Association of GSTTI, M1 and Polymorphism in GSTPI with Chronic Periodontal Disease in a Pakistani Population
Abstract
:1. Introduction
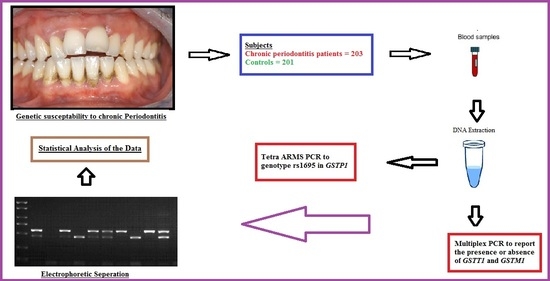
2. Materials and Methods
2.1. Ethical Approval
2.2. Patients and Sample Collection
2.3. DNA Extraction
2.4. Amplification and Genotyping of GSTT1 and GSTM1
2.5. Tetra-Primer ARMS–PCR-Based Amplification of rs1695 in GSTP1
2.6. Statistical Analysis
3. Results
3.1. Presence or Absence of GSTM1 and GSTT1 and Their Association with Chronic Periodontitis
3.2. Genotypic and Allelic Frequency of rs1695 in GSTP1 and Their Association with Chronic Periodontitis
3.3. GSTs Interactions and Their Association with Chronic Periodontitis
3.4. Association of Demographic Factors with the Incidence of Chronic Periodontal Disease
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Petersen, P.E.; Baehni, P.C. Periodontal health and global public health. Periodontology 2012, 60, 7–14. [Google Scholar] [CrossRef]
- Armitage, G.C.; Cullinan, M.P.; Seymour, G.J. Comparative biology of chronic and aggressive periodontitis: Introduction. Periodontology 2010, 53, 7–11. [Google Scholar] [CrossRef]
- Otomo-Corgel, J.; Pucher, J.J.; Rethman, M.P.; Reynolds, M.A. State of the Science: Chronic Periodontitis and Systemic Health. J. Evid. Based Dent. Pract. 2012, 12, 20–28. [Google Scholar] [CrossRef]
- Garlet, G.P. Destructive and protective roles of cytokines in periodontitis: A re-appraisal from host defense and tissue destruction viewpoints. J. Dent. Res. 2010, 89, 1349–1363. [Google Scholar] [CrossRef] [PubMed]
- Graetz, C.; Mann, L.; Krois, J.; Sälzer, S.; Kahl, M.; Springer, C.; Schwendicke, F. Comparison of periodontitis patients’ classification in the 2018 versus 1999 classification. J. Clin. Periodontol. 2019, 46, 908–917. [Google Scholar] [CrossRef] [PubMed]
- Kornman, K.S.; Papapanou, P.N. Clinical application of the new classification of periodontal diseases: Ground rules, clarifications and “gray zones”. J. Periodontol. 2020, 91, 352–360. [Google Scholar] [CrossRef]
- Fahim, A.; Shakeel, S.; Shahid, T.; Anwar, H.; Raja, A.; Khan, A. Prevalence of Periodontitis in Pakistan: A Systematic Review. J. Univ. Coll. Med. Dent. 2021, 1, 30–34. [Google Scholar]
- Leite, F.R.; Nascimento, G.G.; Scheutz, F.; Lopez, R. Effect of smoking on periodontitis: A systematic review and meta-regression. Am. J. Prev. Med. 2018, 54, 831–841. [Google Scholar] [CrossRef] [PubMed]
- Shehzad, S.; Waheed, Z.; Khan, K.; Shah, M.; Durrani, S.H.; Farooq, A. Comparison of Periodontal Diseases among Genders in Khyber Pakhtunkhwa, Pakistan. Int. J. Sci. Innov. Res. 2021, 2, 0100037IJESIR. [Google Scholar]
- Cardoso, E.M.; Reis, C.; Manzanares-Céspedes, M.C. Chronic periodontitis, inflammatory cytokines, and interrelationship with other chronic diseases. Postgrad. Med. 2018, 130, 98–104. [Google Scholar]
