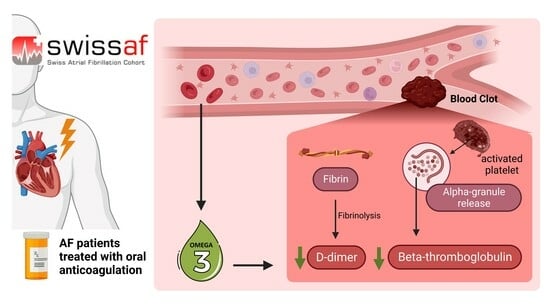
Omega-3 Fatty Acids and Markers of Thrombosis in Patients with Atrial Fibrillation
Abstract
:1. Introduction
2. Methods
2.1. Study Population
2.2. Quantification of Whole Blood n-3 FAs
2.3. Quantification of BTG and D-Dimer
2.4. Statistical Analysis
3. Results
3.1. Study Population
3.2. Association of Omega-3 Fatty Acids and D-Dimer
3.3. Association of Omega-3 Fatty Acids and Beta-Thromboglobulin
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AF | atrial fibrillation |
| ALA | alpha-linolenic acid |
| BTG | beta-thromboglobulin |
| DHA | docosahexaenoic acid |
| DPA | docosapentaenoic acid |
| EPA | eicosapentaenoic acid |
| IQR | interquartile range |
| n-3 FAs | Omega-3 fatty acids |
| SD | standard deviation |
| Swiss AF | Swiss atrial fibrillation |
References
- January, C.T.; Wann, L.S.; Calkins, H.; Chen, L.Y.; Cigarroa, J.E.; Cleveland, J.C.; Ellinor, P.T., Jr.; Ezekowitz, M.D.; Field, M.E.; Furie, K.L.; et al. 2019 AHA/ACC/HRS Focused Update of the 2014 AHA/ACC/HRS Guideline for the Management of Patients with Atrial Fibrillation: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. J. Am. Coll. Cardiol. 2019, 74, 104–132. [Google Scholar] [PubMed]
- Hindricks, G.; Potpara, T.; Dagres, N.; Arbelo, E.; Bax, J.J.; Blomstrom-Lundqvist, C.; Boriani, G.; Castella, M.; Dan, G.A.; Dilaveris, P.E.; et al. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS): The Task Force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) Developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC. Eur. Heart J. 2021, 42, 373–498. [Google Scholar] [PubMed]
- Ruff, C.T.; Giugliano, R.P.; Braunwald, E.; Hoffman, E.B.; Deenadayalu, N.; Ezekowitz, M.D.; Camm, A.J.; Weitz, J.I.; Lewis, B.S.; Parkhomenko, A.; et al. Comparison of the efficacy and safety of new oral anticoagulants with warfarin in patients with atrial fibrillation: A meta-analysis of randomised trials. Lancet 2013, 383, 955–962. [Google Scholar] [CrossRef] [PubMed]
- Gargiulo, G.; Goette, A.; Tijssen, J.; Eckardt, L.; Lewalter, T.; Vranckx, P.; Valgimigli, M. Safety and efficacy outcomes of double vs. triple antithrombotic therapy in patients with atrial fibrillation following percutaneous coronary intervention: A systematic review and meta-analysis of non-vitamin K antagonist oral anticoagulant-based randomized clinical trials. Eur. Heart J. 2019, 40, 3757–3767. [Google Scholar] [PubMed]
- Bhatt, D.L.; Steg, P.G.; Miller, M.; Brinton, E.A.; Jacobson, T.A.; Ketchum, S.B.; Doyle, R.T.; Jr Juliano, R.A.; Jiao, L.; Granowitz, C.; et al. Cardiovascular Risk Reduction with Icosapent Ethyl for Hypertriglyceridemia. N. Engl. J. Med. 2019, 380, 11–22. [Google Scholar] [CrossRef] [PubMed]
- Reiner, M.F.; Baumgartner, P.; Wiencierz, A.; Coslovsky, M.; Bonetti, N.R.; Filipovic, M.G.; Montrasio, G.; Aeschbacher, S.; Rodondi, N.; Baretella, O.; et al. The Omega-3 Fatty Acid Eicosapentaenoic Acid (EPA) Correlates Inversely with Ischemic Brain Infarcts in Patients with Atrial Fibrillation. Nutrients 2021, 13, 651. [Google Scholar] [CrossRef] [PubMed]
