetiology, Prevention, and Treatment. Lancet Oncol. 2003, 4, 595–604. [Google Scholar] [CrossRef]
- Li, X. The Inducers of Immunogenic Cell Death for Tumor Immunotherapy. Tumori 2018, 104, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Pusuluri, A.; Krishnan, V.; Wu, D.; Shields, C.W.; Wang, L.W.; Mitragotri, S. Role of Synergy and Immunostimulation in Design of Chemotherapy Combinations: An Analysis of Doxorubicin and Camptothecin. Bioeng. Transl. Med. 2019, 4, e10129. [Google Scholar] [CrossRef]
- Re, V.D.; Caggiari, L.; Zorzi, M.D.; Talamini, R.; Racanelli, V.; Andrea, M.D.; Buonadonna, A.; Zagonel, V.; Cecchin, E.; Innocenti, F.; et al. Genetic Diversity of the KIR/HLA System and Outcome of Patients with Metastatic Colorectal Cancer Treated with Chemotherapy. PLoS ONE 2014, 9, e84940. [Google Scholar] [CrossRef]
- Zhou, J.; Wang, G.; Chen, Y.; Wang, H.; Hua, Y.; Cai, Z. Immunogenic Cell Death in Cancer Therapy: Present and Emerging Inducers. J. Cell. Mol. Med. 2019, 23, 4854–4865. [Google Scholar] [CrossRef]
- Huyghe, N.; Benidovskaya, E.; Stevens, P.; Van den Eynde, M. Biomarkers of Response and Resistance to Immunotherapy in Microsatellite Stable Colorectal Cancer: Toward a New Personalized Medicine. Cancers 2022, 14, 2241. [Google Scholar] [CrossRef]
- Angell, H.K.; Bruni, D.; Barrett, J.C.; Herbst, R.; Galon, J. The Immunoscore: Colon Cancer and Beyond. Clin. Cancer Res. Off. J. Am. Assoc. Cancer Res. 2020, 26, 332–339. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pagès, F.; Mlecnik, B.; Marliot, F.; Bindea, G.; Ou, F.-S.; Bifulco, C.; Lugli, A.; Zlobec, I.; Rau, T.T.; Berger, M.D.; et al. International Validation of the Consensus Immunoscore for the Classification of Colon Cancer: A Prognostic and Accuracy Study. Lancet 2018, 391, 2128–2139. [Google Scholar] [CrossRef] [PubMed]
- Galon, J.; Hermitte, F.; Mlecnik, B.; Marliot, F.; Bifulco, C.B.; Lugli, A.; Nagtegaal, I.D.; Hartmann, A.; Van Den Eynde, M.; Roehrl, M.H.A.; et al. Immunoscore Clinical Utility to Identify Good Prognostic Colon Cancer Stage II Patients with High-Risk Clinico-Pathological Features for Whom Adjuvant Treatment May Be Avoided. J. Clin. Oncol. 2019, 37, 487. [Google Scholar] [CrossRef]
- Zhao, Y.; Ge, X.; He, J.; Cheng, Y.; Wang, Z.; Wang, J.; Sun, L. The Prognostic Value of Tumor-Infiltrating Lymphocytes in Colorectal Cancer Differs by Anatomical Subsite: A Systematic Review and Meta-Analysis. World J. Surg. Oncol. 2019, 17, 85. [Google Scholar] [CrossRef] [Green Version]
- Scarabel, L.; Bignucolo, A.; Toffoli, G.; Cecchin, E.; De Mattia, E. Pharmacogenetics Role of Genetic Variants in Immune-Related Factors: A Systematic Review Focusing on MCRC. Pharmaceutics 2022, 14, 2468. [Google Scholar] [CrossRef] [PubMed]
