Effectiveness of a Mobile App in Reducing Therapeutic Turnaround Time and Facilitating Communication between Caregivers in a Pediatric Emergency Department: A Randomized Controlled Pilot Trial
Abstract
:1. Introduction
2. Materials and Methods
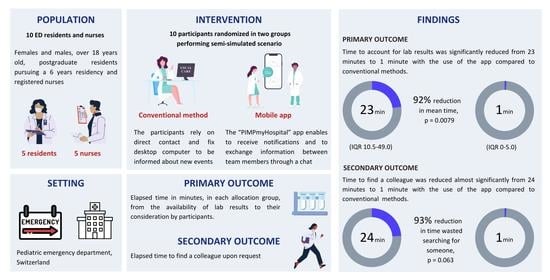
2.1. Study Design and Participants
2.2. Randomization and Blinding
2.3. The PIMPmyHospital App
2.4. Intervention
2.5. Measurement Instruments
2.6. Outcomes
2.7. Statistical Analysis
3. Results
3.1. Overview
3.2. Primary Outcome
3.3. Secondary Outcome
4. Discussion
5. Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Javidan, A.P.; Hansen, K.; Higginson, I.; Jones, P.; Lang, E. The International Federation for Emergency Medicine report on emergency department crowding and access block: A brief summary. Int. J. Emerg. Med. 2021, 14, 4. [Google Scholar] [CrossRef] [PubMed]
- Franklin, B.J.; Li, K.Y.; Somand, D.M.; Kocher, K.E.; Kronick, S.L.; Parekh, V.I.; Goralnick, E.; Nix, A.T.; Haas, N.L. Emergency department provider in triage: Assessing site-specific rationale, operational feasibility, and financial impact. J. Am. Coll. Emerg. Physicians Open 2021, 2, e12450. [Google Scholar] [CrossRef] [PubMed]
- Driesen, B.; van Riet, B.H.G.; Verkerk, L.; Bonjer, H.J.; Merten, H.; Nanayakkara, P.W.B. Long length of stay at the emergency department is mostly caused by organisational factors outside the influence of the emergency department: A root cause analysis. PLoS ONE 2018, 13, e0202751. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Trzeciak, S.; Rivers, E.P. Emergency department overcrowding in the United States: An emerging threat to patient safety and public health. Emerg. Med. J. 2003, 20, 402–405. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Andersson, J.; Nordgren, L.; Cheng, I.; Nilsson, U.; Kurland, L. Long emergency department length of stay: A concept analysis. Int. Emerg. Nurs. 2020, 53, 100930. [Google Scholar] [CrossRef]
- Yoon, P.; Steiner, I.; Reinhardt, G. Analysis of factors influencing length of stay in the emergency department. Can. J. Emerg. Med. 2003, 5, 155–161. [Google Scholar] [CrossRef] [Green Version]
- Van der Veen, D.; Remeijer, C.; Fogteloo, A.J.; Heringhaus, C.; de Groot, B. Independent determinants of prolonged emergency department length of stay in a tertiary care centre: A prospective cohort study. Scand. J. Trauma Resusc. Emerg. Med. 2018, 26, 81. [Google Scholar] [CrossRef]
- Mwogi, T.; Mercer, T.; Tran, D.N.T.; Tonui, R.; Tylleskar, T.; Were, M.C. Therapeutic turnaround times for common laboratory tests in a tertiary hospital in Kenya. PLoS ONE 2020, 15, e0230858. [Google Scholar] [CrossRef]
- Steindel, S.J.; Howanitz, P.J. Changes in emergency department turnaround time performance from 1990 to 1993: A comparison of two College of American Pathologists Q-probes studies. Arch. Pathol. Lab. Med. 1997, 121, 1031–1041. [Google Scholar]
- Hawkins, R.C. Laboratory turnaround time. Clin. Biochem. Rev. 2007, 28, 179–194. [Google Scholar]
- Tindle, K.; David, A.; Carlisle, S.; Faircloth, B.; Fields, J.M.; Hayden, G.; Ku, B. Relationship of the built environment on nursing communication patterns in the emergency department: A task performance and analysis time study. J. Emerg. Nurs. 2020, 46, 440–448. [Google Scholar] [CrossRef] [PubMed]
- Bekkink, M.O.; Farrell, S.E.; Takayesu, J.K. Interprofessional communication in the emergency department: Residents’ perceptions and implications for medical education. Int. J. Med. Educ. 2018, 9, 262–270. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ong, Z.H.; Tan, L.H.E.; Ghazali, H.Z.B.; Ong, Y.T.; Koh, Y.T.; Ang, R.Z.E.; Bok, C.; Chiam, M.; Lee, A.S.I.; Chin, A.M.C.; et al. A systematic scoping review on pedagogical strategies of interprofessional communication for physicians in emergency medicine. J. Med. Educ. Curric. Dev. 2021, 8, 23821205211041794. [Google Scholar] [CrossRef] [PubMed]
- Coiera, E.W.; Jayasuriya, R.A.; Hardy, J.; Bannan, A.; Thorpe, M.E. Communication loads on clinical staff in the emergency department. Med. J. Aust. 2002, 176, 415–418. [Google Scholar] [CrossRef] [PubMed]
