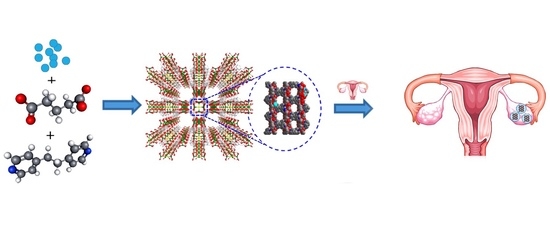
Therapeutic Application of Metal–Organic Frameworks Composed of Copper, Cobalt, and Zinc: Their Anticancer Activity and Mechanism
Abstract
:1. Introduction
2. Experimental Methods
2.1. Preparation of Cu-MOF 1, [Cu2(Glu)2(μ-bpa)]·3H2O
2.2. Preparation of Co-MOF 2, [Co2(Glu)2(μ-bpa)2]·4H2O
2.3. Preparation of Zn-MOF 3, [{Zn(H2O)(Glu)}2(μ-bpa)]
2.4. Instrumentation
2.5. Metal Ion Release Test
2.6. Metabolic Viability
2.7. Flow Cytometric Analysis for Cell Death
2.8. Statistical Analysis
3. Results and Discussion
3.1. Physical Characterizations of MOFs, 1–3
3.2. The Degradability of MOFs in Physiological Media
3.3. Effect of MOF on Cell Viability and Cytotoxicity
3.4. Cell Death Analysis
3.5. Summary
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2018, 68, 394–424. [Google Scholar] [CrossRef] [Green Version]
- Ibrahim, M.; Sabouni, R.; Husseini, G.A. Anti-cancer Drug Delivery Using Metal Organic Frameworks (MOFs). Curr. Med. Chem. 2017, 24, 193–214. [Google Scholar] [CrossRef] [PubMed]
- DeVita, V.T., Jr.; Chu, E. A history of cancer chemotherapy. Cancer Res. 2008, 68, 8643–8653. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Abazari, R.; Mahjoub, A.R.; Slawin, A.M.; Carpenter-Warren, C.L. Morphology- and size-controlled synthesis of a metal-organic framework under ultrasound irradiation: An efficient carrier for pH responsive release of anti-cancer drugs and their applicability for adsorption of amoxicillin from aqueous solution. Ultrason. Sonochem. 2018, 42, 594–608. [Google Scholar] [CrossRef] [Green Version]
- Yang, Z.; Guo, F.; Albers, A.E.; Sehouli, J.; Kaufmann, A.M. Disulfiram modulates ROS accumulation and overcomes synergistically cisplatin resistance in breast cancer cell lines. Biomed. Pharmacother. 2019, 113, 108727. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.N.; Han, I.; Choi, S.A. Metal organic frameworks compound and anticancer agents with that. KR Patent No. 1022642410000, 2021. [Google Scholar]
- Lattuada, E.; Leo, M.; Caprara, D.; Salvatori, L.; Stoppacciaro, A.; Sciortino, F.; Filetici, P. DNA-GEL, Novel Nanomaterial for Biomedical Applications and Delivery of Bioactive Molecules. Front. Pharmacol. 2020, 11, 01345. [Google Scholar] [CrossRef] [PubMed]
- Liu, W.; Zhong, Y.; Wang, X.; Zhuang, C.; Chen, J.; Liu, D.; Xiao, W.; Pan, Y.; Huang, J.; Liu, J. A porous Cu(II)-based metal-organic framework carrier for pH-controlled anticancer drug delivery. Inorg. Chem. Commun. 2020, 111, 107675. [Google Scholar] [CrossRef]
- Kosower, N.S.; Kosower, E.M. The Glutathione Status of Cells. Int. Rev. Cytol. 1978, 54, 109–160. [Google Scholar] [PubMed]
- Hall, M.D.; Hambley, T.W. Platinum(IV) Antitumour Compounds: Their Bioinorganic Chemistry. Coord. Chem. Rev. 2002, 232, 49–67. [Google Scholar] [CrossRef]
