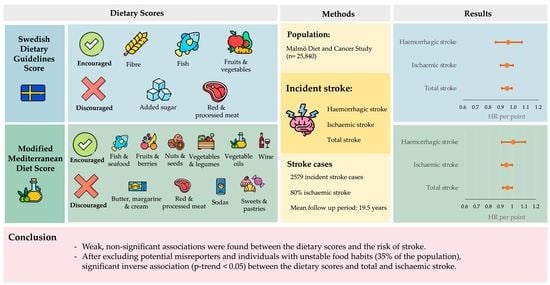
Association between Adherence to Swedish Dietary Guidelines and Mediterranean Diet and Risk of Stroke in a Swedish Population
Abstract
:1. Introduction
2. Materials and Methods
2.1. Subjects and Data Collection
2.2. Dietary Data Collection and Construction of Scores
2.3. Endpoint Ascertainment
2.4. Other Variables
2.5. Statistical Analyses
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Krishnamurthi, R.V.; Ikeda, T.; Feigin, V.L. Global, regional and country-specific burden of ischaemic stroke, intracerebral haemorrhage and subarachnoid haemorrhage: A systematic analysis of the global burden of disease study 2017. Neuroepidemiology 2020, 54, 171–179. [Google Scholar] [CrossRef] [PubMed]
- Tadi, T.; Lui, F. Acute Stroke. Available online: https://www.ncbi.nlm.nih.gov/books/NBK535369 (accessed on 26 September 2021).
- Feigin, V.L.; Lawes, C.M.; Bennett, D.A.; Barker-Collo, S.L.; Parag, V. Worldwide stroke incidence and early case fatality reported in 56 population-based studies: A systematic review. Lancet. Neurol. 2009, 8, 355–369. [Google Scholar] [CrossRef]
- An, S.J.; Kim, T.J.; Yoon, B.W. Epidemiology, Risk Factors, and Clinical features of intracerebral hemorrhage: An update. J. Stroke 2017, 19, 3–10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Feigin, V.L.; Stark, B.A.; Johnson, C.O.; Roth, G.A.; Bisignano, C.; Abady, G.G.; Abbasifard, M.; Abbasi-Kangevari, M.; Abd-Allah, F.; Abedi, V.; et al. Global, regional, and national burden of stroke and its risk factors, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet Neurol. 2021, 20, 795–820. [Google Scholar] [CrossRef]
- Evers, S.M.; Struijs, J.N.; Ament, A.J.; van Genugten, M.L.; Jager, J.H.; van den Bos, G.A. International comparison of stroke cost studies. Stroke 2004, 35, 1209–1215. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Price, A.J.; Wright, F.L.; Green, J.; Balkwill, A.; Kan, S.W.; Yang, T.O.; Floud, S.; Kroll, M.E.; Simpson, R.; Sudlow, C.L.M.; et al. Differences in risk factors for 3 types of stroke: UK prospective study and meta-analyses. Neurology 2018, 90, e298–e306. [Google Scholar] [CrossRef] [Green Version]
- Boehme, A.K.; Esenwa, C.; Elkind, M.S. Stroke risk factors, genetics, and prevention. Circ. Res. 2017, 120, 472–495. [Google Scholar] [CrossRef]
- Tong, T.Y.N.; Appleby, P.N.; Key, T.J.; Dahm, C.C.; Overvad, K.; Olsen, A.; Tjonneland, A.; Katzke, V.; Kuhn, T.; Boeing, H.; et al. The associations of major foods and fibre with risks of ischaemic and haemorrhagic stroke: A prospective study of 418 329 participants in the EPIC cohort across nine European countries. Eur. Heart J. 2020, 41, 2632–2640. [Google Scholar] [CrossRef]
- Yang, C.; Pan, L.; Sun, C.; Xi, Y.; Wang, L.; Li, D. Red meat consumption and the risk of stroke: A dose-response meta-analysis of prospective cohort studies. J. Stroke Cerebrovasc. Dis. 2016, 25, 1177–1186. [Google Scholar] [CrossRef] [Green Version]
- Hu, D.; Huang, J.; Wang, Y.; Zhang, D.; Qu, Y. Fruits and vegetables consumption and risk of stroke: A meta-analysis of prospective cohort studies. Stroke 2014, 45, 1613–1619. [Google Scholar] [CrossRef] [Green Version]