- Saber, H.; Yakoob, M.Y.; Shi, P.; Longstreth, W.T.; Jr Lemaitre, R.N.; Siscovick, D.; Rexrode, K.M.; Willett, W.C.; Mozaffarian, D. Omega-3 Fatty Acids and Incident Ischemic Stroke and Its Atherothrombotic and Cardioembolic Subtypes in 3 US Cohorts. Stroke 2017, 48, 2678–2685. [Google Scholar] [CrossRef]
- Wu, N.; Tong, S.; Xiang, Y.; Wu, L.; Xu, B.; Zhang, Y.; Ma, X.; Li, Y.; Song, Z.; Zhong, L. Association of hemostatic markers with atrial fibrillation: A meta-analysis and meta-regression. PLoS ONE 2015, 10, e0124716. [Google Scholar] [CrossRef]
- Adam, S.S.; Key, N.S.; Greenberg, C.S. D-dimer antigen: Current concepts and future prospects. Blood 2009, 113, 2878–2887. [Google Scholar] [CrossRef]
- Bates, S.M. D-dimer assays in diagnosis and management of thrombotic and bleeding disorders. Semin. Thromb. Hemost. 2012, 38, 673–682. [Google Scholar] [CrossRef]
- Lip, G.Y.; Lip, P.L.; Zarifis, J.; Watson, R.D.; Bareford, D.; Lowe, G.D.; Beevers, D.G. Fibrin D-dimer and beta-thromboglobulin as markers of thrombogenesis and platelet activation in atrial fibrillation. Effects of introducing ultra-low-dose warfarin and aspirin. Circulation 1996, 94, 425–431. [Google Scholar] [CrossRef] [PubMed]
- Siegbahn, A.; Oldgren, J.; Andersson, U.; Ezekowitz, M.D.; Reilly, P.A.; Connolly, S.J.; Yusuf, S.; Wallentin, L.; Eikelboom, J.W. D-dimer and factor VIIa in atrial fibrillation—Prognostic values for cardiovascular events and effects of anticoagulation therapy. A RE-LY substudy. Thromb. Haemost. 2016, 115, 921–930. [Google Scholar] [PubMed]
- Christersson, C.; Wallentin, L.; Andersson, U.; Alexander, J.H.; Ansell, J.; De Caterina, R.; Gersh, B.J.; Granger, C.B.; Hanna, M.; Horowitz, J.D.; et al. D-dimer and risk of thromboembolic and bleeding events in patients with atrial fibrillation--observations from the ARISTOTLE trial. J. Thromb. Haemost. 2014, 12, 1401–1412. [Google Scholar] [CrossRef] [PubMed]
- Choi, K.H.; Seo, W.K.; Park, M.S.; Kim, J.T.; Chung, J.W.; Bang, O.Y.; Kim, G.M.; Song, T.J.; Kim, B.J.; Heo, S.H.; et al. Baseline D-Dimer Levels as a Risk Assessment Biomarker for Recurrent Stroke in Patients with Combined Atrial Fibrillation and Atherosclerosis. J. Clin. Med. 2019, 8, 1457. [Google Scholar] [CrossRef] [PubMed]
- Kaplan, K.L.; Owen, J. Plasma levels of beta-thromboglobulin and platelet factor 4 as indices of platelet activation in vivo. Blood 1981, 57, 199–202. [Google Scholar] [CrossRef] [PubMed]
- Heppell, R.M.; Berkin, K.E.; McLenachan, J.M.; Davies, J.A. Haemostatic and haemodynamic abnormalities associated with left atrial thrombosis in non-rheumatic atrial fibrillation. Heart 1997, 77, 407–411. [Google Scholar] [CrossRef] [PubMed]
- Conen, D.; Schon, T.; Aeschbacher, S.; Pare, G.; Frehner, W.; Risch, M.; Risch, L. Genetic and phenotypic determinants of blood pressure and other cardiovascular risk factors (GAPP). Swiss Med. Wkly. 2013, 143, w13728. [Google Scholar] [CrossRef] [PubMed]