- Lin, A.; Yan, W.-H. Human Leukocyte Antigen-G (HLA-G) Expression in Cancers: Roles in Immune Evasion, Metastasis and Target for Therapy. Mol. Med. Camb. Mass. 2015, 21, 782–791. [Google Scholar] [CrossRef]
- Kirana, C.; Ruszkiewicz, A.; Stubbs, R.S.; Hardingham, J.E.; Hewett, P.J.; Maddern, G.J.; Hauben, E. Soluble HLA-G Is a Differential Prognostic Marker in Sequential Colorectal Cancer Disease Stages. Int. J. Cancer 2017, 140, 2577–2586. [Google Scholar] [CrossRef] [Green Version]
- Samadi, R.; Mojarad, E.N.; Molaei, M.; Kazerouni, F.; Aghdaei, H.A.; Navidinia, M.; Rahimipour, A. Clinical Value of Human Leucocyte Antigen G (HLA-G) Expression in the Prognosis of Colorectal Cancer. Int. J. Cancer Manag. 2017, 10, e9346. [Google Scholar] [CrossRef] [Green Version]
- Zhang, R.-L.; Zhang, X.; Dong, S.-S.; Hu, B.; Han, Q.-Y.; Zhang, J.-G.; Zhou, W.-J.; Lin, A.; Yan, W.-H.; Zhang, R.-L.; et al. Predictive Value of Different Proportion of Lesion HLA-G Expression in Colorectal Cancer. Oncotarget 2017, 8, 107441–107451. [Google Scholar] [CrossRef] [Green Version]
- Guo, Z.-Y.; Lv, Y.-G.; Wang, L.; Shi, S.-J.; Yang, F.; Zheng, G.-X.; Wen, W.-H.; Yang, A.-G. Predictive Value of HLA-G and HLA-E in the Prognosis of Colorectal Cancer Patients. Cell. Immunol. 2015, 293, 10–16. [Google Scholar] [CrossRef]
- Li, J.-B.; Ruan, Y.-Y.; Hu, B.; Dong, S.-S.; Bi, T.-N.; Lin, A.; Yan, W.-H. Importance of the Plasma Soluble HLA-G Levels for Prognostic Stratification with Traditional Prognosticators in Colorectal Cancer. Oncotarget 2017, 8, 48854–48862. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Scarabel, L.; Garziera, M.; Fortuna, S.; Asaro, F.; Toffoli, G.; Geremia, S. Soluble HLA-G Expression Levels and HLA-G/Irinotecan Association in Metastatic Colorectal Cancer Treated with Irinotecan-Based Strategy. Sci. Rep. 2020, 10, 8773. [Google Scholar] [CrossRef] [PubMed]
- Garziera, M.; Bidoli, E.; Cecchin, E.; Mini, E.; Nobili, S.; Lonardi, S.; Buonadonna, A.; Errante, D.; Pella, N.; D’Andrea, M.; et al. HLA-G 3′UTR Polymorphisms Impact the Prognosis of Stage II-III CRC Patients in Fluoropyrimidine-Based Treatment. PLoS ONE 2015, 10, e0144000. [Google Scholar] [CrossRef] [PubMed]
- Garziera, M.; Virdone, S.; De Mattia, E.; Scarabel, L.; Cecchin, E.; Polesel, J.; D’Andrea, M.; Pella, N.; Buonadonna, A.; Favaretto, A.; et al. HLA-G 3′UTR Polymorphisms Predict Drug-Induced G3-4 Toxicity Related to Folinic Acid/5-Fluorouracil/Oxaliplatin (FOLFOX4) Chemotherapy in Non-Metastatic Colorectal Cancer. Int. J. Mol. Sci. 2017, 18, 1366. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Toffoli, G.; Cecchin, E.; Corona, G.; Russo, A.; Buonadonna, A.; D’Andrea, M.; Pasetto, L.M.; Pessa, S.; Errante, D.; De Pangher, V.; et al. The Role of UGT1A1*28 Polymorphism in the Pharmacodynamics and Pharmacokinetics of Irinotecan in Patients with Metastatic Colorectal Cancer. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2006, 24, 3061–3068. [Google Scholar] [CrossRef]
