Quality of Automated Stereotactic Radiosurgery Plans in Patients with 4 to 10 Brain Metastases
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Selection, Imaging, and Dose Prescription
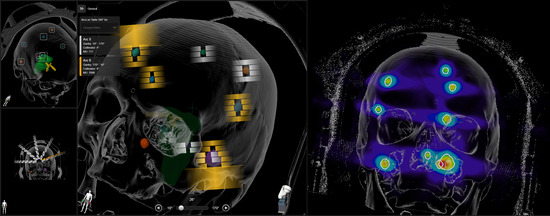
2.2. Treatment Planning
2.3. Plan Comparison
2.4. Statistics
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lippitz, B.; Lindquist, C.; Paddick, I.; Peterson, D.; O’Neill, K.; Beaney, R. Stereotactic radiosurgery in the treatment of brain metastases: The current evidence. Cancer Treat. Rev. 2014, 40, 48–59. [Google Scholar] [CrossRef] [Green Version]
- Tsao, M.N.; Rades, D.; Wirth, A.; Lo, S.S.; Danielson, B.L.; Gaspar, L.E.; Sperduto, P.W.; Vogelbaum, M.A.; Radawski, J.D.; Wang, J.Z.; et al. Radiotherapeutic and surgical management for newly diagnosed brain metastasis(es): An American Society for Radiation Oncology evidence-based guideline. Pract. Radiat. Oncol. 2012, 2, 210–225. [Google Scholar] [CrossRef] [Green Version]
- Yamamoto, M.; Serizawa, T.; Shuto, T.; Akabane, A.; Higuchi, Y.; Kawagishi, J.; Yamanaka, K.; Sato, Y.; Jokura, H.; Yomo, S.; et al. Stereotactic radiosurgery for patients with multiple brain metastases (JLGK0901): A multi-institutional prospective observational study. Lancet Oncol. 2014, 15, 387–395. [Google Scholar] [CrossRef]
- Hartgerink, D.; van der Heijden, B.; De Ruysscher, D.; Postma, A.; Ackermans, L.; Hoeben, A.; Anten, M.; Lambin, P.; Terhaag, K.; Jochems, A.; et al. Stereotactic radiosurgery in the management of patients with brain metastases of non-small cell lung cancer: Indications, decision tools and future directions. Front. Oncol. 2018, 8, 154. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- NICE (National Institute for Health and Care Excellence). Brain tumours (primary) and brain metastases in adults|Guidance|NICE. In NICE Clinical Guidelines; NICE: London, UK, 2018; pp. 1–24. [Google Scholar]
- Zindler, J.D.; Schiffelers, J.; Lambin, P.; Hoffmann, A.L. Improved effectiveness of stereotactic radiosurgery in large brain metastases by individualized isotoxic dose prescription: An in silico study. Strahlenther. Onkol. 2018, 194, 560–569. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lesueur, P.; Lequesne, J.; Barraux, V.; Kao, W.; Geffrelot, J.; Grellard, J.M.; Habrand, J.L.; Emery, E.; Marie, B.; Thariat, J.; et al. Radiosurgery or hypofractionated stereotactic radiotherapy for brain metastases from radioresistant primaries (melanoma and renal cancer). Radiat. Oncol. 2018, 13, 1–10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wiggenraad, R.; De Kanter, A.V.; Kal, H.B.; Taphoorn, M.; Vissers, T.; Struikmans, H. Dose-effect relation in stereotactic radiotherapy for brain metastases. A systematic review. Radiother. Oncol. 2011, 98, 292–297. [Google Scholar] [CrossRef] [PubMed]
