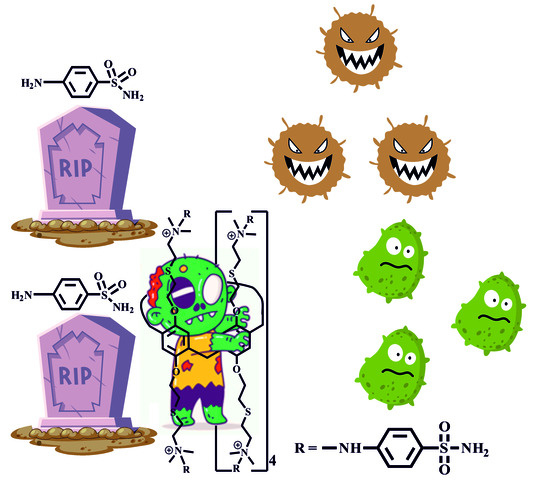
The Synthesis and Antibacterial Properties of Pillar[5]arene with Streptocide Fragments
Abstract
:1. Introduction
2. Materials and Methods
2.1. Synthesis of Compounds 2–9
2.1.1. 4,8,14,18,23,26,28,31,32,35-Deca-[thioethane(2′-(N,N-dimethyl)amino)ethoxy]-pillar[5]arene (2)
2.1.2. General Procedure for the Synthesis of Macrocycles 3–7
2.1.3. 4,8,14,18,23,26,28,31,32,35-Deca-[thioethane (2′-(N,N-dimethyl, N-propane-1-sulfonate)ammonium)ethoxy)-pillar[5]arene (8)
2.1.4. 4,8,14,18,23,26,28,31,32,35-Deca-[thioethane (2′-(N,N-dimethyl, N-acetate)ammonium)ethoxy]-pillar[5]arene (9)
2.2. Biological Investigations
2.2.1. Bacterial Strains and Cell Cultures
2.2.2. MICs Determination
2.2.3. BPC Analysis
2.2.4. Mutagenicity Assay
2.2.5. Cytotoxicity
2.2.6. Statistical Analysis
3. Results and Discussion
3.1. Synthesis and the Aggregation Characteristics of Water-Soluble Ammonium Derivatives of pillar[5]arene
3.2. Biologic Activity
3.2.1. Antibacterial Activity
3.2.2. Antibiofilm Activity
3.2.3. Cytotoxicity and Mutagenicity
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Fernández-Villa, D.; Aguilar, M.R.; Rojo, L. Folic Acid Antagonists: Antimicrobial and Immunomodulating Mechanisms and Applications. Int. J. Mol. Sci. 2019, 20, 4996. [Google Scholar] [CrossRef]
- Mbarga, M.J.A.; Anyutoulou, K.L.D.; Podoprigora, I.V.; Smolyakova, L.A.; Sarra, S.; Khelifi, I.; Das, M.S. The public health issue of antibiotic residues in food and feed: Causes, consequences, and potential solutions. Vet. World 2022, 15, 662–671. [Google Scholar] [CrossRef]
- Dai, T.; Huang, Y.Y.; Sharma, S.K.; Hashmi, J.T.; Kurup, D.B.; Hamblin, M.R. Topical antimicrobials for burn wound infections. Recent. Pat. Antiinfect. Drug Discov. 2010, 5, 124–151. [Google Scholar] [CrossRef] [PubMed]
- Ovung, A.; Bhattacharyya, J. Sulfonamide drugs: Structure, antibacterial property, toxicity, and biophysical interactions. Biophys. Rev. 2021, 13, 259–272. [Google Scholar] [CrossRef]
- Hassanein, M.M. Sulfonamides: Far from obsolete. Int. J. Contemp. Pediatr. 2019, 6, 2740–2745. [Google Scholar] [CrossRef]
- Rahimpour, E.; Acree, W.E.; Jouyban, A. Prediction of sulfonamides’ solubilities in the mixed solvents using solvation parameters. J. Mol. Liquids 2021, 339, 116269. [Google Scholar] [CrossRef]
- Wang, L.; Li, L.L.; Fan, Y.S.; Wang, H. Host-guest supramolecular nanosystems for cancer diagnostics and therapeutics. Adv. Mater. 2013, 25, 3888–3898. [Google Scholar] [CrossRef]
- Yan, M.; Zhou, J. Pillararene-Based Supramolecular Polymers for Cancer Therapy. Molecules 2023, 28, 1470. [Google Scholar] [CrossRef]
- Guo, S.; Huang, Q.; Chen, Y.; Wei, J.; Zheng, J.; Wang, L.; Wang, Y.; Wang, R. Synthesis and Bioactivity of Guanidinium-Functionalized Pillar[5]arene as a Biofilm Disruptor. Angew. Chem. Int. Ed. Engl. 2021, 60, 618–623. [Google Scholar] [CrossRef]
