Prevalence of Myocardial Injury and Myocardial Infarction in Patients with a Hypertensive Emergency: A Systematic Review
Abstract
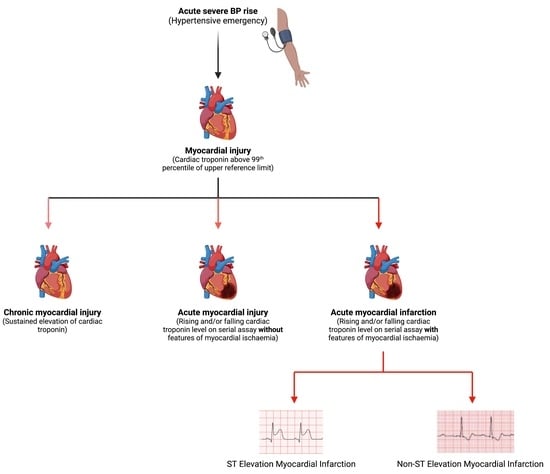
:1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Criteria for Eligibility
2.3. Study Selection and Data Extraction
2.4. Assessment of Risk of Bias
2.5. Data Synthesis and Analysis
3. Results
3.1. Search Results
3.2. Study Characteristics
3.3. Risk of Bias
3.4. Prevalence of Myocardial Infarction
3.5. Prevalence of Myocardial Injury
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mills, K.T.; Bundy, J.D.; Kelly, T.N.; Reed, J.E.; Kearney, P.M.; Reynolds, K.; Chen, J.; He, J. Global Disparities of Hypertension Prevalence and Control: A Systematic Analysis of Population-Based Studies From 90 Countries. Circulation 2016, 134, 441–450. [Google Scholar] [CrossRef] [PubMed]
- Arima, H.; Barzi, F.; Chalmers, J. Mortality patterns in hypertension. J. Hypertens. 2011, 29, S3–S7. Available online: https://pubmed.ncbi.nlm.nih.gov/22157565/ (accessed on 21 December 2022). [CrossRef] [PubMed]
- Janke, A.T.; McNaughton, C.D.; Brody, A.M.; Welch, R.D.; Levy, P.D. Trends in the Incidence of Hypertensive Emergencies in US Emergency Departments From 2006 to 2013. J. Am. Heart Assoc. 2016, 5, e004511. [Google Scholar] [CrossRef] [PubMed]
- Lip, G.Y.H.; Beevers, M.; Beevers, G. The failure of malignant hypertension to decline—A survey of 24 years experience in a mul-tiracial population in England. J. Hypertens. 1994, 12, 1297–1305. Available online: http://search.ebscohost.com/login.aspx?direct=true&db=cmedm&AN=7868878&site=ehost-live&scope=site (accessed on 23 May 2022).
- Polgreen, L.A.; Suneja, M.; Tang, F.; Carter, B.L.; Polgreen, P.M. Increasing Trend in Admissions for Malignant Hypertension and Hypertensive Encephalopathy in the United States. Hypertension 2015, 65, 1002–1007. [Google Scholar] [CrossRef] [Green Version]
- Deshmukh, A.; Kumar, G.; Kumar, N.; Nanchal, R.; Gobal, F.; Sakhuja, A.; Mehta, J.L. Effect of Joint National Committee VII Report on Hospitalizations for Hypertensive Emergencies in the United States. Am. J. Cardiol. 2011, 108, 1277–1282. [Google Scholar] [CrossRef]
- Astarita, A.; Covella, M.; Vallelonga, F.; Cesareo, M.; Totaro, S.; Ventre, L.; Apra’, F.; Veglio, F.; Milan, A. Hypertensive emergencies and urgencies in emergency departments: A systematic review and meta-analysis. J. Hypertens. 2021, 39, e271. [Google Scholar] [CrossRef]
- González, R.; Morales, E.; Segura, J.; Ruilope, L.M.; Praga, M. Long-term renal survival in malignant hypertension. Nephrol. Dial. Transplant. 2010, 25, 3266–3272. [Google Scholar] [CrossRef] [Green Version]
- Guiga, H.; Decroux, C.; Michelet, P.; Loundou, A.; Cornand, D.; Silhol, F.; Vaisse, B.; Sarlon-Bartoli, G. Hospital and out-of-hospital mortality in 670 hypertensive emergencies and urgencies. J. Clin. Hypertens. 2017, 19, 1137–1142. [Google Scholar] [CrossRef]
