Polyester Polymeric Nanoparticles as Platforms in the Development of Novel Nanomedicines for Cancer Treatment
Abstract
:Simple Summary
Abstract
1. Introduction
2. From Raw Materials to Polymeric NPs
2.1. PLA
2.2. PGA
2.3. PLGA
2.4. PCL
2.5. Other Synthetic Polymers
3. Mechanism of Action of Polymeric NPs
3.1. Stage I
3.2. Stage II
3.3. Stage III
3.4. The Release of the Therapeutic Depends on Many Factors
3.4.1. Cellular and Intracellular Barriers
3.4.2. Crystallinity
3.4.3. Hydrophilic/Hydrophobic Ratio
3.4.4. Degradability
3.4.5. Type of Surfactants
3.5. Systemic Administration of Polymeric NPs Is Common for Cancer Treatment
4. Methods to Formulate Polymeric NPs
4.1. Simple Nano-Emulsion (Top-Down)
4.2. Double or Multiple Nano-Emulsion (Top-Down)
4.3. Salting Out (Top-Down)
4.4. Nanoprecipitation and Displacement Solvent Method (Top-Down)
4.5. Electrosprying (Top-Down)
4.6. Microfluids (Top-Down)
4.7. Emulsion Polymerization (Bottom-Up)
4.8. Interfacial Polymerization (Bottom-Up)
5. Polymeric NPs in Clinical Investigations
6. Guided and Smart NPs
7. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Binnig, G.; Quate, C.F.; Gerber, C. Atomic Force Microscope. Phys. Rev. Lett. 1986, 56, 930–933. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Drexler, K.; Peterson, C.L.; Pergamit, G. Unbounding the Future: The Nanotechnology Revolution; William Morrow and Company, Inc.: New York, NY, USA, 1991. [Google Scholar]
- Freitas, R.A. What Is Nanomedicine? Nanomed. Nanotechnol. Biol. Med. 2005, 1, 2–9. [Google Scholar] [CrossRef] [PubMed]
- Kreuter, J. Nanoparticles—A historical perspective. Int. J. Pharm. 2007, 331, 1–10. [Google Scholar] [CrossRef]
- Kulkarni, R.K.; Moore, E.G.; Hegyeli, A.F.; Leonard, F. Biodegradable Poly(Lactic Acid) Polymers. J. Biomed. Mater. Res. 1971, 5, 169–181. [Google Scholar] [CrossRef] [PubMed]
- Köhler, G.; Milstein, C. Continuous Cultures of Fused Cells Secreting Antibody of Predefined Specificity. Nature 1975, 256, 495–497. [Google Scholar] [CrossRef]
- Abbasi, E.; Aval, S.F.; Akbarzadeh, A.; Milani, M.; Nasrabadi, H.T.; Joo, S.W.; Hanifehpour, Y.; Nejati-Koshki, K.; Pashaei-Asl, R. Dendrimers: Synthesis, Applications, and Properties. Nanoscale Res. Lett. 2014, 9, 247. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Santini, J.T.; Cima, M.J.; Langer, R. A Controlled-Release Microchip. Nature 1999, 397, 335–338. [Google Scholar] [CrossRef] [PubMed]
- Langer, R.; Vacanti, J.P. Tissue Engineering. Science 1993, 260, 920–926. [Google Scholar] [CrossRef] [Green Version]
- Barenholz, Y. Doxil®—The First FDA-Approved Nano-Drug: Lessons Learned. J. Control. Release 2012, 160, 117–134. [Google Scholar] [CrossRef] [PubMed]
- Zingg, R.; Fischer, M. The Consolidation of Nanomedicine. Wiley Interdiscip. Rev. Nanomed. Nanobiotechnol. 2019, 11, e1569. [Google Scholar] [CrossRef] [Green Version]
- Shi, J.; Votruba, A.R.; Farokhzad, O.C.; Langer, R. Nanotechnology in Drug Delivery and Tissue Engineering: From Discovery to Applications. Nano Lett. 2010, 10, 3223–3230. [Google Scholar] [CrossRef] [Green Version]
- Jain, K.K. Nanodiagnostics: Application of Nanotechnology in Molecular Diagnostics. Expert Rev. Mol. Diagn. 2003, 3, 153–161. [Google Scholar] [CrossRef]
- Bonam, S.R.; Kotla, N.G.; Bohara, R.A.; Rochev, Y.; Webster, T.J.; Bayry, J. Potential Immuno-Nanomedicine Strategies to Fight COVID-19 like Pulmonary Infections. Nano Today 2021, 36, 101051. [Google Scholar] [CrossRef]
- Rana, M.M. Polymer-Based Nano-Therapies to Combat COVID-19 Related Respiratory Injury: Progress, Prospects, and Challenges. J. Biomater. Sci. Polym. Ed. 2021, 32, 1219–1249. [Google Scholar] [CrossRef]
- Windmiller, J.R.; Wang, J. Wearable Electrochemical Sensors and Biosensors: A Review. Electroanalysis 2013, 25, 29–46. [Google Scholar] [CrossRef]
- Madurantakam, P.A.; Cost, C.P.; Simpson, D.G.; Bowlin, G.L. Science of Nanofibrous Scaffold Fabrication: Strategies for next Generation Tissue-Engineering Scaffolds. Future Med. 2009, 4, 193–206. [Google Scholar] [CrossRef] [PubMed]
- Seruga, B.; Ocana, A.; Tannock, I.F. Drug Resistance in Metastatic Castration-Resistant Prostate Cancer; Nature Publishing Group: Berlin, Germany, 2011; Volume 8. [Google Scholar]
- Scheetz, L.; Park, K.S.; Li, Q.; Lowenstein, P.R.; Castro, M.G.; Schwendeman, A.; Moon, J.J. Engineering Patient-Specific Cancer Immunotherapies. Nat. Biomed. Eng. 2019, 3, 768–782. [Google Scholar] [CrossRef]
- Brannon-Peppas, L.; Blanchette, J.O. Nanoparticle and Targeted Systems for Cancer Therapy. Adv. Drug Deliv. Rev. 2012, 64, 206–212. [Google Scholar] [CrossRef]
- Fenton, O.S.; Olafson, K.N.; Pillai, P.S.; Mitchell, M.J.; Langer, R. Advances in Biomaterials for Drug Delivery. Adv. Mater. 2018, 30, 1705328. [Google Scholar] [CrossRef]
