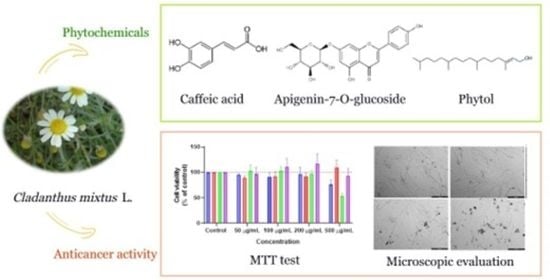
Phytochemical Compounds and Anticancer Activity of Cladanthus mixtus Extracts from Northern Morocco
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Standards and Chemical Reagents
2.2. Plant Material
2.3. Analysis of Phenolic Compounds by HPLC-MS
2.3.1. Extraction of Phenolic Compounds from Cladanthus mixtus
2.3.2. Analysis by HPLC-MS
2.4. Preparation of Methanolic Extracts
2.5. GC-MS Analysis of the Methanolic Extracts from Cladathus mixtus
2.6. In Vitro Anticancer Studies
2.6.1. Cell Culture
2.6.2. Cell Treatment
2.6.3. Morphological Analysis
2.6.4. MTT Assay
2.7. Statistical Analysis
3. Results
3.1. Phenolic Acids and Flavonoids Characterized in Cladanthus Mixtus by HPLC-MS
3.2. Biochemical Constituents of the Different Organs of Cladanthus mixtus by GC-MS
3.3. Cytotoxic Effect In Vitro of Cladanthus mixtus Extracts
3.3.1. Human Normal Lung Fibroblast (MRC-5)
3.3.2. Human Breast Carcinoma Cell (MCF-7)
3.3.3. Human Prostate Carcinoma Cell (PC-3)
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kamran, S.; Sinniah, A.; Abdulghani, M.A.M.; Alshawsh, M.A. Therapeutic Potential of Certain Terpenoids as Anticancer Agents: A Scoping Review. Cancers 2022, 14, 1100. [Google Scholar] [CrossRef] [PubMed]
- Ferlay, J.; Ervik, M.; Lam, F.; Colombet, M.; Mery, L.; Piñeros, M.; Znaor, A.; Soerjomataram, I.; Bray, F. Observatory: “Cancer Today”. Lyon International Agency Res. Cancer. 2020. Available online: https://gco.iarc.fr/today (accessed on 1 February 2021).
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA A Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Hanahan, D.; Weinberg, R.A. Hallmarks of Cancer: The Next Generation. Cell 2011, 144, 646–674. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Roos, W.P.; Kaina, B. DNA Damage-Induced Cell Death: From Specific DNA Lesions to the DNA Damage Response and Apoptosis. Cancer Lett. 2013, 332, 237–248. [Google Scholar] [CrossRef] [PubMed]
- Kondrashov, F.A.; Kondrashov, A. Measurements of Spontaneous Rates of Mutations in the Recent Past and the near Future. Philos. Trans. R. Soc. London. Ser. B Biol. Sci. 2010, 365, 1169–1176. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Torgovnick, A.; Schumacher, B. DNA Repair Mechanisms in Cancer Development and Therapy. Front. Genet. 2015, 6, 1–15. [Google Scholar] [CrossRef] [Green Version]
- Yang, L.; Yang, C.; Li, C.; Zhao, Q.; Liu, L.; Fang, X.; Chen, X.-Y. Recent Advances in Biosynthesis of Bioactive Compounds in Traditional Chinese Medicinal Plants. Sci. Bull. 2016, 61, 3–17. [Google Scholar] [CrossRef] [Green Version]
- Solowey, E.; Lichtenstein, M.; Sallon, S.; Paavilainen, H.; Solowey, E.; Lorberboum-Galski, H. Evaluating Medicinal Plants for Anticancer Activity. Sci. World J. 2014, 2014, 1–12. [Google Scholar] [CrossRef] [Green Version]
- Kuete, V.; Omosa, L.K.; Midiwo, J.O.; Karaosmanoğlu, O.; Sivas, H. Cytotoxicity of Naturally Occurring Phenolics and Terpenoids from Kenyan Flora towards Human Carcinoma Cells. J. Ayurveda Integr. Med. 2019, 10, 178–184. [Google Scholar] [CrossRef]