- Pinna, G.; Pascale, C.; Fornengo, P.; Arras, S.; Piras, C.; Panzarasa, P.; Carmosino, G.; Franza, O.; Semeraro, V.; Lenti, S.; et al. Hospital Admissions for Hypertensive Crisis in the Emergency Departments: A Large Multicenter Italian Study. PLoS ONE 2014, 9, e93542. [Google Scholar] [CrossRef] [Green Version]
- Shah, M.; Patil, S.; Patel, B.; Arora, S.; Patel, N.; Garg, L.; Agrawal, S.; Jacobs, L.; Steigerwalt, S.P.; Martinez, M.W. Trends in Hospitalization for Hypertensive Emergency, and Relationship of End-Organ Damage With In-Hospital Mortality. Am. J. Hypertens. 2017, 30, 700–706. [Google Scholar] [CrossRef] [PubMed]
- Furman, M.I.; Dauerman, H.L.; Goldberg, R.J.; Yarzbeski, J.; Lessard, D.; Gore, J.M. Twenty-two year (1975 to 1997) trends in the incidence, in-hospital and long-term case fatality rates from initial q-wave and non-q-wave myocardial infarction: A multi-hospital, community-wide perspective. J. Am. Coll. Cardiol. 2001, 37, 1571–1580. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thygesen, K.; Alpert, J.S.; Jaffe, A.S.; Chaitman, B.R.; Bax, J.J.; Morrow, D.A.; White, H.D.; Executive Group on behalf of the Joint European Society of Cardiology (ESC)/American College of Cardiology (ACC)/American Heart Association (AHA)/World Heart Federation (WHF) Task Force for the Universal Definition of Myocardial Infarction. Fourth Universal Definition of Myocardial Infarction (2018). J. Am. Coll. Cardiol. 2018, 72, 2231–2264. [Google Scholar] [CrossRef] [PubMed]
- Sarkisian, L.; Saaby, L.; Poulsen, T.S.; Gerke, O.; Hosbond, S.; Jangaard, N.; Diederichsen, A.C.P.; Thygesen, K.; Mickley, H. Prognostic Impact of Myocardial Injury Related to Various Cardiac and Noncardiac Conditions. Am. J. Med. 2016, 129, 506–514.e1. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chapman, A.R.; Shah, A.; Lee, K.K.; Anand, A.; Francis, O.; Adamson, P.; McAllister, D.A.; Strachan, F.E.; Newby, D.E.; Mills, N. Long-Term Outcomes in Patients With Type 2 Myocardial Infarction and Myocardial Injury. Circulation 2018, 137, 1236–1245. [Google Scholar] [CrossRef] [PubMed]
- Pattanshetty, D.J.; Bhat, P.K.; Aneja, A.; Pillai, D.P. Elevated troponin predicts long-term adverse cardiovascular outcomes in hy-pertensive crisis: A retrospective study. J. Hypertens. 2012, 30, 2410–2415. [Google Scholar] [CrossRef]
- Kim, W.; Kim, B.S.; Kim, H.-J.; Lee, J.H.; Shin, J.; Shin, J.-H. Clinical implications of cardiac troponin-I in patients with hypertensive crisis visiting the emergency department. Ann. Med. 2022, 54, 507–515. [Google Scholar] [CrossRef]
- Page, M.J.; Moher, D.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. PRISMA 2020 explanation and elaboration: Updated guidance and exemplars for reporting systematic reviews. BMJ 2021, 372, n160. [Google Scholar] [CrossRef]
- Hoy, D.; Brooks, P.; Woolf, A.; Blyth, F.; March, L.; Bain, C.; Baker, P.; Smith, E.; Buchbinder, R. Assessing risk of bias in prevalence studies: Modification of an existing tool and evidence of interrater agreement. J. Clin. Epidemiol. 2012, 65, 934–939. [Google Scholar] [CrossRef]