- Cheng, Q.; Wei, T.; Farbiak, L.; Johnson, L.T.; Dilliard, S.A.; Siegwart, D.J. Selective Organ Targeting (SORT) Nanoparticles for Tissue-Specific MRNA Delivery and CRISPR–Cas Gene Editing. Nat. Nanotechnol. 2020, 15, 313–320. [Google Scholar] [CrossRef] [PubMed]
- Huang, H.-C.; Barua, S.; Sharma, G.; Dey, S.K.; Rege, K. Inorganic Nanoparticles for Cancer Imaging and Therapy. J. Control. Release 2011, 155, 344–357. [Google Scholar] [CrossRef]
- Aguado, B.A.; Grim, J.C.; Rosales, A.M.; Watson-Capps, J.J.; Anseth, K.S. Engineering Precision Biomaterials for Personalized Medicine. Sci. Transl. Med. 2018, 10. [Google Scholar] [CrossRef]
- Gagliardi, A.; Giuliano, E.; Venkateswararao, E.; Fresta, M.; Bulotta, S.; Awasthi, V.; Cosco, D. Biodegradable Polymeric Nanoparticles for Drug Delivery to Solid Tumors. Front. Pharm. 2021, 12. [Google Scholar] [CrossRef] [PubMed]
- Sun, L.; Wu, Q.; Peng, F.; Liu, L.; Gong, C. Strategies of Polymeric Nanoparticles for Enhanced Internalization in Cancer Therapy. Colloids Surf. B Biointerfaces 2015, 135, 56–72. [Google Scholar] [CrossRef]
- Liu, Y.; Chen, Z.; Liu, C.; Yu, D.; Lu, Z.; Zhang, N. Gadolinium-Loaded Polymeric Nanoparticles Modified with Anti-VEGF as Multifunctional MRI Contrast Agents for the Diagnosis of Liver Cancer. Biomaterials 2011, 32, 5167–5176. [Google Scholar] [CrossRef] [PubMed]
- Niza, E.; Nieto-Jiménez, C.; Noblejas-López, M.d.M.; Bravo, I.; Castro-Osma, J.A.; De La Cruz-Martínez, F.; Martínez de Sarasa Buchaca, M.; Posadas, I.; Canales-Vázquez, J.; Lara-Sanchez, A. Poly (Cyclohexene Phthalate) Nanoparticles for Controlled Dasatinib Delivery in Breast Cancer Therapy. Nanomaterials 2019, 9, 1208. [Google Scholar] [CrossRef] [Green Version]
- Gu, F.X.; Karnik, R.; Wang, A.Z.; Alexis, F.; Levy-Nissenbaum, E.; Hong, S.; Langer, R.S.; Farokhzad, O.C. Targeted Nanoparticles for Cancer Therapy. Nano Today 2007, 2, 14–21. [Google Scholar] [CrossRef]
- Valcourt, D.M.; Dang, M.N.; Scully, M.A.; Day, E.S. Nanoparticle-Mediated Co-Delivery of Notch-1 Antibodies and ABT-737 as a Potent Treatment Strategy for Triple-Negative Breast Cancer. ACS Nano 2020, 14, 3378–3388. [Google Scholar] [CrossRef]
- Jia, R.; Teng, L.; Gao, L.; Su, T.; Fu, L.; Qiu, Z.; Bi, Y. Advances in Multiple Stimuli-Responsive Drug-Delivery Systems for Cancer Therapy. Int. J. Nanomed. 2021, 16, 1525–1551. [Google Scholar] [CrossRef]
- Zhao, X.; Bai, J.; Yang, W. Stimuli-Responsive Nanocarriers for Therapeutic Applications in Cancer. Cancer Biol. Med. 2021, 18, 319–335. [Google Scholar] [CrossRef]
- Anselmo, A.C.; Mitragotri, S. Nanoparticles in the Clinic: An Update. Bioeng. Transl. Med. 2019, 4, e10143. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kamaly, N.; Yameen, B.; Wu, J.; Farokhzad, O.C. Degradable Controlled-Release Polymers and Polymeric Nanoparticles: Mechanisms of Controlling Drug Release. Chem. Rev. 2016, 16, 2602–2663. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- James, R.; Manoukian, O.S.; Kumbar, S.G. Poly(Lactic Acid) for Delivery of Bioactive Macromolecules. Adv. Drug Deliv. Rev. 2016, 107, 277–288. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bazile, D.V.; Ropert, C.; Huve, P.; Verrecchia, T.; Marlard, M.; Frydman, A.; Veillard, M.; Spenlehauer, G. Body Distribution of Fully Biodegradable [14C]-Poly(Lactic Acid) Nanoparticles Coated with Albumin after Parenteral Administration to Rats. Biomaterials 1992, 13, 1093–1102. [Google Scholar] [CrossRef]
- Nagarajan, V.; Mohanty, A.K.; Misra, M. Perspective on Polylactic Acid (PLA) Based Sustainable Materials for Durable Applications: Focus on Toughness and Heat Resistance. ACS Sustain. Chem. Eng. 2016, 4, 2899–2916. [Google Scholar] [CrossRef]
- Avérous, L. Chapter 21—Polylactic Acid: Synthesis, Properties and Applications. In Monomers, Polymers and Composites from Renewable Resources; Belgacem, M.N., Gandini, A., Eds.; Elsevier: Amsterdam, The Netherlands, 2008; pp. 433–450. ISBN 978-0-08-045316-3. [Google Scholar]
- Jenkins, A.D. Contemporary Polymer Chemistry (3rd Edition). HR Allcock, FW Lampe and JE Mark. Pearson Education, Inc. (Pearson/Prentice Hall): Upper Saddle River, NJ, USA, 2003, ISBN 0-13-065056-0 Pp Xviii + 814. Polym. Int. 2004, 53, 1395. [Google Scholar] [CrossRef]
- Coolen, A.-L.; Lacroix, C.; Mercier-Gouy, P.; Delaune, E.; Monge, C.; Exposito, J.-Y.; Verrier, B. Poly(Lactic Acid) Nanoparticles and Cell-Penetrating Peptide Potentiate MRNA-Based Vaccine Expression in Dendritic Cells Triggering Their Activation. Biomaterials 2019, 195, 23–37. [Google Scholar] [CrossRef]
- Feng, C.; Yuan, X.; Chu, K.; Zhang, H.; Ji, W.; Rui, M. Preparation and Optimization of Poly (Lactic Acid) Nanoparticles Loaded with Fisetin to Improve Anti-Cancer Therapy. Int. J. Biol. Macromol. 2019, 125, 700–710. [Google Scholar] [CrossRef]
- A New Absorbable Suture—Frazza—1971—Journal of Biomedical Materials Research—Wiley Online Library. Available online: https://onlinelibrary.wiley.com/doi/abs/10.1002/jbm.820050207 (accessed on 28 May 2021).
