Circulating microRNAs Correlate with Multiple Myeloma and Skeletal Osteolytic Lesions
Abstract
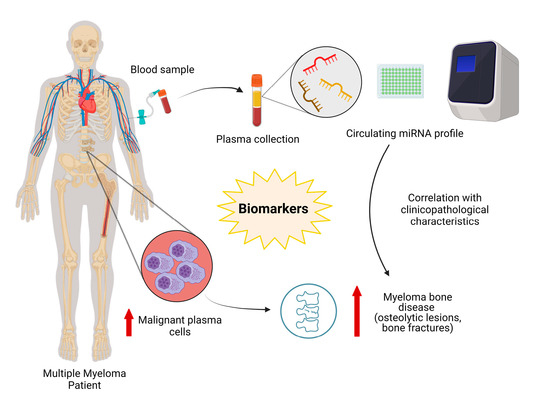
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients and Plasma Samples
2.2. Isolation and Purification of Circulating microRNAs
2.3. Selection of the miRNA Panel, Reverse Transcription and Real Time Quantitative Polymerase Chain Reaction (RT-qPCR)
2.4. Statistical Analysis
3. Results
3.1. Patients Characteristics
3.2. Differences in the Expression of Circulating miRNAs between Multiple Myeloma Patients and Control Group
3.3. Specificity and Sensibility of Circulting microRNAs as Multiple Myeloma Biomarkers
3.4. Correlation between Circulating microRNAs and Clinicopathological Variables in Multiple Myeloma Patients
3.5. Correlation between Circulating microRNAs and Skeletal Osteolytic Lesions
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- García-Ortiz, A.; Rodríguez-García, Y.; Encinas, J.; Maroto-Martín, E.; Castellano, E.; Teixidó, J.; Martínez-López, J. The Role of Tumor Microenvironment in Multiple Myeloma Development and Progression. Cancers 2021, 13, 217. [Google Scholar] [CrossRef]
- Oldham, R.A.A.; Faber, M.L.; Keppel, T.R.; Buchberger, A.R.; Waas, M.; Hari, P.; Gundry, R.L.; Medin, J.A. Discovery and validation of surface N-glycoproteins in MM cell lines and patient samples uncovers immunotherapy targets. J. Immunother. Cancer 2020, 8, e000915. [Google Scholar] [CrossRef] [PubMed]
- Kazandjian, D.; Branch, L.M. Multiple Myeloma Epidemiology and Survival, a Unique Malignancy. Semin. Oncol. 2017, 43, 676–681. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Terpos, E.; Ntanasis-Stathopoulos, I.; Gavriatopoulou, M.; Dimopoulos, M.A. Pathogenesis of bone disease in multiple myeloma: From bench to bedside. Blood Cancer J. 2018, 8, 1–12. [Google Scholar] [CrossRef] [Green Version]
- Terpos, E.; Dimopoulos, M.-A. Myeloma bone disease: Pathophysiology and management. Ann. Oncol. 2005, 16, 1223–1231. [Google Scholar] [CrossRef] [PubMed]
- Visconti, R.J.; Kolaja, K.; Cottrell, J.A. A functional three-dimensional microphysiological human model of myeloma bone disease. J. Bone Miner. Res. 2021. [Google Scholar] [CrossRef]
- Parrondo, R.D.; Sher, T. Prevention Of Skeletal Related Events In Multiple Myeloma: Focus On The RANK-L Pathway In The Treatment Of Multiple Myeloma. OncoTargets Ther. 2019, 12, 8467–8478. [Google Scholar] [CrossRef] [Green Version]
- Lasocki, A.; Gaillard, F.; Harrison, S.J. Multiple myeloma of the spine. Neuroradiol. J. 2017, 30, 259–268. [Google Scholar] [CrossRef]
