Occupational Exposures and Risks of Non-Hodgkin Lymphoma: A Meta-Analysis
Abstract
:Simple Summary
Abstract
1. Introduction
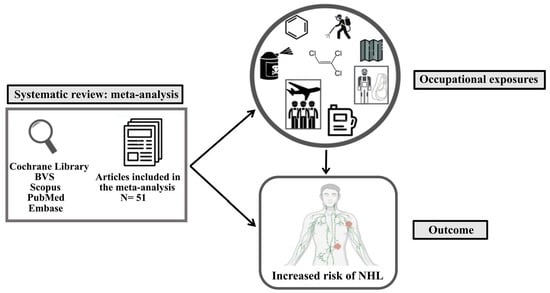
2. Materials and Methods
2.1. Search Strategy
2.2. Study Selection and Data Extraction
2.3. Quality Assessment
2.4. Data Analysis of the Systematic Review
- wk = (bk ck)/nk
- K = total number of studies
- k = 1, 2,…, K
- ψk = (ak dk)/(bk ck)
- nk = study sample size k
- ak = number of events in the group exposed in the study k
- bk = number of non-events in the group exposed in the study k
- ck = number of events in the unexposed group in the study k
- dk = number of non-events in the non-exposed group in the study k
- nk = sample size (all studies)
3. Results and Discussion
3.1. Characterization of the Studies
3.2. Characteristics of the Studies Included in the Meta-Analysis
3.3. Strengths
3.4. Limitations
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ansell, S.M. Non-Hodgkin Lymphoma: Diagnosis and Treatment. Mayo Clin. Proc. 2015, 90, 1152–1163. [Google Scholar] [CrossRef]
- Rieutort, D.; Moyne, O.; Cocco, P.; Gaudemaris, R.d.; Bicout, D.J. Ranking Occupational Contexts Associated with Risk of Non-Hodgkin Lymphoma. Am. J. Ind. Med. 2016, 59, 561–574. [Google Scholar] [CrossRef]
- Moubadder, L.; McCullough, L.E.; Flowers, C.R.; Koff, J.L. Linking Environmental Exposures to Molecular Pathogenesis in Non-Hodgkin Lymphoma Subtypes. Cancer Epidemiol. Biomark. Prev. 2020, 29, 1844–1855. [Google Scholar] [CrossRef]
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef]
- Hartge, P.; Smith, M.T. Environmental and Behavioral Factors and the Risk of Non-Hodgkin Lymphoma. Cancer Epidemiol. Biomark. Prev. 2007, 16, 367–368. [Google Scholar] [CrossRef]
- Estimativa 2020: Incidência de Câncer No Brasil|INCA—Instituto Nacional de Câncer. Available online: https://www.inca.gov.br/publicacoes/livros/estimativa-2020-incidencia-de-cancer-no-brasil (accessed on 4 July 2021).
- Benavente, Y.; Costas, L.; Rodríguez-Suarez, M.M.; Alguacil, J.; Santibáñez, M.; Vila, J.; Robles, C.; Alonso, E.; de la Banda, E.; Gonzalez-Barca, E.; et al. Occupational Exposure to Pesticides and Chronic Lymphocytic Leukaemia in the MCC-Spain Study. Int. J. Environ. Res. Public Health 2020, 17, 5174. [Google Scholar] [CrossRef]
- Cocco, P.; Vermeulen, R.; Flore, V.; Nonne, T.; Campagna, M.; Purdue, M.; Blair, A.; Monnereau, A.; Orsi, L.; Clavel, J.; et al. Occupational Exposure to Trichloroethylene and Risk of Non-Hodgkin Lymphoma and Its Major Subtypes: A Pooled IinterLlymph Analysis. Occup. Environ. Med. 2013, 70, 795–802. [Google Scholar] [CrossRef]
- Cocco, P.; t’Mannetje, A.; Fadda, D.; Melis, M.; Becker, N.; Sanjosé, S.d.; Foretova, L.; Mareckova, J.; Staines, A.; Kleefeld, S.; et al. Occupational Exposure to Solvents and Risk of Lymphoma Subtypes: Results from the Epilymph Case–Control Study. Occup. Environ. Med. 2010, 67, 341–347. [Google Scholar] [CrossRef]
- Gold, L.S.; Stewart, P.A.; Milliken, K.; Purdue, M.; Severson, R.; Seixas, N.; Blair, A.; Hartge, P.; Davis, S.; De Roos, A.J. The Relationship between Multiple Myeloma and Occupational Exposure to Six Chlorinated Solvents. Occup. Environ. Med. 2011, 68, 391–399. [Google Scholar] [CrossRef]
- Zakerinia, M.; Namdari, M.; Amirghofran, S. The Relationship between Exposure to Pesticides and the Occurrence of Lymphoid Neoplasm. Iran. Red Crescent Med. J. 2012, 14, 337–344. [Google Scholar]
- Van Balen, E.; Font, R.; Cavallé, N.; Font, L.; Garcia-Villanueva, M.; Benavente, Y.; Brennan, P.; de Sanjose, S. Exposure to Non-Arsenic Pesticides Is Associated with Lymphoma among Farmers in Spain. Occup. Environ. Med. 2006, 63, 663–668. [Google Scholar] [CrossRef]
