Acute Toxic Effects of Tetrodotoxin in Mice via Intramuscular Injection and Oral Gavage
Abstract
:1. Introduction
2. Results
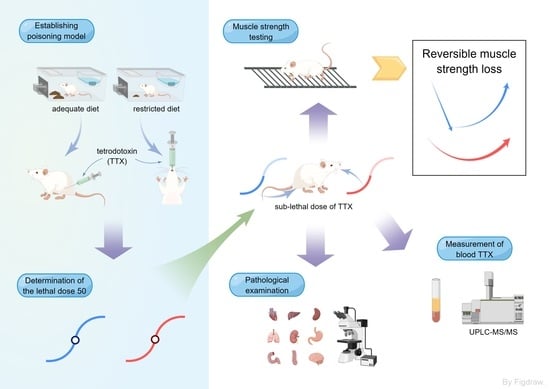
2.1. TTX Poisoning Models
2.2. Acute Toxicity of TTX
2.3. TTX Concentration in Blood following i.m. and o.g. Administration
2.4. Muscle Strength Changes after TTX Poisoning
2.5. Pathological Examination
3. Discussion
4. Conclusions
5. Materials and Methods
5.1. Reagents
5.2. Animals and Poisoning Model
5.3. Experimental Design
5.3.1. Determination of the Lethal Dose 50 (LD50)
5.3.2. Blood Sample Collection and Measurement of Blood TTX
5.3.3. Muscle-Strength Testing
5.3.4. Experimental Conditions
5.4. Statistical Analysis
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Katikou, P.; Gokbulut, C.; Kosker, A.R.; Campàs, M.; Ozogul, F. An updated review of tetrodotoxin and its peculiarities. Mar. Drugs 2022, 20, 47. [Google Scholar] [CrossRef] [PubMed]
- Lago, J.; Rodríguez, L.P.; Blanco, L.; Vieites, J.M.; Cabado, A.G. Tetrodotoxin, an extremely potent marine neurotoxin: Distribution, toxicity, origin and therapeutical uses. Mar. Drugs 2015, 13, 6384–6406. [Google Scholar] [CrossRef]
- Liu, S.; Tseng, C.; Lin, C. Is neostigmine effective in severe pufferfish-associated tetrodotoxin poisoning? Clin. Toxicol. 2015, 53, 13–21. [Google Scholar] [CrossRef]
- Magarlamov, T.; Melnikova, D.; Chernyshev, A. Tetrodotoxin-producing bacteria: Detection, distribution and migration of the toxin in aquatic systems. Toxins 2017, 9, 166. [Google Scholar] [CrossRef] [PubMed]
- Lorentz, M.N.; Stokes, A.N.; Rößler, D.C.; Lötters, S. Tetrodotoxin. Curr. Biol. 2016, 26, R870–R872. [Google Scholar] [CrossRef]
- Makarova, M.; Rycek, L.; Hajicek, J.; Baidilov, D.; Hudlicky, T. Tetrodotoxin: History, biology, and synthesis. Angew. Chem. Int. Ed. Engl. 2019, 58, 18338–18387. [Google Scholar] [CrossRef] [PubMed]
- Biessy, L.; Boundy, M.J.; Smith, K.F.; Harwood, D.T.; Hawes, I.; Wood, S.A. Tetrodotoxin in marine bivalves and edible gastropods: A mini-review. Chemosphere 2019, 236, 124404. [Google Scholar] [CrossRef] [PubMed]
- Antonelli, P.; Salerno, B.; Bordin, P.; Peruzzo, A.; Orsini, M.; Arcangeli, G.; Barco, L.; Losasso, C. Tetrodotoxin in live bivalve mollusks from Europe: Is it to be considered an emerging concern for food safety? Compr. Rev. Food Sci. Food Saf. 2022, 21, 719–737. [Google Scholar] [CrossRef]
- Zhao, C.; Liu, A.; Santamaria, C.M.; Shomorony, A.; Ji, T.; Wei, T.; Gordon, A.; Elofsson, H.; Mehta, M.; Yang, R.; et al. Polymer-tetrodotoxin conjugates to induce prolonged duration local anesthesia with minimal toxicity. Nat. Commun. 2019, 10, 2566. [Google Scholar] [CrossRef]
- Hong, B.; He, J.; Le, Q.; Bai, K.; Chen, Y.; Huang, W. Combination formulation of tetrodotoxin and lidocaine as a potential therapy for severe arrhythmias. Mar. Drugs 2019, 17, 685. [Google Scholar] [CrossRef]