- Tournigand, C.; André, T.; Achille, E.; Lledo, G.; Flesh, M.; Mery-Mignard, D.; Quinaux, E.; Couteau, C.; Buyse, M.; Ganem, G.; et al. FOLFIRI Followed by FOLFOX6 or the Reverse Sequence in Advanced Colorectal Cancer: A Randomized GERCOR Study. J. Clin. Oncol. 2004, 22, 229–237. [Google Scholar] [CrossRef] [Green Version]
- Miller, A.B.; Hoogstraten, B.; Staquet, M.; Winkler, A. Reporting Results of Cancer Treatment. Cancer 1981, 47, 207–214. [Google Scholar] [CrossRef]
- Castelli, E.C.; Mendes-Junior, C.T.; Deghaide, N.H.S.; de Albuquerque, R.S.; Muniz, Y.C.N.; Simões, R.T.; Carosella, E.D.; Moreau, P.; Donadi, E.A. The Genetic Structure of 3′untranslated Region of the HLA-G Gene: Polymorphisms and Haplotypes. Genes Immun. 2010, 11, 134–141. [Google Scholar] [CrossRef] [Green Version]
- Garziera, M.; Catamo, E.; Crovella, S.; Montico, M.; Cecchin, E.; Lonardi, S.; Mini, E.; Nobili, S.; Romanato, L.; Toffoli, G. Association of the HLA-G 3′UTR Polymorphisms with Colorectal Cancer in Italy: A First Insight. Int. J. Immunogenet. 2016, 43, 32–39. [Google Scholar] [CrossRef]
- Stephens, M.; Smith, N.J.; Donnelly, P. A New Statistical Method for Haplotype Reconstruction from Population Data. Am. J. Hum. Genet. 2001, 68, 978–989. [Google Scholar] [CrossRef]
- Stephens, M.; Donnelly, P. A Comparison of Bayesian Methods for Haplotype Reconstruction from Population Genotype Data. Am. J. Hum. Genet. 2003, 73, 1162–1169. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kalbfleisch, J.; Prentice, R. The Statistical Analysis of Failure Time Data, 2nd ed.; John Wiley & Sons: Hoboken, NJ, USA, 2011; Volume 77. [Google Scholar]
- Fine, J.P.; Gray, R.J. A Proportional Hazards Model for the Subdistribution of a Competing Risk. J. Am. Stat. Assoc. 1999, 94, 496–509. [Google Scholar] [CrossRef]
- Gray, R.J. A Class of $K$-Sample Tests for Comparing the Cumulative Incidence of a Competing Risk. Ann. Stat. 1988, 16, 1141–1154. [Google Scholar] [CrossRef]
- Benjamini, Y.; Hochberg, Y. Controlling the False Discovery Rate: A Practical and Powerful Approach to Multiple Testing. J. R. Stat. Soc. Ser. B Methodol. 1995, 57, 289–300. [Google Scholar] [CrossRef]
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global Cancer Statistics 2018: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA. Cancer J. Clin. 2018, 68, 394–424. [Google Scholar] [CrossRef] [Green Version]
- Malvezzi, M.; Carioli, G.; Bertuccio, P.; Boffetta, P.; Levi, F.; La Vecchia, C.; Negri, E. European Cancer Mortality Predictions for the Year 2018 with Focus on Colorectal Cancer. Ann. Oncol. Off. J. Eur. Soc. Med. Oncol. 2018, 29, 1016–1022. [Google Scholar] [CrossRef]