- Yang, K.; Chang, Y.; Wen, J.; Lu, Y.; Pei, Y.; Cao, S.; Wang, F.; Pei, Z. Supramolecular Vesicles Based on Complex of Trp-Modified Pillar[5]arene and Galactose Derivative for Synergistic and Targeted Drug Delivery. Chem. Mater. 2016, 28, 1990–1993. [Google Scholar] [CrossRef]
- Shurpik, D.N.; Aleksandrova, Y.I.; Mostovaya, O.A.; Nazmutdinova, V.A.; Tazieva, R.E.; Murzakhanov, F.F.; Gafurov, M.R.; Zelenikhin, P.V.; Subakaeva, E.V.; Sokolova, E.A.; et al. Self-Healing Thiolated Pillar[5]arene Films Containing Moxifloxacin Suppress the Development of Bacterial Biofilms. Nanomaterials 2022, 12, 1604. [Google Scholar] [CrossRef]
- Zyryanov, G.V.; Kopchuk, D.S.; Kovalev, I.S.; Santra, S.; Majee, A.; Ranu, B.C. Pillararenes as Promising Carriers for Drug Delivery. Int. J. Mol. Sci. 2023, 24, 5167. [Google Scholar] [CrossRef]
- Kakuta, T.; Yamagishi, T.A.; Ogoshi, T. Stimuli-Responsive Supramolecular Assemblies Constructed from Pillar[n]arenes. Acc. Chem. Res. 2018, 51, 1656–1666. [Google Scholar] [CrossRef]
- Feng, W.; Jin, M.; Yang, K.; Pei, Y.; Pei, Z. Supramolecular delivery systems based on pillararenes. Chem. Commun. 2018, 54, 13626–13640. [Google Scholar] [CrossRef] [PubMed]
- Gangemi, C.M.A.; Puglisi, R.; Pappalardo, A.; Sfrazzetto, G.T. Supramolecular complexes for nanomedicine. Bioorg. Med. Chem. Lett. 2018, 28, 3290–3301. [Google Scholar] [CrossRef] [PubMed]
- Yu, G.; Chen, X. Host-Guest Chemistry in Supramolecular Theranostics. Theranostics 2019, 9, 3041–3074. [Google Scholar] [CrossRef]
- Xin, P.; Zhao, L.; Mao, L.; Xu, L.; Hou, S.; Kong, H.; Fang, H.; Zhu, H.; Jiang, T.; Chen, C.P. Effect of charge status on the ion transport and antimicrobial activity of synthetic channels. Chem. Commun. 2020, 56, 13796–13799. [Google Scholar] [CrossRef]
- Yao, Y.; Xue, M.; Chi, X.; Ma, Y.; He, J.; Abliz, Z.; Huang, F. A new water-soluble pillar[5]arene: Synthesis and application in the preparation of gold nanoparticles. Chem. Commun. 2012, 48, 6505–6507. [Google Scholar] [CrossRef] [PubMed]
- Kayumov, A.; Heinrich, A.; Sharipova, M.; Iljinskaya, O.; Forchhammer, K. Inactivation of the general transcription factor TnrA in Bacillus subtilis by proteolysis. Microbiology 2008, 154, 2348–2355. [Google Scholar] [CrossRef]
- Sarker, S.D.; Nahar, L.; Kumarasamy, Y. Microtitre plate-based antibacterial assay incorporating resazurin as an indicator of cell growth, and its application in the in vitro antibacterial screening of phytochemicals. Methods 2007, 42, 321–324. [Google Scholar] [CrossRef]
- Merritt, J.H.; Kadouri, D.E.; O’Toole, G.A. Growing and analyzing static biofilms. Curr. Protoc. Microbiol. 2005, 1B.1.1–1B.1.17. [Google Scholar] [CrossRef]
- Mortelmans, K.; Zeiger, E. The Ames Salmonella/microsome mutagenicity assay. Mutat. Res. 2000, 455, 29–60. [Google Scholar] [CrossRef] [PubMed]
- Levy, D.D.; Zeiger, E.; Escobar, P.A.; Hakura, A.; van der Leede, B.M.; Kato, M.; Moore, M.M.; Sugiyama, K.I. Recommended criteria for the evaluation of bacterial mutagenicity data (Ames test). Mutat. Res. Genet. Toxicol. Environ. Mutagen. 2019, 848, 403074. [Google Scholar] [CrossRef]