- Reiner, M.F.; Stivala, S.; Limacher, A.; Bonetti, N.R.; Mean, M.; Egloff, M.; Rodondi, N.; Aujesky, D.; von Schacky, C.; Luscher, T.F.; et al. Omega-3 fatty acids predict recurrent venous thromboembolism or total mortality in elderly patients with acute venous thromboembolism. J. Thromb. Haemost. 2017, 15, 47–56. [Google Scholar] [CrossRef]
- Kohler, A.; Bittner, D.; Low, A.; von Schacky, C. Effects of a convenience drink fortified with n-3 fatty acids on the n-3 index. Br. J. Nutr. 2010, 104, 729–736. [Google Scholar] [CrossRef]
- Vignali, D.A. Multiplexed particle-based flow cytometric assays. J. Immunol. Methods 2000, 243, 243–255. [Google Scholar] [CrossRef]
- Matsudo, M.; Aladio, J.M.; Costa, D.; Scazziota, A.S.; Swieszkowski, S.; Perez de la Hoz, R. Association of hemostasis and inflammation biomarkers with outcomes in acute coronary syndromes. Blood Coagul. Fibrinolysis 2023, 34, 179–183. [Google Scholar] [CrossRef] [PubMed]
- Tunjungputri, R.N.; van de Heijden, W.; Urbanus, R.T.; de Groot, P.G.; van der Ven, A.; de Mast, Q. Higher platelet reactivity and platelet-monocyte complex formation in Gram-positive sepsis compared to Gram-negative sepsis. Platelets 2017, 28, 595–601. [Google Scholar] [CrossRef] [PubMed]
- Adan, Y.; Shibata, K.; Sato, M.; Ikeda, I.; Imaizumi, K. Effects of docosahexaenoic and eicosapentaenoic acid on lipid metabolism, eicosanoid production, platelet aggregation and atherosclerosis in hypercholesterolemic rats. Biosci. Biotechnol. Biochem. 1999, 63, 111–119. [Google Scholar] [CrossRef] [PubMed]
- Malle, E.; Sattler, W.; Prenner, E.; Leis, H.J.; Hermetter, A.; Gries, A.; Kostner, G.M. Effects of dietary fish oil supplementation on platelet aggregability and platelet membrane fluidity in normolipemic subjects with and without high plasma Lp(a) concentrations. Atherosclerosis 1991, 88, 193–201. [Google Scholar] [CrossRef] [PubMed]
- Yoshimura, T.; Matsui, K.; Ito, M.; Yunohara, T.; Kawasaki, N.; Nakamura, T.; Okamura, H. Effects of highly purified eicosapentaenoic acid on plasma beta thromboglobulin level and vascular reactivity to angiotensin II. Artery 1987, 14, 295–303. [Google Scholar]
- Hendra, T.J.; Britton, M.E.; Roper, D.R.; Wagaine-Twabwe, D.; Jeremy, J.Y.; Dandona, P.; Haines, A.P.; Yudkin, J.S. Effects of fish oil supplements in NIDDM subjects. Controlled study. Diabetes Care 1990, 13, 821–829. [Google Scholar] [CrossRef]
- Leng, G.C.; Smith, F.B.; Fowkes, F.G.; Horrobin, D.F.; Ells, K.; Morse-Fisher, N.; Lowe, G.D. Relationship between plasma essential fatty acids and smoking, serum lipids, blood pressure and haemostatic and rheological factors. Prostaglandins Leukot. Essent. Fat. Acids 1994, 51, 101–108. [Google Scholar] [CrossRef]
- Park, Y.; Harris, W. EPA, but not DHA, decreases mean platelet volume in normal subjects. Lipids 2002, 37, 941–946. [Google Scholar] [CrossRef]
- Stivala, S.; Sorrentino, S.; Gobbato, S.; Bonetti, N.R.; Camici, G.G.; Luscher, T.F.; Medalia, O.; Beer, J.H. Glycoprotein Ib clustering in platelets can be inhibited by alpha-linolenic acid as revealed by cryo-electron tomography. Haematologica 2020, 105, 1660–1666. [Google Scholar] [CrossRef]