- Tang, X.; Thankappan, S.K.; Lee, P.; Fard, S.E.; Harmon, M.D.; Tran, K.; Yu, X. Chapter 21—Polymeric Biomaterials in Tissue Engineering and Regenerative Medicine. In Natural and Synthetic Biomedical Polymers; Kumbar, S.G., Laurencin, C.T., Deng, M., Eds.; Elsevier: Oxford, UK, 2014; pp. 351–371. ISBN 978-0-12-396983-5. [Google Scholar]
- Xu, Y.; Kim, C.-S.; Saylor, D.M.; Koo, D. Polymer Degradation and Drug Delivery in PLGA-Based Drug-Polymer Applications: A Review of Experiments and Theories. J. Biomed. Mater. Res. B Appl. Biomater. 2017, 105, 1692–1716. [Google Scholar] [CrossRef]
- Kapoor, D.N.; Bhatia, A.; Kaur, R.; Sharma, R.; Kaur, G.; Dhawan, S. PLGA: A Unique Polymer for Drug Delivery. Ther. Deliv. 2015, 6, 41–58. [Google Scholar] [CrossRef]
- Song, Z.; Feng, R.; Sun, M.; Guo, C.; Gao, Y.; Li, L.; Zhai, G. Curcumin-Loaded PLGA-PEG-PLGA Triblock Copolymeric Micelles: Preparation, Pharmacokinetics and Distribution in Vivo. J. Colloid Interface Sci. 2011, 354, 116–123. [Google Scholar] [CrossRef] [PubMed]
- Mittal, G.; Sahana, D.K.; Bhardwaj, V.; Ravi Kumar, M.N.V. Estradiol Loaded PLGA Nanoparticles for Oral Administration: Effect of Polymer Molecular Weight and Copolymer Composition on Release Behavior in Vitro and in Vivo. J. Control. Release 2007, 119, 77–85. [Google Scholar] [CrossRef] [PubMed]
- Torchilin, V.P. Polymer-Coated Long-Circulating Microparticulate Pharmaceuticals. J. Microencapsul. 1998, 15, 1–19. [Google Scholar] [CrossRef]
- Knop, K.; Hoogenboom, R.; Fischer, D.; Schubert, U.S. Poly(Ethylene Glycol) in Drug Delivery: Pros and Cons as Well as Potential Alternatives. Angew Chem. Int. Ed. Engl. 2010, 49, 6288–6308. [Google Scholar] [CrossRef] [PubMed]
- Torchilin, V.P.; Omelyanenko, V.G.; Papisov, M.I.; Bogdanov, A.A.; Trubetskoy, V.S.; Herron, J.N.; Gentry, C.A. Poly(Ethylene Glycol) on the Liposome Surface: On the Mechanism of Polymer-Coated Liposome Longevity. Biochim. Biophys. Acta 1994, 1195, 11–20. [Google Scholar] [CrossRef]
- Pan, C.; Zhang, T.; Li, S.; Xu, Z.; Pan, B.; Xu, S.; Jin, S.; Lu, G.; Yang, S.; Xue, Z.; et al. Hybrid Nanoparticles Modified by Hyaluronic Acid Loading an HSP90 Inhibitor as a Novel Delivery System for Subcutaneous and Orthotopic Colon Cancer Therapy. Int. J. Nanomed. 2021, 16, 1743–1755. [Google Scholar] [CrossRef] [PubMed]
- Rudnik, E. Compostable Polymer Materials; Elsevier: Amsterdam, The Netherlands, 2019; ISBN 978-0-08-099442-0. [Google Scholar]
- Dash, T.K.; Konkimalla, V.B. Poly-є-Caprolactone Based Formulations for Drug Delivery and Tissue Engineering: A Review. J. Control. Release 2012, 158, 15–33. [Google Scholar] [CrossRef]
- Dash, T.K.; Konkimalla, V.B. Polymeric Modification and Its Implication in Drug Delivery: Poly-ε-Caprolactone (PCL) as a Model Polymer. Mol. Pharm 2012, 9, 2365–2379. [Google Scholar] [CrossRef] [PubMed]
- Lu, X.L.; Sun, Z.J.; Cai, W.; Gao, Z.Y. Study on the Shape Memory Effects of Poly(L-Lactide-Co-Epsilon-Caprolactone) Biodegradable Polymers. J. Mater. Sci. Mater. Med. 2008, 19, 395–399. [Google Scholar] [CrossRef]
- Jeong, J.-C.; Lee, J.; Cho, K. Effects of Crystalline Microstructure on Drug Release Behavior of Poly(Epsilon-Caprolactone) Microspheres. J. Control. Release 2003, 92, 249–258. [Google Scholar] [CrossRef]
- Chawla, J.S.; Amiji, M.M. Biodegradable Poly(Epsilon -Caprolactone) Nanoparticles for Tumor-Targeted Delivery of Tamoxifen. Int. J. Pharm. 2002, 249, 127–138. [Google Scholar] [CrossRef]
- Niza, E.; Castro-Osma, J.A.; Posadas, I.; Alonso-Moreno, C.; Bravo, I.; Garzón, A.; Canales-Vázquez, J.; Ceña, V.; Lara-Sánchez, A.; Albaladejo, J. Assessment of Doxorubicin Delivery Devices Based on Tailored Bare Polycaprolactone against Glioblastoma. Int. J. Pharm. 2019, 558, 110–119. [Google Scholar] [CrossRef]
- Pachence, J.M.; Bohrer, M.P.; Kohn, J. Biodegradable Polymers. Princ. Tissue Eng. 2007, 323–339. [Google Scholar] [CrossRef]
- Pulapura, S.; Kohn, J. Trends in the Development of Bioresorbable Polymers for Medical Applications. J. Biomater. Appl. 1992, 6, 216–250. [Google Scholar] [CrossRef] [PubMed]
- Poly (γ-Glutamic Acid) Based Combination of Water-Insoluble Paclitaxel and TLR7 Agonist for Chemo-Immunotherapy—PubMed. Available online: https://pubmed.ncbi.nlm.nih.gov/24954733/ (accessed on 28 May 2021).