- Li, D.; Du, Z.; Li, C.; Liu, Y.; Goodin, S.; Huang, H.; He, Y.; Zhang, Y.; Wang, H.; Zheng, X.; et al. Potent Inhibitory Effect of Terpenoids from Acanthopanax Trifoliatus on Growth of PC-3 Prostate Cancer Cells in Vitro and in Vivo Is Associated with Suppression of NF-ΚB and STAT3 Signalling. J. Funct. Foods 2015, 15, 274–283. [Google Scholar] [CrossRef]
- Nevzorova, Y.A.; Grossmann, J.; Trautwein, C. Anti-Tumorigenic and Anti-Angiogenic Effects of Natural Conifer Abies Sibirica Terpenoids in Vivo and in Vitro. Biomed. Pharmacother. 2017, 89, 386–395. [Google Scholar] [CrossRef] [PubMed]
- Mishra, A.; Sharma, A.K.; Kumar, S.; Saxena, A.K.; Pandey, A.K. Bauhinia Variegata Leaf Extracts Exhibit Considerable Antibacterial, Antioxidant, and Anticancer Activities. Biomed Res. Int. 2013, 2013, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Ahmed, S.I.; Hayat, M.Q.; Tahir, M.; Mansoor, Q.; Ismail, M.; Keck, K.; Bates, R.B. Pharmacologically Active Flavonoids from the Anticancer, Antioxidant and Antimicrobial Extracts of Cassia Angustifolia Vahl. BMC Complement. Altern. Med. 2016, 16, 460. [Google Scholar] [CrossRef] [Green Version]
- African Plants Database. Conservatoire et Jardin Botaniques de La Ville de Genève and South African National Biodiversity Institute; Pretoria. 2012. Available online: http://www.ville-ge.ch/musinfo/bd/cjb/africa/ (accessed on 1 February 2021).
- Oberprieler, C.; Töpfer, A.; Dorfner, M.; Stock, M.; Vogt, R. An updated subtribal classification of Compositae tribe Anthemideae based on extended phylogenetic reconstructions. Willdenowia 2022, 52, 117–149. [Google Scholar] [CrossRef]
- Bellakhdar, J. La Pharmacopée Marocaine Traditionnelle; Médecine Arabe Ancienne et Savoirs Populaires; Edition Ibis Press: Paris, France, 1997; 766p. [Google Scholar]
- Merghoub, N.; Benbacer, L.; Amzazi, S.; Morjani, H.; El Mzibri, M. Cytotoxic Effect of Some Moroccan Medicinal Plant Extracts on Human Cervical Cell Lines. J. Med. Plants Res. 2009, 3, 1045–1050. [Google Scholar] [CrossRef]
- Lahsissene, H.; Kahouadji, A.; Hseini, S. Catalogue Des Plantes Médicinales Utilisées Dans La Région de Zaër (Maroc Occidental). Lejeunia Rev. De Bot. 2009, 186, 1–26. [Google Scholar]
- El Mihyaoui, A.; Candela Castillo, M.E.; Cano, A.; Hernández-Ruiz, J.; Lamarti, A.; Arnao, M.B. Comparative Study of Wild Chamomile Plants from the North-West of Morocco: Bioactive Components and Total Antioxidant Activity. J. Med. Plants Res. 2021, 5, 431–441. [Google Scholar] [CrossRef]
- Erbiai, E.H.; Bouchra, B.; da Silva, L.P.; Lamrani, Z.; Pinto, E.; da Silva, J.C.G.E.; Maouni, A. Chemical Composition and Antioxidant and Antimicrobial Activities of Lactarius Sanguifluus, a Wild Edible Mushroom from Northern Morocco. Euro-Mediterranean J. Environ. Integr. 2021, 6, 43. [Google Scholar] [CrossRef]
- Barros, L.; Calhelha, R.C.; Vaz, J.A.; Ferreira, I.C.F.R.; Baptista, P.; Estevinho, L.M. Antimicrobial Activity and Bioactive Compounds of Portuguese Wild Edible Mushrooms Methanolic Extracts. Eur. Food Res. Technol. 2007, 225, 151–156. [Google Scholar] [CrossRef]
