Telenutrition: Changes in Professional Practice and in the Nutritional Assessments of Italian Dietitian Nutritionists in the COVID-19 Era
Abstract
:1. Introduction
2. Materials and Methods
2.1. Survey Development and Design
2.2. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. 2019 Novel Coronavirus (2019-nCoV): Strategic Preparedness and Response Plan. 4 February 2020. Available online: https://www.who.int/publications/i/item/strategic-preparedness-and-response-plan-for-the-new-coronavirus (accessed on 10 December 2021).
- Italian Government Official Gazette of the Italian Republic. Decree of the President of the Council of Ministers (DPCM) 9 March 2020. Italy. Available online: https://www.gazzettaufficiale.it/eli/id/2020/03/09/20A01558/sg (accessed on 10 December 2021).
- Galimberti, F.; Bonomi Boseggia, S.; Tragni, E. Consequences of COVID-19 pandemic on healthcare services. G. Ital. Di Farm. E Farm. 2021, 13, 5–16. Available online: https://www.sefap.it/web/upload/GIFF2021_1_5_16.pdf (accessed on 10 December 2021).
- Verhoeven, V.; Tsakitzidis, G.; Philips, H.; Van Royen, P. Impact of the COVID-19 pandemic on the core functions of primary care: Will the cure be worse than the disease? A qualitative interview study in Flemish GPs. BMJ Open 2020, 10, e039674. [Google Scholar] [PubMed]
- Italian National Health Institute. PASSI and PASSI d’Argento and the COVID-19 Pandemic. Version of 9 March 2021. Available online: https://www.iss.it/documents/20126/0/Rapporto+ISS+COVID-19+5_2021.pdf/85ea5f8e-74f8-2d50-2cd5-48e9a6cf479a?t=1615542933549 (accessed on 12 December 2021).
- Kichloo, A.; Albosta, M.; Dettloff, K.; Wani, F.; El-Amir, Z.; Singh, J.; Aljadah, M.; Chakinala, R.C.; Kanugula, A.K.; Solanki, S.; et al. Telemedicine, the current COVID-19 pandemic and the future: A narrative review and perspectives moving forward in the USA. Fam. Med. Community Health 2020, 8, e000530. [Google Scholar] [PubMed]
- Keesara, S.; Jonas, A.; Schulman, K. COVID-19 and Health Care’s Digital Revolution. N. Engl. J. Med. 2020, 382, e82. [Google Scholar] [PubMed]
- Elbarbary, N.S.; Dos Santos, T.J.; de Beaufort, C.; Agwu, J.C.; Calliari, L.E.; Scaramuzza, A.E. COVID-19 outbreak and pediatric diabetes: Perceptions of health care professionals worldwide. Pediatr. Diabetes 2020, 21, 1083–1092. [Google Scholar]
- Fortney, J.C.; Pyne, J.M.; Edlund, M.J.; Williams, D.K.; Robinson, D.E.; Mittal, D.; Henderson, K.L. A randomized trial of telemedicine-based collaborative care for depression. J. Gen. Intern. Med. 2007, 22, 1086–1093. [Google Scholar] [PubMed] [Green Version]
- World Health Organization. Global Observatory for eHealth. Telemedicine: Opportunities and developments in Member States: Report on the Second Global Survey on eHealth. World Health Organization. 2010. Available online: https://apps.who.int/iris/handle/10665/44497 (accessed on 15 December 2021).
- The European Federation of the Associations of Dietitians. Role of Dietitians in the fight against COVID-19. 2020. Available online: https://www.efad.org/media/1985/role-of-dietitians-in-the-fight-against-covid19-efad-briefing-paper-may-2020.pdf (accessed on 14 December 2021).
- Handu, D.; Moloney, L.; Rozga, M.; Cheng, F.W. Malnutrition Care During the COVID-19 Pandemic: Considerations for Registered Dietitian Nutritionists. J. Acad. Nutr. Diet. 2021, 121, 979–987. [Google Scholar]
- Williams, K.; Eggett, D.; Patten, E.V. How work and family caregiving responsibilities interplay and affect registered dietitian nutritionists and their work: A national survey. PLoS ONE 2021, 16, e0248109. [Google Scholar]
- Academy of Nutrition and Dietetics. Practicing Telehealth. 2021. Available online: https://www.eatrightpro.org/practice/practice-resources/telehealth/practicingtelehealth (accessed on 12 January 2022).