- Bracci, P.M.; Benavente, Y.; Turner, J.J.; Paltiel, O.; Slager, S.L.; Vajdic, C.M.; Norman, A.D.; Cerhan, J.R.; Chiu, B.C.H.; Becker, N.; et al. Medical History, Lifestyle, Family History, and Occupational Risk Factors for Marginal Zone Lymphoma: The InterLymph Non-Hodgkin Lymphoma Subtypes Project. J. Natl. Cancer Inst. Monogr. 2014, 2014, 52–65. [Google Scholar] [CrossRef]
- Cerhan, J.R.; Kricker, A.; Paltiel, O.; Flowers, C.R.; Wang, S.S.; Monnereau, A.; Blair, A.; Maso, L.D.; Kane, E.V.; Nieters, A.; et al. Medical History, Lifestyle, Family History, and Occupational Risk Factors for Diffuse Large B-Cell Lymphoma: The InterLymph Non-Hodgkin Lymphoma Subtypes Project. J. Natl. Cancer Inst. Monogr. 2014, 2014, 15–25. [Google Scholar] [CrossRef]
- Chia, S.E.; Wong, K.Y.; Tai, B.C. Occupation and Risk of Non-Hodgkin’s Lymphoma in Singapore. Occup. Med. 2012, 62, 29–33. [Google Scholar] [CrossRef]
- McLean, D.; Mannetje, A.T.; Dryson, E.; Walls, C.; McKenzie, F.; Maule, M.; Cheng, S.; Cunningham, C.; Kromhout, H.; Boffetta, P.; et al. Leukaemia and Occupation: A New Zealand Cancer Registry-Based Case-Control Study. Int. J. Epidemiol. 2009, 38, 594–606. [Google Scholar] [CrossRef]
- Mester, B.; Nieters, A.; Deeg, E.; Elsner, G.; Becker, N.; Seidler, A. Occupation and Malignant Lymphoma: A Population Based Case Control Study in Germany. Occup. Environ. Med. 2006, 63, 17–26. [Google Scholar] [CrossRef]
- Morton, L.M.; Slager, S.L.; Cerhan, J.R.; Wang, S.S.; Vajdic, C.M.; Skibola, C.F.; Bracci, P.M.; de Sanjosé, S.; Smedby, K.E.; Chiu, B.C.H.; et al. Etiologic Heterogeneity Among Non-Hodgkin Lymphoma Subtypes: The InterLymph Non-Hodgkin Lymphoma Subtypes Project. J. Natl. Cancer Inst. Monogr. 2014, 2014, 130–144. [Google Scholar] [CrossRef]
- Catalani, S.; Donato, F.; Tomasi, C.; Pira, E.; Apostoli, P.; Boffetta, P. Occupational and Environmental Exposure to Polychlorinated Biphenyls and Risk of Non-Hodgkin Lymphoma: A Systematic Review and Meta-Analysis of Epidemiology Studies. Eur. J. Cancer Prev. 2019, 28, 441–450. [Google Scholar] [CrossRef]
- Jephcote, C.; Brown, D.; Verbeek, T.; Mah, A. A Systematic Review and Meta-Analysis of Haematological Malignancies in Residents Living near Petrochemical Facilities. Environ. Health 2020, 19, 53. [Google Scholar] [CrossRef]
- Odutola, M.K.; Benke, G.; Fritschi, L.; Giles, G.G.; van Leeuwen, M.T.; Vajdic, C.M. A Systematic Review and Meta-Analysis of Occupational Exposures and Risk of Follicular Lymphoma. Environ. Res. 2021, 197, 110887. [Google Scholar] [CrossRef]
- Smith, A.M.; Smith, M.T.; La Merrill, M.A.; Liaw, J.; Steinmaus, C. 2,4-Dichlorophenoxyacetic Acid (2,4-D) and Risk of Non-Hodgkin Lymphoma: A Meta-Analysis Accounting for Exposure Levels. Ann. Epidemiol. 2017, 27, 281–289.e4. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. BMJ 2009, 339, b2535. [Google Scholar] [CrossRef]
- Shamseer, L.; Moher, D.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A. PRISMA-P Group Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols (PRISMA-P) 2015: Elaboration and Explanation. BMJ 2015, 350, g7647. [Google Scholar] [CrossRef]
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan—A Web and Mobile App for Systematic Reviews. Syst. Rev. 2016, 5, 1–10. [Google Scholar] [CrossRef]
- Ghimire, P.R.; Agho, K.E.; Akombi, B.J.; Wali, N.; Dibley, M.; Raynes-Greenow, C.; Renzaho, A.M.N. Perinatal Mortality in South Asia: Systematic Review of Observational Studies. Int. J. Environ. Res. Public Health 2018, 15, 1428. [Google Scholar] [CrossRef]
- Schwarzer, G.; Carpenter, J.R.; Rücker, G. Fixed Effect and Random Effects Meta-Analysis. In Meta-Analysis with R; Schwarzer, G., Carpenter, J.R., Rücker, G., Eds.; Use R! Springer International Publishing: Cham, Switzerland, 2015; pp. 21–53. ISBN 978-3-319-21416-0. [Google Scholar]
- Dwamena, B. MIDAS: Stata Module for Meta-Analytical Integration of Diagnostic Test Accuracy Studies. 2009. Available online: https://ideas.repec.org/c/boc/bocode/s456880.html (accessed on 7 March 2023).