- Salvetti, M.; Paini, A.; Colonetti, E.; Tarozzi, L.; Bertacchini, F.; Aggiusti, C.; Stassaldi, D.; Rosei, C.A.; Rosei, E.A.; Muiesan, M.L. Hypertensive emergencies and urgencies: A sin-gle-centre experience in Northern Italy 2008–2015. J. Hypertens. 2020, 38, 52–58. [Google Scholar] [CrossRef]
- Acosta, G.; Amro, A.; Aguilar, R.; Abusnina, W.; Bhardwaj, N.; Koromia, G.A.; Studeny, M.; Irfan, A. Clinical Determinants of Myocardial Injury, Detectable and Serial Troponin Levels among Patients with Hypertensive Crisis. Cureus 2020, 12, e6787. [Google Scholar] [CrossRef] [PubMed]
- Abdallah, T.M.; Ibrahem, A.A.; Ali, E.A.; Ahmed, E.G.; Ali, A.A. Clinico-epidemiological characteristics and survival outcome of patients with hypertensive crisis at Kassala Hospital, Eastern Sudan. J. Clin. Intensiv. Care Med. 2018, 3, 029–034. [Google Scholar] [CrossRef] [Green Version]
- Zampaglione, B.; Pascale, C.; Marchisio, M.; Cavallo-Perin, P. Hypertensive Urgencies and Emergencies. Prevalence and clinical presentation. Hypertension 1996, 27, 144–147. [Google Scholar] [CrossRef]
- Kotruchin, P.; Pratoomrat, W.; Mitsungnern, T.; Khamsai, S.; Imoun, S. Clinical treatment outcomes of hypertensive emergency patients: Results from the hypertension registry program in Northeastern Thailand. J. Clin. Hypertens. 2020, 23, 621–627. [Google Scholar] [CrossRef]
- Katz, J.N.; Gore, J.M.; Amin, A.; Anderson, F.A.; Dasta, J.F.; Ferguson, J.J.; Kleinschmidt, K.; Mayer, S.A.; Multz, A.S.; Peacock, W.F.; et al. Practice patterns, outcomes, and end-organ dysfunction for patients with acute severe hypertension: The Studying the Treatment of Acute hyperTension (STAT) Registry. Am. Heart J. 2009, 158, 599–606.e1. [Google Scholar] [CrossRef]
- Benenson, I.; Waldron, F.A.; Dillon, S.A.J.; Zinzuwadia, S.N.; Mbadugha, N.; Vicente, N.; Aris, E.; Adeboye, A.M.; Makdisi, C. Hypertensive emergencies in diabetic patients from predominantly African American urban communities. Clin. Exp. Hypertens. 2018, 41, 531–537. [Google Scholar] [CrossRef] [PubMed]
- Fragoulis, C.; Dimitriadis, K.; Siafi, E.; Iliakis, P.; Kasiakogias, A.; Kalos, T.; Leontsinis, I.; Andrikou, I.; Konstantinidis, D.; Nihoyannopoulos, P.; et al. Profile and management of hypertensive urgencies and emergencies in the emergency cardiology department of a tertiary hospital: A 12-month registry. Eur. J. Prev. Cardiol. 2021, 29, 194–201. [Google Scholar] [CrossRef]
- Nkoke, C.; Jingi, A.M.; Noubiap, J.J.; Teuwafeu, D.; Nkouonlack, C.; Gobina, R.; Djibrilla, S.; Abas, A.; Dzudie, A. Gender Differences in Cardiovascular Risk Factors, Clinical Presentation, and Outcome of Patients Admitted with a Hypertensive Crisis at the Buea Regional Hospital, Cameroon. Int. J. Hypertens. 2022, 2022, 3062526. [Google Scholar] [CrossRef]
- Martin, J.F.V.; Higashiama, É.; Garcia, E.; Luizon, M.R.; Cipullo, J.P. Perfil de crise hipertensiva: Prevalência e apresentação clínica. Arq. Bras. Cardiol. 2004, 83, 125–130. [Google Scholar] [CrossRef] [Green Version]