- Terpos, E.; Sezer, O.; Croucher, P.I.; García-Sanz, R.; Boccadoro, M.; Miguel, J.S.; Ashcroft, J.; Bladé, J.; Cavo, M.; Delforge, M.; et al. The use of bisphosphonates in multiple myeloma: Recommendations of an expert panel on behalf of the European Myeloma Network. Ann. Oncol. 2009, 20, 1303–1317. [Google Scholar] [CrossRef]
- Zamagni, E.; Tacchetti, P.; Cavo, M. Imaging in multiple myeloma: How? When? Blood 2019, 133, 644–651. [Google Scholar] [CrossRef] [Green Version]
- Almeida, M.I.; Reis, R.M.; Calin, G.A. MicroRNA history: Discovery, recent applications, and next frontiers. Mutat. Res. Mol. Mech. Mutagen. 2011, 717, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Almeida, M.I.; Reis, R.M.; Calin, G.A. Decoy activity through microRNAs: The therapeutic implications. Expert Opin. Biol. Ther. 2012, 12, 1153–1159. [Google Scholar] [CrossRef] [Green Version]
- Soliman, A.M.; Lin, T.S.; Mahakkanukrauh, P.; Das, S. Role of microRNAs in Diagnosis, Prognosis and Management of Multiple Myeloma. Int. J. Mol. Sci. 2020, 21, 7539. [Google Scholar] [CrossRef] [PubMed]
- Handa, H.; Murakami, Y.; Ishihara, R.; Kimura-Masuda, K.; Masuda, Y. The Role and Function of microRNA in the Pathogenesis of Multiple Myeloma. Cancers 2019, 11, 1738. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mori, M.A.; Ludwig, R.G.; Garcia-Martin, R.; Brandão, B.B.; Kahn, C.R. Extracellular miRNAs: From Biomarkers to Mediators of Physiology and Disease. Cell Metab. 2019, 30, 656–673. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, P.S.; Parkin, R.K.; Kroh, E.M.; Fritz, B.R.; Wyman, S.K.; Pogosova-Agadjanyan, E.L.; Peterson, A.; Noteboom, J.; O’Briant, K.C.; Allen, A.; et al. Circulating microRNAs as stable blood-based markers for cancer detection. Proc. Natl. Acad. Sci. USA 2008, 105, 10513–10518. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Silva, A.M.; Teixeira, J.H.; Almeida, M.I.; Gonçalves, R.M.; Barbosa, M.A.; Santos, S.G. Extracellular Vesicles: Immunomodulatory messengers in the context of tissue repair/regeneration. Eur. J. Pharm. Sci. 2017, 98, 86–95. [Google Scholar] [CrossRef] [PubMed]
- Turchinovich, A.; Weiz, L.; Langheinz, A.; Burwinkel, B. Characterization of extracellular circulating microRNA. Nucleic Acids Res. 2011, 39, 7223–7233. [Google Scholar] [CrossRef] [PubMed]
- Almeida, M.I.; Silva, A.M.; Vasconcelos, D.M.; Almeida, C.R.; Caires, H.R.; Pinto, M.T.; Calin, G.A.; Santos, S.G.; Barbosa, M.A. miR-195 in human primary mesenchymal stromal/stem cells regulates proliferation, osteogenesis and paracrine effect on angiogenesis. Oncotarget 2016, 7, 7–22. [Google Scholar] [CrossRef] [Green Version]
- Moura, S.R.; Brás, J.P.; Freitas, J.; Osório, H.; Barbosa, M.A.; Santos, S.G.; Almeida, M.I. miR-99a in bone homeostasis: Regulating osteogenic lineage commitment and osteoclast differentiation. Bone 2020, 134, 115303. [Google Scholar] [CrossRef]