- Cheng, L.; Wang, C.; Feng, L.; Yang, K.; Liu, Z. Functional Nanomaterials for Phototherapies of Cancer. Chem. Rev. 2014, 114, 10869–10939. [Google Scholar] [CrossRef]
- Liang, C.; Xu, L.; Song, G.; Liu, Z. Emerging Nanomedicine Approaches Fighting Tumor Metastasis: Animal Models, Metastasis-Targeted Drug Delivery, Phototherapy, and Immunotherapy. Chem. Soc. Rev. 2016, 45, 6250–6269. [Google Scholar] [CrossRef]
- Zhang, W.; Lu, J.; Gao, X.; Li, P.; Zhang, W.; Ma, Y.; Wang, H.; Tang, B. Enhanced Photodynamic Therapy by Reduced Levels of Intracellular Glutathione Obtained By Employing a Nano-MOF with CuII as the Active Center. Angew. Chem. 2018, 130, 4985–4990. [Google Scholar] [CrossRef]
- Cui, Y.; Yue, Y.; Qian, G.; Chen, B. Luminescent Functional Metal-Organic Frameworks. Chem. Rev. 2012, 112, 1126–1162. [Google Scholar] [CrossRef]
- Wang, C.; Zhang, T.; Lin, W. Rational Synthesis of Noncentrosymmetric Metal-Organic Frameworks for Second-Order Nonlinear Optics. Chem. Rev. 2012, 112, 1084–1104. [Google Scholar] [CrossRef]
- Park, J.; Jiang, Q.; Feng, D.; Mao, L.; Zhou, H.-C. Size-Controlled Synthesis of Porphyrinic Metal-Organic Framework and Functionalization for Targeted Photodynamic Therapy. J. Am. Chem. Soc. 2016, 138, 3518–3525. [Google Scholar] [CrossRef] [PubMed]
- Lu, K.; He, C.; Lin, W. Nanoscale Metal-Organic Framework for Highly Effective Photodynamic Therapy of Resistant Head and Neck Cancer. J. Am. Chem. Soc. 2014, 136, 16712–16715. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, Y.; Wu, W.; Liu, J.; Manghnani, P.N.; Hu, F.; Ma, D.; Teh, C.; Wang, B.; Liu, B. Cancer-Cell-Activated Photodynamic Therapy Assisted by Cu(II)-Based Metal−Organic Framework. ACS Nano 2019, 13, 6879–6890. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Lu, A.; Long, M.; Cui, L.; Chen, Z.; Zhu, L. Nitroimidazole derivative incorporated liposomes for hypoxia-triggered drug delivery and enhanced therapeutic efficacy in patient-derived tumor xenografts. Acta Biomater. 2019, 83, 334–348. [Google Scholar] [CrossRef] [PubMed]
- Mousavikhamene, Z.; Abdekhodaie, M.J.; Ahmadieh, H. Facilitation of transscleral drug delivery by drug loaded magnetic polymeric particles. Mater. Sci. Eng. C 2017, 79, 812–820. [Google Scholar] [CrossRef] [PubMed]
- Leong, J.; Chin, W.; Ke, X.; Gao, S.; Kong, H.; Hedrick, J.L.; Yang, Y.Y. Disease-directed design of biodegradable polymers: Reactive oxygen species and pH-responsive micellar nanoparticles for anticancer drug delivery. Nanomedicine 2018, 14, 2666–2677. [Google Scholar] [CrossRef] [PubMed]
- Cai, H.; Huang, Y.-L.; Li, D. Biological Metal–Organic Frameworks: Structures, Host–Guest Chemistry and Bio-Applications. Coord. Chem. Rev. 2019, 378, 207–221. [Google Scholar] [CrossRef]