- Vilela-Martin, J.F.; Vaz-De-Melo, R.O.; Kuniyoshi, C.H.; Abdo, A.N.R.; Yugar-Toledo, J.C. Hypertensive crisis: Clinical–epidemiological profile. Hypertens. Res. 2010, 34, 367–371. [Google Scholar] [CrossRef]
- Pacheco, H.G.; Victorino, N.M.; Urquiza, J.P.N.; Castillo, A.A.; Herrera, U.J.; Mendoza, A.A.; Manzur, F.A.; de la Cruz, J.L.B.; Sánchez, C.M. Patients With Hypertensive Crises Who Are Admitted to a Coronary Care Unit: Clinical Characteristics and Outcomes. J. Clin. Hypertens. 2013, 15, 210–214. [Google Scholar] [CrossRef] [PubMed]
- Rubin, S.; Cremer, A.; Boulestreau, R.; Rigothier, C.; Kuntz, S.; Gosse, P. Malignant hypertension: Diagnosis, treatment and prog-nosis with experience from the Bordeaux cohort. J. Hypertens. 2019, 37, 316–324. [Google Scholar] [CrossRef] [PubMed]
- Van den Born, B.-J.H.; Lip, G.Y.H.; Brguljan-Hitij, J.; Cremer, A.; Segura, J.; Morales, E.; Mahfoud, F.; Amraoui, F.; Persu, A.; Kahan, T.; et al. ESC Council on hypertension position document on the management of hypertensive emergencies. Eur. Heart J. Cardiovasc. Pharmacother. 2018, 5, 37–46. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Williams, B.; Mancia, G.; Spiering, W.; Agabiti Rosei, E.; Azizi, M.; Burnier, M.; Clement, D.L.; Coca, A.; de Simone, G.; Dominiczak, A.; et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology (ESC) and the European Society of Hypertension (ESH). Eur. Heart J. 2018, 39, 3021–3104. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Unger, T.; Borghi, C.; Charchar, F.; Khan, N.A.; Poulter, N.R.; Prabhakaran, D.; Ramirez, A.; Schlaich, M.; Stergiou, G.S.; Tomaszewski, M.; et al. 2020 International Society of Hypertension Global Hypertension Practice Guidelines. Hypertension 2020, 75, 1334–1357. [Google Scholar] [CrossRef] [PubMed]
- McCarthy, C.; Murphy, S.; Cohen, J.A.; Rehman, S.; Jones-O’Connor, M.; Olshan, D.; Singh, A.; Vaduganathan, M.; Januzzi, J.L.; Wasfy, J.H. Misclassification of Myocardial Injury as Myocardial Infarction. JAMA Cardiol. 2019, 4, 460–464. [Google Scholar] [CrossRef] [Green Version]
- Cremer, A.; Amraoui, F.; Lip, G.Y.; Morales, E.; Rubin, S.; Segura, J.; Van den Born, B.J.; Gosse, P. From malignant hypertension to hypertension-MOD: A modern definition for an old but still dangerous emergency. J. Hum. Hypertens. 2015, 30, 463–466. [Google Scholar] [CrossRef] [PubMed]

| Author, Year, Country | Study Design | Mean Age Years (SD) | Male (%) | Diagnosis of HC | HE (%) | Diagnosis of MI | MI (%) | Sub-Types of MI/ACS (%) | NIMI (%) | Comments | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| STEMI | NSTEMI | UA | ||||||||||
| Rubin et al. [32], 2019, France | Prospective (Registry) | 46.5 ± 12.5 | 68 | 180/110 aHMOD | NR | Excluded MI | NR | - | - | - | 63 | Cohorts comprised patients of the malignant hypertension registry from 1995 to 2017. Excluded MI. 63% had elevated cardiac troponin without signs of ongoing infarction. |
| Gonzalez Pacheco et al. [31], 2013, Mexico | Retrospective | 62.6 ± 12.7 | 57.8 | JNC VII | 76.6 | NR | 59.5 (ACS) | 25.2 | 19.2 | 15.1 | NR | Cohorts comprised high-risk patients admitted into the coronary care unit from 2005 to 2011. Reported a high prevalence of MI and acute aortic syndrome. Provided data on subtypes of ACS. |