- Chen, G.C.; Lv, D.B.; Pang, Z.; Dong, J.Y.; Liu, Q.F. Dietary fiber intake and stroke risk: A meta-analysis of prospective cohort studies. Eur. J. Clin. Nutr. 2013, 67, 96–100. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hu, F.B. Dietary pattern analysis: A new direction in nutritional epidemiology. Curr. Opin. Lipidol. 2002, 13, 3–9. [Google Scholar] [CrossRef] [PubMed]
- Willett, W.C.; Sacks, F.; Trichopoulou, A.; Drescher, G.; Ferro-Luzzi, A.; Helsing, E.; Trichopoulos, D. Mediterranean diet pyramid: A cultural model for healthy eating. Am. J. Clin. Nutr. 1995, 61, 1402s–1406s. [Google Scholar] [CrossRef]
- Sánchez-Villegas, A.; Zazpe, I. Chapter 1-A healthy-eating model called mediterranean diet. In The Prevention of Cardiovascular Disease through the Mediterranean Diet; Sánchez-Villegas, A., Sánchez-Tainta, A., Eds.; Academic Press: Cambridge, MA, USA, 2018; pp. 1–24. [Google Scholar] [CrossRef]
- Hlebowicz, J.; Drake, I.; Gullberg, B.; Sonestedt, E.; Wallström, P.; Persson, M.; Nilsson, J.; Hedblad, B.; Wirfält, E. A high diet quality is associated with lower incidence of cardiovascular events in the malmö diet and cancer cohort. PLoS ONE 2013, 8, e71095. [Google Scholar] [CrossRef] [PubMed]
- Manjer, J.; Carlsson, S.; Elmståhl, S.; Gullberg, B.; Janzon, L.; Lindström, M.; Mattisson, I.; Berglund, G. The Malmö Diet and Cancer study: Representativity, cancer incidence and mortality in participants and non-participants. Eur. J. Cancer Prev. 2001, 10, 489–499. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Elmståhl, S.; Riboli, E.; Lindgärde, F.; Gullberg, B.; Saracci, R. The Malmö food study: The relative validity of a modified diet history method and an extensive food frequency questionnaire for measuring food intake. Eur. J. Clin. Nutr. 1996, 50, 143–151. [Google Scholar] [PubMed]
- Riboli, E.; Elmståhl, S.; Saracci, R.; Gullberg, B.; Lindgärde, F. The Malmö Food Study: Validity of two dietary assessment methods for measuring nutrient intake. Int. J. Epidemiol. 1997, 26 (Suppl. 1), S161–S173. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wirfält, E.; Mattisson, I.; Johansson, U.; Gullberg, B.; Wallström, P.; Berglund, G. A methodological report from the Malmö Diet and Cancer study: Development and evaluation of altered routines in dietary data processing. Nutr. J. 2002, 1, 3. [Google Scholar] [CrossRef] [Green Version]
- Callmer, E.; Riboli, E.; Saracci, R.; Akesson, B.; Lindgärde, F. Dietary assessment methods evaluated in the Malmö food study. J. Intern. Med. 1993, 233, 53–57. [Google Scholar] [CrossRef]
- FAO. Food-Based Dietary Guidelines-Sweden. Available online: https://www.fao.org/nutrition/education/food-based-dietary-guidelines/regions/countries/sweden/en/ (accessed on 26 September 2021).
- The Nordic Council and the Nordic Council of Ministers’. Nordic Nutrition Recommendations. 2012. Available online: https://www.norden.org/en/publication/nordic-nutrition-recommendations-2012 (accessed on 20 February 2022).