- Deeks, J.J.; Macaskill, P.; Irwig, L. The Performance of Tests of Publication Bias and Other Sample Size Effects in Systematic Reviews of Diagnostic Test Accuracy Was Assessed. J. Clin. Epidemiol. 2005, 58, 882–893. [Google Scholar] [CrossRef]
- Alavanja, M.C.R.; Hofmann, J.N.; Lynch, C.F.; Hines, C.J.; Barry, K.H.; Barker, J.; Buckman, D.W.; Thomas, K.; Sandler, D.P.; Hoppin, J.A.; et al. Non-Hodgkin Lymphoma Risk and Insecticide, Fungicide and Fumigant Use in the Agricultural Health Study. PLoS ONE 2014, 9, e109332. [Google Scholar] [CrossRef]
- Beane Freeman, L.E.; Deroos, A.J.; Koutros, S.; Blair, A.; Ward, M.H.; Alavanja, M.; Hoppin, J.A. Poultry and Livestock Exposure and Cancer Risk among Farmers in the Agricultural Health Study. Cancer Causes Control 2012, 23, 663–670. [Google Scholar] [CrossRef]
- Bonner, M.R.; Williams, B.A.; Rusiecki, J.A.; Blair, A.; Freeman, L.E.B.; Hoppin, J.A.; Dosemeci, M.; Lubin, J.; Sandler, D.P.; Alavanja, M.C.R. Occupational Exposure to Terbufos and the Incidence of Cancer in the Agricultural Health Study. Cancer Causes Control 2010, 21, 871–877. [Google Scholar] [CrossRef]
- Bonner, M.R.; Coble, J.; Blair, A.; Beane Freeman, L.E.; Hoppin, J.A.; Sandler, D.P.; Alavanja, M.C.R. Malathion Exposure and the Incidence of Cancer in the Agricultural Health Study. Am. J. Epidemiol. 2007, 166, 1023–1034. [Google Scholar] [CrossRef]
- De Roos, A.J.; Blair, A.; Rusiecki, J.A.; Hoppin, J.A.; Svec, M.; Dosemeci, M.; Sandler, D.P.; Alavanja, M.C. Cancer Incidence among Glyphosate-Exposed Pesticide Applicators in the Agricultural Health Study. Environ. Health Perspect. 2005, 113, 49–54. [Google Scholar] [CrossRef]
- Koutros, S.; Alavanja, M.C.R.; Lubin, J.H.; Sandler, D.P.; Hoppin, J.A.; Lynch, C.F.; Knott, C.; Blair, A.; Beane Freeman, L.E. An Update of Cancer Incidence in the Agricultural Health Study. J. Occup. Environ. Med. 2010, 52, 1098–1105. [Google Scholar] [CrossRef]
- Lerro, C.C.; Koutros, S.; Andreotti, G.; Sandler, D.P.; Lynch, C.F.; Louis, L.M.; Blair, A.; Parks, C.G.; Shrestha, S.; Lubin, J.H.; et al. Cancer Incidence in the Agricultural Health Study after Twenty Years of Follow-Up. Cancer Causes Control 2019, 30, 311–322. [Google Scholar] [CrossRef]
- Lynch, S.M.; Mahajan, R.; Freeman, L.E.B.; Hoppin, J.A.; Alavanja, M.C.R. Cancer Incidence among Pesticide Applicators Exposed to Butylate in the Agricultural Health Study (AHS). Environ. Res. 2009, 109, 860–868. [Google Scholar] [CrossRef]
- Mahajan, R.; Blair, A.; Coble, J.; Lynch, C.F.; Hoppin, J.A.; Sandler, D.P.; Alavanja, M.C.R. Carbaryl Exposure and Incident Cancer in the Agricultural Health Study. Int. J. Cancer 2007, 121, 1799–1805. [Google Scholar] [CrossRef]
- Park, S.K.; Kang, D.; Beane-Freeman, L.; Gwak, J.; Hoppin, J.A.; Sandler, D.P.; Knott, C.; Lynch, C.F.; Blair, A.; Alavanja, M. Cancer Incidence among Paraquat-Exposed Pesticide Applicators in the Agricultural Health Study. Int. J. Occup. Environ. Health 2009, 15, 274–281. [Google Scholar]
- Purdue, M.P.; Hoppin, J.A.; Blair, A.; Dosemeci, M.; Alavanja, M.C.R. Occupational Exposure to Organochlorine Insecticides and Cancer Incidence in the Agricultural Health Study. Int. J. Cancer 2007, 120, 642–649. [Google Scholar] [CrossRef]
- Rusiecki, J.A.; Patel, R.; Koutros, S.; Beane-Freeman, L.; Landgren, O.; Bonner, M.R.; Coble, J.; Lubin, J.; Blair, A.; Hoppin, J.A.; et al. Cancer Incidence among Pesticide Applicators Exposed to Permethrin in the Agricultural Health Study. Environ. Health Perspect. 2009, 117, 581–586. [Google Scholar] [CrossRef]
- Fisher, J.A.; Freeman, L.E.B.; Hofmann, J.N.; Blair, A.; Parks, C.G.; Thorne, P.S.; Ward, M.H.; Jones, R.R. Residential Proximity to Intensive Animal Agriculture and Risk of Lymphohematopoietic Cancers in the Agricultural Health Study. Epidemiology 2020, 31, 478–489. [Google Scholar] [CrossRef]
- Aschebrook-Kilfoy, B.; Cocco, P.; La Vecchia, C.; Chang, E.T.; Vajdic, C.M.; Kadin, M.E.; Spinelli, J.J.; Morton, L.M.; Kane, E.V.; Sampson, J.N.; et al. Medical History, Lifestyle, Family History, and Occupational Risk Factors for Mycosis Fungoides and Sézary Syndrome: The InterLymph Non-Hodgkin Lymphoma Subtypes Project. J. Natl. Cancer Inst. Monogr. 2014, 2014, 98–105. [Google Scholar] [CrossRef]
- ’t Mannetje, A.; De Roos, A.J.; Boffetta, P.; Vermeulen, R.; Benke, G.; Fritschi, L.; Brennan, P.; Foretova, L.; Maynadié, M.; Becker, N.; et al. Occupation and Risk of Non-Hodgkin Lymphoma and Its Subtypes: A Pooled Analysis from the InterLymph Consortium. Environ. Health Perspect. 2016, 124, 396–405. [Google Scholar] [CrossRef]