- Woloshynowych, M.; Davis, R.; Brown, R.; Vincent, C. Communication patterns in a UK emergency department. Ann. Emerg. Med. 2007, 50, 407–413. [Google Scholar] [CrossRef]
- Weng, S.J.; Tsai, M.C.; Tsai, Y.T.; Gotcher, D.F.; Chen, C.H.; Liu, S.C.; Xu, Y.Y.; Kim, S.H. Improving the efficiency of an emergency department based on activity-relationship diagram and radio frequency identification technology. Int. J. Environ. Res. Public Health 2019, 16, 4478. [Google Scholar] [CrossRef] [Green Version]
- Hollingsworth, J.C.; Chisholm, C.D.; Giles, B.K.; Cordell, W.H.; Nelson, D.R. How do physicians and nurses spend their time in the emergency department? Ann. Emerg. Med. 1998, 31, 87–91. [Google Scholar] [CrossRef]
- Weigl, M.; Handl, T.; Wehler, M.; Schneider, A. Time-allocation study of nurse and physician activities in the emergency department. Med. Klin. Intensivmed. Notfmed. 2021, 116, 229–237. [Google Scholar] [CrossRef] [Green Version]
- Mamykina, L.; Vawdrey, D.K.; Hripcsak, G. How do residents spend their shift time? A time and motion study with a particular focus on the use of computers. Acad. Med. 2016, 91, 827–832. [Google Scholar] [CrossRef]
- Peters, G.A.; Wong, M.L.; Sanchez, L.D. Pedometer-measured physical activity among emergency physicians during shifts. Am. J. Emerg. Med. 2020, 38, 118–121. [Google Scholar] [CrossRef]
- Raymond, L.; Pare, G.; Maillet, E.; de Guinea, A.O.; Trudel, M.C.; Marsan, J. Improving performance in the ED through laboratory information exchange systems. Int. J. Emerg. Med. 2018, 11, 15. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alhejily, W.A. Implementing “chest pain pathway” using smartphone messaging application “WhatsApp” as a corrective action plan to improve ischemia time in “ST-Elevation Myocardial Infarction” in primary PCI capable center “WhatsApp-STEMI Trial”. Crit. Pathw. Cardiol. 2021, 20, 179–184. [Google Scholar] [CrossRef] [PubMed]
- Noone, M.L.; Moideen, F.; Krishna, R.B.; Kumar, V.G.P.; Karadan, U.; Chellenton, J.; Salam, K.A. Mobile app based strategy improves door-to-needle time in the treatment of acute ischemic stroke. J. Stroke Cerebrovasc. Dis. 2020, 29, 105319. [Google Scholar] [CrossRef] [PubMed]
- Ehrler, F.; Sahyoun, C.; Manzano, S.; Sanchez, O.; Gervaix, A.; Lovis, C.; Courvoisier, D.S.; Lacroix, L.; Siebert, J.N. Impact of a shared decision-making mHealth tool on caregivers’ team situational awareness, communication effectiveness, and performance during pediatric cardiopulmonary resuscitation: Study protocol of a cluster randomized controlled trial. Trials 2021, 22, 277. [Google Scholar] [CrossRef]
- Boillat, T.; Siebert, J.N.; Alduaij, N.; Ehrler, F. GOFlow: Smartwatch app to deliver laboratory results in emergency departments—A feasibility study. Int. J. Med. Inform. 2020, 134, 104034. [Google Scholar] [CrossRef]
- Ehrler, F.; Tuor, C.; Rey, R.; Siebert, J.N. A mobile app to improve patient management in emergency departments: Caregiver needs analysis, design and early technology acceptance assessment. Stud. Health Technol. Inform. 2021, 285, 233–238. [Google Scholar]
- Cheng, A.; Kessler, D.; Mackinnon, R.; Chang, T.P.; Nadkarni, V.M.; Hunt, E.A.; Duval-Arnould, J.; Lin, Y.; Cook, D.A.; Pusic, M.; et al. Reporting guidelines for health care simulation research: Extensions to the CONSORT and STROBE statements. Simul. Healthc. 2016, 11, 238–248. [Google Scholar] [CrossRef]
- Eysenbach, G.; Consort-Ehealth Group. Consort-Ehealth: Improving and standardizing evaluation reports of Web-based and mobile health interventions. J. Med. Internet Res. 2011, 13, e126. [Google Scholar] [CrossRef]
- Schulz, K.F.; Altman, D.G.; Moher, D.; Consort Group. CONSORT 2010 statement: Updated guidelines for reporting parallel group randomised trials. BMJ 2010, 340, c332. [Google Scholar] [CrossRef]
- Sealed Envelope Ltd. Simple Randomisation Service. 2021. Available online: https://www.sealedenvelope.com/simple-randomiser/v1 (accessed on 7 February 2022).