- Drake, I.; Gullberg, B.; Sonestedt, E.; Wallstrom, P.; Persson, M.; Hlebowicz, J.; Nilsson, J.; Hedblad, B.; Wirfalt, E. Scoring models of a diet quality index and the predictive capability of mortality in a population-based cohort of Swedish men and women. Public Health Nutr. 2013, 16, 468–478. [Google Scholar] [CrossRef] [Green Version]
- Martínez-González, M.A.; García-Arellano, A.; Toledo, E.; Salas-Salvadó, J.; Buil-Cosiales, P.; Corella, D.; Covas, M.I.; Schröder, H.; Arós, F.; Gómez-Gracia, E.; et al. A 14-item Mediterranean diet assessment tool and obesity indexes among high-risk subjects: The PREDIMED trial. PLoS ONE 2012, 7, e43134. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schroder, H.; Fito, M.; Estruch, R.; Martinez-Gonzalez, M.A.; Corella, D.; Salas-Salvado, J.; Lamuela-Raventos, R.; Ros, E.; Salaverria, I.; Fiol, M.; et al. A short screener is valid for assessing Mediterranean diet adherence among older Spanish men and women. J. Nutr. 2011, 141, 1140–1145. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ludvigsson, J.F.; Andersson, E.; Ekbom, A.; Feychting, M.; Kim, J.-L.; Reuterwall, C.; Heurgren, M.; Olausson, P.O. External review and validation of the Swedish national inpatient register. BMC Public Health 2011, 11, 450. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mutie, P.M.; Drake, I.; Ericson, U.; Teleka, S.; Schulz, C.-A.; Stocks, T.; Sonestedt, E. Different domains of self-reported physical activity and risk of type 2 diabetes in a population-based Swedish cohort: The Malmö diet and Cancer study. BMC Public Health 2020, 20, 261. [Google Scholar] [CrossRef] [PubMed]
- Frondelius, K.; Borg, M.; Ericson, U.; Borné, Y.; Melander, O.; Sonestedt, E. Lifestyle and dietary determinants of serum apolipoprotein a1 and apolipoprotein b concentrations: Cross-sectional analyses within a Swedish cohort of 24,984 Individuals. Nutrients 2017, 9, 211. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Manjer, J.; Elmstahl, S.; Janzon, L.; Berglund, G. Invitation to a population-based cohort study: Differences between subjects recruited using various strategies. Scand. J. Public Health 2002, 30, 103–112. [Google Scholar] [CrossRef] [PubMed]
- Mattisson, I.; Wirfalt, E.; Aronsson, C.A.; Wallstrom, P.; Sonestedt, E.; Gullberg, B.; Berglund, G. Misreporting of energy: Prevalence, characteristics of misreporters and influence on observed risk estimates in the Malmo Diet and Cancer cohort. Br. J. Nutr. 2005, 94, 832–842. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sonestedt, E.; Wirfält, E.; Gullberg, B.; Berglund, G. Past food habit change is related to obesity, lifestyle and socio-economic factors in the Malmo Diet and Cancer Cohort. Public Health Nutr. 2005, 8, 876–885. [Google Scholar] [CrossRef] [Green Version]
- Hansen, C.P.; Overvad, K.; Kyrø, C.; Olsen, A.; Tjønneland, A.; Johnsen, S.P.; Jakobsen, M.U.; Dahm, C.C. Adherence to a Healthy Nordic Diet and Risk of Stroke: A Danish Cohort Study. Stroke 2017, 48, 259–264. [Google Scholar] [CrossRef]