- An, H.; Li, M.; Gao, J.; Zhang, Z.; Ma, S.; Chen, Y. Incorporation of Biomolecules in Metal-Organic Frameworks for Advanced Applications. Coord. Chem. Rev. 2019, 384, 90–106. [Google Scholar] [CrossRef]
- Abánades Lázaro, I.; Forgan, R.S. Application of Zirconium MOFs in Drug Delivery and Biomedicine. Coord. Chem. Rev. 2019, 380, 230–259. [Google Scholar] [CrossRef] [Green Version]
- Zhang, Z.; Sang, W.; Xie, L.; Dai, Y. Metal-Organic Frameworks for Multimodal Bioimaging and Synergistic Cancer Chemotherapy. Coord. Chem. Rev. 2019, 399, 213022. [Google Scholar] [CrossRef]
- Wang, H.-S. Metal–Organic Frameworks for Biosensing and Bioimaging Applications. Coord. Chem. Rev. 2017, 349, 139–155. [Google Scholar] [CrossRef]
- Horcajada, P.; Serre, C.; Vallet-Regí, M.; Sebban, M.; Taulelle, F.; Férey, G. Metal–organic frameworks as efficient materials for drug delivery. Angew.Chem. Int. Ed. 2006, 118, 6120–6124. [Google Scholar] [CrossRef]
- Aguilera-Sigalat, J.; Bradshaw, D. Synthesis and Applications of Metal-Organic Framework–Quantum Dot (QD@MOF) Composites. Coord. Chem. Rev. 2016, 307, 267–291. [Google Scholar] [CrossRef] [Green Version]
- Yang, J.-C.; Chen, Y.; Li, Y.-H.; Yin, X.-B. Magnetic Resonance Imaging-Guided Multi-Drug Chemotherapy and Photothermal Synergistic Therapy with pH and NIR-Stimulation Release. ACS Appl. Mater. Interfaces 2017, 9, 22278–22288. [Google Scholar] [CrossRef]
- Liu, W.; Wang, Y.-M.; Li, Y.-H.; Cai, S.-J.; Yin, X.-B.; He, X.-W.; Zhang, Y.K. Fluorescent Imaging-Guided Chemotherapy-and-Photodynamic Dual Therapy with Nanoscale Porphyrin Metal-Organic Framework. Small 2017, 13, 1603459. [Google Scholar] [CrossRef]
- Yang, J.; Yang, Y.W. Metal-Organic Frameworks for Biomedical Applications. Small 2020, 16, e1906846. [Google Scholar] [CrossRef] [PubMed]
- Giliopoulos, D.; Zamboulis, A.; Giannakoudakis, D.; Bikiaris, D.; Triantafyllidis, K. Polymer/Metal Organic Framework (MOF) Nanocomposites for Biomedical Applications. Molecules 2020, 25, 185. [Google Scholar] [CrossRef] [Green Version]
- Chedid, G.; Yassin, A. Recent Trends in Covalent and Metal Organic Frameworks for Biomedical Applications. Nanomaterials 2018, 8, 916. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lu, K.; Aung, T.; Guo, N.; Weichselbaum, R.; Lin, W. Nanoscale Metal-Organic Frameworks for Therapeutic, Imaging, and Sensing Applications. Adv. Mater. 2018, 30, e1707634. [Google Scholar] [CrossRef] [PubMed]
- Jo, J.H.; Kim, H.-C.; Huh, S.; Kim, Y.; Lee, D.N. Antibacterial activities of Cu-MOFs containing glutarates and bipyridyl ligands. Dalton Trans. 2019, 48, 8084–8093. [Google Scholar] [CrossRef]
- Motakef-Kazemi, N.; Shojaosadati, S.A.; Morsali, A. In situ synthesis of a drug-loaded MOF at room temperature. Microporous Mesoporous Mater. 2014, 186, 73–79. [Google Scholar] [CrossRef]
- Oh, H.; Li, T.; An, J. Drug Release Properties of a Series of Adenine-Based Metal–Organic Frameworks. Chem.—Eur. J. 2015, 21, 17010–17015. [Google Scholar] [CrossRef]