| Guiga et al. [9], 2017, France | Prospective | 76.6 ± 18 | 46.8 | ESH/ESC 2013 | 57.5 | Symptoms ECG Troponin | 13.8 (ACS) | NR | NR | NR | NR | Assessed hospital and out-of-hospital mortality in patients with hypertensive crises admitted over 12 months from January to December 2015. Short- and long-term mortality is driven by neurovascular and cardiovascular complications. |
| Salvetti et al. [20], 2008, Italy | Prospective | 71.4 ± 14 | 53.9 | JNC VII | 20.4 | 3rd UD | 25 (ACS) | NR | NR | NR | NR | Evaluated patients admitted over 12 months in 2008. Excluded resuscitated, cardiac arrest, and those going directly for coronary angiography. |
| Salvetti et al. [20], 2015, Italy | Prospective | 72.5 ± 13 | 55.1 | JNC VII | 15.4 | 3rd UD | 25 (ACS) | NR | NR | NR | NR | Evaluated patients admitted over 12 months in 2015. Excluded resuscitated, cardiac arrest, and those going directly for coronary angiography. |
| Pinna et al. [10], 2014, Italy | Prospective | 69.9 ± 14.3 | 53.2 | 220/120 aHMOD | 25.3 | 3rd UD | 17.9 | NR | NR | NR | NR | A multicenter study involving 10 Italian centers over 12 months in 2009. Reported similar rates of cardiological symptoms in hypertensive emergencies and urgencies. |
| Kotruchin et al. [24], 2021, Thailand | Retrospective (Registry) | 65.9 ± 13.6 | 52.1 | ACC/AHA 2017 | 13.7 | 3rd UD | 6.5 (ACS) | NR | NR | NR | NR | Reviewed data of hypertension registry cohorts admitted from 2016 to 2019. Reported aHMOD involving the brain in 70% and overall in-hospital mortality of 1.6%. |
| Vilela-Martin et al. [30], 2011, Brazil | CS | 63.4 ± 13.4 | 50.6 | JNC VII | 63.8 | Symptoms ECG Troponin | 25.1 (MI and UA) | NR | NR | 12.1 | NR | Evaluated records of patients admitted over 12 months in 2000. Found an equal proportion of UA (12.1%) and MI (13%). |
| Acosta et al. [21], 2020, USA | Retrospective | NR | 47.6 | ICD 10 Codes | NR | - | - | - | - | - | 15 | Evaluated myocardial injury in patients with hypertensive crisis using serial cardiac troponin assay. Found detectable cardiac troponin levels in 2/3, and myocardial injury in 15%. Excluded patients with ACS. |
| Zampaglione et al. [23], 1994, Italy | Prospective | 67 ± 16 | 49.1 | JNC V | 24.1 | NR | 12 (MI or UA) | NR | NR | NR | NR | Enrolled patients with hypertensive crisis from June 1992 to May 1993. Women constituted 60% of their cohorts. |
| Martin et al. [29], 2004, Brazil | Retrospective | 59.6 ± 14.8 | 55.3 | JNC VI | 39.6 | ICD Code | 13 (AMI and UA) | NR | NR | 5 | NR | Evaluated the medical records of patients admitted over 12 months in 2000. The most common aHMOD was cerebrovascular lesions. Reported UA separately from MI. |
| TajEldin M et al. [22], 2018, Sudan | CS | 61.9 ± 11.8 | 54 | JNC VII | 61.7 | NR | 13.6 (ACS) | NR | NR | 4.9 | NR | Enrolled patients with hypertensive emergencies from January to October 2017. Stroke was the most common aHMOD. |