- Olsen, A.; Egeberg, R.; Halkjær, J.; Christensen, J.; Overvad, K.; Tjønneland, A. Healthy aspects of the Nordic diet are related to lower total mortality. J. Nutr. 2011, 141, 639–644. [Google Scholar] [CrossRef]
- Aune, D.; Keum, N.; Giovannucci, E.; Fadnes, L.T.; Boffetta, P.; Greenwood, D.C.; Tonstad, S.; Vatten, L.J.; Riboli, E.; Norat, T. Whole grain consumption and risk of cardiovascular disease, cancer, and all cause and cause specific mortality: Systematic review and dose-response meta-analysis of prospective studies. BMJ 2016, 353, i2716. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- He, F.J.; Nowson, C.A.; MacGregor, G.A. Fruit and vegetable consumption and stroke: Meta-analysis of cohort studies. Lancet 2006, 367, 320–326. [Google Scholar] [CrossRef]
- Reynolds, A.; Mann, J.; Cummings, J.; Winter, N.; Mete, E.; Te Morenga, L. Carbohydrate quality and human health: A series of systematic reviews and meta-analyses. Lancet 2019, 393, 434–445. [Google Scholar] [CrossRef] [Green Version]
- Sofi, F.; Abbate, R.; Gensini, G.F.; Casini, A. Accruing evidence on benefits of adherence to the Mediterranean diet on health: An updated systematic review and meta-analysis. Am. J. Clin. Nutr. 2010, 92, 1189–1196. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Trichopoulou, A.; Kouris-Blazos, A.; Wahlqvist, M.L.; Gnardellis, C.; Lagiou, P.; Polychronopoulos, E.; Vassilakou, T.; Lipworth, L.; Trichopoulos, D. Diet and overall survival in elderly people. BMJ 1995, 311, 1457–1460. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rees, K.; Hartley, L.; Flowers, N.; Clarke, A.; Hooper, L.; Thorogood, M.; Stranges, S. ‘Mediterranean’ dietary pattern for the primary prevention of cardiovascular disease. Cochrane Database Syst. Rev. 2019, 3, Cd009825. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Widmer, R.J.; Flammer, A.J.; Lerman, L.O.; Lerman, A. The Mediterranean diet, its components, and cardiovascular disease. Am. J. Med. 2015, 128, 229–238. [Google Scholar] [CrossRef] [Green Version]
- Martinez-Gonzalez, M.A.; Bes-Rastrollo, M. Dietary patterns, Mediterranean diet, and cardiovascular disease. Curr. Opin. Lipidol. 2014, 25, 20–26. [Google Scholar] [CrossRef]
- Tektonidis, T.G.; Åkesson, A.; Gigante, B.; Wolk, A.; Larsson, S.C. A Mediterranean diet and risk of myocardial infarction, heart failure and stroke: A population-based cohort study. Atherosclerosis 2015, 243, 93–98. [Google Scholar] [CrossRef]
- Zhang, C.; Qin, Y.Y.; Chen, Q.; Jiang, H.; Chen, X.Z.; Xu, C.L.; Mao, P.J.; He, J.; Zhou, Y.H. Alcohol intake and risk of stroke: A dose-response meta-analysis of prospective studies. Int. J. Cardiol. 2014, 174, 669–677. [Google Scholar] [CrossRef]
- Bernstein, A.M.; de Koning, L.; Flint, A.J.; Rexrode, K.M.; Willett, W.C. Soda consumption and the risk of stroke in men and women. Am. J. Clin. Nutr. 2012, 95, 1190–1199. [Google Scholar] [CrossRef] [PubMed]