- Beveridge, R. CAEP issues. The Canadian Triage and Acuity Scale: A new and critical element in health care reform. Canadian Association of Emergency Physicians. J. Emerg. Med. 1998, 16, 507–511. [Google Scholar]
- Cairns, C.; Kang, K.; Santo, L. National Hospital Ambulatory Medical Care Survey: 2018 Emergency Department Summary Tables. 2018. Available online: https://www.cdc.gov/nchs/data/nhamcs/web_tables/2018-ed-web-tables-508.pdf (accessed on 7 February 2022).
- Rohr, U.P.; Binder, C.; Dieterle, T.; Giusti, F.; Messina, C.G.; Toerien, E.; Moch, H.; Schafer, H.H. The value of in vitro diagnostic testing in medical practice: A status report. PLoS ONE 2016, 11, e0149856. [Google Scholar] [CrossRef] [PubMed]
- Ong, M.S.; Magrabi, F.; Coiera, E. Delay in reviewing test results prolongs hospital length of stay: A retrospective cohort study. BMC Health Serv. Res. 2018, 18, 369. [Google Scholar] [CrossRef] [PubMed]
- Schimke, I. Quality and timeliness in medical laboratory testing. Anal. Bioanal. Chem. 2009, 393, 1499–1504. [Google Scholar] [CrossRef] [PubMed]
- Wilson, S.; Bohn, M.K.; Adeli, K. POCT: An inherently ideal tool in pediatric laboratory medicine. EJIFCC 2021, 32, 145–157. [Google Scholar]
- Goyder, C.; Tan, P.S.; Verbakel, J.; Ananthakumar, T.; Lee, J.J.; Hayward, G.; Turner, P.J.; Van Den Bruel, A. Impact of point-of-care panel tests in ambulatory care: A systematic review and meta-analysis. BMJ Open 2020, 10, e032132. [Google Scholar] [CrossRef] [Green Version]
- Alter, D.N. Point-of-care testing for the emergency department patient: Quantity and quality of the available evidence. Arch. Pathol. Lab. Med. 2021, 145, 308–319. [Google Scholar] [CrossRef]
- Gottlieb, M.; Farcy, D.A.; Moreno, L.A.; Vilke, G.M.; Guittard, J.A. Triage nurse-ordered testing in the emergency department setting: A review of the literature for the clinician. J. Emerg. Med. 2021, 60, 570–575. [Google Scholar] [CrossRef]
- Larsson, A.; Greig-Pylypczuk, R.; Huisman, A. The state of point-of-care testing: A European perspective. Ups. J. Med. Sci. 2015, 120, 1–10. [Google Scholar] [CrossRef]
- Á Torkilsheyggi, A.; Hertzum, M.; From, G. Evaluating the impact of electronic whiteboard icons: An observational study of the work with blood tests in an emergency department. Scand. J. Trauma Resusc. Emerg. Med. 2013, 1. [Google Scholar] [CrossRef] [Green Version]
- Hertzum, M.; Simonsen, J. Effects of electronic emergency-department whiteboards on clinicians’ time distribution and mental workload. Health Inform. J. 2016, 22, 3–20. [Google Scholar] [CrossRef] [Green Version]
- Salmasian, H.; Landman, A.B.; Morris, C. An electronic notification system for improving patient flow in the emergency department. AMIA Jt Summits Transl. Sci. Proc. 2019, 2019, 242–247. [Google Scholar] [PubMed]