- Sabbagh, A.; Luisi, P.; Castelli, E.C.; Gineau, L.; Courtin, D.; Milet, J.; Massaro, J.D.; Laayouni, H.; Moreau, P.; Donadi, E.A.; et al. Worldwide Genetic Variation at the 3′ Untranslated Region of the HLA-G Gene: Balancing Selection Influencing Genetic Diversity. Genes Immun. 2014, 15, 95–106. [Google Scholar] [CrossRef] [Green Version]
- Galluzzi, L.; Buqué, A.; Kepp, O.; Zitvogel, L.; Kroemer, G. Immunological Effects of Conventional Chemotherapy and Targeted Anticancer Agents. Cancer Cell 2015, 28, 690–714. [Google Scholar] [CrossRef] [Green Version]
- Rousseau, P.; Le Discorde, M.; Mouillot, G.; Marcou, C.; Carosella, E.D.; Moreau, P. The 14 Bp Deletion-Insertion Polymorphism in the 3′ UT Region of the HLA-G Gene Influences HLA-G MRNA Stability. Hum. Immunol. 2003, 64, 1005–1010. [Google Scholar] [CrossRef]
- Manaster, I.; Goldman-Wohl, D.; Greenfield, C.; Nachmani, D.; Tsukerman, P.; Hamani, Y.; Yagel, S.; Mandelboim, O. MiRNA-Mediated Control of HLA-G Expression and Function. PLoS ONE 2012, 7, e33395. [Google Scholar] [CrossRef] [Green Version]
- Castelli, E.C.; Moreau, P.; Oya e Chiromatzo, A.; Mendes-Junior, C.T.; Veiga-Castelli, L.C.; Yaghi, L.; Giuliatti, S.; Carosella, E.D.; Donadi, E.A. In Silico Analysis of MicroRNAS Targeting the HLA-G 3′ Untranslated Region Alleles and Haplotypes. Hum. Immunol. 2009, 70, 1020–1025. [Google Scholar] [CrossRef] [PubMed]
- Veit, T.D.; Chies, J.A.B. Tolerance versus Immune Response--MicroRNAs as Important Elements in the Regulation of the HLA-G Gene Expression. Transpl. Immunol. 2009, 20, 229–231. [Google Scholar] [CrossRef] [PubMed]
- Castelli, E.C.; Veiga-Castelli, L.C.; Yaghi, L.; Moreau, P.; Donadi, E.A. Transcriptional and Posttranscriptional Regulations of the HLA-G Gene. Available online: https://www.hindawi.com/journals/jir/2014/734068/ (accessed on 28 January 2019).
- Chen, X.-Y.; Yan, W.-H.; Lin, A.; Xu, H.-H.; Zhang, J.-G.; Wang, X.-X. The 14 Bp Deletion Polymorphisms in HLA-G Gene Play an Important Role in the Expression of Soluble HLA-G in Plasma. Tissue Antigens 2008, 72, 335–341. [Google Scholar] [CrossRef] [PubMed]
- Hviid, T.V.F.; Hylenius, S.; Rørbye, C.; Nielsen, L.G. HLA-G Allelic Variants Are Associated with Differences in the HLA-G MRNA Isoform Profile and HLA-G MRNA Levels. Immunogenetics 2003, 55, 63–79. [Google Scholar] [CrossRef]
- Rouas-Freiss, N.; Moreau, P.; LeMaoult, J.; Carosella, E.D. The Dual Role of HLA-G in Cancer. J. Immunol. Res. 2014, 2014, 359748. [Google Scholar] [CrossRef] [Green Version]
- Marques, D.; Ferreira-Costa, L.R.; Ferreira-Costa, L.L.; da Silva Correa, R.; Borges, A.M.P.; Ito, F.R.; de Oliveira Ramos, C.C.; Bortolin, R.H.; Luchessi, A.D.; Ribeiro-dos-Santos, Â.; et al. Association of Insertion-Deletions Polymorphisms with Colorectal Cancer Risk and Clinical Features. World J. Gastroenterol. 2017, 23, 6854–6867. [Google Scholar] [CrossRef]