- Yang, L.; Cheng, P.; Chen, C.; He, H.-B.; Xie, G.-Q.; Zhou, H.-D.; Xie, H.; Wu, X.-P.; Luo, X.-H. miR-93/Sp7 function loop mediates osteoblast mineralization. J. Bone Miner. Res. 2012, 27, 1598–1606. [Google Scholar] [CrossRef] [PubMed]
- Tan, K.; Peng, Y.-T.; Guo, P. MiR-29a promotes osteogenic differentiation of mesenchymal stem cells via targeting HDAC4. Eur. Rev. Med. Pharmacol. Sci. 2018, 22, 3318–3326. [Google Scholar] [PubMed]
- Khalife, J.; Ghose, J.; Martella, M.; Viola, D.; Rocci, A.; Troadec, E.; Terrazas, C.; Satoskar, A.R.; Gunes, E.G.; Dona, A.; et al. MiR-16 regulates crosstalk in NF-κB tolerogenic inflammatory signaling between myeloma cells and bone marrow macrophages. JCI Insight 2019, 4. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.-H.; Zheng, W.-W.; Cheng, S.-T.; Liu, B.-X.; Liu, F.-R.; Song, J.-Q. Correlation between microRNA-21 and sprouty homolog 2 gene expression in multiple myeloma. Mol. Med. Rep. 2015, 11, 4220–4224. [Google Scholar] [CrossRef] [Green Version]
- Federico, C.; Sacco, A.; Belotti, A.; Ribolla, R.; Cancelli, V.; Giacomini, A.; Ronca, R.; Chiarini, M.; Imberti, L.; Marini, M.; et al. Circulating microRNAs and Their Role in Multiple Myeloma. Non-Coding RNA 2019, 5, 37. [Google Scholar] [CrossRef] [Green Version]
- Bustin, S.A.; Benes, V.; Garson, J.A.; Hellemans, J.; Huggett, J.; Kubista, M.; Mueller, R.; Nolan, T.; Pfaffl, M.W.; Shipley, G.L.; et al. The MIQE Guidelines: Minimum Information for Publication of Quantitative Real-Time PCR Experiments. Clin. Chem. 2009, 55, 611–622. [Google Scholar] [CrossRef] [Green Version]
- Tsimberidou, A.M.; Kantarjian, H.M.; Wen, S.; O’Brien, S.; Cortes, J.; Wierda, W.G.; Koller, C.; Pierce, S.; Brandt, M.; Freireich, E.J.; et al. The Prognostic Significance of Serum β2 Microglobulin Levels in Acute Myeloid Leukemia and Prognostic Scores Predicting Survival: Analysis of 1,180 Patients. Clin. Cancer Res. 2008, 14, 721–730. [Google Scholar] [CrossRef] [Green Version]
- Litam, P.; Swan, F.; Cabanillas, F.; Tucker, S.L.; McLaughlin, P.; Hagemeister, F.B.; Rodríguez, M.A.; Velasquez, W.S. Prognostic Value of Serum ?-2 Microglobulin in Low-Grade Lymphoma. Ann. Intern. Med. 1991, 114, 855. [Google Scholar] [CrossRef]
- Kim, J.E.; Yoo, C.; Lee, D.H.; Kim, S.-W.; Lee, J.-S.; Suh, C. Serum albumin level is a significant prognostic factor reflecting disease severity in symptomatic multiple myeloma. Ann. Hematol. 2010, 89, 391–397. [Google Scholar] [CrossRef]
- Chen, Y.H. Hypoalbuminemia in patients with multiple myeloma. Arch. Intern. Med. 1990, 150, 605–610. [Google Scholar] [CrossRef]