- Brunton, C.; Arensberg, M.B.; Drawert, S.; Badaracco, C.; Everett, W.; McCauley, S.M. Perspectives of Registered Dietitian Nutritionists on Adoption of Telehealth for Nutrition Care during the COVID-19 Pandemic. Healthcare 2021, 9, 235. [Google Scholar]
- Greenhalgh, T.; Vijayaraghavan, S.; Wherton, J.; Shaw, S.; Byrne, E.; Campbell-Richards, D.; Bhattacharya, S.; Hanson, P.; Ramoutar, S.; Gutteridge, C.; et al. Virtual online consultations: Advantages and limitations (VOCAL) study. BMJ Open 2016, 6, e009388. [Google Scholar]
- Rozga, M.; Handu, D.; Kelley, K.; Jimenez, E.Y.; Martin, H.; Schofield, M.; Steiber, A. Telehealth During the COVID-19 Pandemic: A Cross-Sectional Survey of Registered Dietitian Nutritionists. J. Acad. Nutr. Diet. 2021, 121, 2524–2535. [Google Scholar] [PubMed]
- Geldsetzer, P. Use of Rapid Online Surveys to Assess People’s Perceptions During Infectious Disease Outbreaks: A Cross-sectional Survey on COVID-19. J. Med. Internet Res. 2020, 22, e18790. [Google Scholar] [PubMed]
- Jortberg, B.T.; Parrott, J.S.; Schofield, M.; Myers, E.; Ayoob, K.T.; Beseler, L.; Davis, A.; Jimenez, E.Y.; Pavlinac, J.; Smith, K. Rends in Registered Dietitian Nutritionists’ Knowledge and Patterns of Coding, Billing, and Payment. J. Acad. Nutr. Diet. 2020, 120, 134–145.e3. [Google Scholar] [PubMed]
- Rzymski, P.; Nowicki, M. COVID-19-related prejudice toward Asian medical students: A consequence of SARS-CoV-2 fears in Poland. J. Infect. Public Health 2020, 13, 873–876. [Google Scholar] [PubMed]
- Mazza, E.; Ferro, Y.; Pujia, R.; Maurotti, S.; Montalcini, T.; Pujia, A. Homemade food, alcohol, and body weight: Change in eating habits in young individuals at the time of COVID-19 Lockdown. J. Educ. Health Promot. 2021, 10, 427. [Google Scholar] [PubMed]
- Pujia, R.; Ferro, Y.; Maurotti, S.; Khoory, J.; Gazzaruso, C.; Pujia, A.; Montalcini, T.; Mazza, E. The Effects of COVID-19 on the Eating Habits of Children and Adolescents in Italy: A Pilot Survey Study. Nutrients 2021, 13, 2641. [Google Scholar] [PubMed]
- Sideli, L.; Lo Coco, G.; Bonfanti, R.C.; Borsarini, B.; Fortunato, L.; Sechi, C.; Micali, N. Effects of COVID-19 lockdown on eating disorders and obesity: A systematic review and meta-analysis. Eur. Eat. Disord. Rev. 2021, 29, 826–841. [Google Scholar]
- Ventura Marra, M.; Lilly, C.L.; Nelson, K.R.; Woofter, D.R.; Malone, J. A Pilot Randomized Controlled Trial of a Telenutrition Weight Loss Intervention in Middle-Aged and Older Men with Multiple Risk Factors for Cardiovascular Disease. Nutrients 2019, 11, 229. [Google Scholar]
- Ventura Marra, M.; Shotwell, M.; Nelson, K.; Malone, J. Improving Weight Status In Obese Middle-Aged And Older Men Through Telenutrition. Innov. Aging 2017, 1, 635–636. [Google Scholar]