- Zlobec, I.; Lugli, A. Prognostic and Predictive Factors in Colorectal Cancer. J. Clin. Pathol. 2008, 61, 561–569. [Google Scholar] [CrossRef]
- Yan, X.; Zhang, S.; Deng, Y.; Wang, P.; Hou, Q.; Xu, H. Prognostic Factors for Checkpoint Inhibitor Based Immunotherapy: An Update With New Evidences. Front. Pharmacol. 2018, 9, 1050. [Google Scholar] [CrossRef] [Green Version]
- Hiam-Galvez, K.J.; Allen, B.M.; Spitzer, M.H. Systemic Immunity in Cancer. Nat. Rev. Cancer 2021, 21, 345–359. [Google Scholar] [CrossRef]
- Kanterman, J.; Sade-Feldman, M.; Biton, M.; Ish-Shalom, E.; Lasry, A.; Goldshtein, A.; Hubert, A.; Baniyash, M. Adverse Immunoregulatory Effects of 5FU and CPT11 Chemotherapy on Myeloid-Derived Suppressor Cells and Colorectal Cancer Outcomes. Cancer Res. 2014, 74, 6022–6035. [Google Scholar] [CrossRef]
- Köstlin, N.; Ostermeir, A.-L.; Spring, B.; Schwarz, J.; Marmé, A.; Walter, C.B.; Poets, C.F.; Gille, C. HLA-G Promotes Myeloid-Derived Suppressor Cell Accumulation and Suppressive Activity during Human Pregnancy through Engagement of the Receptor ILT4. Eur. J. Immunol. 2017, 47, 374–384. [Google Scholar] [CrossRef] [PubMed]
- Morandi, F.; Airoldi, I. HLA-G and Other Immune Checkpoint Molecules as Targets for Novel Combined Immunotherapies. Int. J. Mol. Sci. 2022, 23, 2925. [Google Scholar] [CrossRef] [PubMed]




| Characteristic | n | (%) |
|---|---|---|
| Gender | ||
| Female | 87 | (35.1) |
| Male | 161 | (64.9) |
| Age (years) | ||
| <55 | 62 | (25.0) |
| 55–64 | 85 | (34.3) |
| 65–75 | 101 | (40.7) |
| Cancer site | ||
| Left colon | 99 | (39.9) |
| Right colon | 78 | (31.5) |
| Rectum | 71 | (28.6) |
| Stage at diagnosis | ||
| I–II | 25 | (10.1) |
| III | 65 | (26.2) |
| IV | 158 | (63.7) |
| Radical surgery | ||
| No | 50 | (20.2) |
| Yes | 198 | (79.8) |
| Adjuvant treatment | ||
| None | 161 | (64.9) |
| Chemotherapy | 54 | (21.8) |
| Radio-chemotherapy | 33 | (11.3) |
| Number of metastatic sites | ||
| 1 | 107 | (43.2) |
| ≥2 | 141 | (56.8) |
| Best clinical response | ||
| Complete response | 18 | (7.3) |
| Partial response | 84 | (33.9) |
| Stable disease | 66 | (26.6) |
| Progression | 68 | (27.4) |
| Not evaluated | 12 | (4.8) |
| Oncological outcome from treatment initiation | OS | PFS |
| 1 year | 77.1% | 70.9% |
| 2 years | 44.7% | 39.5% |
| 3 years | 24.5% | 19.9% |
| HLA-G 3′UTR Haplotypes | +296014-bp | +3003 T>C | +3010 C>G | +3027 C>A | +3035 C>T | +3142 G>C | +3187 A>G | +3196 C>G | Haplotype | Diplotype | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| n (%) | Het n (%) | Hom n (%) | |||||||||
| UTR-2 | Ins | T | C | C | C | G | A | G | 146 (29.5) | 109 (44.0) | 18 (7.3) |
| UTR-1 | Del | T | G | C | C | C | G | C | 140 (28.2) | 104 (41.9) | 18 (7.3) |
| UTR-3 | Del | T | C | C | C | G | A | C | 65 (13.1) | 53 (21.4) | 6 (2.4) |
| UTR-4 | Del | C | G | C | C | C | A | C | 65 (13.1) | 53 (21.4) | 6 (2.4) |