- Wang, S.S.; Flowers, C.R.; Kadin, M.E.; Chang, E.T.; Hughes, A.M.; Ansell, S.M.; Feldman, A.L.; Lightfoot, T.; Boffetta, P.; Melbye, M.; et al. Medical History, Lifestyle, Family History, and Occupational Risk Factors for Peripheral T-Cell Lymphomas: The InterLymph Non-Hodgkin Lymphoma Subtypes Project. J. Natl. Cancer Inst. Monogr. 2014, 2014, 66–75. [Google Scholar] [CrossRef]
- Hu, L.; Luo, D.; Zhou, T.; Tao, Y.; Feng, J.; Mei, S. The Association between Non-Hodgkin Lymphoma and Organophosphate Pesticides Exposure: A Meta-Analysis. Environ. Pollut. 2017, 231, 319–328. [Google Scholar] [CrossRef]
- Zhang, L.; Rana, I.; Shaffer, R.M.; Taioli, E.; Sheppard, L. Exposure to Glyphosate-Based Herbicides and Risk for Non-Hodgkin Lymphoma: A Meta-Analysis and Supporting Evidence. Mutat Res. Rev. Mutat. Res. 2019, 781, 186–206. [Google Scholar] [CrossRef]
- Linet, M.S.; Gilbert, E.S.; Vermeulen, R.; Dores, G.M.; Yin, S.-N.; Portengen, L.; Hayes, R.B.; Ji, B.-T.; Lan, Q.; Li, G.-L.; et al. Benzene Exposure-Response and Risk of Lymphoid Neoplasms in Chinese Workers: A Multicenter Case-Cohort Study. Am. J. Ind. Med. 2020, 63, 741–754. [Google Scholar] [CrossRef]
- Satta, G.; Loi, M.; Becker, N.; Benavente, Y.; De Sanjose, S.; Foretova, L.; Staines, A.; Maynadie, M.; Nieters, A.; Meloni, F.; et al. Occupational Exposure to Ionizing Radiation and Risk of Lymphoma Subtypes: Results of the Epilymph European Case-Control Study. Environ. Health 2020, 19, 43. [Google Scholar] [CrossRef]
- Loomis, D.; Guha, N.; Kogevinas, M.; Fontana, V.; Gennaro, V.; Kolstad, H.A.; McElvenny, D.M.; Sallmén, M.; Saracci, R. Cancer Mortality in an International Cohort of Reinforced Plastics Workers Exposed to Styrene: A Reanalysis. Occup. Environ. Med. 2019, 76, 157–162. [Google Scholar] [CrossRef]
- Jordan, H.T.; Stein, C.R.; Li, J.; Cone, J.E.; Stayner, L.; Hadler, J.L.; Brackbill, R.M.; Farfel, M.R. Mortality among Rescue and Recovery Workers and Community Members Exposed to the September 11, 2001 World Trade Center Terrorist Attacks, 2003–2014. Environ. Res. 2018, 163, 270–279. [Google Scholar] [CrossRef]
- McBride, D.I.; Collins, J.J.; Bender, T.J.; Bodner, K.M.; Aylward, L.L. Cohort Study of Workers at a New Zealand Agrochemical Plant to Assess the Effect of Dioxin Exposure on Mortality. BMJ Open 2018, 8, e019243. [Google Scholar] [CrossRef]
- Tsai, S.-S.; Weng, Y.-H.; Chiu, Y.-W.; Yang, C.-Y. Farming and Mortality Rates Attributed to Non-Hodgkin’s Lymphoma in Taiwan. J. Toxicol. Environ. Health Part A 2018, 81, 31–36. [Google Scholar] [CrossRef]
- Boccolini, P.d.M.M.; Boccolini, C.S.; Chrisman, J.d.R.; Koifman, R.J.; Meyer, A. Non-Hodgkin Lymphoma among Brazilian Agricultural Workers: A Death Certificate Case-Control Study. Arch. Environ. Occup. Health 2017, 72, 139–144. [Google Scholar] [CrossRef]
- Ferri, G.M.; Specchia, G.; Mazza, P.; Ingravallo, G.; Intranuovo, G.; Guastadisegno, C.M.; Congedo, M.L.; Lagioia, G.; Loparco, M.C.; Giordano, A.; et al. Risk of Lymphoma Subtypes by Occupational Exposure in Southern Italy. J. Occup. Med. Toxicol. 2017, 12, 31. [Google Scholar] [CrossRef]
- Lemarchand, C.; Tual, S.; Levêque-Morlais, N.; Perrier, S.; Belot, A.; Velten, M.; Guizard, A.-V.; Marcotullio, E.; Monnereau, A.; Clin, B.; et al. Cancer Incidence in the AGRICAN Cohort Study (2005-2011). Cancer Epidemiol. 2017, 49, 175–185. [Google Scholar] [CrossRef]
- González, A.B.d.; Ntowe, E.; Kitahara, C.M.; Gilbert, E.; Miller, D.L.; Kleinerman, R.A.; Linet, M.S. Long-Term Mortality in 43 763 U.S. Radiologists Compared with 64 990 U.S. Psychiatrists. Radiology 2016, 281, 847. [Google Scholar] [CrossRef]
- Bassig, B.A.; Friesen, M.C.; Vermeulen, R.; Shu, X.-O.; Purdue, M.P.; Stewart, P.A.; Xiang, Y.-B.; Chow, W.-H.; Zheng, T.; Ji, B.-T.; et al. Occupational Exposure to Benzene and Non-Hodgkin Lymphoma in a Population-Based Cohort: The Shanghai Women’s Health Study. Environ. Health Perspect. 2015, 123, 971–977. [Google Scholar] [CrossRef]
- Kachuri, L.; Demers, P.A.; Blair, A.; Spinelli, J.J.; Pahwa, M.; McLaughlin, J.R.; Pahwa, P.; Dosman, J.A.; Harris, S.A. Multiple Pesticide Exposures and the Risk of Multiple Myeloma in Canadian Men. Int. J. Cancer 2013, 133, 1846–1858. [Google Scholar] [CrossRef]
- Karunanayake, C.P.; Dosman, J.A.; Pahwa, P. Non-Hodgkin’s Lymphoma and Work in Agriculture: Results of a Two Case-Control Studies in Saskatchewan, Canada. Indian J. Occup. Environ. Med. 2013, 17, 114–121. [Google Scholar] [CrossRef]