- Polyphosphoesters in Drug and Gene Delivery—PubMed. Available online: https://pubmed.ncbi.nlm.nih.gov/12706047/ (accessed on 28 May 2021).
- Andrieux, K.; Couvreur, P. Polyalkylcyanoacrylate Nanoparticles for Delivery of Drugs across the Blood-Brain Barrier. Wiley Interdiscip. Rev. Nanomed. Nanobiotechnol. 2009, 1, 463–474. [Google Scholar] [CrossRef]
- Fusser, M.; Øverbye, A.; Pandya, A.D.; Mørch, Ý.; Borgos, S.E.; Kildal, W.; Snipstad, S.; Sulheim, E.; Fleten, K.G.; Askautrud, H.A.; et al. Cabazitaxel-Loaded Poly(2-Ethylbutyl Cyanoacrylate) Nanoparticles Improve Treatment Efficacy in a Patient Derived Breast Cancer Xenograft. J. Control. Release 2019, 293, 183–192. [Google Scholar] [CrossRef] [PubMed]
- Villamagna, I.J.; Gordon, T.N.; Hurtig, M.B.; Beier, F.; Gillies, E.R. Poly(Ester Amide) Particles for Controlled Delivery of Celecoxib. J. Biomed. Mater. Res. A 2019, 107, 1235–1243. [Google Scholar] [CrossRef]
- The Mechanisms of Drug Release in Poly(Lactic-Co-Glycolic Acid)-Based Drug Delivery Systems—A Review—PubMed. Available online: https://pubmed.ncbi.nlm.nih.gov/21640806/ (accessed on 28 May 2021).
- Fu, Y.; Kao, W.J. Drug Release Kinetics and Transport Mechanisms of Non-Degradable and Degradable Polymeric Delivery Systems. Expert Opin. Drug Deliv. 2010, 7, 429–444. [Google Scholar] [CrossRef] [PubMed]
- Paarakh, M.P.; Jose, P.A.; Setty, C.; Christoper, G.P. Release kinetics—Concepts and applications. Int. J. Pharm. Res. Technol. 2018, 8, 12–20. [Google Scholar]
- Uhrich, K.E.; Cannizzaro, S.M.; Langer, R.S.; Shakesheff, K.M. Polymeric Systems for Controlled Drug Release. Chem. Rev. 1999, 99, 3181–3198. [Google Scholar] [CrossRef] [PubMed]
- Wilhelm, S.; Tavares, A.J.; Dai, Q.; Ohta, S.; Audet, J.; Dvorak, H.F.; Chan, W.C.W. Analysis of Nanoparticle Delivery to Tumours. Nat. Rev. Mater. 2016, 1, 1–12. [Google Scholar] [CrossRef]
- Tenzer, S.; Docter, D.; Kuharev, J.; Musyanovych, A.; Fetz, V.; Hecht, R.; Schlenk, F.; Fischer, D.; Kiouptsi, K.; Reinhardt, C.; et al. Rapid Formation of Plasma Protein Corona Critically Affects Nanoparticle Pathophysiology. Nat. Nanotechnol. 2013, 8, 772–781. [Google Scholar] [CrossRef] [PubMed]
- Liechty, W.B.; Kryscio, D.R.; Slaughter, B.V.; Peppas, N.A. Polymers for Drug Delivery Systems. Annu. Rev. Chem. Biomol. Eng. 2010, 1, 149–173. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zheng, Y.; Zheng, M.; Ma, Z.; Xin, B.; Guo, R.; Xu, X. 8—Sugar Fatty Acid Esters. In Polar Lipids; Ahmad, M.U., Xu, X., Eds.; Elsevier: Amsterdam, The Netherlands, 2015; pp. 215–243. ISBN 978-1-63067-044-3. [Google Scholar]
- Sharipova, A.A.; Aidarova, S.B.; Mutaliyeva, B.Z.; Babayev, A.A.; Issakhov, M.; Issayeva, A.B.; Madybekova, G.M.; Grigoriev, D.O.; Miller, R. The Use of Polymer and Surfactants for the Microencapsulation and Emulsion Stabilization. Colloids Interfaces 2017, 1, 3. [Google Scholar] [CrossRef] [Green Version]
- Mu, L.; Seow, P.-H.; Ang, S.-N.; Feng, S.-S. Study on Surfactant Coating of Polymeric Nanoparticles for Controlled Delivery of Anticancer Drug. Colloid Polym Sci. 2004, 283, 58–65. [Google Scholar] [CrossRef]
- Hoshyar, N.; Gray, S.; Han, H.; Bao, G. The Effect of Nanoparticle Size on in Vivo Pharmacokinetics and Cellular Interaction. Nanomedicine 2016, 11, 673–692. [Google Scholar] [CrossRef] [Green Version]
- Juan, A.; Cimas, F.J.; Bravo, I.; Pandiella, A.; Ocaña, A.; Alonso-Moreno, C. An Overview of Antibody Conjugated Polymeric Nanoparticles for Breast Cancer Therapy. Pharmaceutics 2020, 12, 802. [Google Scholar] [CrossRef] [PubMed]
- Juan, A.; Cimas, F.J.; Bravo, I.; Pandiella, A.; Ocaña, A.; Alonso-Moreno, C. Antibody Conjugation of Nanoparticles as Therapeutics for Breast Cancer Treatment. Int. J. Mol. Sci. 2020, 21, 6018. [Google Scholar] [CrossRef] [PubMed]
- Xiao, K.; Li, Y.; Luo, J.; Lee, J.S.; Xiao, W.; Gonik, A.M.; Agarwal, R.G.; Lam, K.S. The Effect of Surface Charge on in Vivo Biodistribution of PEG-Oligocholic Acid Based Micellar Nanoparticles. Biomaterials 2011, 32, 3435–3446. [Google Scholar] [CrossRef] [Green Version]
- Nakamura, Y.; Mochida, A.; Choyke, P.L.; Kobayashi, H. Nanodrug Delivery: Is the Enhanced Permeability and Retention Effect Sufficient for Curing Cancer? Bioconjugate Chem. 2016, 27, 2225–2238. [Google Scholar] [CrossRef]
