The Effectiveness of Predicting Suicidal Ideation through Depressive Symptoms and Social Isolation Using Machine Learning Techniques
Abstract
:1. Introduction
2. Materials and Methods
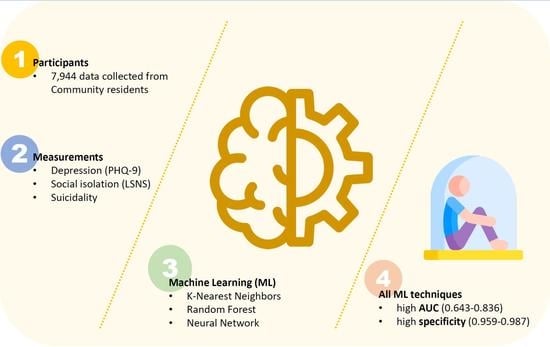
2.1. Participants
2.2. Measurements
2.2.1. The Patient Health Quessionnaire-9 (PHQ-9)
2.2.2. Lubben Social Network Scale (LSNS)
2.2.3. Assessment for Suicide
2.3. Statistical Analysis
2.3.1. K-Nearest Neighbors Classification (KNN)
2.3.2. Random Forest Classification (RF)
2.3.3. Neural Network (NN) Classification
3. Results
3.1. Experimental Results
General Characteristics
3.2. Machine Learning Model Analysis
3.2.1. Validation Accuracy of the Prediction Machine Learning Model
3.2.2. Diagnostics Characteristics of Suicidal Ideation Using Machine Learning
3.2.3. Variable Importance in Random Forest Model
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| No. | Question |
|---|---|
| item 1 | Think that you would be better off dead or wish you were dead? |
| item 2 | Want to harm yourself or to hurt or to injure yourself? |
| item 3 | Think about suicide? |
| ML Methods | Model | Validation Accuracy | Test Accuracy | Precision | Recall | F1 Score |
|---|---|---|---|---|---|---|
| KNN | model 1 | 0.909 | 0.902 | 0.880 | 0.902 | 0.884 |
| model 2 | 0.900 | 0.907 | 0.888 | 0.907 | 0.892 | |
| RF | model 1 | 0.905 | 0.904 | 0.885 | 0.904 | 0.871 |
| model 2 | 0.905 | 0.911 | 0.895 | 0.911 | 0.896 | |
| NN | model 1 | 0.922 | 0.918 | 0.904 | 0.918 | 0.904 |
| model 2 | 0.916 | 0.911 | 0.896 | 0.911 | 0.896 |
References
- Beutel, M.E.; Klein, E.M.; Brähler, E.; Reiner, I.; Jünger, C.; Michal, M.; Wiltink, J.; Wild, P.S.; Münzel, T.; Lackner, K.J.; et al. Loneliness in the general population: Prevalence, determinants and relations to mental health. BMC Psychiatry 2017, 17, 97. [Google Scholar] [CrossRef] [Green Version]
- Silvera, D.H.; Seger, C.R. Feeling good about ourselves: Unrealistic self-evaluations and their relation to self-esteem in the United States and Norway. J. Cross-Cult. Psychol. 2004, 35, 571–585. [Google Scholar] [CrossRef]
- Mellor, D.; Stokes, M.; Firth, L.; Hayashi, Y.; Cummins, R. Need for belonging, relationship satisfaction, loneliness, and life satisfaction. Personal. Individ. Differ. 2008, 45, 213–218. [Google Scholar] [CrossRef]
- House, J.S.; Landis, K.R.; Umberson, D. Social relationships and health. Science 1988, 241, 540–545. [Google Scholar] [CrossRef]
- Buda, M.; Tsuang, M.T. The epidemiology of suicide: Implications for clinical practice. In Suicide over the Life Cycle: Risk Factors, Assessment, and Treatment of Suicidal Patients; American Psychiatric Association: Washington, DC, USA, 1990. [Google Scholar]
- Maris, R.; Maris, R.W.; Lazerwitz, B.M. Pathways to Suicide: A Survey of Self-Destructive Behaviors; Johns Hopkins University Press: Baltimore, MD, USA, 1981. [Google Scholar]