- Hong, B.; He, J.; Sun, J.; Le, Q.; Bai, K.; Mou, Y.; Zhang, Y.; Chen, W.; Huang, W. Analgesia effect of enteric sustained-release tetrodotoxin pellets in the rat. Pharmaceutics 2020, 12, 32. [Google Scholar] [CrossRef] [PubMed]
- Konrad, D.B.; Rühmann, K.; Ando, H.; Hetzler, B.E.; Strassner, N.; Houk, K.N.; Matsuura, B.S.; Trauner, D. A concise synthesis of tetrodotoxin. Science 2022, 377, 411–415. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Han, C.; Chen, S.; Li, L.; Zong, J.; Zeng, J.; Mei, G. Response surface methodology for the optimization of ultrasound-assisted extraction of tetrodotoxin from the liver of Takifugu pseudommus. Toxins 2018, 10, 529. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Zhang, X.; Ye, Y.; Li, X.; Gu, Y.; Yun, L. Awareness on tetrodotoxin of illegal activity: Forensic issue from a rare homicide case report and literature review. J. Forensic Leg. Med. 2021, 79, 102152. [Google Scholar] [CrossRef]
- Xu, Q.; Huang, K.; Gao, L.; Zhang, H.; Rong, K. Toxicity of tetrodotoxin towards mice and rabbits. J. Hyg. Res. 2003, 32, 371–374. [Google Scholar]
- Shefner, J.M. Strength testing in motor neuron diseases. Neurotherapeutics 2017, 14, 154–160. [Google Scholar] [CrossRef] [PubMed]
- Stevens, M.; Peigneur, S.; Tytgat, J. Neurotoxins and their binding areas on voltage-gated sodium channels. Front. Pharmacol. 2011, 2, 71. [Google Scholar] [CrossRef]
- Shen, H.; Li, Z.; Jiang, Y.; Pan, X.; Wu, J.; Cristofori-Armstrong, B.; Smith, J.J.; Chin, Y.K.Y.; Lei, J.; Zhou, Q.; et al. Structural basis for the modulation of voltage-gated sodium channels by animal toxins. Science 2018, 362, eaau2596. [Google Scholar] [CrossRef]
- Zimmer, T. Effects of tetrodotoxin on the mammalian cardiovascular system. Mar. Drugs 2010, 8, 741–762. [Google Scholar] [CrossRef]
- Melnikova, D.I.; Khotimchenko, Y.S.; Magarlamov, T.Y. Addressing the issue of tetrodotoxin targeting. Mar. Drugs 2018, 16, 352. [Google Scholar] [CrossRef]
- Hong, B.; Chen, H.; Han, J.; Xie, Q.; He, J.; Bai, K.; Dong, Y.; Yi, R. A study of 11-[³H]-tetrodotoxin absorption, distribution, metabolism and excretion (ADME) in adult Sprague-Dawley rats. Mar. Drugs 2017, 15, 159. [Google Scholar] [CrossRef]
- Alhatali, B.; Al Lawatia, S.; Khamis, F.; Kantur, S.; Al-Abri, S.; Kapil, V.; Thomas, J.; Johnson, R.; Hamelin, E.I.; Coleman, R.M.; et al. A cluster of tetrodotoxin poisoning in Oman. Clin. Toxicol. 2021, 60, 262–266. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Fígares, M.; Fernández, V.; Postigo, M.J.; Feron, P. Acute paralysis after seafood ingestion. Neurophysiol. Clin. 2013, 43, 299–302. [Google Scholar] [CrossRef] [PubMed]