- Li, J.; Cone, J.E.; Kahn, A.R.; Brackbill, R.M.; Farfel, M.R.; Greene, C.M.; Hadler, J.L.; Stayner, L.T.; Stellman, S.D. Association Between World Trade Center Exposure and Excess Cancer Risk. JAMA 2012, 308, 2479–2488. [Google Scholar] [CrossRef]
- Lipworth, L.; Sonderman, J.S.; Mumma, M.T.; Tarone, R.E.; Marano, D.E.; Boice, J.D.J.; McLaughlin, J.K. Cancer Mortality Among Aircraft Manufacturing Workers: An Extended Follow-Up. J. Occup. Environ. Med. 2011, 53, 992–1007. [Google Scholar] [CrossRef]
- Purdue, M.P.; Bakke, B.; Stewart, P.; De Roos, A.J.; Schenk, M.; Lynch, C.F.; Bernstein, L.; Morton, L.M.; Cerhan, J.R.; Severson, R.K.; et al. A Case–Control Study of Occupational Exposure to Trichloroethylene and Non-Hodgkin Lymphoma. Environ. Health Perspect. 2011, 119, 232–238. [Google Scholar] [CrossRef]
- Kiran, S.; Cocco, P.; Mannetje, A.; Satta, G.; D’Andrea, I.; Becker, N.; de Sanjosé, S.; Foretova, L.; Staines, A.; Kleefeld, S.; et al. Occupational Exposure to Ethylene Oxide and Risk of Lymphoma. Epidemiology 2010, 21, 905–910. [Google Scholar] [CrossRef]
- Seidler, A.; Becker, N.; Nieters, A.; Arhelger, R.; Mester, B.; Rossnagel, K.; Deeg, E.; Elsner, G.; Melis, M.; Sesler, S.; et al. Asbestos Exposure and Malignant Lymphoma: A Multicenter Case–Control Study in Germany and Italy. Int. Arch. Occup. Environ. Health 2010, 83, 563–570. [Google Scholar] [CrossRef]
- Wong, O.; Harris, F.; Wang, Y.; Fu, H. A Hospital-Based Case-Control Study of Non-Hodgkin Lymphoid Neoplasms in Shanghai: Analysis of Personal Characteristics, Lifestyle, and Environmental Risk Factors by Subtypes of the WHO Classification. J. Occup. Environ. Med. 2010, 52, 39–53. [Google Scholar] [CrossRef]
- McBride, D.I.; Collins, J.J.; Humphry, N.F.; Herbison, P.; Bodner, K.M.; Aylward, L.L.; Burns, C.J.; Wilken, M. Mortality in Workers Exposed to 2,3,7,8-Tetrachlorodibenzo-p-Dioxin at a Trichlorophenol Plant in New Zealand. J. Occup. Environ Med. 2009, 51, 1049–1056. [Google Scholar] [CrossRef]
- Wang, R.; Zhang, Y.; Lan, Q.; Holford, T.R.; Leaderer, B.; Hoar Zahm, S.; Boyle, P.; Dosemeci, M.; Rothman, N.; Zhu, Y.; et al. Occupational Exposure to Solvents and Risk of Non-Hodgkin Lymphoma in Connecticut Women. Am. J. Epidemiol. 2009, 169, 176–185. [Google Scholar] [CrossRef]
- Kirkeleit, J.; Riise, T.; Bråtveit, M.; Moen, B.E. Increased Risk of Acute Myelogenous Leukemia and Multiple Myeloma in a Historical Cohort of Upstream Petroleum Workers Exposed to Crude Oil. Cancer Causes Control 2008, 19, 13–23. [Google Scholar] [CrossRef]
- Tranah, G.J.; Bracci, P.M.; Holly, E.A. Domestic and Farm-Animal Exposures and Risk of Non-Hodgkin Lymphoma in a Population-Based Study in the San Francisco Bay Area. Cancer Epidemiol. Biomark. Prev. 2008, 17, 2382–2387. [Google Scholar] [CrossRef]
- Moore, T.; Brennan, P.; Becker, N.; de Sanjosé, S.; Maynadié, M.; Foretova, L.; Cocco, P.; Staines, A.; Nieters, A.; Font, R.; et al. Occupational Exposure to Meat and Risk of Lymphoma: A Multicenter Case-Control Study from Europe. Int. J. Cancer 2007, 121, 2761–2766. [Google Scholar] [CrossRef]
- Xu, J.-X.; Hoshida, Y.; Yang, W.-I.; Inohara, H.; Kubo, T.; Kim, G.-E.; Yoon, J.-H.; Kojya, S.; Bandoh, N.; Harabuchi, Y.; et al. Life-Style and Environmental Factors in the Development of Nasal NK/T-Cell Lymphoma: A Case–Control Study in East Asia. Int. J. Cancer 2007, 120, 406–410. [Google Scholar] [CrossRef]
- Miligi, L.; Costantini, A.S.; Benvenuti, A.; Kriebel, D.; Bolejack, V.; Tumino, R.; Ramazzotti, V.; Rodella, S.; Stagnaro, E.; Crosignani, P.; et al. Occupational Exposure to Solvents and the Risk of Lymphomas. Epidemiology 2006, 17, 552–561. [Google Scholar] [CrossRef]
- Fritschi, L.; Benke, G.; Hughes, A.M.; Kricker, A.; Turner, J.; Vajdic, C.M.; Grulich, A.; Milliken, S.; Kaldor, J.; Armstrong, B.K. Occupational Exposure to Pesticides and Risk of Non-Hodgkin’s Lymphoma. Amr. J. Epidemiol. 2005, 162, 849–857. [Google Scholar] [CrossRef]
- Kato, I.; Koenig, K.L.; Watanabe-Meserve, H.; Baptiste, M.S.; Lillquist, P.P.; Frizzera, G.; Burke, J.S.; Moseson, M.; Shore, R.E. Personal and Occupational Exposure to Organic Solvents and Risk of Non-Hodgkin’s Lymphoma (NHL) in Women (United States). Cancer Causes Control 2005, 16, 1215–1224. [Google Scholar] [CrossRef]
- Chiu, B.C.-H.; Weisenburger, D.D.; Zahm, S.H.; Cantor, K.P.; Gapstur, S.M.; Holmes, F.; Burmeister, L.F.; Blair, A. Agricultural Pesticide Use, Familial Cancer, and Risk of Non-Hodgkin Lymphoma. Cancer Epidemiol. Biomark. Prev. 2004, 13, 525–531. [Google Scholar]