- Chapple, I.L.C.; Brock, G.; Eftimiadi, C.; Matthews, J.B. Glutathione in gingival crevicular fluid and its relationship to local antioxidant capacity in periodontal health and disease. Mol. Pathol. 2002, 55, 367–373. [Google Scholar] [CrossRef]
- Borges, I., Jr.; Moreira, E.A.M.; Filho, D.W.; de Oliveira, T.B.; da Silva, M.B.S.; Fröde, T.S.F. Proinflammatory and Oxidative Stress Markers in Patients with Periodontal Disease. Clin. Study 2007, 2007, 045794. [Google Scholar] [CrossRef] [PubMed]
- Varghese, J.; Bhat, V.; Bhat, G.; Rao, N. Evaluation of Glutathione-S-transferase and ceruloplasmin levels in gingival crevicular fluid and gingival tissue as diagnostic markers for chronic periodontitis. Adv. Biosci. Biotechnol. 2012, 3, 437–441. [Google Scholar] [CrossRef] [Green Version]
- Nishinaka, T.; Ichijo, Y.; Ito, M.; Kimura, M.; Katsuyama, M.; Iwata, K.; Miura, T.; Terada, T.; Yabe-Nishimura, C. Curcumin activates human glutathione S-transferase P1 expression through antioxidant response element. Toxicol. Letters 2007, 170, 238–247. [Google Scholar] [CrossRef]
- Sanchez, F.M.; Diaz, A.C.; Sánchez, Q.H.; Navarro, J.B.; Cadena, J.C. Polymorphisms of GSTM1, GSTT1 and GSTP1 and their possible association with the development of dental caries. Pilot study. Int. J. Manag. Inf. Technol. Eng. 2019, 7, 15–24. [Google Scholar]
- Concolino, P.; Cecchetti, F.; D’ Autilia, C.; Santonocito, C.; Di Stasio, E.; Zuppi, C.; Arcuri, C.; Deli, G.; Giardina, B.; Capoluongo, E.; et al. Association of periodontitis with GSTM1/GSTT1-null variants-a pilot study. Clin. Biochem. 2007, 40, 939–945. [Google Scholar] [CrossRef]
- Ortega, V.R.C.; López, L.D.B.; Salgado, A.V.; Sanchez, F.M.; Cadena, J.C. Polymorphisms in Glutathione S-Transferase M1, T1, and P1 in Patients with Chronic Periodontitis: A Pilot Study. Int. Sch. Res. Not. 2014, 2014, 135368. [Google Scholar] [CrossRef]
- Küchler, E.C.; Mazzi-Chaves, J.F.; Antunes, L.S.; Kirschneck, C.; Baratto-Filho, F.; Sousa-Neto, M.D. Current trends of genetics in apical periodontitis research. Braz. Oral Res. 2018, 32, e72. [Google Scholar] [CrossRef]
- Jones, S.R.; Carley, S.; Harrison, M. An introduction to power and sample size estimation. Emerg. Med. J. 2003, 20, 453–458. [Google Scholar] [CrossRef] [PubMed]
- Jamil, H.; Awan, A.; Akbar, A.; Babar, M.; Akhtar, S.; Iqbal, R.K.; Iqbal, F. A study of association between presence or absence of GSTT1 and GSTM1 and/or single nucleotide polymorphism in FABP2 and GSTP1 with incidence of diabetes type 2: A case-control study. J. Pak. Med. Assoc. 2022, 72, 714–719. [Google Scholar] [CrossRef] [PubMed]
- Panjamurthy, K.; Manoharan, S.; Ramachandran, C.R. Lipid peroxidation and antioxidants status in patients with periodontitis. Cell Mol. Biol. Lett. 2005, 10, 255–264. [Google Scholar] [PubMed]