- Putz, F.; Weissmann, T.; Oft, D.; Schmidt, M.A.; Roesch, J.; Siavooshhaghighi, H.; Filimonova, I.; Schmitter, C.; Mengling, V.; Bert, C.; et al. FSRT vs. SRS in Brain Metastases—Differences in Local Control and Radiation Necrosis—A Volumetric Study. Front. Oncol. 2020, 10, 559193. [Google Scholar] [CrossRef] [PubMed]
- Ma, L.; Petti, P.; Wang, B.; Descovich, M.; Chuang, C.; Barani, I.J.; Kunwar, S.; Shrieve, D.C.; Sahgal, A.; Larson, D.A. Apparatus dependence of normal brain tissue dose in stereotactic radiosurgery for multiple brain metastases. J. Neurosurg. 2011, 114, 1580–1584. [Google Scholar] [CrossRef]
- McDonald, D.; Schuler, J.; Takacs, I.; Peng, J.; Jenrette, J.; Vanek, K. Comparison of radiation dose spillage from the Gamma Knife Perfexion with that from volumetric modulated arc radiosurgery during treatment of multiple brain metastases in a single fraction. J. Neurosurg. 2014, 121 (Suppl. 2), 51–59. [Google Scholar] [CrossRef] [Green Version]
- Eaton, D.J.; Lee, J.; Paddick, I. Stereotactic radiosurgery for multiple brain metastases: Results of multicenter benchmark planning studies. Pract. Radiat. Oncol. 2018, 8, e212–e220. [Google Scholar] [CrossRef] [PubMed]
- Gevaert, T.; Steenbeke, F.; Pellegri, L.; Engels, B.; Christian, N.; Hoornaert, M.T.; Verellen, D.; Mitine, C.; De Ridder, M. Evaluation of a dedicated brain metastases treatment planning optimization for radiosurgery: A new treatment paradigm? Radiat. Oncol. 2016, 11, 1–7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Narayanasamy, G.; Stathakis, S.; Gutierrez, A.N.; Pappas, E.; Crownover, R.; Ii, J.R.F.; Papanikolaou, N. A Systematic Analysis of 2 Monoisocentric Techniques for the Treatment of Multiple Brain Metastases. Technol. Cancer Res. Treat. 2017, 16, 639–644. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Huang, Y.; Chin, K.; Robbins, J.R.; Kim, J.; Li, H.; Amro, H.; Chetty, I.J.; Gordon, J.; Ryu, S. Radiosurgery of multiple brain metastases with single-isocenter dynamic conformal arcs ( SIDCA ). Radiother. Oncol. 2014, 112, 128–132. [Google Scholar] [CrossRef]
- Hardcastle, N.; Tome, W.A. On a single isocenter volumetric modulated arc therapy SRS planning technique for multiple brain metastases. J. Radiosurg. SBRT 2012, 2, 1–9. [Google Scholar] [PubMed]
- Iwai, Y.; Ozawa, S.; Ageishi, T.; Pellegrini, R.; Yoda, K. Feasibility of single-isocenter, multi-arc non-coplanar volumetric modulated arc therapy for multiple brain tumors using a linear accelerator with a 160-leaf multileaf collimator: A phantom study. J. Radiat. Res. 2014, 55, 1015–1020. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hossain, S.; Keeling, V.; Hildebrand, K.; Ahmad, S.; Larson, D.A.; Sahgal, A.; Ma, L. Normal Brain Sparing With Increasing Number of Beams and Isocenters in Volumetric-Modulated Arc Beam Radiosurgery of Multiple Brain Metastases. Technol. Cancer Res. Treat. 2016, 15, 766–771. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hofmaier, J.; Bodensohn, R.; Garny, S.; Hadi, I.; Fleischmann, D.F.; Eder, M.; Dinc, Y.; Reiner, M.; Corradini, S.; Parodi, K.; et al. Single isocenter stereotactic radiosurgery for patients with multiple brain metastases: Dosimetric comparison of VMAT and a dedicated DCAT planning tool. Radiat. Oncol. 2019, 14, 4–11. [Google Scholar] [CrossRef]