- Wicki, A.; Witzigmann, D.; Balasubramanian, V.; Huwyler, J. Nanomedicine in Cancer Therapy: Challenges, Opportunities, and Clinical Applications; Elsevier: Amsterdam, The Netherlands, 2015; Volume 200. [Google Scholar]
- Bareford, L.M.; Swaan, P.W. Endocytic Mechanisms for Targeted Drug Delivery. Adv. Drug Deliv. Rev. 2007, 59, 748–758. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bregoli, L.; Movia, D.; Gavigan-Imedio, J.D.; Lysaght, J.; Reynolds, J.; Prina-Mello, A. Nanomedicine Applied to Translational Oncology: A Future Perspective on Cancer Treatment. Nanomed. Nanotechnol. Biol. Med. 2016, 12, 81–103. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Battistella, C.; Klok, H.-A. Controlling and Monitoring Intracellular Delivery of Anticancer Polymer Nanomedicines. Macromol. Biosci. 2017, 17, 1700022. [Google Scholar] [CrossRef] [Green Version]
- Han, J.; Zhao, D.; Li, D.; Wang, X.; Jin, Z.; Zhao, K. Polymer-Based Nanomaterials and Applications for Vaccines and Drugs. Polymers 2018, 10, 31. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Krishnaswamy, K.; Orsat, V. Chapter 2—Sustainable Delivery Systems Through Green Nanotechnology. In Nano- and Microscale Drug Delivery Systems; Grumezescu, A.M., Ed.; Elsevier: Amsterdam, The Netherlands, 2017; pp. 17–32. ISBN 978-0-323-52727-9. [Google Scholar]
- Avgoustakis, K. Pegylated Poly(Lactide) and Poly(Lactide-Co-Glycolide) Nanoparticles: Preparation, Properties and Possible Applications in Drug Delivery. Curr. Drug Deliv. 2004, 1, 321–333. [Google Scholar] [CrossRef]
- Wang, Q.; Wu, P.; Ren, W.; Xin, K.; Yang, Y.; Xie, C.; Yang, C.; Liu, Q.; Yu, L.; Jiang, X.; et al. Comparative Studies of Salinomycin-Loaded Nanoparticles Prepared by Nanoprecipitation and Single Emulsion Method. Nanoscale Res. Lett. 2014, 9, 351. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cohen-Sela, E.; Teitlboim, S.; Chorny, M.; Koroukhov, N.; Danenberg, H.D.; Gao, J.; Golomb, G. Single and Double Emulsion Manufacturing Techniques of an Amphiphilic Drug in PLGA Nanoparticles: Formulations of Mithramycin and Bioactivity. J. Pharm. Sci. 2009, 98, 1452–1462. [Google Scholar] [CrossRef]
- Cegnar, M.; Kos, J.; Kristl, J. Cystatin Incorporated in Poly(Lactide-Co-Glycolide) Nanoparticles: Development and Fundamental Studies on Preservation of Its Activity. Eur. J. Pharm. Sci. 2004, 22, 357–364. [Google Scholar] [CrossRef]
- Allémann, E.; Gurny, R.; Doelker, E. Preparation of Aqueous Polymeric Nanodispersions by a Reversible Salting-out Process: Influence of Process Parameters on Particle Size. Int. J. Pharm. 1992, 87, 247–253. [Google Scholar] [CrossRef]
- Das, S.; Suresh, P.K.; Desmukh, R. Design of Eudragit RL 100 Nanoparticles by Nanoprecipitation Method for Ocular Drug Delivery. Nanomedicine 2010, 6, 318–323. [Google Scholar] [CrossRef]
- Draheim, C.; de Crécy, F.; Hansen, S.; Collnot, E.-M.; Lehr, C.-M. A Design of Experiment Study of Nanoprecipitation and Nano Spray Drying as Processes to Prepare PLGA Nano- and Microparticles with Defined Sizes and Size Distributions. Pharm. Res. 2015, 32, 2609–2624. [Google Scholar] [CrossRef]
- Jaworek, A. Micro- and Nanoparticle Production by Electrospraying. Powder Technol. 2007, 176, 18–35. [Google Scholar] [CrossRef]
- Xu, S.; Nie, Z.; Seo, M.; Lewis, P.; Kumacheva, E.; Stone, H.A.; Garstecki, P.; Weibel, D.B.; Gitlin, I.; Whitesides, G.M. Generation of Monodisperse Particles by Using Microfluidics: Control over Size, Shape, and Composition. Angew Chem. Int. Ed. Engl. 2005, 44, 724–728. [Google Scholar] [CrossRef] [PubMed]
- DeMello, A.J. Control and Detection of Chemical Reactions in Microfluidic Systems. Nature 2006, 442, 394–402. [Google Scholar] [CrossRef]
- Reis, C.P.; Neufeld, R.J.; Ribeiro, A.J.; Veiga, F. Nanoencapsulation I. Methods for Preparation of Drug-Loaded Polymeric Nanoparticles. Nanomedicine 2006, 2, 8–21. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- He, H.; Liu, L.; Morin, E.E.; Liu, M.; Schwendeman, A. Survey of Clinical Translation of Cancer Nanomedicines—Lessons Learned from Successes and Failures Published as Part of the Accounts of Chemical Research Special Issue “ Nanomedicine and Beyond. Acc. Chem. Res. 2019, 52, 2445–2461. [Google Scholar] [CrossRef] [PubMed]