- Erbiai, E.H.; Pinto da Silva, L.; Saidi, R.; Lamrani, Z.; Esteves da Silva, J.C.G.; Maouni, A. Chemical Composition, Bioactive Compounds and Antioxidant Activity of Two Wild Edible Mushrooms Armillaria mellea and Macrolepiota procera from Two Countries (Morocco and Portugal). Biomolecules 2021, 11, 575. [Google Scholar] [CrossRef]
- Ghouse, S.M.; Nguyen, H.M.; Bommareddy, P.K.; Guz-Montgomery, K.; Saha, D. Oncolytic Herpes Simplex Virus Encoding IL12 Controls Triple-Negative Breast Cancer Growth and Metastasis. Front. Oncol. 2020, 10, 384. [Google Scholar] [CrossRef] [PubMed]
- Aboul-Enein, A.M.; Faten, A.E.E.; Emad, A.S.; Hany, A.E.S. Simultaneous Analysis of Eight Phenolic Compounds in Phyllanthus simplex Retz by HPLC-DAD-ESI/MS. J. Med. Plants Res. 2012, 6, 689–703. [Google Scholar] [CrossRef] [Green Version]
- Kalimuthu, K.; Prabakaran, R. Preliminary Phytochemical Screening and GC-MS Analysis of Methanol Extract of Ceropegia pusilla. Int. J. Res. Applied, Nat. Soc. Sci. 2013, 1, 49–58. [Google Scholar]
- Lantto, T.A.; Colucci, M.; Závadová, V.; Hiltunen, R.; Raasmaja, A. Cytotoxicity of Curcumin, Resveratrol and Plant Extracts from Basil, Juniper, Laurel and Parsley in SH-SY5Y and CV1-P Cells. Food Chem. 2009, 117, 405–411. [Google Scholar] [CrossRef]
- Pan, M.H.; Ghai, G.; Ho, C.T. Food Bioactives, Apoptosis, and Cancer. Mol. Nutr. Food Res. 2008, 52, 43–52. [Google Scholar] [CrossRef] [PubMed]
- Elouaddari, A.; Elamrani, A.; Moutia, M.; Oubrim, N.; Habti, N.; JamalEddine, J. Chemical Composition and Evaluation of Antioxidant, Antimicrobial and Cytotoxic Activities of Moroccan Cladanthus mixtus Essential Oil and Extracts. J. Essent. Oil Bear. Plants. 2019, 22, 1450–1466. [Google Scholar] [CrossRef]
- Haghi, G.; Hatami, A.; Safaei, A.; Mehran, M. Analysis of Phenolic Compounds in Matricaria chamomilla and Its Extracts by UPLC-UV. Res. Pharm. Sci. 2014, 9, 31–37. [Google Scholar]
- Elsemelawy, S.A. Antidiabetic and Antioxidative Activity of Chamomile (Matricaria chamomilla L.) Powder on Diabetic Rats. J. Stud. Res. Qual. Educ. 2017, 3, 501–520. [Google Scholar] [CrossRef]
- Piri, E.; Sourestani, M.M.; Khaleghi, E.; Mottaghipisheh, J.; Zomborszki, Z.P.; Hohmann, J.; Csupor, D. Chemo-diversity and antiradical potential of twelve Matricaria chamomilla L. populations from Iran: Proof of ecological effects. Molecules 2019, 24, 1315. [Google Scholar] [CrossRef] [Green Version]
- Abotaleb, M.; Liskova, A.; Kubatka, P.; Büsselberg, D. Therapeutic Potential of Plant Phenolic Acids in the Treatment of Cancer. Biomolecules 2020, 10, 221. [Google Scholar] [CrossRef] [Green Version]
- Velli, S.; Sundaram, J.; Murugan, M.; Balaraman, G.; Thiruvengadam, D. Protective Effect of Vanillic Acid against Benzo(a)Pyrene Induced Lung Cancer in Swiss Albino Mice. J. Biochem. Mol. Toxicol. 2019, 33, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Anbalagan, V.; Raju, K.; Shanmugam, M. Assessment of Lipid Peroxidation and Antioxidant Status in Vanillic Acid Treated 7, 12-Dimethylbenz[a] Anthracene Induced Hamster Buccal Pouch Carcinogenesis. J. Clin. Diagn. Res. 2017, 11, BF01–BF04. [Google Scholar] [CrossRef] [PubMed]