- Davis, R.M.; Hitch, A.D.; Salaam, M.M.; Herman, W.H.; Zimmer-Galler, I.E.; Mayer-Davis, E.J. TeleHealth improves diabetes self-management in an underserved community: Diabetes TeleCare. Diabetes Care. 2010, 33, 1712–1717. [Google Scholar]
- Kelly, J.T.; Reidlinger, D.P.; Hoffmann, T.C.; Campbell, K.L. Telehealth methods to deliver dietary interventions in adults with chronic disease: A systematic review and meta-analysis. Am. J. Clin. Nutr. 2016, 104, 1693–1702. [Google Scholar] [PubMed] [Green Version]
- Rushton, A.; Edwards, A.; Bauer, J.; Bell, J.J. Dietitian assistant opportunities within the nutrition care process for patients with or at risk of malnutrition: A systematic review. Nutr. Diet. 2021, 78, 69–85. [Google Scholar] [PubMed]
- Mudge, A.M.; Ross, L.J.; Young, A.M.; Isenring, E.A.; Banks, M.D. Helping understand nutritional gaps in the elderly (HUNGER): A prospective study of patient factors associated with inadequate nutritional intake in older medical inpatients. Clin. Nutr. 2011, 30, 320–325. [Google Scholar] [PubMed] [Green Version]
- Rouget, A.; Vardon-Bounes, F.; Lorber, P.; Vavasseur, A.; Marion, O.; Marcheix, B.; Lairez, O.; Balardy, L.; Fourcade, O.; Conil, J.M.; et al. Prevalence of malnutrition in coronavirus disease 19: The NUTRICOV study. Br. J. Nutr. 2021, 126, 1296–1303. [Google Scholar]
- Bedock, D.; Bel Lassen, P.; Mathian, A.; Moreau, P.; Couffignal, J.; Ciangura, C.; Poitou-Bernert, C.; Jeannin, A.C.; Mosbah, H.; Fadlallah, J.; et al. Prevalence and severity of malnutrition in hospitalized COVID-19 patients. Clin. Nutr. ESPEN 2020, 40, 214–219. [Google Scholar]
- Technical Scientific Association of Food, Nutrition and Dietetics. Le Linee di Indirizzo per L’assistenza Nutrizionale del Paziente SARS-CoV-2 Positivo Paucisintomatico o Post-Dimissione a Domicilio o Presso Strutture Non Ospedaliere. 2020. Available online: https://www.asand.it/wp-content/uploads/2020/04/ASAND-linee-indirizzo-nutrizionale-SARS-CoV-2__.pdf (accessed on 20 January 2022).
- Tornese, G.; Schiaffini, R.; Mozzillo, E.; Franceschi, R.; Frongia, A.P.; Scaramuzza, A.; On Behalf Of Hcl Expert Pathway Pediatric Group; The Diabetes Study Group of The Italian Society for Pediatric Endocrinology. Telemedicine in the Time of the COVID-19 Pandemic: Results from the First Survey among Italian Pediatric Diabetes Centers. Healthcare 2021, 9, 815. [Google Scholar]
- Primary Health Care Research & Information Service; Raven, M.; Bywood, P. Allied Health Video Consultation Services. 2013. Available online: https://dspace.flinders.edu.au/xmlui/bitstream/handle/2328/36217/PIR_Allied%20health%20video%20consultation%20services.pdf?sequence=1&isAllowed=y (accessed on 10 February 2022).