- Phang, M.; Scorgie, F.E.; Seldon, M.; Garg, M.L.; Lincz, L.F. Reduction of prothrombin and Factor V levels following supplementation with omega-3 fatty acids is sex dependent: A randomised controlled study. J. Nutr. Biochem. 2014, 25, 997–1002. [Google Scholar] [CrossRef]
- Zhang, Y.; Ding, J.; Guo, H.; Liang, J.; Li, Y. Associations of Fish and Omega-3 Fatty Acids Consumption With the Risk of Venous Thromboembolism. A Meta-Analysis of Prospective Cohort Studies. Front. Nutr. 2020, 7, 614784. [Google Scholar] [CrossRef] [PubMed]
- Bork, C.S.; Veno, S.K.; Lundbye-Christensen, S.; Jakobsen, M.U.; Tjonneland, A.; Schmidt, E.B.; Overvad, K. Dietary Intake of alpha-Linolenic Acid Is Not Appreciably Associated with Risk of Ischemic Stroke among Middle-Aged Danish Men and Women. J. Nutr. 2018, 148, 952–958. [Google Scholar] [CrossRef] [PubMed]
- Bork, C.S.; Veno, S.K.; Lundbye-Christensen, S.; Jakobsen, M.U.; Tjonneland, A.; Calder, P.C.; Overvad, K.; Schmidt, E.B. Adipose tissue content of alpha-linolenic acid and the risk of ischemic stroke and ischemic stroke subtypes: A Danish case-cohort study. PLoS ONE 2018, 13, e0198927. [Google Scholar] [CrossRef] [PubMed]
- Gencer, B.; Djousse, L.; Al-Ramady, O.T.; Cook, N.R.; Manson, J.E.; Albert, C.M. Effect of Long-Term Marine ɷ-3 Fatty Acids Supplementation on the Risk of Atrial Fibrillation in Randomized Controlled Trials of Cardiovascular Outcomes: A Systematic Review and Meta-Analysis. Circulation 2021, 144, 1981–1990. [Google Scholar] [CrossRef] [PubMed]
- Qian, F.; Tintle, N.; Jensen, P.N.; Lemaitre, R.N.; Imamura, F.; Feldreich, T.R.; Nomura, S.O.; Guan, W.; Laguzzi, F.; Kim, E.; et al. Omega-3 Fatty Acid Biomarkers and Incident Atrial Fibrillation. J. Am. Coll. Cardiol. 2023, 82, 336–349. [Google Scholar] [CrossRef] [PubMed]
- Baumgartner, P.; Reiner, M.F.; Wiencierz, A.; Coslovsky, M.; Bonetti, N.R.; Filipovic, M.G.; Aeschbacher, S.; Kuhne, M.; Zuern, C.S.; Rodondi, N.; et al. Omega-3 Fatty Acids and Heart Rhythm, Rate, and Variability in Atrial Fibrillation. J. Am. Heart Assoc. 2023, 12, e027646. [Google Scholar] [CrossRef]
- Lombardi, M.; Chiabrando, J.G.; Vescovo, G.M.; Bressi, E.; Del Buono, M.G.; Carbone, S.; Koenig, R.A.; Van Tassell, B.W.; Abbate, A.; Biondi-Zoccai, G.; et al. Impact of Different Doses of Omega-3 Fatty Acids on Cardiovascular Outcomes: A Pairwise and Network Meta-analysis. Curr. Atheroscler. Rep. 2020, 22, 45. [Google Scholar] [CrossRef]
- Olshansky, B.; Bhatt, D.L.; Miller, M.; Steg, P.G.; Brinton, E.A.; Jacobson, T.A.; Ketchum, S.B.; Doyle, R.T.; Juliano, R.A., Jr.; Jiao, L.; et al. Cardiovascular Benefits of Icosapent Ethyl in Patients With and Without Atrial Fibrillation in REDUCE-IT. J. Am. Heart Assoc. 2023, 12, e026756. [Google Scholar] [CrossRef]
- Ruff, C.T.; Giugliano, R.P.; Braunwald, E.; Murphy, S.A.; Brown, K.; Jarolim, P.; Mercuri, M.; Antman, E.M.; Morrow, D.A. Cardiovascular Biomarker Score and Clinical Outcomes in Patients With Atrial Fibrillation: A Subanalysis of the ENGAGE AF-TIMI 48 Randomized Clinical Trial. JAMA Cardiol. 2016, 1, 999–1006. [Google Scholar] [CrossRef]