- Srinivasulu, C.; Ramgopal, M.; Ramanjaneyulu, G.; Anuradha, C.M.; Suresh Kumar, C. Syringic Acid (SA)—A Review of Its Occurrence, Biosynthesis, Pharmacological and Industrial Importance. Biomed. Pharmacother. 2018, 108, 547–557. [Google Scholar] [CrossRef] [PubMed]
- Semaming, Y.; Pannengpetch, P.; Chattipakorn, S.C.; Chattipakorn, N. Pharmacological Properties of Protocatechuic Acid and Its Potential Roles as Complementary Medicine. Evid.-Based Complement. Altern. Med. 2015, eCAM, 593902. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yin, M.C.; Lin, C.C.; Wu, H.C.; Tsao, S.M.; Hsu, C.K. Apoptotic Effects of Protocatechuic Acid in Human Breast, Lung, Liver, Cervix, and Prostate Cancer Cells: Potential Mechanisms of Action. J. Agric. Food Chem. 2009, 57, 6468–6473. [Google Scholar] [CrossRef] [PubMed]
- Velu, P.; Vinothkumar, V.; Babukumar, S.; Ramachandhiran, D. Chemopreventive Effect of Syringic Acid on 7,12-Dimethylbenz(a)Anthracene Induced Hamster Buccal Pouch Carcinogenesis. Toxicol. Mech. Methods 2017, 27, 631–640. [Google Scholar] [CrossRef]
- Anantharaju, P.G.; Gowda, P.C.; Vimalambike, M.G.; Madhunapantula, S.V. An Overview on the Role of Dietary Phenolics for the Treatment of Cancers. Nutr. J. 2016, 15, 1–16. [Google Scholar] [CrossRef] [Green Version]
- Nasr Bouzaiene, N.; Kilani Jaziri, S.; Kovacic, H.; Chekir-Ghedira, L.; Ghedira, K.; Luis, J. The Effects of Caffeic, Coumaric and Ferulic Acids on Proliferation, Superoxide Production, Adhesion and Migration of Human Tumor Cells in Vitro. Eur. J. Pharmacol. 2015, 766, 99–105. [Google Scholar] [CrossRef]
- Zhou, Y.; Zheng, J.; Li, Y.; Xu, D.P.; Li, S.; Chen, Y.M.; Li, H.B. Natural Polyphenols for Prevention and Treatment of Cancer. Nutrients 2016, 8, 515. [Google Scholar] [CrossRef] [Green Version]
- Eroğlu, C.; Seçme, M.; Bağci, G.; Dodurga, Y. Assessment of the Anticancer Mechanism of Ferulic Acid via Cell Cycle and Apoptotic Pathways in Human Prostate Cancer Cell Lines. Tumor Biol. 2015, 36, 9437–9446. [Google Scholar] [CrossRef]
- Dodurga, Y.; Eroğlu, C.; Seçme, M.; Elmas, L.; Avcı, Ç.B.; Şatıroğlu-Tufan, N.L. Anti-Proliferative and Anti-Invasive Effects of Ferulic Acid in TT Medullary Thyroid Cancer Cells Interacting with URG4/URGCP. Tumor Biol. 2016, 37, 1933–1940. [Google Scholar] [CrossRef] [PubMed]
- Boz, H. P-Coumaric Acid in Cereals: Presence, Antioxidant and Antimicrobial Effects. Int. J. Food Sci. Technol. 2015, 50, 2323–2328. [Google Scholar] [CrossRef]
- Sharma, S.H.; Rajamanickam, V.; Nagarajan, S. Antiproliferative Effect of p-Coumaric Acid Targets UPR Activation by Downregulating Grp78 in Colon Cancer. Chem. -Biol. Interact. 2018, 291, 16–28. [Google Scholar] [CrossRef] [PubMed]