- Jain, M.M.; Gupte, S.U.; Patil, S.G.; Pathak, A.B.; Deshmukh, C.D.; Bhatt, N.; Haritha, C.; Babu, K.G.; Bondarde, S.A.; Digumarti, R.; et al. Paclitaxel Injection Concentrate for Nanodispersion versus Nab-Paclitaxel in Women with Metastatic Breast Cancer: A Multicenter, Randomized, Comparative Phase II/III Study. Breast Cancer Res. Treat. 2016, 156, 125–134. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Saif, M.W.; Podoltsev, N.A.; Rubin, M.S.; Figueroa, J.A.; Lee, M.Y.; Kwon, J.; Rowen, E.; Yu, J.; Kerr, R.O. Phase II Clinical Trial of Paclitaxel Loaded Polymeric Micelle in Patients with Advanced Pancreatic Cancer. Cancer Investig. 2010, 28, 186–194. [Google Scholar] [CrossRef]
- Kim, T.Y.; Kim, D.W.; Chung, J.Y.; Shin, S.G.; Kim, S.C.; Heo, D.S.; Kim, N.K.; Bang, Y.J. Phase I and Pharmacokinetic Study of Genexol-PM, a Cremophor-Free, Polymeric Micelle-Formulated Paclitaxel, in Patients with Advanced Malignancies. Clin. Cancer Res. 2004, 10, 3708–3716. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, K.S.; Chung, H.C.; Im, S.A.; Park, Y.H.; Kim, C.S.; Kim, S.B.; Rha, S.Y.; Lee, M.Y.; Ro, J. Multicenter Phase II Trial of Genexol-PM, a Cremophor-Free, Polymeric Micelle Formulation of Paclitaxel, in Patients with Metastatic Breast Cancer. Breast Cancer Res. Treat. 2008, 108, 241–250. [Google Scholar] [CrossRef]
- Natale, R.; Socinski, M.; Hart, L.; Lipatov, O.; Spigel, D.; Gershenhorn, B.; Weiss, G.; Kazmi, S.; Karaseva, N.; Gladkov, O.; et al. 41 Clinical Activity of BIND-014 (Docetaxel Nanoparticles for Injectable Suspension) as Second-Line Therapy in Patients (Pts) with Stage III/IV Non-Small Cell Lung Cancer. Eur. J. Cancer 2014, 50, 19. [Google Scholar] [CrossRef]
- Hoff, D.D.V.; Mita, M.M.; Ramanathan, R.K.; Weiss, G.J.; Mita, A.C.; Lorusso, P.M.; Burris, H.A.; Hart, L.L.; Low, S.C.; Parsons, D.M.; et al. Phase I Study of PSMA-Targeted Docetaxel-Containing Nanoparticle BIND-014 in Patients with Advanced Solid Tumors. Clin. Cancer Res. 2016, 22, 3157–3163. [Google Scholar] [CrossRef] [Green Version]
- Autio, K.A.; Garcia, J.A.; Alva, A.S.; Hart, L.L.; Milowsky, M.I.; Posadas, E.M.; Ryan, C.J.; Summa, J.M.; Youssoufian, H.; Scher, H.I.; et al. A Phase 2 Study of BIND-014 (PSMA-Targeted Docetaxel Nanoparticle) Administered to Patients with Chemotherapy-Naive Metastatic Castration-Resistant Prostate Cancer (mCRPC). J. Clin. Oncol. 2016, 34, 233. [Google Scholar]
- Merle, P.; Camus, P.; Abergel, A.; Pageaux, G.P.; Masliah, C.; Bronowicki, J.P.; Zarski, J.P.; Pelletier, G.; Bouattour, M.; Farloux, L.; et al. Safety and Efficacy of Intra-Arterial Hepatic Chemotherapy with Doxorubicin-Loaded Nanoparticles in Hepatocellular Carcinoma. ESMO Open 2017, 2. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ribas, A.; Kalinoski, L.; Heidel, J.D.; Peterkin, J.; Seligson, D.B.; Zuckerman, J.E.; Choi, C.; Yen, Y.; Davis, M.E.; Tolcher, A.W. Systemic Delivery of SiRNA via Targeted Nanoparticles in Patients with Cancer: Results from a First-in-Class Phase I Clinical Trial. J. Clin. Oncol. 2010, 28, 3022. [Google Scholar] [CrossRef]
- Zuckerman, J.E.; Gritli, I.; Tolcher, A.; Heidel, J.D.; Lim, D.; Morgan, R.; Chmielowski, B.; Ribas, A.; Davis, M.E.; Yen, Y. Correlating Animal and Human Phase Ia/Ib Clinical Data with CALAA-01, a Targeted, Polymer-Based Nanoparticle Containing SiRNA. Proc. Natl. Acad. Sci. USA 2014, 111, 11449–11454. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ocana, A.; Pandiella, A.; Siu, L.L.; Tannock, I.F. Preclinical Development of Molecular-Targeted Agents for Cancer. Nat. Rev. Clin. Oncol. 2010, 8, 200–209. [Google Scholar] [CrossRef]
- Seruga, B.; Templeton, A.J.; Badillo, F.E.V.; Ocana, A.; Amir, E.; Tannock, I.F. Under-Reporting of Harm in Clinical Trials. Lancet Oncol. 2016, 17, e209–e219. [Google Scholar] [CrossRef]
- Saleh, R.R.; Meti, N.; Ribnikar, D.; Goldvaser, H.; Ocana, A.; Templeton, A.J.; Seruga, B.; Amir, E. Associations between Safety, Tolerability, and Toxicity and the Reporting of Health-Related Quality of Life in Phase III Randomized Trials in Common Solid Tumors. Cancer Med. 2020, 9, 7888–7895. [Google Scholar] [CrossRef]