- Barraclough, B.M.; Pallis, D.J. Depression followed by suicide: A comparison of depressed suicides with living depressives. Psychol. Med. 1975, 5, 55–61. [Google Scholar] [CrossRef]
- Chynoweth, R.; Tonge, J.I.; Armstrong, J. Suicide in Brisbane—A Retrospective Psychosocial Study. Aust. New Zeal. J. Psychiatry 1980, 14, 37–45. [Google Scholar] [CrossRef]
- Robins, E.; Gassner, S.; Kayes, J.; Wilkinson, R.H., Jr.; Murphy, G.E. The communication of suicidal intent: A study of 134 consecutive cases of successful (completed) suicide. Am. J. Psychiatry 1959, 115, 724–733. [Google Scholar] [CrossRef]
- Bastiampillai, T.; Allison, S.; Chan, K.W. Is depression contagious? The importance of social networks and the implications of contagion theory. Aust. New Zeal. J. Psychiatry 2013, 47, 299–303. [Google Scholar] [CrossRef] [PubMed]
- Flaherty, J.A.; Gaviria, F.M.; Black, E.M.; Altman, E.; Mitchell, T. The role of social support in the functioning of patients with unipolar depression. Am. J. Psychiatry 1983, 140, 473–476. [Google Scholar] [CrossRef] [PubMed]
- Greenblatt, M.; Becerra, R.M.; Serafetinides, E.A. Social networks and mental health: On overview. Am. J. Psychiatry 1982, 139, 977–984. [Google Scholar] [CrossRef] [PubMed]
- Allebeck, P.; Allgulander, C. Suicide among young men: Psychiatric illness, deviant behaviour and substance abuse. Acta Psychiatr. Scand. 1990, 81, 565–570. [Google Scholar] [CrossRef]
- Patterson, W.M.; Dohn, H.H.; Bird, J.; Patterson, G.A. Evaluation of suicidal patients: The Sad Persons scale. J. Psychosom. Res. 1983, 24, 343–349. [Google Scholar] [CrossRef]
- Almeida, J.; Subramanian, S.V.; Kawachi, I.; Molnar, B.E. Is blood thicker than water? Social support, depression and the modifying role of ethnicity/nativity status. J. Epidemiol. Community Health 2011, 65, 51–56. [Google Scholar] [CrossRef] [PubMed]
- Molloy, G.J.; Perkins-Porras, L.; Bhattacharyya, M.R.; Strike, P.C.; Steptoe, A. Practical support predicts medication adherence and attendance at cardiac rehabilitation following acute coronary syndrome. J. Psychosom. Res. 2008, 65, 581–586. [Google Scholar] [CrossRef]
- Vyavaharkar, M.; Moneyham, L.; Tavakoli, A.; Phillips, K.D.; Murdaugh, C.; Jackson, K.; Meding, G. Social Support, Coping, and Medication Adherence Among HIV-Positive Women with Depression Living in Rural Areas of the Southeastern United States. AIDS Patient Care STDs 2007, 21, 667–680. [Google Scholar] [CrossRef]
- Kotler, M.; Iancu, I.; Efroni, R.; Amir, M. Anger, Impulsivity, Social Support, and Suicide Risk in Patients with Posttraumatic Stress Disorder. J. Nerv. Ment. Dis. 2001, 189, 162–167. [Google Scholar] [CrossRef]
- Hovey, J.D. Acculturative stress, depression, and suicidal ideation among Central American immigrants. Suicide Life-Threat. Behav. 2000, 30, 125–139. [Google Scholar]
- King, C.A.; Franzese, R.; Gargan, S.; McGovern, L.; Ghaziuddin, N.; Naylor, M.W. Suicide contagion among adolescents during acute psychiatric hospitalization. Psychiatry Serv. 1995, 46, 915–918. [Google Scholar] [CrossRef] [PubMed]