- Kelly, J.T.; Allman-Farinelli, M.; Chen, J.; Partridge, S.R.; Collins, C.; Rollo, M.; Haslam, R.; Diversi, T.; Campbell, K.L. Dietitians Australia position statement on telehealth. Nutr. Diet. 2020, 77, 406–415. [Google Scholar]
- Kearns, J.W.; Bowerman, D.; Kemmis, K.; Izquierdo, R.E.; Wade, M.; Weinstock, R.S. Group diabetes education administered through telemedicine: Tools used and lessons learned. Telemed. J. E-Health 2012, 18, 347–353. [Google Scholar]
- Al-Awadhi, B.; Fallaize, R.; Zenun Franco, R.; Hwang, F.; Lovegrove, J.A. Insights Into the Delivery of Personalized Nutrition: Evidence From Face-To-Face and Web-Based Dietary Interventions. Front. Nutr. 2021, 7, 570531. [Google Scholar]
- Mitchell, L.J.; Ball, L.E.; Ross, L.J.; Barnes, K.A.; Williams, L.T. Effectiveness of Dietetic Consultations in Primary Health Care: A Systematic Review of Randomized Controlled Trials. J. Acad. Nutr. Diet. 2017, 117, 1941–1962. [Google Scholar]
- Ring Jacobsson, L.; Milberg, A.; Hjelm, K.; Friedrichsen, M. Gaining perspective on own illness—The lived experiences of a patient education programme for women with treated coeliac disease. J. Clin. Nurs. 2016, 2, 1229–1237. [Google Scholar]
- Marshall, A.L.; Leslie, E.R.; Bauman, A.E.; Marcus, B.H.; Owen, N. Print versus website physical activity programs: A randomized trial. Am. J. Prev. Med. 2003, 2, 88–94. [Google Scholar]
- Gogia, S.B.; Maeder, A.; Mars, M.; Hartvigsen, G.; Basu, A.; Abbott, P. Unintended Consequences of Tele Health and their Possible Solutions. Contribution of the IMIA Working Group on Telehealth. Yearb. Med. Inform. 2016, 1, 41–46. [Google Scholar]
- Matos, R.; Akutsu, R.; Zandonadi, R.P.; Rocha, A.; Botelho, R. Wellbeing at Work before and during the SARS-CoV-2 Pandemic: A Brazilian Nationwide Study among Dietitians. Int. J. Environ. Res. Public Health 2020, 17, 5541. [Google Scholar]
- Charles, B.L. Telemedicine can lower costs and improve access. Healthc. Financ. Manag. 2000, 54, 66–69. [Google Scholar]
- Chauhan, V.; Galwankar, S.; Arquilla, B.; Garg, M.; Somma, S.D.; El-Menyar, A.; Krishnan, V.; Gerber, J.; Holland, R.; Stawicki, S.P. Novel Coronavirus (COVID-19): Leveraging Telemedicine to Optimize Care While Minimizing Exposures and Viral Transmission. J. Emerg. Trauma Shock 2020, 13, 20–24. [Google Scholar]
- Zhou, X.; Snoswell, C.L.; Harding, L.E.; Bambling, M.; Edirippulige, S.; Bai, X.; Smith, A.C. The Role of Telehealth in Reducing the Mental Health Burden from COVID-19. Telemed. J. E-Health 2020, 26, 377–379. [Google Scholar]
- Koinis, A.; Giannou, V.; Drantaki, V.; Angelaina, S.; Stratou, E.; Saridi, M. The Impact of Healthcare Workers Job Environment on Their Mental-emotional Health. Coping Strategies: The Case of a Local General Hospital. Health Psychol. Res. 2015, 3, 1984. [Google Scholar]




| Characteristics | n | % |
|---|---|---|
| Age groups (years) | ||
| 20–39 | 228 | 52.3 |
| 40–59 | 167 | 38.3 |
| 60–75 | 41 | 9.4 |
| Geographical provenance | ||
| Northern Italy | 249 | 57.1 |
| Central Italy | 110 | 25.2 |
| Southern Italy | 77 | 17.7 |
| Highest degree earned | ||
| Bachelor’s Degree | 233 | 53.4 |
| Master’s Degree | 116 | 26.6 |
| 1st level University Master’s Degree | 69 | 15.8 |
| 2nd level University Master’s Degree | 11 | 2.5 |
| Academic Doctorate Degree | 7 | 1.6 |
| Member of ASAND ° | ||
| Yes | 276 | 63.3 |
| No | 160 | 36.7 |
| Current work ϭ | ||
| NHS employed | 146 | 33.5 |
| Private healthcare facility employee | 27 | 6.2 |