- Block, G.; Patterson, B.; Subar, A. Fruit, Vegetables, and Cancer Prevention: A Review of the Epidemiological Evidence. Nutr. Cancer. 1992, 18, 1–29. [Google Scholar] [CrossRef] [PubMed]
- Brusselmans, K.; Chrijver, E.D.E.S.; Eyns, W.H.; Erhoeven, G.V.; Winnen, J.V.S. Epigallocatechin-3-Gallate Is a Potent Natural Inhibitor of Fatty Acid Synthase in Intact Cells and Selectively Induces Apoptosis in Prostate Cancer Cells. Int. J. Cancer. 2003, 106, 856–862. [Google Scholar] [CrossRef]
- Kopustinskiene, D.M.; Jakstas, V.; Savickas, A.; Bernatoniene, J. Flavonoids as Anticancer Agents. Nutrients 2020, 12, 457. [Google Scholar] [CrossRef] [Green Version]
- Maleki, S.J.; Crespo, J.F.; Cabanillas, B. Anti-Inflammatory Effects of Flavonoids. Food Chem. 2019, 299, 1–11. [Google Scholar] [CrossRef]
- Agati, G.; Brunetti, C.; Fini, A.; Gori, A.; Guidi, L.; Landi, M.; Sebastiani, F.; Tattini, M. Are Flavonoids Effective Antioxidants in Plants? Twenty Years of Our Investigation. Antioxidants 2020, 9, 1098. [Google Scholar] [CrossRef]
- Farhadi, F.; Khameneh, B.; Iranshahi, M.; Iranshahy, M. Antibacterial Activity of Flavonoids and Their Structure–Activity Relationship: An Update Review. Phyther. Res. 2019, 33, 13–40. [Google Scholar] [CrossRef] [Green Version]
- Srivastava, J.K.; Gupta, S. Extraction, Characterization, Stability and Biological Activity of Flavonoids Isolated from Chamomile Flowers. Mol. Cell. Pharmacol. 2009, 1, 138. [Google Scholar] [CrossRef]
- Hussain, A.R.; Khan, A.S.; Ahmed, S.O.; Ahmed, M.; Platanias, L.C.; Al-Kuraya, K.S.; Uddin, S. Apigenin Induces Apoptosis via Downregulation of S-Phase Kinase-Associated Protein 2-Mediated Induction of P27Kip1 in Primary Effusion Lymphoma Cells. Cell Prolif. 2010, 43, 170–183. [Google Scholar] [CrossRef] [PubMed]
- Tao, S.; He, H.; Chen, Q. Quercetin Inhibits Proliferation and Invasion Acts by Up-Regulating MiR-146a in Human Breast Cancer Cells. Mol. Cell. Biochem. 2015, 402, 93–100. [Google Scholar] [CrossRef] [PubMed]
- Steiner, J.L.; Davis, J.M.; McClellan, J.L.; Enos, R.T.; Carson, J.A.; Fayad, R.; Nagarkatti, M.; Nagarkatti, P.S.; Altomare, D.; Creek, K.E.; et al. Dose-Dependent Benefits of Quercetin on Tumorigenesis in the C3(1)/SV40Tag Transgenic Mouse Model of Breast Cancer. Cancer Biol. Ther. 2014, 15, 1456–1467. [Google Scholar] [CrossRef] [PubMed]
- Srivastava, J.K.; Gupta, S. Antiproliferative and Apoptotic Effects of Chamomile Extract in Various Human Cancer Cells. J. Agric. Food Chem. 2007, 55, 9470–9478. [Google Scholar] [CrossRef]
- Tuorkey, M.J. Molecular Targets of Luteolin in Cancer. Eur. J. Cancer Prev. 2016, 25, 65–76. [Google Scholar] [CrossRef] [Green Version]
- Imran, M.; Rauf, A.; Abu-Izneid, T.; Nadeem, M.; Shariati, M.A.; Khan, I.A.; Imran, A.; Orhan, I.E.; Rizwan, M.; Atif, M.; et al. Luteolin, a Flavonoid, as an Anticancer Agent: A Review. Biomed. Pharmacother. 2019, 112, 1–10. [Google Scholar] [CrossRef]
- Anand, A.; Khurana, R.; Wahal, N.; Mahajan, S.; Mehta, M.; Satija, S.; Sharma, N.; Vyas, M.; Khurana, N. Vanillin: A Comprehensive Review of Pharmacological Activities. Plant Arch. 2019, 19, 1000–1004. [Google Scholar]