- Summerville, M.B.; Kaslow, N.J.; Abbate, M.F.; Cronan, S. Psychopathology, family functioning, and cognitive style in urban adolescents with suicide attempts. J. Abnorm. Child Psychol. 1994, 22, 221–235. [Google Scholar] [CrossRef] [PubMed]
- Lewinsohn, P.M.; Rohde, P.; Seeley, J.R.; Baldwin, C.L. Gender Differences in Suicide Attempts from Adolescence to Young Adulthood. J. Am. Acad. Child Adolesc. Psychiatry 2001, 40, 427–434. [Google Scholar] [CrossRef]
- King, C.A.; Hovey, J.D.; Brand, E.; Wilson, R.; Ghaziuddin, N. Suicidal Adolescents after Hospitalization: Parent and Family Impacts on Treatment Follow-through. J. Am. Acad. Child Adolesc. Psychiatry 1997, 36, 85–93. [Google Scholar] [CrossRef]
- Hagerty, B.M.; Williams, A. The effects of sense of belonging, social support, conflict, and loneliness on depression. Nurs. Res. 1999, 48, 215–219. [Google Scholar] [CrossRef] [PubMed]
- Hagerty, B.M.; Patusky, K. Developing a measure of sense of belonging. Nurs. Res. 1995, 44, 9–13. [Google Scholar] [CrossRef]
- Hagerty, B.M.; Williams, R.A.; Coyne, J.C.; Early, M.R. Sense of belonging and indicators of social and psychological functioning. Arch. Psychiatr. Nurs. 1996, 10, 235–244. [Google Scholar] [CrossRef]
- McLaren, S.; Jude, B.; Hopes, L.; Sherritt, T. Sense of belonging, stress and depression in rural-urban communities. Int. J. Rural. Psychol. 2001, 2, 15. [Google Scholar]
- Kim, B.-M.; You, S. Social Connections and Emotion Regulation in Suicidal Ideation among Individulas with Interpersonal Trauma. Korean J. Clin. Psychol. 2012, 31, 731–748. [Google Scholar]
- Sainsbury, P. Suicide in London. Maudsley monographs. Br. J. Psychiatry 1955, 157, 871–876. [Google Scholar]
- Bosselman, B.C. Self-Destruction: A Study of the Suicidal Impulse; Thomas: Springfield, IL, USA, 1958. [Google Scholar]
- Carstairs, G.M. Characteristics of the suicide-prone. Proc. R. Soc. Med. 1961, 54, 262–264. [Google Scholar] [CrossRef] [Green Version]
- Cazzulo, C.; Invernizzi, O.; Vitaly, A. Suicide, attempted suicide and community. Soc. Psychiatry 1974, 2, 267–291. [Google Scholar]
- Dublin, L.I. Suicide: An overview of a health and social problem. Bull. Suicidol. 1967, 25–30. [Google Scholar]
- McCulloch, J.; Philip, A. Social factors associated with attempted suicide: A review of the literature. Br. J. Psychiatr. Soc. Work. 1967, 9, 30–36. [Google Scholar]
- Silverman, M.M.; Maris, R.W. The prevention of suicidal behaviors: An overview. Suicide Life-Threat. Behav. 1995, 25, 10–21. [Google Scholar]
- Shneidman, E.S. Suicide, lethality, and the psychological autopsy. Int. Psychiatry Clin. 1969, 6, 225–250. [Google Scholar] [PubMed]
- Feldman, S.S.; Elliott, G.R.; Elliott, G.R. At the Threshold: The Developing Adolescent; Harvard University Press: Cambridge, MA, USA, 1990. [Google Scholar]
- Davidson, L.; Linnoila, M. Risk Factors for Youth Suicide; Taylor & Francis: Abingdon-on-Thames, UK, 2013. [Google Scholar]