- Hrishi, T.S.; Kundapur, P.P.; Naha, A.; Thomas, B.S.; Kamath, S.; Bhat, G.S. Effect of adjunctive use of green tea dentifrice in periodontitis patients—A Randomized Controlled Pilot Study. Int. J. Dent. Hyg. 2016, 14, 178–183. [Google Scholar] [CrossRef] [PubMed]
- Hernández-Ríos, P.; Pussinen, P.J.; Vernal, R.; Hernández, M. Oxidative Stress in the Local and Systemic Events of Apical Periodontitis. Front. Physiol. 2017, 8, 869. [Google Scholar] [CrossRef]
- Kim, J.S.; Park, J.Y.; Chung, W.Y.; Choi, M.A.; Cho, K.S.; Park, K.K. Polymorphisms in genes coding for enzymes metabolizing smoking-derived substances and the risk of periodontitis. J. Clin. Periodontol. 2004, 31, 959–964. [Google Scholar] [CrossRef]
- Jakovljevic, A.; Nikolic, N.; Carkic, J.; Beljic-Ivanovic, K.; Soldatovic, I.; Miletic, M.; Andric, M.; Milasin, J. Association of polymorphisms in TNF-α, IL-1β, GSTM and GSTT genes with apical periodontitis: Is there a link with herpesviral infection? Int. Endod. J. 2020, 53, 895–904. [Google Scholar] [CrossRef]
- Nikita, A.; Andrew, B.; May, T. Hardy-Weinberg Equilibrium in the Large Scale Genomic Sequencing Era. Front. Genet. 2020, 11, 210. [Google Scholar] [CrossRef]
- Graffelman, J.; Jain, D.; Weir, B. A genome-wide study of Hardy–Weinberg equilibrium with next generation sequence data. Hum. Genet. 2017, 136, 727–741. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization. “Oral Health”, Fact Sheet no. 318. 2012. Available online: http://www.who.int/mediacentre/factsheets/fs318/en/# (accessed on 7 January 2023).
- Rajasekar, A.; Mathew, M.G. Prevalence of Periodontal Disease among Individuals between 18–30 Years of Age: A Retrospective Study. Ann. Med. Health Sci. Res. 2021, 11, 198–204. [Google Scholar]
- Balaji, S.; Lavu, V.; Rao, S. Chronic periodontitis prevalence and the inflammatory burden in a sample population from South India. Indian J. Dent. Res. 2018, 29, 254. [Google Scholar]
| Genotype | Controls | Case | Chi-Square Value | p-Value |
|---|---|---|---|---|
| GSTM1 Present | 185 | 66 | 152.1 | <0.001 *** |
| GSTM1 Null | 16 | 137 | ||
| GSTT1 Present | 34 | 83 | ||
| GSTT1 Null | 167 | 120 | 28.2 | <0.001 *** |
| Parameters | Genotypic Frequency | p-Value | Allelic Frequency | p-Value | |||||
|---|---|---|---|---|---|---|---|---|---|
| Nucleotide | AA | AG | GG | Chi-Square Value | p ˂ 0.0001 *** | A | G | Chi-Square Value | p ˂ 0.0001 *** |
| Controls | 177 (88%) | 20 (10%) | 4 (2%) | 51.348 | 374 (93%) | 28 (7%) | 65.507 | ||
| Case | 115 (57%) | 59 (29%) | 29 (14%) | 289 (71%) | 117 (29%) | ||||
| Genotype | Control 202 | Case 203 | Chi-Square | p-Value |
|---|---|---|---|---|
| GSTM1 and GSTT1 | ||||
| Both present | 34 | 17 | 48.346 | p < 0.0001 *** |
| Either Null | 154 | 116 | ||
| Both Null | 14 | 70 | ||
| GSTM1 and GSTP1(rs1695) | ||||