- Kato, I.; Watanabe-Meserve, H.; Koenig, K.L.; Baptiste, M.S.; Lillquist, P.P.; Frizzera, G.; Burke, J.S.; Moseson, M.; Shore, R.E. Pesticide Product Use and Risk of Non-Hodgkin Lymphoma in Women. Environ. Health Perspect. 2004, 112, 1275–1281. [Google Scholar] [CrossRef]
- De Roos, A.J.; Zahm, S.; Cantor, K.; Weisenburger, D.; Holmes, F.; Burmeister, L.; Blair, A. Integrative Assessment of Multiple Pesticides as Risk Factors for Non-Hodgkin’s Lymphoma among Men. Occup. Environ. Med. 2003, 60, e11. [Google Scholar] [CrossRef]
- Fritschi, L.; Johnson, K.C.; Kliewer, E.V.; Fry, R. Canadian Cancer Registries Epidemiology Research Group Animal-Related Occupations and the Risk of Leukemia, Myeloma, and Non-Hodgkin’s Lymphoma in Canada. Cancer Causes Control 2002, 13, 563–571. [Google Scholar] [CrossRef]
- Lee, E.; Burnett, C.A.; Lalich, N.; Cameron, L.L.; Sestito, J.P. Proportionate Mortality of Crop and Livestock Farmers in the United States, 1984–1993. Am. J. Ind. Med. 2002, 42, 410–420. [Google Scholar] [CrossRef]
- McDuffie, H.H.; Pahwa, P.; McLaughlin, J.R.; Spinelli, J.J.; Fincham, S.; Dosman, J.A.; Robson, D.; Skinnider, L.F.; Choi, N.W. Non-Hodgkin’s Lymphoma and Specific Pesticide Exposures in Men: Cross-Canada Study of Pesticides and Health. Cancer Epidemiol. Biomark. Prev. 2001, 10, 1155–1163. [Google Scholar]
- vanWijngaarden, E.; Savitz, D.A. Occupational Sunlight Exposure and Mortality From Non-Hodgkin Lymphoma Among Electric Utility Workers. J. Occup. Environ. Med. 2001, 43, 548–553. [Google Scholar]
- Zheng, T.; Zahm, S.H.; Cantor, K.P.; Weisenburger, D.D.; Zhang, Y.; Blair, A. Agricultural Exposure to Carbamate Pesticides and Risk of Non-Hodgkin Lymphoma. J. Occup. Environ. Med. 2001, 43, 641–649. [Google Scholar] [CrossRef]
- McGeoghegan, D.; Binks, K. The Mortality and Cancer Morbidity Experience of Workers at the Springfields Uranium Production Facility, 1946–1995. J. Radiol. Prot. 2000, 20, 111–137. [Google Scholar] [CrossRef]
- Thörn, Å.; Gustavsson, P.; Sadigh, J.; Westerlund-Hännestrand, B.; Hogstedt, C. Mortality and Cancer Incidence among Swedish Lumberjacks Exposed to Phenoxy Herbicides. Occup. Environ. Med. 2000, 57, 718–720. [Google Scholar] [CrossRef]
- Agents Classified by the IARC Monographs Volumes 1–132. 2022. Available online: https://monographs.iarc.who.int/list-of-classifications (accessed on 12 September 2022).
- Liu, Y.; Barta, S.K. Diffuse Large B-Cell Lymphoma: 2019 Update on Diagnosis, Risk Stratification, and Treatment. Am. J. Hematol. 2019, 94, 604–616. [Google Scholar] [CrossRef]
- Rana, I.; Dahlberg, S.; Steinmaus, C.; Zhang, L. Benzene Exposure and Non-Hodgkin Lymphoma: A Systematic Review and Meta-Analysis of Human Studies. Lancet Planet Health 2021, 5, e633–e643. [Google Scholar] [CrossRef]
- Merhi, M.; Raynal, H.; Cahuzac, E.; Vinson, F.; Cravedi, J.P.; Gamet-Payrastre, L. Occupational Exposure to Pesticides and Risk of Hematopoietic Cancers: Meta-Analysis of Case–Control Studies. Cancer Causes Control 2007, 18, 1209–1226. [Google Scholar] [CrossRef]
- Karami, S.; Bassig, B.; Stewart, P.A.; Lee, K.-M.; Rothman, N.; Moore, L.E.; Lan, Q. Occupational Trichloroethylene Exposure and Risk of Lymphatic and Haematopoietic Cancers: A Meta-Analysis. Occup. Environ. Med. 2013, 70, 591–599. [Google Scholar] [CrossRef]
- Alicandro, G.; Rota, M.; Boffetta, P.; La Vecchia, C. Occupational Exposure to Polycyclic Aromatic Hydrocarbons and Lymphatic and Hematopoietic Neoplasms: A Systematic Review and Meta-Analysis of Cohort Studies. Arch. Toxicol. 2016, 90, 2643–2656. [Google Scholar] [CrossRef]
- Chang, E.T.; Delzell, E. Systematic Review and Meta-Analysis of Glyphosate Exposure and Risk of Lymphohematopoietic Cancers. J. Environ. Sci. Health B 2016, 51, 402–434. [Google Scholar] [CrossRef]
- Clough, L.; Bayakly, A.R.; Ward, K.C.; Khan, M.K.; Chen, S.C.; Lechowicz, M.J.; Flowers, C.R.; Allen, P.B.; Switchenko, J.M. Clustering of Cutaneous T-Cell Lymphoma Is Associated with Increased Levels of the Environmental Toxins Benzene and Trichloroethylene in the State of Georgia. Cancer 2020, 126, 1700–1707. [Google Scholar] [CrossRef]
- Schinasi, L.; Leon, M.E. Non-Hodgkin Lymphoma and Occupational Exposure to Agricultural Pesticide Chemical Groups and Active Ingredients: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2014, 11, 4449–4527. [Google Scholar] [CrossRef]