- Rizwana, H.; Alwhibi, M.S.; Soliman, D.A. Research article antimicrobial activity and chemical composition of flowers of Matricaria aurea a native herb of Saudi Arabia. Int. J. Pharmacol. 2016, 12, 576–586. [Google Scholar] [CrossRef] [Green Version]
- Hajjaj, G.; Bahlouli, A.; Sayah, K.; Tajani, M.; Cherrah, Y.; Zellou, A. Phytochemical screening and in-vivo antipyretic activity of the aqueous extracts of three Moroccan medicinal Plants. Pharm. Biol. Eval. 2017, 4, 88–92. [Google Scholar] [CrossRef]
- Tholl, D. Biosynthesis and Biological Functions of Terpenoids in Plants. Biotechnol. Isoprenoids 2015, 148, 63–106. [Google Scholar] [CrossRef]
- Bartikova, H.; Hanusova, V.; Skalova, L.; Ambroz, M.; Bousova, I. Antioxidant, pro-Oxidant and Other Biological Activities of Sesquiterpenes. Curr. Top. Med. Chem. 2014, 14, 2478–2494. [Google Scholar] [CrossRef] [PubMed]
- Krishnamoorthy, K.; Subramaniam, P. Phytochemical Profiling of Leaf, Stem, and Tuber Parts of Solena amplexicaulis (Lam.) Gandhi Using GC-MS. Int. Sch. Res. Not. 2014, 2014, 1–13. [Google Scholar] [CrossRef] [Green Version]
- Babu, S.; Jayaraman, S. An Update on β-Sitosterol: A Potential Herbal Nutraceutical for Diabetic Management. Biomed. Pharmacother. 2020, 131, 8p. [Google Scholar] [CrossRef] [PubMed]
- Fattore, E.; Fanelli, R. Palm Oil and Palmitic Acid: A Review on Cardiovascular Effects and Carcinogenicity. Int. J. Food Sci. Nutr. 2013, 64, 648–659. [Google Scholar] [CrossRef] [PubMed]









| Content (µg/g DW) | |||||
|---|---|---|---|---|---|
| Compounds | Flowers (CM-F) | Leaves (CM-L) | Stems (CM-S) | Roots (CM-R) | |
| Phenolic acids | Gallic acid | 13.23 ± 0.12 q | 11.17 ± 0.26 o | 7.14 ± 0.07 q | 9.55 ± 0.19 q |
| Protocatechuic acid | 216.11 ± 0.32 n | 41.06 ± 0.43 m | 124.29 ± 0.96 k | 96.68 ± 0.93 kl | |
| Chlorogenic acid | 1987.02 ± 0.69 a | 348.42 ± 0.60 e | 894.49 ± 0.02 q | 561.82 ± 0.94 b | |
| Salicylic acid | 318.11 ± 0.41 j | 133.35 ± 0.11 j | 122.05 ± 0.84 k | 110.20 ± 0.66 ij | |
| p-Hydroxybenzoic acid | 701.10 ± 0.04 f | 65.89 ± 0.35 l | 175.49 ± 0.02 i | 184.41 ± 0.07 g | |
| Caffeic acid | 206.71 ± 0.50 n | 126.80 ± 0.98 j | 123.02 ± 0.21 k | 86.29 ± 0.13 lm | |
| Vanillic acid | -- | 77.51 ± 0.52 l | 192.89 ± 0.12 h | 130.13 ± 0.46 h | |
| Syringic acid | 345.23 ± 0.60 i | 146.81 ± 0.20 i | 135.31 ± 0.39 j | 58.94 ± 0.90 o | |
| Rosmarinic acid | 102.10 ± 0.72 p | 38.04 ± 0.23 m | 14.82 ± 0.23 pq | 11.06 ± 0.15 q | |
| Ellagic acid | 1666.22 ± 0.5 b | 1095.01 ± 0.43 a | 470.40 ± 0.56 d | 415.21 ± 0.53 c | |
| p-Coumaric acid | 407.13 ± 0.77 h | 191.44 ± 0.70 g | 92.76 ± 0.26 m | 83.05 ± 0.27 m | |
| Methyl paraben | 265.61 ± 0.35 l | 16.63 ± 0.15 n o | 18.73 ± 0.91 p | 34.71 ± 0.81 p | |
| Ferulic acid | 161.34 ± 0.16 o | 105.45 ± 0.46 k | 102.22 ± 0.76 l | 82.04 ± 0.75 m | |
| Flavonoids | Luteolin-7-O-glucoside | 836.30 ± 0.38 e | 424.07 ± 0.08 c | 332.46 ± 0.59 e | 305.12 ± 0.88 d |