- Janzi, S.; Ramne, S.; Gonzalez-Padilla, E.; Johnson, L.; Sonestedt, E. Associations between added sugar intake and risk of four different cardiovascular diseases in a Swedish population-based prospective cohort study. Front. Nutr. 2020, 7, 603653. [Google Scholar] [CrossRef] [PubMed]



| Low (0–1 Points) | Medium (2–4 Points) | High (5–10 Points) | p-Value | |
|---|---|---|---|---|
| n | 10,642 | 11,849 | 3349 | |
| Mean (SD) | ||||
| Age, years | 57.5 (7.6) | 58.1 (7.6) | 57.9 (7.6) | <0.001 |
| BMI, kg/m2 | 25.5 (3.9) | 25.7 (3.9) | 25.4 (3.9) | <0.001 |
| Fibre, g/MJ | 1.83 (0.38) | 2.32 (0.59) | 3.00 (0.61) | <0.001 |
| Fish and shellfish, g/week | 215 (179) | 368 (253) | 472 (259) | <0.001 |
| Fruit and vegetables, g/day | 271 (107) | 412 (173) | 584 (196) | <0.001 |
| Added sugar, E% | 12.0 (4.4) | 9.19 (3.78) | 7.39 (2.91) | <0.001 |
| Red and processed meat, g/week | 930 (399) | 798 (431) | 530 (335) | <0.001 |
| Total energy, MJ/day | 9.84 (2.70) | 9.55 (2.80) | 8.65 (2.33) | <0.001 |
| Carbohydrates, E% | 44.6 (5.6) | 45.0 (6.4) | 47.5 (5.7) | <0.001 |
| Protein, E% | 15.0 (2.3) | 16.1 (2.5) | 17.0 (2.7) | <0.001 |
| Fat, E% | 40.4 (5.6) | 38.9 (6.3) | 35.5 (5.6) | <0.001 |
| Vitamin C, mg/MJ | 9.1 (5.3) | 12.1 (6.3) | 17.5 (7.6) | <0.001 |
| Vitamin D, ug/MJ | 0.74 (0.23) | 0.81 (0.30) | 0.87 (0.33) | <0.001 |
| Folate, ug/MJ | 22.7 (5.5) | 27.1 (6.7) | 33.7 (8.0) | <0.001 |
| Iron, mg/MJ | 1.59 (0.32) | 1.64 (0.32) | 1.66 (0.30) | <0.001 |
| Calcium, mg/MJ | 114 (34) | 122 (35) | 134 (36) | <0.001 |
| Potassium, mg/MJ | 326 (59) | 373 (69) | 440 (80) | <0.001 |
| Magnesium, mg/MJ | 34.0 (4.9) | 37.6 (5.7) | 42.8 (6.5) | <0.001 |
| Selenium, ug/MJ | 3.51 (0.96) | 4.20 (1.25) | 4.87 (1.47) | <0.001 |
| Zinc, mg/MJ | 1.15 (0.19) | 1.19 (0.20) | 1.21 (0.20) | <0.001 |
| N (%) | ||||
| Females | 5899 (55.4%) | 7480 (63.1%) | 2692 (80.4%) | <0.001 |
| Smokers | 3743 (35.2%) | 2956 (24.9%) | 639 (19.1%) | <0.001 |
| University degree | 1179 (11.1%) | 1889 (15.9%) | 717 (21.4%) | <0.001 |
| Highest quintile of alcohol intake | 1904 (17.9%) | 2426 (20.5%) | 616 (18.4%) | <0.001 |
| Low leisure-time physical activity | 1287 (12.1%) | 947 (8.0%) | 178 (5.3%) | <0.001 |
| Underreporting | 1366 (12.8%) | 1860 (15.7%) | 704 (21.0%) | <0.001 |
| Past diet change | 1652 (15.5%) | 2677 (22.6%) | 1230 (36.8%) | <0.001 |
| Low (0–1 Points) | Medium (2–4 Points) | High (5–10 Points) | p-Value | |
|---|---|---|---|---|
| n | 4432 | 19,439 | 1969 | |
| Mean (SD) | ||||
| Age, years | 57.3 (7.3) | 58.1 (7.7) | 56.6 (7.2) | <0.001 |
| BMI, kg/m2 | 25.9 (4.0) | 25.5 (3.9) | 25.3 (3.7) | <0.001 |
| Fish and shellfish, servings/week | 1.50 (1.13) | 2.51 (1.88) | 3.94 (2.34) | <0.001 |
| Fruit and berries, servings/week | 11.9 (7.3) | 18.2 (11.5) | 27.8 (13.6) | <0.001 |
| Nuts and seeds, servings/week | 0.29 (0.61) | 0.40 (1.04) | 1.00 (2.30) | <0.001 |
| Vegetables and legumes, servings/week | 3.42 (1.56) | 4.21 (2.22) | 7.03 (3.41) | <0.001 |
| Vegetable oils, servings/week | 0.42 (1.00) | 0.53 (1.16) | 1.08 (2.35) | <0.001 |
| Wine, servings/week | 1.49 (2.30) | 3.38 (4.81) | 7.12 (6.69) | <0.001 |