- Steinmaus, C.; Smith, A.H.; Jones, R.M.; Smith, M.T. Meta-Analysis of Benzene Exposure and Non-Hodgkin Lymphoma: Biases Could Mask an Important Association. Occupr. Environ. Medr. 2008, 65, 371–378. [Google Scholar] [CrossRef]
- Kane, E.V.; Newton, R. Benzene and the Risk of Non-Hodgkin Lymphoma: A Review and Meta-Analysis of the Literature. Cancer Epidemiol. 2010, 34, 7–12. [Google Scholar] [CrossRef]
- Raaschou-Nielsen, O.; Hansen, J.; McLaughlin, J.K.; Kolstad, H.; Christensen, J.M.; Tarone, R.E.; Olsen, J.H. Cancer Risk among Workers at Danish Companies Using Trichloroethylene: A Cohort Study. Am. J. Epidemiol. 2003, 158, 1182–1192. [Google Scholar] [CrossRef]
- Alaggio, R.; Amador, C.; Anagnostopoulos, I.; Attygalle, A.D.; Araujo, I.B.d.O.; Berti, E.; Bhagat, G.; Borges, A.M.; Boyer, D.; Calaminici, M.; et al. The 5th Edition of the World Health Organization Classification of Haematolymphoid Tumours: Lymphoid Neoplasms. Leukemia 2022, 36, 1720–1748. [Google Scholar] [CrossRef]







| Authors | Country | Study Design | Work Class | Carcinogen | NHL Subtype | Odds Ration IC 95% |
|---|---|---|---|---|---|---|
| Benavente et al. (2020) [7] | Spain | Case-control | - | Pesticides | NHL; CLL | 1.61 (1.22–2.12) |
| Fisher et al. (2020) [42] | USA | Cohort | - Pesticide Applicators | - | NHL; BC-NHL; CLL; SLL; DLBCL; FL; MM | 4.05 (3.11–5.27) |
| Linet et al. (2020) [48] | China | Cohort | Benzene | NHL | 2.27 (1.00–5.13) | |
| Satta et al. (2020) [49] | Czech Republic, France, Germany, Ireland, Italy and Spain | Case-control | - | Internal and External Ionizing Radiation | BC-NHL; CLL; DLBCL; FL; MM | 0.87 (0.73–1.05) |
| Loomis et al. (2019) [50] | Denmark, Finland, Italy, Norway, Sweden, and the United Kingdom | Cohort | - Workers in the reinforced plastic industry - Laminators | Styrene | NHL; MM | 0.61 (0.27–1.38) |
| Jordan et al. (2018) [51] | USA | Cohort | - Search/Rescue Workers | - | NHL | 0.44 (0.22–0.86) |
| McBride et al. (2018) [52] | New Zealand | Cohort | - | 2,3,7,8-tetraclorodibenzo-p-dioxin (TCDD) | NHL; MM | 0.51 (0.14–1.91) |
| Tsai et al. (2018) [53] | Taiwan | Cohort | - Farmers | - | NHL | 1.16 (1.0–1.33) |
| Boccolini et al. (2017) [54] | Brazil | Case-control | - Farm Workers | - | NHL | 0.88 (0.75–1.02) |
| Ferri et al. (2017) [55] | Italy | Case-control | - Homemaker - Blue-collar worker - Teachers - Craftsman/Merchant - Farmer - Clerk - Military - Technician - Food handlers - Agricultural occupation | Pesticides and radon | NHL; DLBCL; FL; CLL; Single B-cell Lymphoma; MM | 2.31 (0.73–7.32) |
| Lemarchand et al. (2017) [56] | France | Cohort | - Farm Workers | NHL; CLL/SLL; FL; DLBCL; MCL; MZL; Waldentröm Lymphoplasmacytic Lymphoma; NK/T-CL; MF; NHL-NOS | 1.23 (0.99–1.54) | |
| González et al. (2016) [57] | USA | Cohort | - Radiologist | NHL; CLL; MM | 0.95 (0.77–1.17) | |
| Bassig et al. (2015) [58] | China | Cohort | - Factory Employees Exposed to Benzene | Benzene | NHL | 1.78 (1.13–2.81) |
| Cocco et al. (2013) [8] | USA, Czech Republic, France, Germany, Italy, Ireland, Spain and Canada | Case-control | - | Trichloroethylene | NHL; DLBCL; FL; CLL | 1.01 (0.86–1.17) |
| Kachuri et al. (2013) [59] | Canada | Case-control | - Farm workers | Pesticides and formaldehyde | MM | 1.09 (0.84–1.41) |
| Karunanayake et al. (2013) [60] | Canada | Case-control | - Workers exposed to Pesticides | - | NHL | 1.79 (1.0–3.18) |
| Li et al. (2012) [61] | USA | Cohort | - Search/Rescue Workers | NHL; MM | 1.26 (0.81–1.98) | |
| Zakerinia et al. (2012) [11] | Iran | Case-control | - Workers exposed to Pesticides | - | NHL; MM | 5.48 (3.47–8.65) |
| Lipworth et al. (2011) [62] | USA | Cohort | - Employees of aircraft manufacturing - Aircraft painter - Process or electroplating operator - Plastic parts manufacturer - Welder - Metal bonding worker - Fabrication and structural development mechanic - Final Assembler | Chromate and solvents | NHL; MM; CLL | 1.20 (1.02–1.40) |
| Purdue et al. (2011) [63] | USA | Case-control | - | Trichloroethylene | NHL; DLBCL; FL; SLL; CLL | 1.20 (1.01–1.42) |
| Bonner et al. (2010) [32] | USA | Cohort | - | Terbufos | NHL | 1.39 (0.97–1.97) |
| Cocco et al. (2010) [9] | Czech Republic, France, Germany, Ireland, Italy, and Spain | Case-control | - | Solvents | DLBCL; FL; CLL; MM; BC- NHL | 1.09 (0.97–1.23) |
| Kiran et al. (2010) [64] | Czech Republic, France, Germany, Italy, Ireland, and Spain | Case-control | - | Ethylene | DLBCL; CLL | 1.21 (0.72–2.03) |
| Seidler et al. (2010) [65] | Germany, and Italy | Case-control | - | Asbestos | BC-NHL; DLBCL; FL; CLL; MM | 1.11 (0.83–1.47) |