- Dimopoulos, M.A.; Kastritis, E.; Rosiñol, L.; Blade, J.; Ludwig, H.; Blad, J. Pathogenesis and treatment of renal failure in multiple myeloma. Leukemia 2008, 22, 1485–1493. [Google Scholar] [CrossRef] [Green Version]
- Rocci, A.; Hofmeister, C.C.; Geyer, S.; Stiff, A.; Gambella, M.; Cascione, L.; Guan, J.; Benson, D.M.; Efebera, Y.A.; Talabere, T.; et al. Circulating miRNA markers show promise as new prognosticators for multiple myeloma. Leukemia 2014, 28, 1922–1926. [Google Scholar] [CrossRef] [Green Version]
- Qu, X.; Zhao, M.; Wu, S.; Yu, W.; Xu, J.; Xu, J.; Li, J.; Chen, L. Circulating microRNA 483-5p as a novel biomarker for diagnosis survival prediction in multiple myeloma. Med. Oncol. 2014, 31, 219. [Google Scholar] [CrossRef]
- Li, M.; Zou, X.; Xia, T.; Wang, T.; Liu, P.; Zhou, X.; Wang, S.; Zhu, W. A five-miRNA panel in plasma was identified for breast cancer diagnosis. Cancer Med. 2019, 8, 7006–7017. [Google Scholar] [CrossRef] [Green Version]
- Adam-Artigues, A.; Garrido-Cano, I.; Carbonell-Asins, J.A.; Lameirinhas, A.; Simón, S.; Ortega-Morillo, B.; Martínez, M.T.; Hernando, C.; Constâncio, V.; Burgues, O.; et al. Identification of a Two-MicroRNA Signature in Plasma as a Novel Biomarker for Very Early Diagnosis of Breast Cancer. Cancers 2021, 13, 2848. [Google Scholar] [CrossRef]
- Zhou, X.; Wen, W.; Shan, X.; Zhu, W.; Xu, J.; Guo, R.; Cheng, W.; Wang, F.; Qi, L.-W.; Chen, Y.; et al. A six-microRNA panel in plasma was identified as a potential biomarker for lung adenocarcinoma diagnosis. Oncotarget 2017, 8, 6513–6525. [Google Scholar] [CrossRef]
- Usuba, W.; Urabe, F.; Yamamoto, Y.; Matsuzaki, J.; Sasaki, H.; Ichikawa, M.; Takizawa, S.; Aoki, Y.; Niida, S.; Kato, K.; et al. Circulating miRNA panels for specific and early detection in bladder cancer. Cancer Sci. 2018, 110, 408–419. [Google Scholar] [CrossRef]
- Wang, T.; Tao, W.; Zhang, L.; Li, S. Oncogenic role of microRNA-20a in human multiple myeloma. OncoTargets Ther. 2017, 10, 4465–4474. [Google Scholar] [CrossRef] [Green Version]
- Jiang, Y.; Chang, H.; Chen, G. Effects of microRNA-20a on the proliferation, migration and apoptosis of multiple myeloma via the PTEN/PI3K/AKT signaling pathway. Oncol. Lett. 2018, 15, 10001–10007. [Google Scholar] [CrossRef] [Green Version]
- Wang, W.; Corrigan-Cummins, M.; Barber, E.A.; Saleh, L.M.; Zingone, A.; Ghafoor, A.; Costello, R.; Zhang, Y.; Kurlander, R.J.; Korde, N.; et al. Aberrant Levels of miRNAs in Bone Marrow Microenvironment and Peripheral Blood of Myeloma Patients and Disease Progression. J. Mol. Diagn. 2015, 17, 669–678. [Google Scholar] [CrossRef]