| UTR-7 | Ins | T | C | A | T | G | A | C | 32 (6.5) | 32 (12.9) | 0 (0.0) |
| UTR-5 | Ins | T | C | C | T | G | A | C | 25 (5.0) | 21 (8.5) | 2 (0.8) |
| UTR-6/-18 | Del | T | G | C | C | C | A | C | 21 (4.2) | 15 (6.0) | 2 (0.8) |
| UTR-13 | Del | T | C | C | T | G | A | C | 2 (0.4) | 2 (0.8) | 0 (0.0) |
| Alias | SNP rs | CR | CR + PR | ||||
|---|---|---|---|---|---|---|---|
| HR (95%CI) | p-Value | p-ValueBHb | HR (95%CI) | p-Value | p-ValueBHb | ||
| +2960 Del/Ins | rs371194629 | 0.29 (0.10–0.82) | 0.0192 | 0.0336 | 0.87 (0.65–1.15) | 0.3171 | 0.6702 |
| +3003 T > C | rs1707 | 1.33 (0.54–3.27) | 0.6109 | 0.6109 | 0.93 (0.64–1.35) | 0.7056 | 0.8538 |
| +3010 C > G | rs1710 | 4.58 (1.65–12.72) | 0.0035 | 0.0245 | 1.12 (0.85–1.47) | 0.4329 | 0.6702 |
| +3027 C > A | rs17179101 | - | - | - | 1.28 (0.68–2.39) | 0.4468 | 0.6702 |
| +3035 C > T | rs17179108 | - | - | - | 0.94 (0.64–1.39) | 0.7589 | 0.8538 |
| +3187 A > G | rs9380142 | 3.18 (1.25–8.08) | 0.0154 | 0.0336 | 1.20 (0.86–1.67) | 0.2880 | 0.6702 |
| +3196 C > G | rs1610696 | 0.48 (0.15–1.48) | 0.2020 | 0.2357 | 0.86 (0.62–1.19) | 0.3584 | 0.6702 |
| Haplotype | Patients | CR | CR + PR | ||||
| HR (95%CI) | p-value | p-valueBHb | HR (95%CI) | p-value | p-valueBHb | ||
| UTR-1 | |||||||
| 0 | 120 | Reference | Reference | ||||
| 1 copy | 99 | 2.09 (0.70–6.20) | 0.1855 | 0.2357 | 1.01 (0.67–1.53) | 0.9630 | 0.9630 |
| 2 copies | 17 | 10.59 (1.83–61.26) | 0.0084 | 0.0294 | 1.78 (0.84–3.76) | 0.1313 | 0.6702 |
| SNP | Overall Survival | Progression-Free Survival | ||||
|---|---|---|---|---|---|---|
| HR (95% CI) | p-Value | p-ValueBHb | HR (95% CI) | p-Value | p-ValueBHb | |
| +2960 Del/Ins | 0.94 (0.54–1.62) | 0.8147 | 0.8147 | 1.02 (0.66-1.47) | 0.9299 | 0.9299 |
| +3003 T>C | 0.77 (0.35–1.71) | 0.5199 | 0.6066 | 0.80 (0.43-1.50) | 0.4894 | 0.5710 |
| +3010 C>G | 1.49 (0.91–2.42) | 0.1104 | 0.2151 | 1.35 (0.91-1.99) | 0.1363 | 0.3103 |
| +3027 C>A | 1.74 (0.47–6.43) | 0.4066 | 0.5692 | 1.53 (0.59-4.00) | 0.3820 | 0.5348 |
| +3035 C>T | 2.37 (1.12–5.01) | 0.0245 | 0.1173 | 1.68 (0.93-3.04) | 0.0876 | 0.3180 |
| +3187 A>G | 1.95 (1.05–3.61) | 0.0335 | 0.1173 | 1.46 (0.91-2.33) | 0.1130 | 0.3180 |
| +3196 C>G | 0.59 (0.31–1.15) | 0.1229 | 0.2151 | 0.77 (0.46-1.29) | 0.3150 | 0.5348 |
| Haplotype | Overall survival | Progression-free survival | ||||
| HR (95% CI) | p-value | p-valueBHb | HR (95% CI) | p-value | p-valueBHb | |
| UTR-1 | ||||||
| 0 | Reference | Reference | ||||
| 1 copy | 1.66 (0.63–4.37) | 0.3027 | 0.4793 | 1.43 (0.70–2.90) | 0.3255 | 0.5557 |
| 2 copies | 4.16 (1.17–14.8) | 0.0280 | 0.1330 | 2.16 (0.81–5.80) | 0.1258 | 0.4780 |
| 1 + 2 copies | 2.10 (0.88–5.04) | 0.0964 | 0.3097 | 1.57 (0.81–3.05) | 0.1817 | 0.5557 |
| UTR-2 | ||||||
| 0 | Reference | Reference | ||||
| 1 copy | 0.63 (0.29–1.38) | 0.2436 | 0.4256 | 0.78 (0.42–1.45) | 0.4364 | 0.5557 |