- Chopra, V.; McMahon, L.F., Jr. Redesigning hospital alarms for patient safety: Alarmed and potentially dangerous. JAMA 2014, 311, 1199–1200. [Google Scholar] [CrossRef] [PubMed]
- Winters, B.D.; Slota, J.M.; Bilimoria, K.Y. Safety culture as a patient safety practice for alarm fatigue. JAMA 2021, 326, 1207–1208. [Google Scholar] [CrossRef] [PubMed]
- Slovis, B.H.; Nahass, T.A.; Salmasian, H.; Kuperman, G.; Vawdrey, D.K. Asynchronous automated electronic laboratory result notifications: A systematic review. J. Am. Med. Inform. Assoc. 2017, 24, 1173–1183. [Google Scholar] [CrossRef] [Green Version]
- Verma, A.; Wang, A.S.; Feldman, M.J.; Hefferon, D.A.; Kiss, A.; Lee, J.S. Push-alert notification of troponin results to physician smartphones reduces the time to discharge emergency department patients: A randomized controlled trial. Ann. Emerg Med. 2017, 70, 348–356. [Google Scholar] [CrossRef] [PubMed]
- Trotzky, D.; Posner, L.; Mosery, J.; Cohen, A.; Avisar, S.; Pachys, G. Do automatic push notifications improve patient flow in the emergency department? analysis of an ED in a large medical center in Israel. PLoS ONE 2021, 16, e0258169. [Google Scholar] [CrossRef]
- Koziatek, C.; Swartz, J.; Iturrate, E.; Levy-Lambert, D.; Testa, P. Decreasing the lag between result availability and decision-making in the emergency department using push notifications. West. J. Emerg Med. 2019, 20, 666–671. [Google Scholar] [CrossRef] [Green Version]
- Creswick, N.; Westbrook, J.I.; Braithwaite, J. Understanding communication networks in the emergency department. BMC Health Serv. Res. 2009, 9, 247. [Google Scholar] [CrossRef] [Green Version]
- Pun, J.K.; Chan, E.A.; Murray, K.A.; Slade, D.; Matthiessen, C.M. Complexities of emergency communication: Clinicians’ perceptions of communication challenges in a trilingual emergency department. J. Clin. Nurs. 2017, 26, 3396–3407. [Google Scholar] [CrossRef]
- Weigl, M.; Catchpole, K.; Wehler, M.; Schneider, A. Workflow disruptions and provider situation awareness in acute care: An observational study with emergency department physicians and nurses. Appl. Ergon. 2020, 88, 103155. [Google Scholar] [CrossRef]
- Weigl, M.; Beck, J.; Wehler, M.; Schneider, A. Workflow interruptions and stress at work: A mixed-methods study among physicians and nurses of a multidisciplinary emergency department. BMJ Open 2017, 7, e019074. [Google Scholar] [CrossRef] [PubMed]
- Pun, J.K.; Matthiessen, C.M.; Murray, K.A.; Slade, D. Factors affecting communication in emergency departments: Doctors and nurses’ perceptions of communication in a trilingual ED in Hong Kong. Int. J. Emerg. Med. 2015, 8, 48. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- The Joint Commission. 2022 National Patient Safety Goals. 2022. Available online: https://www.jointcommission.org/standards/national-patient-safety-goals/-/media/131f1a35ea9743eca04b9858b73b0a93.ashx (accessed on 7 February 2022).