- Papanota, A.-M.; Tsiakanikas, P.; Kontos, C.; Malandrakis, P.; Liacos, C.-I.; Ntanasis-Stathopoulos, I.; Kanellias, N.; Gavriatopoulou, M.; Kastritis, E.; Avgeris, M.; et al. A Molecular Signature of Circulating MicroRNA Can Predict Osteolytic Bone Disease in Multiple Myeloma. Cancers 2021, 13, 3877. [Google Scholar] [CrossRef] [PubMed]
- Kapinas, K.; Kessler, C.B.; Delany, A.M. miR-29 suppression of osteonectin in osteoblasts: Regulation during differentiation and by canonical Wnt signaling. J. Cell. Biochem. 2009, 108, 216–224. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kriegel, A.J.; Liu, Y.; Fang, Y.; Ding, X.; Liang, M. The miR-29 family: Genomics, cell biology, and relevance to renal and cardiovascular injury. Physiol. Genom. 2012, 44, 237–244. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.; Hassan, M.Q.; Jafferji, M.; Aqeilan, R.I.; Garzon, R.; Croce, C.M.; van Wijnen, A.J.; Stein, J.L.; Stein, G.S.; Lian, J.B. Biological Functions of miR-29b Contribute to Positive Regulation of Osteoblast Differentiation. J. Biol. Chem. 2009, 284, 15676–15684. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Feichtinger, X.; Muschitz, C.; Heimel, P.; Baierl, A.; Fahrleitner-Pammer, A.; Redl, H.; Resch, H.; Geiger, E.; Skalicky, S.; Dormann, R.; et al. Bone-related Circulating MicroRNAs miR-29b-3p, miR-550a-3p, and miR-324-3p and their Association to Bone Microstructure and Histomorphometry. Sci. Rep. 2018, 8, 1–11. [Google Scholar] [CrossRef] [PubMed]





| Healthy Donors | MM | p-Value | |
|---|---|---|---|
| Demographic characteristics | |||
| Age (years) | 39.00 (24–60) | 71.00 (47–89) | <0.001 |
| Gender (Male-Female) (%) | 45.7–54.3 | 66.0–34.0 | 0.08 |
| Clinical and biochemical characteristics | |||
| ISS stage (I-II-III) (%) | N/A | 23.53–52.94–23.53 | |
| Ig isotype (IgA-IgD-IgE-IgG-IgM) (%) | 23.91-0-0-69.57-0 | ||
| Light chains (%) | 6.52 | ||
| β2-microglobulin (ng/mL) | 4389(1386–29094) | ||
| Albumin (g/dL) | 3.35 (2.3–4.2) | ||
| Creatinine (mg/dL) | 1.1 (0.5–6.3) | ||
| Calcium (mg/dL) | 8.8 (6.4–11.8) | ||
| Treatment | |||
| Chemotherapy (%) | N/A | 38.10 | |
| Radiotherapy (%) | 13.64 | ||
| Bone therapeutic (%) | 28.57 | ||
| Genetic alterations | |||
| del(17)(p13.1) (%) | N/A | 23.26 | |
| del(13)(q14.3) (%) | 34.88 | ||
| t(11;14) (%) | 13.64 | ||
| t(4;14) (%) | 2.33 | ||
| miRNA | p-Value (Adjusted to Age) |
|---|---|
| miR-16-5p | 0.027 |
| miR-20a-5p | 0.024 |
| miR-21-5p | 0.031 |
| miR-29c-3p | 0.334 |
| Stage (ISS) | Serum Proteins | |||||||
|---|---|---|---|---|---|---|---|---|
| I | II | III | β2M (ng/mL) | Albumin (g/dL) | Creatinine (mg/dL) | Total Calcium (mg/dL) | ||
| miR-16-5p | r | 0.155 | 0.102 | −0.276 | −0.414 | −0.178 | −0.287 | 0.053 |
| p | 0.380 | 0.566 | 0.115 | 0.013 | 0.286 | 0.077 | 0.756 | |