- Hirsch, J.K.; Cukrowicz, K.C. Suicide in rural areas: An updated review of the literature. J. Rural Ment. Health 2014, 38, 65–78. [Google Scholar] [CrossRef] [Green Version]
- Jacobs, J. Adolescent Suicide Attempts: The Culmination of a Progressive Social Isolation; University of California at Los Angeles: Los Angeles, CA, USA, 1967. [Google Scholar]
- Joiner, T.E. Why People Die by Suicide; Harvard University Press: Cambridge, MA, USA, 2005. [Google Scholar]
- Stengel, E.; Cook, N.; Kreeger, I. Attempted Suicide: Its Social Significance and Effects; Maudsley Monographs, No. 4; Chapman & Hall London: London, UK, 1958. [Google Scholar]
- Wold, C.I. Characteristics of 26,000 suicide prevention center patients. Bull. Suicidol. 1970, 6, 24–28. [Google Scholar]
- Blazer, D.G. Suicide risk factors in the elderly: An epidemiological study. J. Geriatr. Psychiatry 1991, 24, 175–190. [Google Scholar]
- Lebret, S.; Perret-Vaille, E.; Mulliez, A.; Gerbaud, L.; Jalenques, I. Elderly suicide attempters: Characteristics and outcome. Int. J. Geriatr. Psychiatry J. Psychiatry Late Life Allied Sci. 2006, 21, 1052–1059. [Google Scholar] [CrossRef]
- Palmore, E.B. Handbook on the Aged in the United States; Greenwood Press: Westport, CT, USA, 1984. [Google Scholar]
- Vanderhorst, R.K.; McLaren, S. Social relationships as predictors of depression and suicidal ideation in older adults. Aging Ment. Heal. 2005, 9, 517–525. [Google Scholar] [CrossRef] [PubMed]
- Trout, D.L. The role of social isolation in suicide. Suicide Life-Threat. Behav. 1980, 10, 10–23. [Google Scholar] [CrossRef]
- O’Connor, R.C. Towards an integrated motivational–volitional model of suicidal behaviour. In International Handbook of Suicide Prevention: Research, Policy and Practice; John Wiley & Sons: Hoboken, NJ, USA, 2011; pp. 181–198. [Google Scholar]
- Klonsky, E.D.; May, A.M. The Three-Step Theory (3ST): A New Theory of Suicide Rooted in the “Ideation-to-Action” Framework. Int. J. Cogn. Ther. 2015, 8, 114–129. [Google Scholar] [CrossRef] [Green Version]
- Nock, M.K.; Borges, G.; Bromet, E.J.; Cha, C.B.; Kessler, R.C.; Lee, S. Suicide and suicidal behavior. Epidemiol. Rev. 2008, 30, 133–154. [Google Scholar] [CrossRef] [PubMed]
- Van Heeringen, K.; Mann, J.J. The neurobiology of suicide. Lancet Psychiatry 2014, 1, 63–72. [Google Scholar] [CrossRef]
- Courtet, P.; Gottesman, I.I.; Jollant, F.; Gould, T. The neuroscience of suicidal behaviors: What can we expect from endophenotype strategies? Transl. Psychiatry 2011, 1, e7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mann, J.J. Neurobiology of suicidal behaviour. Nat. Rev. Neurosci. 2003, 4, 819–828. [Google Scholar] [CrossRef] [PubMed]
- Beautrais, A.L. Serious Suicide Attempts in Young People: A Case Control Study; University of Otago: Dunedin, New Zealand, 1996. [Google Scholar]