| Butter, margarine and cream, servings/week | 38.5 (19.3) | 31.9 (17.7) | 24.9 (17.3) | <0.001 |
| Red and processed meat, servings/week | 9.15 (3.21) | 6.15 (3.20) | 4.53 (2.72) | <0.001 |
| Soda, servings/week | 6.66 (7.97) | 2.43 (4.62) | 1.22 (2.47) | <0.001 |
| Sweets and pastries, servings/week | 10.6 (7.1) | 8.87 (6.74) | 5.26 (5.78) | <0.001 |
| Total energy, MJ/day | 10.6 (2.8) | 9.34 (2.67) | 9.23 (2.66) | <0.001 |
| Carbohydrates, E% | 44.4 (5.5) | 45.2 (6.0) | 46.7 (6.9) | <0.001 |
| Protein, E% | 14.9 (2.2) | 15.8 (2.5) | 17.2 (3.0) | <0.001 |
| Fat, E% | 40.7 (5.6) | 39.0 (6.0) | 36.2 (6.8) | <0.001 |
| Vitamin C, mg/MJ | 8.4 (4.5) | 11.7 (6.4) | 18.0 (8.6) | <0.001 |
| Vitamin D, ug/MJ | 0.74 (0.21) | 0.79 (0.28) | 0.84 (0.36) | <0.001 |
| Folate, ug/MJ | 22.1 (5.3) | 26.3 (6.8) | 33.8 (9.6) | <0.001 |
| Iron, mg/MJ | 1.63 (0.33) | 1.61 (0.31) | 1.66 (0.31) | <0.001 |
| Calcium, mg/MJ | 108 (32) | 122 (36) | 131 (38) | <0.001 |
| Potassium, mg/MJ | 319 (58) | 365 (72) | 438 (93) | <0.001 |
| Magnesium, mg/MJ | 33.6 (4.8) | 37.0 (5.8) | 42.3 (7.6) | <0.001 |
| Selenium, ug/MJ | 3.42 (0.89) | 4.04 (1.22) | 4.99 (1.65) | <0.001 |
| Zinc, mg/MJ | 1.19 (0.19) | 1.18 (0.20) | 1.20 (0.21) | <0.001 |
| N (%) | ||||
| Females | 1908 (43.1%) | 12,762 (65.7%) | 1401 (71.2%) | <0.001 |
| Smokers | 1504 (33.9%) | 5358 (27.6%) | 476 (24.2%) | <0.001 |
| University degree | 354 (8.0%) | 2884 (14.8%) | 544 (27.6%) | <0.001 |
| Highest quintile of alcohol intake | 463 (10.4%) | 3658 (18.8%) | 825 (41.9%) | <0.001 |
| Low leisure-time physical activity | 523 (11.8%) | 1769 (9.1%) | 120 (6.1%) | <0.001 |
| Underreporting | 520 (11.7%) | 3027 (15.6%) | 383 (19.5%) | <0.001 |
| Past diet change | 730 (16.5%) | 4146 (21.3%) | 683 (34.8%) | <0.001 |
| Adherence to Swedish Dietary Guidelines Score | ||||||
|---|---|---|---|---|---|---|
| Low (0–1 Points) | Medium (2–3 Points) | High (4–5 Points) | Per Point | p-Trend | ||
| n | 10,642 | 11,849 | 3349 | |||
| Years of follow-up | 203,453 | 232,484 | 67,344 | |||
| Total stroke | Cases/cases per 1000 PY | 1101/5.41 | 1189/5.11 | 289/4.29 | ||
| Model 1 | 1.00 | 0.91 (0.84–0.99) | 0.81 (0.71–0.93) | 0.95 (0.92–0.98) | 0.001 | |
| Model 2 | 1.00 | 0.97 (0.89–1.05) | 0.89 (0.78–1.02) | 0.98 (0.95–1.01) | 0.13 | |
| Model 3 | 1.00 | 0.96 (0.88–1.04) | 0.89 (0.78–1.02) | 0.97 (0.94–1.01) | 0.10 | |
| Model 3 (excl. misreporters) | 1.00 | 0.94 (0.85–1.04) | 0.87 (0.72–1.04) | 0.96 (0.92–1.00) | 0.04 | |
| Ischaemic stroke | Cases/cases per 1000 PY | 910/4.47 | 957/4.12 | 237/3.52 | ||
| Model 1 | 1.00 | 0.89 (0.81–0.98) | 0.81 (0.70–0.94) | 0.94 (0.91–0.98) | 0.001 | |
| Model 2 | 1.00 | 0.95 (0.86–1.04) | 0.90 (0.78–1.05) | 0.97 (0.94–1.01) | 0.14 | |
| Model 3 | 1.00 | 0.94 (0.86–1.03) | 0.90 (0.77–1.04) | 0.97 (0.94–1.01) | 0.10 | |
| Model 3 (excl. misreporters) | 1.00 | 0.91 (0.81–1.02) | 0.87 (0.72–1.07) | 0.95 (0.91–1.00) | 0.03 | |
| Haemorrhagic stroke | Cases/cases per 1000 PY | 172/0.85 | 209/0.90 | 51/0.78 | ||