- Mosmann, T. Rapid colorimetric assay for cellular growth and survival: Application to proliferation and cytotoxicity assays. J. Immunol. Methods 1983, 65, 55–63. [Google Scholar] [CrossRef] [PubMed]
- Kaizerman-Kane, D.; Hadar, M.; Joseph, R.; Logviniuk, D.; Zafrani, Y.; Fridman, M.; Cohen, Y. Design Guidelines for Cationic Pillar[n]arenes that Prevent Biofilm Formation by Gram-Positive Pathogens. ACS Infect. Dis. 2021, 7, 579–585. [Google Scholar] [CrossRef]
- Jiao, Y.; Niu, L.N.; Ma, S.; Li, J.; Tay, F.R.; Chen, J.H. Quaternary ammonium-based biomedical materials: State-of-the-art, toxicological aspects and antimicrobial resistance. Prog. Polym. Sci. 2017, 71, 53–90. [Google Scholar] [CrossRef]
- Leclercq, L.; Lubart, Q.; Dewilde, A.; Aubry, J.M.; Nardello-Rataj, V. Supramolecular effects on the antifungal activity of cyclodextrin/di-n-decyldimethylammonium chloride mixtures. Eur. J. Pharm. Sci. 2012, 46, 336–345. [Google Scholar] [CrossRef]
- Sokolova, A.S.; Yarovaya, O.I.; Shernyukov, A.V.; Pokrovsky, M.A.; Pokrovsky, A.G.; Lavrinenko, V.A.; Zarubaev, V.V.; Tretiak, T.S.; Anfimov, P.M.; Kiselev, O.I.; et al. New quaternary ammonium camphor derivatives and their antiviral activity, genotoxic effects and cytotoxicity. Bioorg. Med. Chem. 2013, 21, 6690–6698. [Google Scholar] [CrossRef]
- Singha, M.; Roy, S.; Pandey, S.D.; Bag, S.S.; Bhattacharya, P.; Das, M.; Ghosh, A.S.; Ray, D.; Basak, A. Use of azidonaphthalimide carboxylic acids as fluorescent templates with a built-in photoreactive group and a flexible linker simplifies protein labeling studies: Applications in selective tagging of HCAII and penicillin binding proteins. Chem. Commun. 2017, 53, 13015–13018. [Google Scholar] [CrossRef]
- Aldrich, C.; Bertozzi, C.; Georg, G.I.; Kiessling, L.; Lindsley, C.; Liotta, D.; Merz, K.M.J.; Schepartz, A.; Wang, S. The ecstasy and agony of assay interference compounds. ACS Chem. Neurosci. 2017, 8, 420–423. [Google Scholar] [CrossRef] [PubMed]
- Kaya, I.; Colmenarejo, G. Analysis of Nuisance Substructures and Aggregators in a Comprehensive Database of Food Chemical Compounds. J. Agric. Food Chem. 2020, 68, 8812–8824. [Google Scholar] [CrossRef]
- Irwin, J.J.; Duan, D.; Torosyan, H.; Doak, A.K.; Ziebart, K.T.; Sterling, T.; Tumanian, G.; Shoichet, B.K. An aggregation advisor for ligand discovery. J. Med. Chem. 2015, 58, 7076–7087. [Google Scholar] [CrossRef]
- Feng, B.Y.; Shoichet, B.K. A detergent-based assay for the detection of promiscuous inhibitors. Nat. Protoc. 2006, 1, 550–553. [Google Scholar] [CrossRef] [PubMed]
- Barbera, L.; De Plano, L.M.; Franco, D.; Gattuso, G.; Guglielmino, S.P.P.; Lando, G.; Notti, A.; Parisi, M.F.; Pisagatti, I. Antiadhesive and antibacterial properties of pillar[5]arene-based multilayers. Chem. Commun. 2018, 54, 10203–10206. [Google Scholar] [CrossRef] [PubMed]
- Aloke, C.; Achilonu, I. Coping with the ESKAPE pathogens: Evolving strategies, challenges and future prospects. Microb. Pathog. 2023, 175, 105963. [Google Scholar] [CrossRef] [PubMed]