| Pattanshety et al. [16], 2012, USA | Retrospective | 57.2 ± 16 | 55 | ICD 10 | NR | NR | 30.2 (MI and UA) | NR | NR | 17.5 | NR | Assessed the prognostic impact of troponin on outcomes in patients with hypertensive emergencies. Found obstructive coronary artery disease in 76.5% of patients with elevated cardiac troponin. The incidence of major adverse cardiovascular or cerebral events was higher in patients with elevated troponin. |
| Nkoke et al. [28], 2022, Cameroon | CS | 51.2 ± 16.8 | 50 | JNC VII | 58.9 | NR | 3.6 (ACS) | NR | NR | NR | NR | Cohorts comprised 56 patients with hypertensive emergency admitted from June 2018 to June 2019. Found acute left ventricular failure with pulmonary edema in 44.6% and ACS in 3.6%. |
| Kim et al. [17], 2022, Republic of Korea | Retrospective | 64.6 ± 15.8 | 50.7 | 180/110 | 23.6 | NR | NR | NR | NR | NR | 60.4 | In total, 60.4% of cohorts with elevated cardiac troponin did not have MI. Found higher mortality in cohorts with detectable and elevated cardiac troponin levels. |
| Fragoulis et al. [27], 2021, Greece | Prospective (Registry) | 67.4 ± 12.9 | 49 | 180/120 | 27.5 | NR | 22.6 (ACS) | NR | NR | NR | NR | Cohorts from the registry data of the emergency department of the National referral center for percutaneous coronary intervention and heart failure. Pulmonary edema occurred in 58%, while ACS occurred in 22.6%. |
| Benenson et al. [26], 2018, USA | Retrospective | 62.2 ± 14.87 | 49.7 | 180/120 | 28.3 | NR | 42.6 | 1.2 | 41.4 | NR | NR | Cohorts predominantly African-American diabetics. Found MI in 42.6% of all participants (diabetic and nondiabetics) with NSTEMI constituting 41.4%. |
| Katz et al. [25], 2009, USA | CS | 58 (49–70) * | 51 | 180/110 | 59.4 | NR | 11 | NR | NR | NR | NR | Studied consecutive patients with acute severe hypertension across 25 institutions in the US. In-hospital mortality is chiefly driven by intracranial hemorrhage. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Talle, M.A.; Ngarande, E.; Doubell, A.F.; Herbst, P.G. Prevalence of Myocardial Injury and Myocardial Infarction in Patients with a Hypertensive Emergency: A Systematic Review. Diagnostics 2023, 13, 60. https://doi.org/10.3390/diagnostics13010060
Talle MA, Ngarande E, Doubell AF, Herbst PG. Prevalence of Myocardial Injury and Myocardial Infarction in Patients with a Hypertensive Emergency: A Systematic Review. Diagnostics. 2023; 13(1):60. https://doi.org/10.3390/diagnostics13010060
Chicago/Turabian StyleTalle, Mohammed A., Ellen Ngarande, Anton F. Doubell, and Philip G. Herbst. 2023. "Prevalence of Myocardial Injury and Myocardial Infarction in Patients with a Hypertensive Emergency: A Systematic Review" Diagnostics 13, no. 1: 60. https://doi.org/10.3390/diagnostics13010060
APA StyleTalle, M. A., Ngarande, E., Doubell, A. F., & Herbst, P. G. (2023). Prevalence of Myocardial Injury and Myocardial Infarction in Patients with a Hypertensive Emergency: A Systematic Review. Diagnostics, 13(1), 60. https://doi.org/10.3390/diagnostics13010060