| Model 1 | 1.00 | 1.02 (0.83–1.25) | 0.89 (0.64–1.22) | 0.97 (0.90–1.05) | 0.48 | |
| Model 2 | 1.00 | 1.07 (0.87–1.32) | 0.95 (0.69–1.31) | 0.99 (0.92–1.07) | 0.88 | |
| Model 3 | 1.00 | 1.07 (0.87–1.32) | 0.95 (0.69–1.31) | 0.99 (0.92–1.07) | 0.89 | |
| Model 3 (excl. misreporters) | 1.00 | 1.15 (0.90–1.48) | 0.96 (0.62–1.48) | 1.01 (0.91–1.11) | 0.87 | |
| Adherence to Modified Mediterranean Diet Score | ||||||
|---|---|---|---|---|---|---|
| Low (0–1 Points) | Medium (2–4 Points) | High (5–10 Points) | Per Point | p-Trend | ||
| n | 4432 | 19,439 | 1696 | |||
| Years of follow-up | 84,834 | 378,907 | 39,542 | |||
| Total stroke | Cases/cases per 1000 PY | 480/5.66 | 1936/5.11 | 163/4.12 | ||
| Model 1 | 1.00 | 0.90 (0.81–0.99) | 0.84 (0.70–1.00) | 0.96 (0.93–0.99) | 0.008 | |
| Model 2 | 1.00 | 0.94 (0.84–1.04) | 0.92 (0.76–1.11) | 0.98 (0.94–1.01) | 0.18 | |
| Model 3 | 1.00 | 0.94 (0.85–1.04) | 0.92 (0.76–1.11) | 0.98 (0.94–1.01) | 0.18 | |
| Model 3 (excl. misreporters) | 1.00 | 0.89 (0.78–1.00) | 0.81 (0.63–1.05) | 0.95 (0.91–0.99) | 0.02 | |
| Ischaemic stroke | Cases/cases per 1000 PY | 396/4.67 | 1576/4.16 | 132/3.34 | ||
| Model 1 | 1.00 | 0.89 (0.79–1.00) | 0.83 (0.68–1.02) | 0.96 (0.93–1.00) | 0.03 | |
| Model 2 | 1.00 | 0.93 (0.83–1.05) | 0.92 (0.75–1.13) | 0.98 (0.95–1.02) | 0.37 | |
| Model 3 | 1.00 | 0.94 (0.84–1.05) | 0.93 (0.75–1.14) | 0.98 (0.95–1.02) | 0.38 | |
| Model 3 (excl. misreporters) | 1.00 | 0.87 (0.76–1.00) | 0.79 (0.59–1.04) | 0.95 (0.90–1.00) | 0.03 | |
| Haemorrhagic stroke | Cases/cases per 1000 PY | 74/0.87 | 329/0.87 | 29/0.73 | ||
| Model 1 | 1.00 | 0.96 (0.74–1.25) | 0.90 (0.59–1.40) | 0.94 (0.87–1.02) | 0.12 | |
| Model 2 | 1.00 | 1.00 (0.77–1.30) | 0.97 (0.62–1.52) | 0.95 (0.87–1.03) | 0.24 | |
| Model 3 | 1.00 | 1.00 (0.77–1.30) | 0.97 (0.62–1.52) | 0.95 (0.87–1.03) | 0.24 | |
| Model 3 (excl. misreporters) | 1.00 | 1.02 (0.74–1.40) | 1.07 (0.60–1.94) | 0.96 (0.86–1.07) | 0.47 | |
| Diet Score | Diet Component | Recommendation | N (%) Reaching Recommendation | HR (95% CI) for Those Reaching Recommendations | |||||
|---|---|---|---|---|---|---|---|---|---|
| Whole Sample | Excluding Misreporters and Diet Changers 2 | ||||||||
| Total Stroke | Ischaemic Stroke | Haemorrhagic Stroke | Total Stroke | Ischaemic Stroke | Haemorrhagic Stroke | ||||
| SDGS | |||||||||
| Encouraged | |||||||||
| Fibre | >2.4 g/MJ | 8510 (32.9%) | 0.92 (0.85–1.01) | 0.92 (0.84–1.02) | 0.94 (0.77–1.17) | 0.89 (0.79–1.00) | 0.90 (0.79–1.02) | 0.88 (0.66–1.16) | |
| Fish | >300 g/week | 11,727 (45.4%) | 0.98 (0.90–1.06) | 1.00 (0.91–1.09) | 0.96 (0.79–1.17) | 0.97 (0.88–1.07) | 0.97 (0.87–1.09) | 1.04 (0.82–1.32) | |
| Fruit and vegetables | >400 g/day | 9884 (35.3%) | 0.96 (0.88–1.05) | 0.93 (0.85–1.02) | 1.12 (0.91–1.37) | 0.92 (0.83–1.03) | 0.90 (0.80–1.01) | 1.07 (0.83–1.38) | |
| Discouraged | |||||||||
| Added sugar | <10%E | 14,043 (54.3%) | 0.99 (0.92–1.08) | 0.97 (0.89–1.06) | 1.08 (0.89–1.31) | 0.97 (0.88–1.07) | 0.94 (0.85–1.05) | 1.12 (0.88–1.42) | |