- Harris, W.S.; Pottala, J.V.; Varvel, S.A.; Borowski, J.J.; Ward, J.N.; McConnell, J.P. Erythrocyte omega-3 fatty acids increase and linoleic acid decreases with age: Observations from 160,000 patients. Prostaglandins Leukot. Essent. Fat. Acids 2013, 88, 257–263. [Google Scholar] [CrossRef]
- Connolly, S.; Pogue, J.; Hart, R.; Pfeffer, M.; Hohnloser, S.; Chrolavicius, S.; Pfeffer, M.; Hohnloser, S.; Yusuf, S. Clopidogrel plus aspirin versus oral anticoagulation for atrial fibrillation in the Atrial fibrillation Clopidogrel Trial with Irbesartan for prevention of Vascular Events (ACTIVE W): A randomised controlled trial. Lancet 2006, 367, 1903–1912. [Google Scholar] [PubMed]
- Stroke Prevention in Atrial Fibrillation Study. Final results. Circulation 1991, 84, 527–539. [Google Scholar]

| Baseline Characteristics of D-Dimer Study Population, n = 1096 | |
|---|---|
| Mean age (SD) | 74.9 (8.4) |
| Female (%) | 291 (26.6) |
| Median body mass index (IQR) | 27.2 (24.4, 30.8) |
| Physical activity (%) | 424 (38.7) |
| Smoker (%) | |
| Never | 474 (43.2) |
| Past | 535 (48.8) |
| Active | 85 (7.8) |
| Median alcohol units per day (IQR) | 0.4 (0.1, 1.2) |
| AF type (%) | |
| Paroxysmal | 483 (44.1) |
| Persistent | 310 (28.3) |
| Permanent | 303 (27.6) |
| Hypertension (%) | 805 (73.4) |
| Diabetes mellitus (%) | 238 (21.7) |
| Chronic kidney disease (%) | 315 (28.7) |
| Cancer (%) | 192 (17.5) |
| Stroke (%) | 155 (14.1) |
| Transient ischemic attack (%) | 107 (9.8) |
| Heart failure (%) | 355 (32.4) |
| Coronary artery disease (%) | 399 (36.4) |
| Major bleeding (%) | 99 (9.0) |
| Aspirin (%) | 262 (23.9) |
| Statin (%) | 557 (50.8) |
| P2Y12 inhibitor (%) | 79 (7.2) |
| Type of anticoagulation | |
| Novel oral anticoagulants (%) | 499 (45.5) |
| Vitamin K antagonist (%) | 417 (38.0) |
| None (%) | 180 (16.4) |
| Baseline Characteristics Beta-Thromboglobulin Study Population, n = 2371 | |
|---|---|
| Mean age (SD) | 73.2 (8.4) |
| Female (%) | 644 (27.2) |
| Median body mass index (IQR) | 27.0 (24.4, 30.3) |
| Physical activity (%) | 1093 (46.1) |
| Smoker (%) | |
| Never | 1038 (43.8) |
| Past | 1158 (48.8) |
| Active | 173 (7.3) |
| Median alcohol units per day (IQR) | 0.5 (0.1, 1.3) |
| AF type (%) | |
| Paroxysmal | 1058 (44.6) |
| Persistent | 724 (30.5) |
| Permanent | 589 (24.8) |
| Hypertension (%) | 1653 (69.7) |
| Diabetes mellitus (%) | 413 (17.4) |
| Chronic kidney disease (%) | 502 (21.2) |
| Cancer (%) | 383 (16.2) |
| Stroke (%) | 312 (13.2) |
| Transient ischemic attack (%) | 213 (9.0) |
| Heart failure (%) | 618 (26.1) |
| Coronary artery disease (%) | 716 (30.2) |
| Major bleeding (%) | 148 (6.2) |
| Aspirin (%) | 395 (16.7) |
| Statin (%) | 1169 (49.3) |
| P2Y12 inhibitor (%) | 146 (6.2) |
| Type of anticoagulation | |
| Novel oral anticoagulants (%) | 1209 (51.0) |
| Vitamin K antagonist (%) | 934 (39.4) |
| None (%) | 228 (9.6) |
| Overall Population, n = 2373 | Mean Fatty Acid Fraction, % (SD) |
|---|---|
| Total Omega-3 fatty acids | 6.0 (1.2) |
| Eicosapentaenoic acid (EPA) | 0.8 (0.3) |
| Docosahexaenoic acid (DHA) | 3.3 (0.8) |
| Docosapentaenoic acid (DPA) | 1.7 (0.3) |