| M1(+/+) and P1(AA) | 164 | 42 | 172.428 | p < 0.0001 *** |
| M1(+/+) and P1(AG) | 19 | 16 | ||
| M1(+/+) and P1(GG) | 3 | 8 | ||
| M1(−/−) and P1(AA) | 13 | 73 | ||
| M1(−/−) and P1(AG) | 1 | 43 | ||
| M1(−/−) and P1(GG) | 2 | 21 | ||
| GSTT1 and GSTP1(rs1695) | ||||
| T1(+/+) and P1(AA) | 27 | 47 | 79.023 | p < 0.0001 *** |
| T1(+/+) and P1(AG) | 6 | 27 | ||
| T1(+/+) and P1(GG) | 1 | 8 | ||
| T1(−/−) and P1(AA) | 152 | 68 | ||
| T1(−/−) and P1(AG) | 14 | 32 | ||
| T1(−/−) and P1(GG) | 2 | 21 | ||
| GSTT1, GSTM1 and GSTP1 (rs1695) | ||||
| T1 and M1(+/+) and P1 (AA) | 27 | 12 | 173.564 | p < 0.0001 *** |
| T1 and M1(+/+) and P1 (AG) | 6 | 4 | ||
| T1 and M1(+/+) and P1 (GG) | 1 | 1 | ||
| T1(+/+), M1(−/−) and P1 (AA) | 1 | 35 | ||
| T1(+/+), M1(−/−) and P1 (AG) | 1 | 23 | ||
| T1(+/+), M1(−/−) and P1 (GG) | 1 | 9 | ||
| T1(−/−),M1(+/+) and P1 (AA) | 135 | 30 | ||
| T1(−/−), M1(+/+) and P1 (AG) | 13 | 12 | ||
| T1(−/−), M1(+/+) and P1 (GG) | 2 | 7 | ||
| T1(−/−), M1(−/−) and P1 (AA) | 13 | 38 | ||
| T1(−/−), M1(−/−) and P1 (AG) | 1 | 20 | ||
| T1(−/−), M1(−/−) and P1 (GG) | 1 | 12 | ||
| Parameters | Category | Chronic Periodontitis Cases (N = 203) | Healthy Control (N = 201) | Chi-Square Value | p-Value |
|---|---|---|---|---|---|
| Age (Years) | 10–30 | 94 | 02 | 123.692 | p ˂ 0.001 *** |
| 31–51 | 78 | 110 | |||
| 52–72 | 29 | 88 | |||
| Above 72 | 02 | 01 | |||
| Gender | Male | 105 | 105 | 0.011 | 0.9 |
| Female | 98 | 96 | |||
| Smoking | Yes | 29 | 24 | 0.487 | 0.5 |
| No | 174 | 177 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Arshad, K.; Ishfaq, U.; Asif, M.; Akbar, A.; Pitafi, K.F.; Mulghani, M.R.; Shaheen, U.; Saeed, S.; Arif, M.; Bashir, A.; et al. Association of GSTTI, M1 and Polymorphism in GSTPI with Chronic Periodontal Disease in a Pakistani Population. Genes 2023, 14, 455. https://doi.org/10.3390/genes14020455
Arshad K, Ishfaq U, Asif M, Akbar A, Pitafi KF, Mulghani MR, Shaheen U, Saeed S, Arif M, Bashir A, et al. Association of GSTTI, M1 and Polymorphism in GSTPI with Chronic Periodontal Disease in a Pakistani Population. Genes. 2023; 14(2):455. https://doi.org/10.3390/genes14020455
Chicago/Turabian StyleArshad, Kainat, Uzma Ishfaq, Muhammad Asif, Atif Akbar, Kehkashan Fatima Pitafi, Muhammad Rehan Mulghani, Uzman Shaheen, Suleman Saeed, Muhammad Arif, Ahsan Bashir, and et al. 2023. "Association of GSTTI, M1 and Polymorphism in GSTPI with Chronic Periodontal Disease in a Pakistani Population" Genes 14, no. 2: 455. https://doi.org/10.3390/genes14020455
APA StyleArshad, K., Ishfaq, U., Asif, M., Akbar, A., Pitafi, K. F., Mulghani, M. R., Shaheen, U., Saeed, S., Arif, M., Bashir, A., Farooq, M., Brook, A. H., & Iqbal, F. (2023). Association of GSTTI, M1 and Polymorphism in GSTPI with Chronic Periodontal Disease in a Pakistani Population. Genes, 14(2), 455. https://doi.org/10.3390/genes14020455