- Fernandes Neto, J.M.; Nadal, E.; Bosdriesz, E.; Ooft, S.N.; Farre, L.; McLean, C.; Klarenbeek, S.; Jurgens, A.; Hagen, H.; Wang, L.; et al. Multiple Low Dose Therapy as an Effective Strategy to Treat EGFR Inhibitor-Resistant NSCLC Tumours. Nat. Commun. 2020, 11, 3157. [Google Scholar] [CrossRef]
- Chang, L.; Ruiz, P.; Ito, T.; Sellers, W.R. Targeting Pan-Essential Genes in Cancer: Challenges and Opportunities. Cancer Cell 2021, 39, 466–479. [Google Scholar] [CrossRef]
- Ocaña, A.; García-Alonso, S.; Amir, E.; Pandiella, A. Refining Early Antitumoral Drug Development. Trends Pharm. Sci. 2018, 39, 922–925. [Google Scholar] [CrossRef] [PubMed]
- Cimas, F.J.; Niza, E.; Juan, A.; Noblejas-López, M.d.M.; Bravo, I.; Lara-Sanchez, A.; Alonso-Moreno, C.; Ocaña, A. Controlled Delivery of BET-PROTACs: In Vitro Evaluation of MZ1-Loaded Polymeric Antibody Conjugated Nanoparticles in Breast Cancer. Pharmaceutics 2020, 12, 986. [Google Scholar] [CrossRef]
- Ahmad, A.; Khan, F.; Mishra, R.K.; Khan, R. Precision Cancer Nanotherapy: Evolving Role of Multifunctional Nanoparticles for Cancer Active Targeting. J. Med. Chem. 2019, 62, 10475–10496. [Google Scholar] [CrossRef] [PubMed]
- Zou, W.; Sarisozen, C.; Torchilin, V.P. The Reversal of Multidrug Resistance in Ovarian Carcinoma Cells by Co-Application of Tariquidar and Paclitaxel in Transferrin-Targeted Polymeric Micelles. J. Drug Target. 2017, 25, 225–234. [Google Scholar] [CrossRef] [PubMed]
- Xu, L.; Xu, S.; Wang, H.; Zhang, J.; Chen, Z.; Pan, L.; Wang, J.; Wei, X.; Xie, H.; Zhou, L.; et al. Enhancing the Efficacy and Safety of Doxorubicin against Hepatocellular Carcinoma through a Modular Assembly Approach: The Combination of Polymeric Prodrug Design, Nanoparticle Encapsulation, and Cancer Cell-Specific Drug Targeting. ACS Appl. Mater. Interfaces 2018, 10, 3229–3240. [Google Scholar] [CrossRef]
- Voltan, R.; Secchiero, P.; Ruozi, B.; Forni, F.; Agostinis, C.; Caruso, L.; Vandelli, M.A.; Zauli, G. Nanoparticles Engineered with Rituximab and Loaded with Nutlin-3 Show Promising Therapeutic Activity in B-Leukemic Xenografts. Clin. Cancer Res. 2013, 19, 3871–3880. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sun, B.; Ranganathan, B.; Feng, S.-S. Multifunctional Poly(D,L-Lactide-Co-Glycolide)/Montmorillonite (PLGA/MMT) Nanoparticles Decorated by Trastuzumab for Targeted Chemotherapy of Breast Cancer. Biomaterials 2008, 29, 475–486. [Google Scholar] [CrossRef] [PubMed]
- Qiao, Y.; Wan, J.; Zhou, L.; Ma, W.; Yang, Y.; Luo, W.; Yu, Z.; Wang, H. Stimuli-Responsive Nanotherapeutics for Precision Drug Delivery and Cancer Therapy. Wiley Interdiscip. Rev. Nanomed. Nanobiotechnol. 2019, 11, e1527. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Xu, X.; Wu, J.; Liu, Y.; Yu, M.; Zhao, L.; Zhu, X.; Bhasin, S.; Li, Q.; Ha, E.; Shi, J.; et al. Ultra-PH-Responsive and Tumor-Penetrating Nanoplatform for Targeted SiRNA Delivery with Robust Anti-Cancer Efficacy. Angew. Chem. Int. Ed. Engl. 2016, 55, 7091–7094. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yin, T.; Wang, P.; Li, J.; Wang, Y.; Zheng, B.; Zheng, R.; Cheng, D.; Shuai, X. Tumor-Penetrating Codelivery of SiRNA and Paclitaxel with Ultrasound-Responsive Nanobubbles Hetero-Assembled from Polymeric Micelles and Liposomes. Biomaterials 2014, 35, 5932–5943. [Google Scholar] [CrossRef] [PubMed]
- Indoria, S.; Singh, V.; Hsieh, M.-F. Recent Advances in Theranostic Polymeric Nanoparticles for Cancer Treatment: A Review. Int. J. Pharm. 2020, 582, 119314. [Google Scholar] [CrossRef] [PubMed]
- Zhang, C.; Zeng, Z.; Cui, D.; He, S.; Jiang, Y.; Li, J.; Huang, J.; Pu, K. Semiconducting Polymer Nano-PROTACs for Activatable Photo-Immunometabolic Cancer Therapy. Nat. Commun. 2021, 12, 2934. [Google Scholar] [CrossRef] [PubMed]







| Advantages of Nanomedicine |
|---|
| Improved bioavailability |
| Greater dose response |
| Enhanced solubility |
| Scope for improvement efficacy |
| Assess therapeutic efficacy in real time: simultaneous monitoring of drug release and imaging distribution |
| Reduced toxicity |
| Allow to design specifically targeted therapies |