| 2 copy | 0.29 (0.04–2.37) | 0.2464 | 0.4256 | 0.55 (0.12–2.49) | 0.4387 | 0.5557 |
| 1 + 2 copies | 0.58 (0.27–1.25) | 0.1653 | 0.3490 | 0.76 (0.41–1.38) | 0.3654 | 0.5557 |
| UTR-3 | ||||||
| 0 | Reference | Reference | ||||
| 1 copy | 0.21 (0.06–0.72) | 0.0130 | 0.0855 | 0.34 (0.14–0.83) | 0.0177 | 0.0841 |
| 2 copies | 0.56 (0.06–4.83) | 0.5940 | 0.7524 | 0.41 (0.05–3.28) | 0.4010 | 0.5557 |
| 1 + 2 copies | 0.25 (0.08-0.75) | 0.0135 | 0.0855 | 0.35 (0.15–0.80) | 0.0129 | 0.0817 |
| UTR-4 | ||||||
| 0 | Reference | Reference | ||||
| 1 copy | 1.12 (0.44–2.85) | 0.8066 | 0.9197 | 1.09 (0.54–2.23) | 0.8061 | 0.8509 |
| 2 copies | - | - | - | - | ||
| 1 + 2 copies | 0.90 (0.36–2.27) | 0.8229 | 0.9197 | 0.91 (0.45–1.86) | 0.8036 | 0.8509 |
| UTR-5 | ||||||
| 0 | Reference | Reference | ||||
| 1 copy | 1.86 (0.50–6.86) | 0.3547 | 0.5184 | 1.70 (0.60–4.83) | 0.3197 | 0.5557 |
| 2 copies | 6.19 (0.65–59.4) | 0.1141 | 0.3097 | 2.37 (0.28–19.94) | 0.4257 | 0.5557 |
| 1 + 2 copies | 2.33 (0.73–7.44) | 0.1535 | 0.3490 | 1.80 (0.70–4.65) | 0.2240 | 0.5557 |
| UTR-6 | ||||||
| 0 | Reference | Reference | ||||
| 1 copy | 12.95 (2.04–82.2) | 0.0066 | 0.0855 | 11.50 (3.60–36.7) | <0.0001 | 0.0002 |
| 2 copies | 0.91 (0.09–9.09) | 0.9324 | 0.9842 | 0.63 (0.08-5.37) | 0.6754 | 0.8020 |
| 1 + 2 copies | 3.16 (0.78–12.8) | 0.1075 | 0.3097 | 3.68 (1.41–9.63) | 0.0078 | 0.0741 |
| UTR-7 | ||||||
| 0 | Reference | Reference | ||||
| 1 copy | 1.74 (0.47–6.43) | 0.4066 | 0.5518 | 1.53 (0.59–4.00) | 0.3820 | 0.5557 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Scarabel, L.; Polesel, J.; De Mattia, E.; Buonadonna, A.; D'Andrea, M.R.; Cecchin, E.; Toffoli, G. Association of HLA-G 3′UTR Polymorphisms with Response to First-Line FOLFIRI Treatment in Metastatic Colorectal Cancer. Pharmaceutics 2022, 14, 2737. https://doi.org/10.3390/pharmaceutics14122737
Scarabel L, Polesel J, De Mattia E, Buonadonna A, D'Andrea MR, Cecchin E, Toffoli G. Association of HLA-G 3′UTR Polymorphisms with Response to First-Line FOLFIRI Treatment in Metastatic Colorectal Cancer. Pharmaceutics. 2022; 14(12):2737. https://doi.org/10.3390/pharmaceutics14122737
Chicago/Turabian StyleScarabel, Lucia, Jerry Polesel, Elena De Mattia, Angela Buonadonna, Mario Rosario D'Andrea, Erika Cecchin, and Giuseppe Toffoli. 2022. "Association of HLA-G 3′UTR Polymorphisms with Response to First-Line FOLFIRI Treatment in Metastatic Colorectal Cancer" Pharmaceutics 14, no. 12: 2737. https://doi.org/10.3390/pharmaceutics14122737
APA StyleScarabel, L., Polesel, J., De Mattia, E., Buonadonna, A., D'Andrea, M. R., Cecchin, E., & Toffoli, G. (2022). Association of HLA-G 3′UTR Polymorphisms with Response to First-Line FOLFIRI Treatment in Metastatic Colorectal Cancer. Pharmaceutics, 14(12), 2737. https://doi.org/10.3390/pharmaceutics14122737