| miR-20a-5p | r | 0.283 | 0.078 | −0.375 | −0.565 | −0.183 | −0.461 | 0.043 |
| p | 0.105 | 0.661 | 0.029 | 0.000 | 0.271 | 0.003 | 0.798 | |
| miR-21-5p | r | −0.170 | 0.096 | 0.057 | 0.146 | −0.296 | −0.150 | −0.175 |
| p | 0.338 | 0.589 | 0.751 | 0.402 | 0.071 | 0.362 | 0.300 | |
| miR-29a-3p | r | −0.007 | 0.156 | −0.177 | −0.315 | −0.349 | −0.328 | 0.042 |
| p | 0.968 | 0.378 | 0.317 | 0.065 | 0.032 | 0.042 | 0.804 | |
| miR-29b-3p | r | 0.233 | 0.066 | −0.311 | −0.499 | −0.124 | −0.414 | 0.054 |
| p | 0.184 | 0.710 | 0.073 | 0.002 | 0.464 | 0.010 | 0.754 | |
| miR-29c-3p | r | 0.198 | −0.060 | -0.127 | −0.419 | −0.157 | −0.326 | −0.060 |
| p | 0.262 | 0.736 | 0.473 | 0.012 | 0.347 | 0.043 | 0.726 | |
| miR-93-5p | r | 0.283 | 0.018 | −0.304 | −0.275 | −0.041 | −0.039 | −0.123 |
| p | 0.105 | 0.919 | 0.081 | 0.111 | 0.805 | 0.815 | 0.469 | |
| miR-99a-5p | r | 0.000 | 0.312 | −0.368 | −0.357 | −0.197 | −0.007 | 0.013 |
| p | 1.000 | 0.072 | 0.032 | 0.035 | 0.235 | 0.966 | 0.938 | |
| miR-146a-5p | r | −0.205 | 0.240 | −0.078 | 0.082 | −0.196 | −0.015 | −0.085 |
| p | 0.245 | 0.171 | 0.662 | 0.642 | 0.239 | 0.927 | 0.618 | |
| miR-195-5p | r | 0.254 | 0.078 | −0.346 | −0.344 | −0.109 | −0.238 | −0.194 |
| p | 0.146 | 0.661 | 0.045 | 0.043 | 0.513 | 0.144 | 0.250 | |
| Treatment | Genetic Alterations | |||||||
|---|---|---|---|---|---|---|---|---|
| Chemotherapy or VTd Regimen | Radiotherapy | Bone Therapy | del(17)(p13.1) | del(13)(q14.3) | t(11;14) Translocation | t(4;14) Translocation | ||
| miR-16-5p | r | −0.150 | −0.162 | 0.216 | 0.253 | 0.016 | −0.114 | −0.114 |
| p | 0.344 | 0.294 | 0.164 | 0.102 | 0.920 | 0.468 | 0.461 | |
| miR-20a-5p | r | −0.138 | −0.089 | 0.114 | 0.271 | −0.063 | −0.081 | −0.078 |
| p | 0.385 | 0.567 | 0.466 | 0.079 | 0.689 | 0.605 | 0.615 | |
| miR-21-5p | r | −0.121 | −0.063 | −0.155 | −0.200 | −0.094 | 0.027 | −0.162 |
| p | 0.444 | 0.687 | 0.321 | 0.199 | 0.547 | 0.863 | 0.293 | |
| miR-29a-3p | r | −0.129 | −0.047 | −0.008 | 0.222 | 0.031 | −0.027 | −0.210 |
| p | 0.414 | 0.762 | 0.959 | 0.153 | 0.841 | 0.863 | 0.171 | |
| miR-29b-3p | r | −0.385 | 0.038 | 0.079 | 0.065 | −0.163 | −0.056 | −0.149 |
| p | 0.013 | 0.810 | 0.621 | 0.685 | 0.304 | 0.724 | 0.340 | |
| miR-29c-3p | r | −0.360 | −0.099 | 0.053 | 0.115 | 0.047 | 0.011 | −0.186 |
| p | 0.019 | 0.522 | 0.735 | 0.461 | 0.764 | 0.945 | 0.226 | |
| miR-93-5p | r | −0.174 | −0.188 | −0.461 | −0.146 | −0.134 | 0.081 | 0.174 |
| p | 0.271 | 0.222 | 0.002 | 0.349 | 0.393 | 0.605 | 0.258 | |
| miR-99a-5p | r | −0.231 | −0.016 | −0.261 | −0.031 | −0.181 | −0.022 | 0.066 |
| p | 0.142 | 0.920 | 0.091 | 0.843 | 0.246 | 0.890 | 0.670 | |