- Kakehi, E.; Matsumoto, M.; Taniguchi, S.; Akamatsu, Y.; Sakurai, S.; Hirotani, A.; Nozaki, T.; Shoji, K.; Adachi, S.; Kotani, K.; et al. Reversible cerebral vasoconstriction syndrome associated with tetrodotoxin poisoning: A case report. J. Am. Coll. Emerg. Physicians Open 2021, 2, e12627. [Google Scholar] [CrossRef]
- Lan, M.Y.; Lai, S.L.; Chen, S.S.; Hwang, D.F. Tetrodotoxin intoxication in a uraemic patient. J. Neurol. Neurosurg. Psychiatry 1999, 67, 127–128. [Google Scholar] [CrossRef]
- Abal, P.; Louzao, M.C.; Antelo, A.; Alvarez, M.; Cagide, E.; Vilariño, N.; Vieytes, M.R.; Botana, L.M. Acute oral toxicity of tetrodotoxin in mice: Determination of lethal dose 50 (LD50) and no observed adverse effect Level (NOAEL). Toxins 2017, 9, 75. [Google Scholar] [CrossRef]
- Abal, P.; Louzao, M.C.; Vilariño, N.; Vieytes, M.R.; Botana, L.M. Acute toxicity assessment: Macroscopic and ultrastructural effects in mice treated with oral tetrodotoxin. Toxins 2019, 11, 305. [Google Scholar] [CrossRef] [PubMed]
- OECD. Test No. 425: Acute oral toxicity: Up-and-Down procedure. In OECD Guidelines for the Testing of Chemicals; OECD Publishing: Paris, France, 2022. [Google Scholar] [CrossRef]
- Boente-Juncal, A.; Vale, C.; Cifuentes, M.; Otero, P.; Camiña, M.; Rodriguez-Vieytes, M.; Botana, L.M. Chronic in vivo effects of repeated exposure to low oral doses of tetrodotoxin: Preliminary evidence of nephrotoxicity and cardiotoxicity. Toxins 2019, 11, 96. [Google Scholar] [CrossRef] [PubMed]







| Dose (μg/kg) | Toxic Symptoms | Mortality | |
|---|---|---|---|
| Apathy | Seizures | ||
| Intramuscular injection | |||
| 10 | 10/10 | 10/10 | 10/10 |
| 9 | 10/10 | 5/10 | 5/10 |
| 8 | 10/10 | 4/10 | 4/10 |
| 7 | 10/10 | 0/10 | 0/10 |
| 6 | 10/10 | 0/10 | 0/10 |
| Oral gavage | |||
| 600 | 10/10 | 10/10 | 10/10 |
| 500 | 10/10 | 8/10 | 8/10 |
| 400 | 10/10 | 6/10 | 6/10 |
| 325 | 10/10 | 3/10 | 3/10 |
| 250 | 10/10 | 0/10 | 0/10 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, F.; Zhang, F.; Song, J.; Zou, S.; Li, J.; Huang, Y.; Zhang, L.; Wang, Q. Acute Toxic Effects of Tetrodotoxin in Mice via Intramuscular Injection and Oral Gavage. Toxins 2023, 15, 334. https://doi.org/10.3390/toxins15050334
Wang F, Zhang F, Song J, Zou S, Li J, Huang Y, Zhang L, Wang Q. Acute Toxic Effects of Tetrodotoxin in Mice via Intramuscular Injection and Oral Gavage. Toxins. 2023; 15(5):334. https://doi.org/10.3390/toxins15050334
Chicago/Turabian StyleWang, Fan, Fuhai Zhang, Juxingsi Song, Shuaijun Zou, Jie Li, Yichao Huang, Liming Zhang, and Qianqian Wang. 2023. "Acute Toxic Effects of Tetrodotoxin in Mice via Intramuscular Injection and Oral Gavage" Toxins 15, no. 5: 334. https://doi.org/10.3390/toxins15050334
APA StyleWang, F., Zhang, F., Song, J., Zou, S., Li, J., Huang, Y., Zhang, L., & Wang, Q. (2023). Acute Toxic Effects of Tetrodotoxin in Mice via Intramuscular Injection and Oral Gavage. Toxins, 15(5), 334. https://doi.org/10.3390/toxins15050334