- Zindler, J.D.; Bruynzeel, A.M.E.; Eekers, D.B.P.; Hurkmans, C.W.; Swinnen, A.; Lambin, P. Whole brain radiotherapy versus stereotactic radiosurgery for 4-10 brain metastases: A phase III randomised multicentre trial. BMC Cancer 2017, 17, 500. [Google Scholar] [CrossRef] [Green Version]
- Eekers, D.B.; In’t Ven, L.; Roelofs, E.; Postma, A.; Alapetite, C.; Burnet, N.G.; Calugaru, V.; Compter, I.; Coremans, I.E.M.; Høyer, M.; et al. The EPTN consensus-based atlas for CT- and MR-based contouring in neuro-oncology. Radiother. Oncol. 2018, 128, 37–43. [Google Scholar] [CrossRef] [Green Version]
- van Santvoort, J.; Wiggenraad, R.; Bos, P. Positioning accuracy in stereotactic radiotherapy using a mask system with added vacuum mouth piece and stereoscopic X-ray positioning. Int. J. Radiat. Oncol. Biol. Phys. 2008, 72, 261–267. [Google Scholar] [CrossRef]
- Buitelaar-Gallé, M.; van Egmond, J.; van Santvoort, J.; RoosL, J.; Versluis, L.; De Vet, S.; van Hameren, M.; van Oorschot, T.; Wiggenraad, R.; van Wingerden, J.; et al. Evaluation of a new mask system for stereotactic radiotherapy in brain lesions. Radiother. Oncol. 2018, 127, S1290–S1291. [Google Scholar] [CrossRef]
- Kirkpatrick, J.P.; Wang, Z.; Sampson, J.H.; McSherry, F.; Herndon, J.E.; Allen, K.J.; Duffy, E.; Hoang, J.K.; Chang, Z.; Yoo, D.S.; et al. Defining the optimal planning target volume in image-guided stereotactic radiosurgery of brain metastases: Results of a randomized trial. Int. J. Radiat. Oncol. Biol. Phys. 2015, 91, 100–108. [Google Scholar] [CrossRef] [PubMed]
- Mayo, C.; Yorke, E.; Merchant, T.E. Radiation Associated Brainstem Injury. Int. J. Radiat. Oncol. Biol. Phys. 2010, 76, 36–41. [Google Scholar] [CrossRef] [Green Version]
- Mayo, C.; Martel, M.K.; Marks, L.B.; Flickinger, J.; Nam, J.; Kirkpatrick, J. Radiation Dose-Volume Effects of Optic Nerves and Chiasm. Int. J. Radiat. Oncol. Biol. Phys. 2010, 76, 28–35. [Google Scholar] [CrossRef]
- Brainlab. Software User Guide RT ELEMENTS MULTIPLE BRAIN METS SRS Version 2.0; Brainlab AG: Munich, Germany, 2019. [Google Scholar]
- Paddick, I. A simple scoring ratio to index the conformity of radiosurgical treatment plans. J. Neurosurg. 2000, 93, 219–222. [Google Scholar] [CrossRef] [PubMed]
- Paddick, I.; Lippitz, B. A simple dose gradient measurement tool to complement the conformity index. J. Neurosurg. 2006, 105, 194–201. [Google Scholar] [CrossRef]