| Apigenin-7-O-glucoside | 1074.03 ± 0.21 d | 958.59 ± 0.41 b | 819.60 ± 0.30 b | 603.02 ± 0.80 a | |
| Luteolin | 257.54 ± 0.71 m | 169.50 ± 0.33 h | 84.25 ± 0.49 m | 67.38 ± 0.88 no | |
| Apigenin | 119.14 ± 0.42 p | 37.14 ± 0.53 m | 29.83 ± 0.12 o | 54.01 ± 0.51 o | |
| Quercetin | 1292.01 ± 0.85 c | 23.38 ± 0.80 n | 307.33 ± 0.86 f | 73.63 ± 0.63 mn | |
| Rutin | 673.12 ± 0.99 g | 377.05 ± 0.55 d | 565.20 ± 0.58 c | 241.15 ± 0.53 f | |
| Naringin | 298.30 ± 0.02 jk | 220.61 ± 0.37 f | 141.63 ± 0.70 j | 105.61 ± 0.18 jk | |
| Catechin | 347.71 ± 0.22 i | 114.42 ± 0.74 k | 240.41 ± 0.12 g | 268.40 ± 0.28 e | |
| Vanillin | 141.94 ± 0.87 o | 138.04 ± 0.60 ij | 140.11 ± 0.79 j | 122.73 ± 0.71 hi | |
| Kaempferol | 290.60 ± 0.03 k | 69.57 ± 0.02 l | 72.98 ± 0.19 n | 39.90 ± 0.53 p | |
| Isorhamnetin | 237.53 ± 0.64 m | 110.90 ± 0.78 k | 108.72 ± 0.92 l | 129.65 ± 0.80 h | |
| Area (%) | ||||
|---|---|---|---|---|
| Compound Groups | Flowers (CM-F) | Leaves (CM-L) | Stems (CM-S) | Roots (CM-R) |
| Terpenoids | 10.41 | 46.20 | 11.32 | 10.88 |
| Esters | 13.88 | 13.21 | 30.11 | 21.91 |
| Alcohols | -- | 6.74 | 5.05 | 24.49 |
| Alkanes | 15.14 | 2.63 | 18.13 | 3.14 |
| Fatty acids | 27.86 | 11.88 | 6.18 | 8.23 |
| Organic acids | 3.07 | 1.85 | 2.74 | 4.7 |
| Benzene and its derivatives | 2.85 | 7.62 | 5.73 | 8.15 |
| Phenols | 0.41 | 0.52 | 1.61 | 6 |
| Ketones | -- | 1.25 | 4.47 | 1.67 |
| Carbonyls | 19.27 | 1.34 | -- | -- |
| Amines | 1.62 | 2.32 | 6.9 | 0.7 |
| Pyrrolidines/pyrimidines | 0.97 | 0.22 | 3.04 | 3.36 |
| Steroids | -- | 2.32 | -- | -- |
| Others | 4.52 | 1.88 | 4.72 | 6.77 |
| Total | 100 | 99.98 | 100 | 100 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
El Mihyaoui, A.; Charfi, S.; Erbiai, E.H.; Pereira, M.; Duarte, D.; Vale, N.; Candela Castillo, M.E.; Badoc, A.; Lamarti, A.; Esteves da Silva, J.C.G.; et al. Phytochemical Compounds and Anticancer Activity of Cladanthus mixtus Extracts from Northern Morocco. Cancers 2023, 15, 152. https://doi.org/10.3390/cancers15010152
El Mihyaoui A, Charfi S, Erbiai EH, Pereira M, Duarte D, Vale N, Candela Castillo ME, Badoc A, Lamarti A, Esteves da Silva JCG, et al. Phytochemical Compounds and Anticancer Activity of Cladanthus mixtus Extracts from Northern Morocco. Cancers. 2023; 15(1):152. https://doi.org/10.3390/cancers15010152
Chicago/Turabian StyleEl Mihyaoui, Amina, Saoulajan Charfi, El Hadi Erbiai, Mariana Pereira, Diana Duarte, Nuno Vale, María Emilia Candela Castillo, Alain Badoc, Ahmed Lamarti, Joaquim C. G. Esteves da Silva, and et al. 2023. "Phytochemical Compounds and Anticancer Activity of Cladanthus mixtus Extracts from Northern Morocco" Cancers 15, no. 1: 152. https://doi.org/10.3390/cancers15010152
APA StyleEl Mihyaoui, A., Charfi, S., Erbiai, E. H., Pereira, M., Duarte, D., Vale, N., Candela Castillo, M. E., Badoc, A., Lamarti, A., Esteves da Silva, J. C. G., & Arnao, M. B. (2023). Phytochemical Compounds and Anticancer Activity of Cladanthus mixtus Extracts from Northern Morocco. Cancers, 15(1), 152. https://doi.org/10.3390/cancers15010152