| Wong et al. (2010) [66] | China e USA | Case-control | - Farmer - Livestock or Animal Husbandry | - | NHL; CLL; FL; DLBCL; T/NK Cell Neoplasms | 1.37 (1.11–1.69) |
| Lynch et al. (2009) [37] | USA | Cohort | - | Butylate | NHL | 1.81 (1.0–3.30) |
| McBride et al. (2009) [67] | New Zealand | Cohort | - | 2,3,7,8-Tetrachlorodibenzo-p-dioxin | NHL; MM | 2.05 (0.24–17.64) |
| Park et al. (2009) [39] | USA | Cohort | - | Paraquat | NHL | 1.15 (0.80–1.66) |
| Rusiecki et al. (2009) [41] | USA | Cohort | - Farmers | - | NHL; MM | 0.08 (0.06–0.12) |
| Wang et al. (2009) [68] | USA | Case-control | - | Solvent | NHL; DLBCL; FL; CLL | 1.61 (1.29–2.01) |
| Kirkeleit et al. (2008) [69] | Norway | Cohort | - Oil industry workers | - | NHL; CLL; MM | 0.67 (0.48–0.93) |
| Tranah et al. (2008) [70] | USA | Case-control | - Animal Husbandry - Farm Laborer | - | NHL; DLBCL or Immunoblastic Large Cell Lymphoma; FL; SLL | 0.93 (0.81–1.07) |
| Bonner et al. (2007) [33] | USA | Cohort | - | Malathion | NHL | 10.10 (5.18–19.68) |
| Mahajan et al. (2007) [38] | USA | Cohort | - | Carbaryl | NHL | 14.67 (8.19–26.25) |
| Moore et al. (2007) [71] | Czech Republic, France, Germany, Ireland, Italy, and Spain | Case-control | - Meat handlers | - | NHL; MM; CLL; SLL; DLBCL; FL | 1.23 (1.00–1.51) |
| Purdue et al. (2007) [40] | USA | Cohort | - | Pesticides | NHL | 2.55 (1.39–4.70) |
| Xu et al. (2007) [72] | Japan, Korea and China | Case-control | - Farmers - Chemical Plant Workers - Self-Employed | Pesticides | Nasal T/NK-cell Lymphoma | 0.81 (0.49–1.34) |
| Miligi et al. (2006) [73] | Italy | Case-control | - | Solvents and hydrocarbons | NHL; SLL; FL; DLBCL | 1.11 (0.92–1.33) |
| Balen et al. (2006) [12] | Spain | Case-control | - Farmer - Animal Husbandry | - | NHL; B-Cell NHL; TC-NHL; MM | 1.34 (1.08–1.66) |
| Fritschi et al. (2005) [74] | Australia | Case-control | - | Pesticides | NHL; BC- NHL; DLBCL; FL | 1.00 (0.71–1.41) |
| Kato et al. (2005) [75] | USA | Case-control | - | Solvents | NHL | 1.18 (0.85–1.63) |
| Chiu et al. (2004) [76] | USA | Case-control | - | Pesticides | NHL; DCL; SLL; FL | 1.11 (0.94–1.32) |
| Kato et al. (2004) [77] | USA | Case-control | - Farm Workers - Pesticide Applicators | Pesticides and naphthalene | NHL | 1.40 (1.01–1.94) |
| De Roos et al. (2003) [78] | USA | Case-control | - | Pesticides | NHL | 1.39 (1.16–1.67) |
| Fritschi et al. (2002) [79] | Canada | Case-control | - Workers in contact with animals - Farm Workers - Fishermen | - | NHL; MM | 0.92 (0.79–1.08) |
| Lee et al. (2002) [80] | USA | Cohort | - Farmers - Cattle Ranchers | - | NHL; MM; CLL | 0.99 (0.65–1.51) |
| McDuffie et al. (2001) [81] | Canada | Case-control | - | Pesticides | NHL | 2.56 (2.09–3.14) |
| VanWijngaarden and Savitz (2001) [82] | USA | Case-control | - Electric Utility Workers - Electric Utility Workers Exposed to Solvents | - | NHL; Low and high-grade NHL | 1.24 (0.85–1.81) |
| Zheng et al. (2001) [83] | USA | Case-control | - | Pesticides | NHL; FL; Diffuse NHL; SLL | 0.42 (0.34–0.51) |
| McGeoghegan and Binks (2000) [84] | England | Cohort | - Uranium Production and Manufacturing Workers | Radiation | NHL; MM | 1.14 (0.53–2.43) |
| Thörn et al. (2000) [85] | Sweden | Cohort | - Lumberjack | - | NHL | 0.95 (0.13–6.77) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Francisco, L.F.V.; da Silva, R.N.; Oliveira, M.A.; dos Santos Neto, M.F.; Gonçalves, I.Z.; Marques, M.M.C.; Silveira, H.C.S. Occupational Exposures and Risks of Non-Hodgkin Lymphoma: A Meta-Analysis. Cancers 2023, 15, 2600. https://doi.org/10.3390/cancers15092600
Francisco LFV, da Silva RN, Oliveira MA, dos Santos Neto MF, Gonçalves IZ, Marques MMC, Silveira HCS. Occupational Exposures and Risks of Non-Hodgkin Lymphoma: A Meta-Analysis. Cancers. 2023; 15(9):2600. https://doi.org/10.3390/cancers15092600
Chicago/Turabian StyleFrancisco, Luiza Flavia Veiga, Rogério Nunes da Silva, Marco Antônio Oliveira, Martins Fideles dos Santos Neto, Iara Zapparoli Gonçalves, Márcia M. C. Marques, and Henrique C. S. Silveira. 2023. "Occupational Exposures and Risks of Non-Hodgkin Lymphoma: A Meta-Analysis" Cancers 15, no. 9: 2600. https://doi.org/10.3390/cancers15092600
APA StyleFrancisco, L. F. V., da Silva, R. N., Oliveira, M. A., dos Santos Neto, M. F., Gonçalves, I. Z., Marques, M. M. C., & Silveira, H. C. S. (2023). Occupational Exposures and Risks of Non-Hodgkin Lymphoma: A Meta-Analysis. Cancers, 15(9), 2600. https://doi.org/10.3390/cancers15092600