- Dungarwalla, M.; Chapireau, D.; Bentley, R. Use of WhatsApp in an oral and maxillofacial surgery department at a major trauma centre and its role during major incidents: Our experience. Br. J. Oral Maxillofac. Surg. 2019, 57, 449–453. [Google Scholar] [CrossRef] [PubMed]
- Johnston, M.J.; King, D.; Arora, S.; Behar, N.; Athanasiou, T.; Sevdalis, N.; Darzi, A. Smartphones let surgeons know WhatsApp: An analysis of communication in emergency surgical teams. Am. J. Surg. 2015, 209, 45–51. [Google Scholar] [CrossRef] [PubMed]
- Watson, L.; Pathiraja, F.; Depala, A.; O’Brien, B.; Beyzade, S. Ensuring safe communication in health care: A response to Johnston et al on their paper “Smartphones let surgeons know WhatsApp: An analysis of communication in emergency surgical teams”. Am. J. Surg. 2016, 211, 302–303. [Google Scholar] [CrossRef] [PubMed]
- Kentab, O.; Soliman, K.; Al Ibrahim, A.A.; Alresseeni, A.; Aljohani, K.; Aljahany, M. A Push-to-talk Application as an interprofessional communication tool in an emergency department during the COVID-19 pandemic. Open Access Emerg. Med. 2021, 13, 189–199. [Google Scholar] [CrossRef]
- Hansen, J.E.; Lazow, M.; Hagedorn, P.A. Reducing interdisciplinary communication failures through secure text messaging: A quality improvement project. Pediatr. Qual. Saf. 2018, 3, e053. [Google Scholar] [CrossRef]
- Pourmand, A.; Roberson, J.; Gallugi, A.; Sabha, Y.; O’Connell, F. Secure smartphone application-based text messaging in emergency department, a system implementation and review of literature. Am. J. Emerg. Med. 2018, 36, 1680–1685. [Google Scholar] [CrossRef]
- Cheng, A.; Auerbach, M.; Hunt, E.A.; Chang, T.P.; Pusic, M.; Nadkarni, V.; Kessler, D. Designing and conducting simulation-based research. Pediatrics 2014, 133, 1091–1101. [Google Scholar] [CrossRef] [Green Version]
- Lundberg, G.D. Acting on significant laboratory results. JAMA 1981, 245, 1762–1763. [Google Scholar] [CrossRef]
- Pati, H.P.; Singh, G. Turnaround Time (TAT): Difference in Concept for Laboratory and Clinician. Indian J. Hematol. Blood Transfus. 2014, 30, 81–84. [Google Scholar] [CrossRef] [PubMed] [Green Version]




| PIMPmyHospital (N = 5) a | Control Group (N = 5) | |
|---|---|---|
| Age in years, mean (SD) | 34.2 (8.5) | 30.8 (3.7) |
| Age in years, n (%) | ||
| <30 | 1 (20.0) | 2 (40.0) |
| 30−39 | 3 (60.0) | 3 (60.0) |
| ≥40 | 1 (20.0) | 0 (0) |
| Gender, n (%) | ||
| Female | 4 (40) | 4 (40) |
| Male | 1 (10) | 1 (10) |
| Work experience in years since certification, mean (SD) | 10.8 (9.1) | 5.8 (3.4) |
| Work experience in years since certification, n (%) | ||
| <5 | 1 (20.0) | 2 (40.0) |
| 5−9 | 2 (40.0) | 2 (40.0) |
| ≥9 | 2 (40.0) | 1 (20.0) |
| Work experience in months in the PED, mean (SD) | 36.6 (26.6) | |
| Work experience in months in the PED, n (%) | ||
| <12 | 1 (20.0) | 1 (20.0) |
| 12−24 | 1 (20.0) | 1 (20.0) |
| ≥24 | 3 (60.0) | 3 (60.0) |
| Satisfaction b with current timelines from laboratory report to review, mean (SD) | ||
| 4.4 (1.1) | 5.0 (3.0) | |
| Satisfaction b with current situation to find a peer, mean (SD) | ||
| 3.6 (0.5) | 2.2 (1.8) | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ehrler, F.; Tuor, C.; Trompier, R.; Berger, A.; Ramusi, M.; Rey, R.; Siebert, J.N. Effectiveness of a Mobile App in Reducing Therapeutic Turnaround Time and Facilitating Communication between Caregivers in a Pediatric Emergency Department: A Randomized Controlled Pilot Trial. J. Pers. Med. 2022, 12, 428. https://doi.org/10.3390/jpm12030428
Ehrler F, Tuor C, Trompier R, Berger A, Ramusi M, Rey R, Siebert JN. Effectiveness of a Mobile App in Reducing Therapeutic Turnaround Time and Facilitating Communication between Caregivers in a Pediatric Emergency Department: A Randomized Controlled Pilot Trial. Journal of Personalized Medicine. 2022; 12(3):428. https://doi.org/10.3390/jpm12030428
Chicago/Turabian StyleEhrler, Frederic, Carlotta Tuor, Remy Trompier, Antoine Berger, Michael Ramusi, Robin Rey, and Johan N. Siebert. 2022. "Effectiveness of a Mobile App in Reducing Therapeutic Turnaround Time and Facilitating Communication between Caregivers in a Pediatric Emergency Department: A Randomized Controlled Pilot Trial" Journal of Personalized Medicine 12, no. 3: 428. https://doi.org/10.3390/jpm12030428
APA StyleEhrler, F., Tuor, C., Trompier, R., Berger, A., Ramusi, M., Rey, R., & Siebert, J. N. (2022). Effectiveness of a Mobile App in Reducing Therapeutic Turnaround Time and Facilitating Communication between Caregivers in a Pediatric Emergency Department: A Randomized Controlled Pilot Trial. Journal of Personalized Medicine, 12(3), 428. https://doi.org/10.3390/jpm12030428