- Sahgal, A.; Ruschin, M.; Ma, L.; Verbakel, W.; Larson, D.; Brown, P.D. Stereotactic radiosurgery alone for multiple brain metastases? A review of clinical and technical issues. Neuro. Oncol. 2017, 19, ii2–ii15. [Google Scholar] [CrossRef] [Green Version]
- Van Dyk, J.; Barnett, R.B.; Cygler, J.E.; Shragge, P.C. Commissioning and quality assurance of treatment planning computers. Int. J. Radiat. Oncol. Biol. Phys. 1993, 26, 261–273. [Google Scholar] [CrossRef]
- Low, D.A.; Dempsey, J.F. Evaluation of the gamma dose distribution comparison method. Med. Phys. 2003, 30, 2455–2464. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ruggieri, R.; Naccarato, S.; Mazzola, R.; Ricchetti, F.; Corradini, S.; Fiorentino, A.; Alongi, F. Linac-based VMAT radiosurgery for multiple brain lesions: Comparison between a conventional multi-isocenter approach and a new dedicated mono-isocenter technique. Radiat. Oncol. 2018, 13, 38. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vergalasova, I.; Liu, H.; Alonso-basanta, M.; Dong, L.; Li, J.; Nie, K. Multi-Institutional Dosimetric Evaluation of Modern Day Stereotactic Radiosurgery (SRS) Treatment Options for Multiple Brain Metastases. Front. Oncol. 2019, 9, 483. [Google Scholar] [CrossRef] [PubMed]






| Patient | Prescription | Total PTV (cm3) | PTV for Each Metastasis (cm3) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | |||
| 1 | 1 × 21 Gy | 3.05 | 1.16 | 0.14 | 1.6 | 0.15 | - | - | - | - | - | - |
| 2 | 1 × 21 Gy | 8.56 | 2.61 | 1.84 | 3.53 | 0.58 | - | - | - | - | - | - |
| 3 | 1 × 18 Gy | 15.42 | 13.5 | 0.49 | 0.34 | 1.09 | - | - | - | - | - | - |
| 4 | 1 × 15 Gy | 27.30 | 0.25 | 21.14 | 2.92 | 2.99 | - | - | - | - | - | - |
| 5 | 1 × 21 Gy | 3.12 | 0.37 | 1.04 | 0.90 | 0.62 | 0.20 | - | - | - | - | - |
| 6 | 1 × 18 Gy | 15.17 | 0.12 | 0.06 | 11.72 | 2.86 | 0.42 | - | - | - | - | - |
| 7 | 1 × 21 Gy | 14.60 | 6.41 | 1.35 | 0.73 | 0.95 | 2.26 | 2.36 | 0.54 | - | - | - |
| 8 | 1 × 18 Gy | 24.09 | 0.49 | 0.47 | 10.68 | 1.63 | 5.94 | 0.28 | 4.61 | - | - | - |
| 9 | 3 × 8.5 Gy | 34.78 | 2.46 | 0.11 | 0.70 | 0.39 | 4.14 | 0.84 | 2.50 | 23.64 | - | - |
| 10 | 1 × 21 Gy | 2.86 | 0.17 | 0.07 | 0.12 | 0.30 | 0.06 | 0.08 | 1.60 | 0.14 | 0.32 | - |
| 11 | 1 × 21 Gy | 23.55 | 2.14 | 3.64 | 3.59 | 0.91 | 1.79 | 7.29 | 0.51 | 3.07 | 0.10 | 0.51 |
| 12 | 3 × 8.5 Gy | 32.68 | 15.60 | 14.30 | 0.27 | 0.17 | 1.1 | 0.37 | 0.13 | 0.45 | 0.16 | 0.13 |
| Plan | Conformity Index | Gradient Index | Mean Brain-GTVs (Gy) | V12Gy (cm3) | V5Gy (cm3) | MUs | Irradiation Time (s) | Pass Rate (%) |
|---|---|---|---|---|---|---|---|---|
| Separate-isocenter DCA many couch angles | 0.72 ± 0.06 | 3.7 ± 0.6 | 3.1 ± 1.7 | 54 ± 58 | 276 ± 254 | 14,947 ± 907 | 1859 ± 7414 | 97.0 ± 2.5 |
| IMRT 1 isoc 3 angles | 0.73 ± 0.06 | 4.8 ± 1.1 ** | 3.5 ± 2.0 | 66 ± 71 | 388 ± 347 | 7517 ± 322 ** | 1235 ± 2468 ** | 99.7 ± 0.2 * |
| VMAT 1 isoc 3 angles | 0.71 ± 0.08 | 7.1 ± 3.0 *** | 4.9 ± 2.0 * | 85 ± 77 | 563 ± 394 * | 4123 ± 185 *** | 955 ± 1066 ** | 87.7 ± 4.8 *** |