| miR-146a-5p | r | −0.170 | −0.130 | −0.510 | −0.075 | 0.035 | −0.043 | 0.030 |
| p | 0.282 | 0.399 | <0.001 | 0.631 | 0.822 | 0.783 | 0.847 | |
| miR-195-5p | r | −0.162 | −0.005 | −0.073 | 0.129 | −0.295 | −0.011 | −0.078 |
| p | 0.306 | 0.973 | 0.640 | 0.411 | 0.055 | 0.945 | 0.615 | |
| Bone Disease | Regions of the Spine | |||||
|---|---|---|---|---|---|---|
| Cervical | Thoracic | Lumbar | Sacrum | |||
| miR-16-5p | r | −0.147 | 0.118 | 0.127 | −0.163 | 0.175 |
| p | 0.341 | 0.456 | 0.415 | 0.303 | 0.267 | |
| miR-20a-5p | r | −0.073 | 0.076 | 0.146 | −0.119 | 0.155 |
| p | 0.640 | 0.633 | 0.349 | 0.453 | 0.327 | |
| miR-21-5p | r | 0.057 | −0.270 | −0.007 | 0.202 | 0.060 |
| p | 0.714 | 0.084 | 0.962 | 0.199 | 0.706 | |
| miR-29a-3p | r | −0.041 | −0.112 | −0.022 | −0.103 | 0.270 |
| p | 0.791 | 0.479 | 0.886 | 0.515 | 0.084 | |
| miR-29b-3p | r | −0.135 | −0.340 | −0.304 | −0.205 | 0.153 |
| p | 0.389 | 0.030 | 0.050 | 0.198 | 0.338 | |
| miR-29c-3p | r | −0.308 | −0.215 | −0.191 | −0.226 | −0.125 |
| p | 0.042 | 0.171 | 0.219 | 0.150 | 0.430 | |
| miR-93-5p | r | −0.100 | −0.185 | −0.079 | 0.087 | 0.115 |
| p | 0.518 | 0.241 | 0.616 | 0.582 | 0.468 | |
| miR-99a-5p | r | −0.151 | −0.215 | −0.120 | −0.008 | 0.285 |
| p | 0.328 | 0.171 | 0.444 | 0.960 | 0.067 | |
| miR-146a-5p | r | −0.226 | −0.112 | −0.015 | 0.032 | −0.025 |
| p | 0.141 | 0.479 | 0.924 | 0.842 | 0.875 | |
| miR-195-5p | r | −0.080 | −0.143 | −0.307 | 0.000 | 0.095 |
| p | 0.604 | 0.368 | 0.045 | 1.000 | 0.549 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Moura, S.R.; Abreu, H.; Cunha, C.; Ribeiro-Machado, C.; Oliveira, C.; Barbosa, M.A.; Marques, H.; Almeida, M.I. Circulating microRNAs Correlate with Multiple Myeloma and Skeletal Osteolytic Lesions. Cancers 2021, 13, 5258. https://doi.org/10.3390/cancers13215258
Moura SR, Abreu H, Cunha C, Ribeiro-Machado C, Oliveira C, Barbosa MA, Marques H, Almeida MI. Circulating microRNAs Correlate with Multiple Myeloma and Skeletal Osteolytic Lesions. Cancers. 2021; 13(21):5258. https://doi.org/10.3390/cancers13215258
Chicago/Turabian StyleMoura, Sara Reis, Hugo Abreu, Carla Cunha, Cláudia Ribeiro-Machado, Carla Oliveira, Mario Adolfo Barbosa, Herlander Marques, and Maria Inês Almeida. 2021. "Circulating microRNAs Correlate with Multiple Myeloma and Skeletal Osteolytic Lesions" Cancers 13, no. 21: 5258. https://doi.org/10.3390/cancers13215258
APA StyleMoura, S. R., Abreu, H., Cunha, C., Ribeiro-Machado, C., Oliveira, C., Barbosa, M. A., Marques, H., & Almeida, M. I. (2021). Circulating microRNAs Correlate with Multiple Myeloma and Skeletal Osteolytic Lesions. Cancers, 13(21), 5258. https://doi.org/10.3390/cancers13215258