| Possibility of designing smart nanosystems capable of responding to external stimuli |
| Type of DDS | Structure | Benefits | Indented Use |
|---|---|---|---|
| Lipid-based NPs | Spherical vesicle having a lipid bilayer | Formulation simplicity and high drug loading | First vehicle for administration of pharmaceutical drugs |
| Solid lipid NPs | Spherical solid lipid core stabilized by surfactants | Temporal and in vivo stability | Delivery vehicle for nucleic acids |
| Dendrimers | Branched polymeric molecules | Encapsulation of hydrophobic drugs | Easy chemical modification to increase in vivo suitability |
| MOFs | Clusters of metal ions coordinated to organic ligands | High encapsulation and loading efficiency | pH-, magnetic-, ion-, temperature- and pressure-response carriers |
| Metallic NPs | Mainly iron oxide, gold, or silver core | Small size and easy surface functionalization | Development of diagnostic and therapeutic agents |
| Silica mesoporous NPs | Mesoporous silica core | Extensive multi-functionality based on its high specific surface | Stimuli-reactive guided liberation of drugs through chemical coatings |
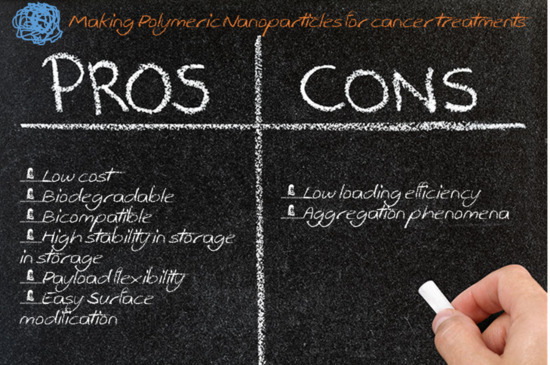
| Polymeric NPs | Biodegradable and biocompatible polymers | Low cost, large-scale synthesis, payload flexibility, biocompatibility and easy surface modification | Clinical translation of nanomedicines |
| Nanomedicine | Drug | Polymer | Conditions | Reference Clinical Trials |
|---|---|---|---|---|
| Genexol-PM® | Paclitaxel | polymeric micelle formulation | Metastatic adenocarcinoma of the pancreas | NCT02739633 |
| Hepatocellular carcinoma after failure of sorafenib | NCT03008512 | |||
| Advanced urothelial cancer | NCT01426126 | |||
| Advanced non-small-cell lung cancer | NCT01770795 | |||
| Advanced, metastatic and recurrent breast cancer | NCT01784120 NCT00876486 NCT01169870 NCT00912639 NCT02263495 NCT02064829 | |||
| Gynecologic cancer | NCT02739529 | |||
| Advanced ovarian cancer | NCT00877253 NCT01276548 NCT00886717 | |||
| Advanced and metastatic pancreatic cancer | NCT00882973 NCT00111904 | |||
| Advanced non-small-cell lung cancer | NCT01023347 | |||
| Advanced head and neck cancer | NCT01689194 | |||
| Advanced esophageal squamous cell carcinoma | NCT01474642 NCT00816634 | |||
| PICN® | Paclitaxel | copolymer polylactide-polyehtylene glycol | Metastatic breast cancer | CTRI/2010/091/001116 |
| BIND-014® | Docetaxel | copolymer polylactide-polyethylene glycol | Metastatic castration-resistant prostate cancer | NCT01812746 |
| Non-small-cell lung cancer | NCT01792479 | |||
| Advanced or metastatic cancer | NCT01300533 | |||
| KRAS positive or squamous cell non-small-cell lung cancer | NCT02283320 | |||
| Urothelial carcinoma, cholangiocarcinoma, cervical cancer and squamous cell carcinoma of the head and neck | NCT02479178 | |||
| Livatag® | Doxorrubicin | Polyalkylcyanoacrylate | Advanced hepatocarcinoma | EudraCT-2006-004088-77 |
| CALAA-01® | siRNA | Adamantane polyethylene glycol containing cyclodextrin | Solid tumor cancers | NCT00689065 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Niza, E.; Ocaña, A.; Castro-Osma, J.A.; Bravo, I.; Alonso-Moreno, C. Polyester Polymeric Nanoparticles as Platforms in the Development of Novel Nanomedicines for Cancer Treatment. Cancers 2021, 13, 3387. https://doi.org/10.3390/cancers13143387
Niza E, Ocaña A, Castro-Osma JA, Bravo I, Alonso-Moreno C. Polyester Polymeric Nanoparticles as Platforms in the Development of Novel Nanomedicines for Cancer Treatment. Cancers. 2021; 13(14):3387. https://doi.org/10.3390/cancers13143387
Chicago/Turabian StyleNiza, Enrique, Alberto Ocaña, José Antonio Castro-Osma, Iván Bravo, and Carlos Alonso-Moreno. 2021. "Polyester Polymeric Nanoparticles as Platforms in the Development of Novel Nanomedicines for Cancer Treatment" Cancers 13, no. 14: 3387. https://doi.org/10.3390/cancers13143387
APA StyleNiza, E., Ocaña, A., Castro-Osma, J. A., Bravo, I., & Alonso-Moreno, C. (2021). Polyester Polymeric Nanoparticles as Platforms in the Development of Novel Nanomedicines for Cancer Treatment. Cancers, 13(14), 3387. https://doi.org/10.3390/cancers13143387