- Sharafutdinov, I.S.; Trizna, E.Y.; Baidamshina, D.R.; Ryzhikova, M.N.; Sibgatullina, R.R.; Khabibrakhmanova, A.M.; Latypova, L.Z.; Kurbangalieva, A.R.; Rozhina, E.V.; Klinger-Strobel, M.; et al. Antimicrobial Effects of Sulfonyl Derivative of 2(5H)-Furanone against Planktonic and Biofilm Associated Methicillin-Resistant and -Susceptible Staphylococcus aureus. Front. Microbiol. 2017, 8, 2246. [Google Scholar] [CrossRef] [PubMed]


| Sample | Concentration, µM | daverage, nm | PDI | ζ-Potential, mV |
|---|---|---|---|---|
| 3 | 10 | 304 ± 52 | 0.35 ± 0.04 | 44.4 |
| 4 | 10 | 279 ± 46 | 0.42 ± 0.02 | 2.2 |
| 5 | 10 | 347 ± 31 | 0.37 ± 0.03 | 46.7 |
| 6 | 10 | 214 ± 23 | 0.49 ± 0.03 | 3.5 |
| 8 | 10 | 413 ± 91 | 0.42 ± 0.06 | - |
| 9 | 10 | 141 ± 5 | 0.27 ± 0.01 | 17.5 |
| Sample | S. typhimurium TA 98 | K. pneumonia | S. epidermidis | S. aureus | P. aeruginosa |
|---|---|---|---|---|---|
| 2 | >300 | >300 | >300 | >300 | >300 |
| 3 | >300 | >300 | >300 | >300 | >300 |
| 4 | >300 | >300 | >300 | >300 | >300 |
| 5 | >300 | >300 | >300 | >300 | >300 |
| 6 | 37.5 | 150 | 75 | 75 | 75 |
| 8 | >300 | >300 | >300 | >300 | >300 |
| 9 | 300 | 300 | 300 | >300 | 300 |
| Sulfonamide | 4800 | 4800 | 4800 | 4800 | 2400 |
| Microorganism | BPC, µM |
|---|---|
| S. aureus | 20 |
| P. aeruginosa | 50 |
| Compound, µM | Excess of the Revertants Number in the Experiment Compared to the Negative Control, Fold | ||
|---|---|---|---|
| S. typhimurium Strain | |||
| TA98 | TA100 | ||
| 2 | 3 | 1.14 ± 0.12 | 1.26 ± 0.41 |
| 30 | 1.28 ± 0.19 | 1.15 ± 0.26 | |
| 300 | 1.06 ± 0.08 | 1.31 ± 0.35 | |
| 6 | 3 | 1.08 ± 0.17 | 1.19 ± 0.23 |
| 30 | 1.27 ± 0.14 | 1.37 ± 0.40 | |
| Negative control (ddH2O) | 1.00 | 1.00 | |
| NaN3, 10 µg/plate | - | 12.42 ± 4.51 | |
| 4-Nitro-o-phenylenediamine, 2.5 µg/plate | 31.81 ± 6.72 | - | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Subakaeva, E.; Zelenikhin, P.; Sokolova, E.; Pergat, A.; Aleksandrova, Y.; Shurpik, D.; Stoikov, I. The Synthesis and Antibacterial Properties of Pillar[5]arene with Streptocide Fragments. Pharmaceutics 2023, 15, 2660. https://doi.org/10.3390/pharmaceutics15122660
Subakaeva E, Zelenikhin P, Sokolova E, Pergat A, Aleksandrova Y, Shurpik D, Stoikov I. The Synthesis and Antibacterial Properties of Pillar[5]arene with Streptocide Fragments. Pharmaceutics. 2023; 15(12):2660. https://doi.org/10.3390/pharmaceutics15122660
Chicago/Turabian StyleSubakaeva, Evgenia, Pavel Zelenikhin, Evgenia Sokolova, Arina Pergat, Yulia Aleksandrova, Dmitriy Shurpik, and Ivan Stoikov. 2023. "The Synthesis and Antibacterial Properties of Pillar[5]arene with Streptocide Fragments" Pharmaceutics 15, no. 12: 2660. https://doi.org/10.3390/pharmaceutics15122660
APA StyleSubakaeva, E., Zelenikhin, P., Sokolova, E., Pergat, A., Aleksandrova, Y., Shurpik, D., & Stoikov, I. (2023). The Synthesis and Antibacterial Properties of Pillar[5]arene with Streptocide Fragments. Pharmaceutics, 15(12), 2660. https://doi.org/10.3390/pharmaceutics15122660