| SIDCA_1: v.1.6 MBM Elements 3 angles | 0.70 ± 0.10 | 4.4 ± 0.6 * | 3.5 ± 1.9 | 71 ± 83 | 305 ± 271 | 6130 ± 250 *** | 820 ± 1881 *** | 99.3 ± 0.8 |
| SIDCA_2: v.1.6 MBM Elements 5 angles | 0.72 ± 0.08 | 4.2 ± 0.6 | 3.0 ± 2.0 | 61 ± 62 | 273 ± 241 | 5403 ± 191 *** | 724 ± 1434 *** | 99.5 ± 0.5 * |
| SIDCA_3: v.2.0 MBM Elements high NT 5 angles | 0.71 ± 0.08 | 3.4 ± 0.4 | 3.3 ± 1.7 | 50 ± 51 | 257 ± 242 | 6726 ± 236 *** | 904 ± 1791 ** | 94.3 ± 6.9 |
| SIDCA_4: v.2.0 MBM Elements low NT 5 angles | 0.73 ± 0.07 | 3.8 ± 0.6 | 3.3 ± 1.8 | 55 ± 54 | 283 ± 268 | 5958 ± 383 *** | 676 ± 1726 ** | 96.0 ± 3.8 |
| Plan | Maximum Dose (Gy) | ||||||
|---|---|---|---|---|---|---|---|
| Brain Stem | Chiasm | Optic Nerve Left | Optic Nerve Right | Eye Left | Eye Right | Pituitary Gland | |
| Separate-isocenter DCA many couch angles | 8.2 ± 7.8 | 2.8 ± 4.1 | 1.6 ± 1.1 | 2.5 ± 4.8 | 2.1 ± 2.2 | 1.0 ± 0.7 | 2.5 ± 3.5 |
| IMRT 1 isoc 3 angles | 9.8 ± 7.1 | 4.6 ± 3.9 | 2.6 ± 1.9 | 3.6 ± 4.4 | 2.3 ± 1.9 | 2.7 ± 2.8 | 3.7 ± 3.3 |
| VMAT 1 isoc 3 angles | 10.5 ± 7.1 | 5.2 ± 4.4 | 2.8 ± 1.7 | 4.3 ± 4.7 | 1.2 ± 1.1 | 0.9 ± 0.6 | 3.9 ± 3.1 |
| SIDCA_1: v.1.6 MBM Elements 3 angles | 9.4 ± 8.6 | 4.0 ± 5.4 | 2.6 ± 2.4 | 3.8 ± 5.9 | 2.9 ± 1.8 | 3.8 ± 3.1 * | 4.2 ± 4.8 |
| SIDCA_2: v.1.6 MBM Elements 5 angles | 8.4 ± 8.1 | 3.5 ± 4.6 | 2.0 ± 1.5 | 3.3 ± 4.9 | 2.6 ± 1.4 | 2.7 ± 2.2 * | 3.3 ± 3.5 |
| SIDCA_3: v.2.0 MBM Elements high NT 5 angles | 8.0 ± 7.7 | 3.6 ± 4.5 | 2.3 ± 1.3 | 3.3 ± 4.8 | 2.3 ± 1.5 | 2.5 ± 2.3 | 3.1 ± 3.1 |
| SIDCA_4: v.2.0 MBM Elements low NT 5 angles | 8.3 ± 8.2 | 3.5 ± 4.7 | 2.4 ± 1.4 | 3.4 ± 4.9 | 2.3 ± 1.5 | 2.8 ± 2.2 * | 3.1 ± 3.2 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Petoukhova, A.; Snijder, R.; Wiggenraad, R.; de Boer-de Wit, L.; Mudde-van der Wouden, I.; Florijn, M.; Zindler, J. Quality of Automated Stereotactic Radiosurgery Plans in Patients with 4 to 10 Brain Metastases. Cancers 2021, 13, 3458. https://doi.org/10.3390/cancers13143458
Petoukhova A, Snijder R, Wiggenraad R, de Boer-de Wit L, Mudde-van der Wouden I, Florijn M, Zindler J. Quality of Automated Stereotactic Radiosurgery Plans in Patients with 4 to 10 Brain Metastases. Cancers. 2021; 13(14):3458. https://doi.org/10.3390/cancers13143458
Chicago/Turabian StylePetoukhova, Anna, Roland Snijder, Rudolf Wiggenraad, Linda de Boer-de Wit, Ivonne Mudde-van der Wouden, Mireille Florijn, and Jaap Zindler. 2021. "Quality of Automated Stereotactic Radiosurgery Plans in Patients with 4 to 10 Brain Metastases" Cancers 13, no. 14: 3458. https://doi.org/10.3390/cancers13143458
APA StylePetoukhova, A., Snijder, R., Wiggenraad, R., de Boer-de Wit, L., Mudde-van der Wouden, I., Florijn, M., & Zindler, J. (2021). Quality of Automated Stereotactic Radiosurgery Plans in Patients with 4 to 10 Brain Metastases. Cancers, 13(14), 3458. https://doi.org/10.3390/cancers13143458