| Alpha-linolenic acid (ALA) | 0.2 (0.1) |
| Association of Omega-3 Fatty Acids with D-Dimer | ||||||
|---|---|---|---|---|---|---|
| Omega-3 Fatty Acid | Model 1, n = 1096 | Model 2, n = 1090 | Model 3, n = 1088 | |||
| Coefficient (Cl) | p-value | Coefficient (Cl) | p-value | Coefficient (Cl) | p-value | |
| Total Omega-3 fatty acids | 0.93 (0.89–0.97) | <0.001 | 0.93 (0.89–0.97) | 0.001 | 0.94 (0.90–0.98) | 0.004 |
| Eicosapentaenoic acid (EPA) | 0.88 (0.73–1.06) | 0.185 | 0.92 (0.76–1.11) | 0.398 | 0.91 (0.76–1.10) | 0.336 |
| Docosahexaenoic acid (DHA) | 0.94 (0.88–1.01) | 0.099 | 0.94 (0.88–1.00) | 0.060 | 0.95 (0.89–1.01) | 0.124 |
| Docosapentaenoic acid (DPA) | 0.95 (0.80–1.14) | 0.591 | 0.92 (0.77–1.10) | 0.379 | 0.93 (0.78–1.12) | 0.452 |
| Alpha-linolenic acid(ALA) | 0.88 (0.58–1.34) | 0.552 | 0.87 (0.57–1.32) | 0.508 | 0.95 (0.63–1.45) | 0.827 |
| Association of Omega-3 Fatty Acids with Beta-thromboglobulin (BTG) | ||||||
|---|---|---|---|---|---|---|
| Omega-3 fatty acid | Model 1, n = 2371 | Model 2, n = 2365 | Model 3, n = 2339 | |||
| Coefficient (Cl) | p-value | Coefficient (Cl) | p-value | Coefficient (Cl) | p-value | |
| Total Omega-3 fatty acids | 0.97 (0.96–0.99) | 0.004 | 0.97 (0.95–0.99) | 0.001 | 0.97 (0.95–0.99) | 0.003 |
| Eicosapentaenoic acid (EPA) | 1.11 (1.02–1.20) | 0.015 | 1.12 (1.03–1.22) | 0.007 | 1.12 (1.03–1.22) | 0.010 |
| Docosahexaenoic acid (DHA) | 0.95 (0.92–0.97) | <0.001 | 0.94 (0.91–0.97) | <0.001 | 0.94 (0.92–0.97) | <0.001 |
| Docosapentaenoic acid (DPA) | 0.93 (0.86–1.00) | 0.053 | 0.91 (0.84–0.98) | 0.018 | 0.91 (0.84–0.98) | 0.019 |
| Alpha-linolenic acid (ALA) | 0.86 (0.71–1.03) | 0.100 | 0.83 (0.69–1.00) | 0.055 | 0.83 (0.69–1.01) | 0.060 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Reiner, M.F.; Bertschi, D.A.; Werlen, L.; Wiencierz, A.; Aeschbacher, S.; Lee, P.; Rodondi, N.; Moutzouri, E.; Bonati, L.; Reichlin, T.; et al. Omega-3 Fatty Acids and Markers of Thrombosis in Patients with Atrial Fibrillation. Nutrients 2024, 16, 178. https://doi.org/10.3390/nu16020178
Reiner MF, Bertschi DA, Werlen L, Wiencierz A, Aeschbacher S, Lee P, Rodondi N, Moutzouri E, Bonati L, Reichlin T, et al. Omega-3 Fatty Acids and Markers of Thrombosis in Patients with Atrial Fibrillation. Nutrients. 2024; 16(2):178. https://doi.org/10.3390/nu16020178
Chicago/Turabian StyleReiner, Martin F., Daniela A. Bertschi, Laura Werlen, Andrea Wiencierz, Stefanie Aeschbacher, Pratintip Lee, Nicolas Rodondi, Elisavet Moutzouri, Leo Bonati, Tobias Reichlin, and et al. 2024. "Omega-3 Fatty Acids and Markers of Thrombosis in Patients with Atrial Fibrillation" Nutrients 16, no. 2: 178. https://doi.org/10.3390/nu16020178
APA StyleReiner, M. F., Bertschi, D. A., Werlen, L., Wiencierz, A., Aeschbacher, S., Lee, P., Rodondi, N., Moutzouri, E., Bonati, L., Reichlin, T., Moschovitis, G., Rutishauser, J., Kühne, M., Osswald, S., Conen, D., & Beer, J. H. (2024). Omega-3 Fatty Acids and Markers of Thrombosis in Patients with Atrial Fibrillation. Nutrients, 16(2), 178. https://doi.org/10.3390/nu16020178