- Taylor-Pashow, K.M.; Della Rocca, J.; Xie, Z.; Tran, S.; Lin, W. Postsynthetic modifications of iron-carboxylate nanoscale metal− organic frameworks for imaging and drug delivery. Am. Chem. Soc. 2009, 131, 14261–14263. [Google Scholar] [CrossRef] [Green Version]
- Bellido, E.; Hidalgo, T.; Lozano, M.V.; Guillevic, M.; Simón-Vázquez, R.; Santander-Ortega, M.J.; Gonzalez-Fernandez, A.; Serre, C.; Alonso, M.J.; Horcajada, P. Heparin-engineered mesoporous iron metal-organic framework nanoparticles: Toward stealth drug nanocarriers. Adv. Healthc. Mater. 2015, 4, 1246–1257. [Google Scholar] [CrossRef]
- Ding, N.; Li, H.; Feng, X.; Wang, Q.; Wang, S.; Ma, L.; Zhou, J.; Wang, B. Partitioning MOF-5 into confined and hydrophobic compartments for carbon capture under humid conditions. J. Am. Chem. Soc. 2016, 138, 10100–10103. [Google Scholar] [CrossRef]
- Ma, D.; Li, Z.; Zhu, J.; Zhou, Y.; Chen, L.; Mai, X.; Liufu, M.; Wu, Y.; Li, Y. Inverse and highly selective separation of CO2/C2H2 on a thulium–organic framework. J. Mater. Chem. A. 2020, 8, 11933–11937. [Google Scholar] [CrossRef]
- Luo, J.; Ying, L.F.; Zhang, F.; Zhou, Z.; Zhang, Y.G. Cu(II)-Containing Metal−Organic Framework with 1D Hexagonal Channels for Cyanosilylation Reaction and Anticancer Activity on Osteosarcoma Cells. ACS Omega 2021, 6, 5856–5864. [Google Scholar] [CrossRef]
- Hwang, I.H.; Bae, J.M.; Kim, W.S.; Jo, Y.D.; Kim, C.; Kim, Y.; Kim, S.-J.; Huh, S. Bifunctional 3D Cu-MOFs containing glutarates and bipyridyl ligands: Selective CO2 sorption and heterogeneous catalysis. Dalton Trans. 2012, 41, 12759–12765. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.-C.; Mitra, S.; Veerana, M.; Lim, J.-S.; Jeong, H.-R.; Park, G.; Huh, S.; Kim, S.-J.; Kim, Y. Cobalt(II)-coordination polymers containing glutarates and bipyridyl ligands and their antifungal potential. Sci. Rep. 2019, 9, 14983. [Google Scholar] [CrossRef] [PubMed]
- Hwang, I.H.; Kim, H.Y.; Lee, M.M.; Na, Y.J.; Kim, J.H.; Kim, H.C.; Kim, C.; Huh, S.; Kim, Y.; Kim, S.-J. Zn-MOFs containing flexible α,ω-alkane (or alkene)-dicarboxylates and 1,2-bis(4-pyridyl) ethane ligands: CO2 sorption and photoluminescence. Cryst. Growth Des. 2013, 13, 4815–4823. [Google Scholar] [CrossRef]
- Xu, J.; Xue, D. Fabrication of copper hydroxyphosphate with complex architectures. J. Phys. Chem. B 2006, 110, 7750–7756. [Google Scholar] [CrossRef]
- Cho, I.-S.; Kim, D.W.; Lee, S.; Kwak, C.H.; Bae, S.-T.; Noh, J.H.; Yoon, S.H.; Jung, H.S.; Kim, D.-W.; Hong, K.S. Synthesis of Cu2PO4OH hierarchical superstructures with photocatalytic activity in visible light. Adv. Funct. Mater. 2008, 18, 2154–2162. [Google Scholar] [CrossRef]