| Freelance | 243 | 55.7 |
| Employed by two institutes/centers # | 12 | 2.8 |
| University professor | 2 | 0.5 |
| Other | 6 | 1.3 |
| Experience as dietitian (years) | ||
| 0–10 | 185 | 42.4 |
| 11–20 | 123 | 28.2 |
| 21–30 | 75 | 17.2 |
| 31–40 | 41 | 9.4 |
| 41–50 | 12 | 2.8 |
| Focus area in which most time is spent | ||
| Artificial nutrition | 16 | 3.7 |
| Diabetes care | 50 | 11.5 |
| Disordered eating | 51 | 11.7 |
| Food and nutrition consultant | 44 | 10.1 |
| Food manager in collective catering companies | 17 | 3.9 |
| Gastroenterological support | 18 | 4.1 |
| Gerontological nutrition | 10 | 2.3 |
| Health prevention and nutrition education | 9 | 2,1 |
| Oncology | 20 | 4.6 |
| Other § | 13 | 3.0 |
| Kidney disease nutrition | 14 | 3.2 |
| Sports nutrition | 17 | 3.9 |
| Weight management | 137 | 31.4 |
| Women and pediatric nutrition | 20 | 4.6 |
| Age range of studying populations * | ||
| Older adults (age 65+) | 187 | 42.9 |
| Adults (ages 22–64) | 382 | 87.6 |
| Pregnant/postpartum women | 122 | 28 |
| Teenagers and young adults (ages 13–21) | 182 | 41.7 |
| Children (ages 6–12) | 105 | 24.1 |
| Young children (ages 1–5) | 44 | 10.1 |
| Infants | 17 | 3.9 |
| Prior to COVID-19 Pandemic | Mean ± SD | |
|---|---|---|
| Hours per week providing face-to-face nutrition care (n = 417) ≠ | 22.3 ± 12 | |
| Years of experience providing nutrition care via telehealth (n = 70) | 4.7 ± 5 | |
| During the COVID-19 pandemic | n | % |
| Targets of patients via telenutrition | ||
| Individuals | 216 | 78.5 |
| Groups | 12 | 4.4 |
| Both individuals and groups | 47 | 17.1 |
| Current modalities used to provide telenutrition | ||
| Telephone (audio only) | 47 | 17.1 |
| Audiovisual | 129 | 46.9 |
| Both telephone and audiovisual | 89 | 32.4 |
| Other § | 10 | 3.6 |
| Audiovisual options used to provide telenutrition | ||
| Audiovisual capability built into the electronic health record | 7 | 2.5 |
| Google Meet | 65 | 23.6 |
| Lifesize | 6 | 2.2 |
| Teams/Cisco WebEx Meetings/WebEx Teams | 23 | 8.4 |
| Zoom | 5 | 1.8 |
| Zoom/Google/Teams/Skype | 77 | 28.0 |
| 23 | 8.4 | |
| WhatsApp, Skype | 12 | 4.4 |
| Healthcare specialized platforms | 14 | 5.1 |
| Other # | 43 | 15.6 |
| Types of nutrition assessment and/or monitoring and evaluation conducted via telehealth * | ||
| Self-reported body measurements | 173 | 62.9 |
| Food and nutrition assessment | 233 | 84.7 |
| Evaluation of knowledge/beliefs/attitudes | 184 | 66.9 |
| Nutritional history | 227 | 82.5 |
| Behaviors | 34 | 12.4 |
| Assessment/monitoring tools | 30 | 10.9 |
| Physical activity and function | 171 | 62.2 |
| Biochemical data | 11 | 4.0 |
| Types of nutrition interventions provided via telehealth * | ||
| Coordination of nutrition care | 30 | 10.9 |
| Nutrition counseling | 220 | 80.0 |
| Nutrition education | 215 | 78.2 |
| Nutrition prescription | 109 | 39.6 |
| Nutrition supplementation | 39 | 14.2 |
| Enteral and parenteral nutrition | 27 | 9.8 |
| Groups of population-based nutrition action | 44 | 16.0 |
| No intervention | 10 | 3.6 |
| Critical issues encountered in patients during telenutrition * | ||
| Unhealthy eating habits | 10 | 3.6 |
| Eating disorders | 37 | 13.5 |
| Obstacles to care access | 5 | 1.8 |
| Emotional eating | 2 | 0.7 |
| Emotional frailty, fear, anxiety, stress, depression | 38 | 13.8 |
| Weight gain | 91 | 33.1 |
| Malnutrition | 5 | 1.8 |
| Redaction of economic possibilities | 8 | 2.9 |