| Red and processed meat | <500 g/week | 5613 (21.7%) | 0.94 (0.85–1.04) | 0.97 (0.86–1.08) | 0.81 (0.63–1.04) | 0.94 (0.82–1.08) | 0.95 (0.81–1.10) | 0.90 (0.65–1.25) | |
| mMDS | |||||||||
| Encouraged | |||||||||
| Fish and seafood | ≥3 svg/week | 7991 (30.9%) | 1.02 (0.94–1.11) | 1.04 (0.95–1.15) | 0.97 (0.78–1.19) | 1.00 (0.90–1.11) | 1.00 (0.89–1.12) | 1.04 (0.81–1.33) | |
| Fruits and berries | ≥21 svg/week | 8632 (33.4%) | 0.94 (0.86–1.03) | 0.94 (0.86–1.04) | 0.88 (0.71–1.08) | 0.89 (0.80–1.00) | 0.89 (0.78–1.00) | 0.87 (0.67–1.13) | |
| Nuts and seeds | ≥3 svg/week | 749 (2.9%) | 0.78 (0.60–1.01) | 0.77 (0.57–1.04) | 0.81 (0.43–1.52) | 0.79 (0.57–1.10) | 0.81 (0.57–1.16) | 0.77 (0.34–1.73) | |
| Vegetables and legumes | ≥7 svg/week | 2875 (11.1%) | 0.96 (0.83–1.09) | 0.95 (0.82–1.11) | 0.97 (0.70–1.33) | 0.93 (0.77–1.13) | 0.91 (0.74–1.12) | 1.05 (0.69–1.61) | |
| Vegetable oils | ≥28 svg/week | 4 (0%) | - | - | - | - | - | - | |
| Wine | ≥7 svg/week | 4738 (18.3%) | 0.87 (0.75–1.00) | 0.92 (0.79–1.07) | 0.65 (0.45–0.93) | 0.88 (0.75–1.04) | 0.93 (0.78–1.12) | 0.66 (0.43–1.01) | |
| Discouraged | |||||||||
| Butter, margarine, and cream | <7 svg/week | 850 (3.3%) | 1.14 (0.91–1.42) | 1.15 (0.90–1.48) | 1.14 (0.66–1.96) | 1.17 (0.81–1.69) | 1.09 (0.71–1.66) | 1.72 (0.81–3.67) | |
| Red and processed meat | <7 svg/week | 16,179 (62.6%) | 0.97 (0.88–1.06) | 0.97 (0.88–1.07) | 1.06 (0.85–1.33) | 0.95 (0.85–1.06) | 0.94 (0.83–1.06) | 1.07 (0.81–1.41) | |
| Soda | <7 svg/week | 22,074 (85.4%) | 0.89 (0.80–0.99) | 0.89 (0.79–1.00) | 0.86 (0.66–1.12) | 0.83 (0.73–0.94) | 0.81 (0.70–0.93) | 0.88 (0.64–1.22) | |
| Sweets and pastries | <3 svg/week | 4499 (17.4%) | 1.12 (1.01–1.24) | 1.12 (1.00–1.26) | 1.10 (0.85–1.42) | 1.13 (0.98–1.30) | 1.15 (0.98–1.34) | 1.01 (0.71–1.45) | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
González-Padilla, E.; Tao, Z.; Sánchez-Villegas, A.; Álvarez-Pérez, J.; Borné, Y.; Sonestedt, E. Association between Adherence to Swedish Dietary Guidelines and Mediterranean Diet and Risk of Stroke in a Swedish Population. Nutrients 2022, 14, 1253. https://doi.org/10.3390/nu14061253
González-Padilla E, Tao Z, Sánchez-Villegas A, Álvarez-Pérez J, Borné Y, Sonestedt E. Association between Adherence to Swedish Dietary Guidelines and Mediterranean Diet and Risk of Stroke in a Swedish Population. Nutrients. 2022; 14(6):1253. https://doi.org/10.3390/nu14061253
Chicago/Turabian StyleGonzález-Padilla, Esther, Zhen Tao, Almudena Sánchez-Villegas, Jacqueline Álvarez-Pérez, Yan Borné, and Emily Sonestedt. 2022. "Association between Adherence to Swedish Dietary Guidelines and Mediterranean Diet and Risk of Stroke in a Swedish Population" Nutrients 14, no. 6: 1253. https://doi.org/10.3390/nu14061253
APA StyleGonzález-Padilla, E., Tao, Z., Sánchez-Villegas, A., Álvarez-Pérez, J., Borné, Y., & Sonestedt, E. (2022). Association between Adherence to Swedish Dietary Guidelines and Mediterranean Diet and Risk of Stroke in a Swedish Population. Nutrients, 14(6), 1253. https://doi.org/10.3390/nu14061253