- Luo, Y.-K.; Song, F.; Wang, X.-L.; Wang, Y.-Z. Pure copper phosphate nanostructures with controlled growth: A versatile support for enzyme immobilization. CrystEngComm 2017, 19, 2996–3002. [Google Scholar] [CrossRef]
- Jiang, L.; Kon, N.; Li, T.; Wang, S.-J.; Su, T.; Hibshoosh, H.; Baer, R.; Gu, W. Ferroptosis as a p53-mediated activity during tumour suppression. Nature 2015, 520, 57–62. [Google Scholar] [CrossRef] [PubMed] [Green Version]










| Cu-MOF | Co-MOF | Zn-MOF | |
|---|---|---|---|
| Empirical formula | C22H24Cu2N2O8 | C34H44 Co2N4O8 | C22H28N2O10Zn |
| Formula weight | 571.51 | 723.34 | 611.20 |
| Temperature | 223(2) K | 296(2) K | 293(2) K |
| Wavelength | 0.71073 Å | 0.71073 Å | 0.71073 Å |
| Space group | C 2/c | P 21/n | P 21/c |
| Unit cell dimensions | a = 24.848(7) Å, | a = 9.1670(3) Å, | a = 11.025(2) Å, |
| b = 13.263(4) Å, | b = 27.1849(8) Å, | b = 14.176(3) Å, | |
| c = 8.675(2) Å, | c = 13.5929(4) Å, | c = 16.191(3) Å, | |
| β = 92.745(3)° | β = 95.6332(16)° | β = 95.50(3)° | |
| Volume | 2855.8(14) Å3 | 3371.05(18) Å3 | 2518.8(9) Å3 |
| Z | 4 | 4 | 4 |
| Density (calculated) | 1.329 mg/m3 | 1.425 mg/m3 | 1.612 mg/m3 |
| Independent reflections | 3231 ((int) = 0.0484) | 5828 (R(int) = 0.0387) | 4954 (R(int) = 0.0252) |
| Data/restraints/parameters | 3231/36/206 | 5828/120/529 | 4954/9/338 |
| Goodness of fit on F2 | 1.076 | 1.061 | 1.049 |
| Final R indices [I > 2sigma(I)] | R1 = 0.0569, wR2 = 0.1702 | R1 = 0.0757, wR2 = 0.1903 | R1 = 0.0621, wR2 = 0.1836 |
| Bond | Cu-MOF | Co-MOF | Zn-MOF |
|---|---|---|---|
| M–O | Cu–O 1.969(3)–1.993(3) Å | Co–O 1.994(4)–2.285(4) Å | Zn–O 1.957(4) Å |
| M–N | Cu–N 2.117(11)–2.193(3) Å | Co–N 2.150(3)–2.184(3) Å | Zn–N 2.048(4), 2.056(4) Å |
| C–O | 1.239(6)–1.254(5) Å | 1.239(7)–1.261(7) Å | 1.213(7)–1.246(6) Å |
| N–C | 1.390 | 1.387(2)–1.432(13) Å | 1.316(7)–1.330(7) Å |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Han, I.; Choi, S.A.; Lee, D.N. Therapeutic Application of Metal–Organic Frameworks Composed of Copper, Cobalt, and Zinc: Their Anticancer Activity and Mechanism. Pharmaceutics 2022, 14, 378. https://doi.org/10.3390/pharmaceutics14020378
Han I, Choi SA, Lee DN. Therapeutic Application of Metal–Organic Frameworks Composed of Copper, Cobalt, and Zinc: Their Anticancer Activity and Mechanism. Pharmaceutics. 2022; 14(2):378. https://doi.org/10.3390/pharmaceutics14020378
Chicago/Turabian StyleHan, Ihn, Seung Ah Choi, and Do Nam Lee. 2022. "Therapeutic Application of Metal–Organic Frameworks Composed of Copper, Cobalt, and Zinc: Their Anticancer Activity and Mechanism" Pharmaceutics 14, no. 2: 378. https://doi.org/10.3390/pharmaceutics14020378
APA StyleHan, I., Choi, S. A., & Lee, D. N. (2022). Therapeutic Application of Metal–Organic Frameworks Composed of Copper, Cobalt, and Zinc: Their Anticancer Activity and Mechanism. Pharmaceutics, 14(2), 378. https://doi.org/10.3390/pharmaceutics14020378