| Poor compliance | 17 | 6.2 |
| Sedentary lifestyle | 44 | 16.0 |
| None | 16 | 5.8 |
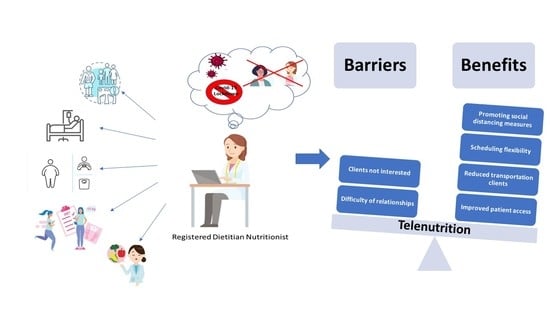
| Barriers to Providing Telenutrition * | n | % |
|---|---|---|
| Not being able to conduct or evaluate some typical assessment or monitoring/evaluation activities | 67 | 24.4 |
| Not being able to deliver some routine nutrition interventions | 24 | 8.7 |
| Not having equipment to deliver telenutrition at home | 11 | 4.0 |
| Not having remote access to the electronic health record at home | 16 | 5.8 |
| Clients not having a telephone (landline or mobile phone) | 11 | 4.0 |
| Clients not having access to the Internet | 46 | 16.7 |
| Clients not interested in receiving telenutrition | 85 | 30.9 |
| Payer(s) do not include RDNs in their provider networks | 12 | 4.4 |
| Payer(s) do not include nutrition services in their telehealth policies | 21 | 7.6 |
| Lack of employer support | 12 | 4.4 |
| Difficulty of establishing relationships/therapeutic alliance via telehealth | 66 | 24.0 |
| Discomfort with delivering nutrition care via telehealth | 24 | 8.7 |
| None | 67 | 24.4 |
| Benefits experienced by delivering telenutrition * | ||
| Improved patient access | 122 | 44.4 |
| Scheduling flexibility | 150 | 54.5 |
| Reduced transportation costs for patients/clients | 117 | 42.5 |
| Promoting compliance with social distancing measures recommended due to COVID-19 pandemic | 177 | 64.4 |
| None | 5 | 1.8 |
| Age Groups | p-value | |||
| 20–39 yrs (n = 228) | 40–59 yrs (n = 167) | 60–75 yrs (n = 41) | ||
| Providing telenutrition (%) | 70 | 56 | 56 | 0.007 |
| Geographical provenance | ||||
| Northern Italy (n = 249) | Central Italy (n = 110) | Southern Italy (n = 77) | p-value | |
| Providing telenutrition (%) | 65 | 58 | 64 | 0.56 |
| Degree earned | p-value | |||
| Bachelor’s Degree/1st Level University Master’s Degree (n = 302) | Master’s Degree (n = 116) | 2nd Level University Master’s Degree/Academic Doctorate Degree (n = 18) | ||
| Providing telenutrition (%) | 59 | 72 | 72 | 0.019 |
| Experience as RDN | p-value | |||
| 0–20 yrs (n = 308) | 21–40 yrs (n = 116) | 41–50 yrs (n = 12) | ||
| Providing telenutrition (%) | 66 | 59 | 25 | 0.005 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gnagnarella, P.; Ferro, Y.; Monge, T.; Troiano, E.; Montalcini, T.; Pujia, A.; Mazza, E. Telenutrition: Changes in Professional Practice and in the Nutritional Assessments of Italian Dietitian Nutritionists in the COVID-19 Era. Nutrients 2022, 14, 1359. https://doi.org/10.3390/nu14071359
Gnagnarella P, Ferro Y, Monge T, Troiano E, Montalcini T, Pujia A, Mazza E. Telenutrition: Changes in Professional Practice and in the Nutritional Assessments of Italian Dietitian Nutritionists in the COVID-19 Era. Nutrients. 2022; 14(7):1359. https://doi.org/10.3390/nu14071359
Chicago/Turabian StyleGnagnarella, Patrizia, Yvelise Ferro, Taira Monge, Ersilia Troiano, Tiziana Montalcini, Arturo Pujia, and Elisa Mazza. 2022. "Telenutrition: Changes in Professional Practice and in the Nutritional Assessments of Italian Dietitian Nutritionists in the COVID-19 Era" Nutrients 14, no. 7: 1359. https://doi.org/10.3390/nu14071359
APA StyleGnagnarella, P., Ferro, Y., Monge, T., Troiano, E., Montalcini, T., Pujia, A., & Mazza, E. (2022). Telenutrition: Changes in Professional Practice and in the Nutritional Assessments of Italian Dietitian Nutritionists in the COVID-19 Era. Nutrients, 14(7), 1359. https://doi.org/10.3390/nu14071359