- Henriksson, M.M.; Aro, H.M.; Marttunen, M.J.; Heikkinen, M.E.; Isometsä, E.T.; Kuoppasalmi, K.I.; Lönnqvist, J.K. Mental disorders and comorbidity in suicide. Am. J. Psychiatry 1993, 150, 935–940. [Google Scholar] [CrossRef]
- Brent, D.A.; Perper, J.A.; Moritz, G.; Allman, C.; Friend, A.; Roth, C.; Schweers, J.; Balach, L.; Baugher, M. Psychiatric Risk Factors for Adolescent Suicide: A Case-Control Study. J. Am. Acad. Child Adolesc. Psychiatry 1993, 32, 521–529. [Google Scholar] [CrossRef] [PubMed]
- Lesage, A.D.; Boyer, R.; Grunberg, F.; Morisette, R.; Vanier, C.; Morissette, R.; Ménard-Buteau, C.; Loyer, M. Suicide and mental disorders: A case-control study of young men. Am. J. Psychiatry 1994, 151, 1063–1068. [Google Scholar] [CrossRef]
- Trautman, P.D.; Rotheram-Borus, M.J.; Dopkins, S.; Lewin, N. Psychiatric Diagnoses in Minority Female Adolescent Suicide Attempters. J. Am. Acad. Child Adolesc. Psychiatry 1991, 30, 617–622. [Google Scholar] [CrossRef]
- Packman, W.L.; Marlitt, R.E.; Bongar, B.; O’Connor Pennuto, T. A comprehensive and concise assessment of suicide risk. Behav. Sci. Law 2004, 22, 667–680. [Google Scholar] [CrossRef]
- O’Connor, R.C.; Nock, M.K. The psychology of suicidal behaviour. Lancet Psychiatry 2014, 1, 73–85. [Google Scholar] [CrossRef]
- May, A.M.; Klonsky, E.D. What distinguishes suicide attempters from suicide ideators? A meta-analysis of potential factors. Clin. Psychol. Sci. Pract. 2016, 23, 5. [Google Scholar]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B. The PHQ-9: Validity of a brief depression severity measure. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef] [PubMed]
- Park, S.-J.; Choi, H.-R.; Choi, J.-H.; Kim, K.-W.; Hong, J.-P. Reliability and validity of the Korean version of the Patient Health Questionnaire-9 (PHQ-9). Anxiety Mood 2010, 6, 119–124. [Google Scholar]
- Lubben, J.E. Assessing social networks among elderly populations. Fam. Community Health 1988, 11, 42–52. [Google Scholar] [CrossRef]
- Yoo, S.-W.; Kim, Y.-S.; Noh, J.-S.; Oh, K.-S.; Kim, C.-H.; NamKoong, K.; Chae, J.-H.; Lee, G.-C.; Jeon, S.-I.; Min, K.-J. Validity of Korean version of the mini-international neuropsychiatric interview. Anxiety Mood 2006, 2, 50–55. [Google Scholar]
- James, G.; Witten, D.; Hastie, T.; Tibshirani, R. An Introduction to Statistical Learning; Springer: Berlin/Heidelberg, Germany, 2013; Volume 112. [Google Scholar]
- Breiman, L. Random forests. Mach. Learn. 2001, 45, 5–32. [Google Scholar] [CrossRef] [Green Version]
- Fine, T.L. Feedforward Neural Network Methodology; Springer Science & Business Media: Berlin/Heidelberg, Germany, 2006. [Google Scholar]
- Cheong, K.-S.; Choi, M.-H.; Cho, B.-M.; Yoon, T.-H.; Kim, C.-H.; Kim, Y.-M.; Hwang, I.-K. Suicide rate differences by sex, age, and urbanicity, and related regional factors in Korea. J. Prev. Med. Public Health 2012, 45, 70. [Google Scholar] [CrossRef]
- Kim, S.; Lee, H.-K.; Lee, K. Which PHQ-9 Items Can Effectively Screen for Suicide? Machine Learning Approaches. Int. J. Environ. Res. Public Health 2021, 18, 3339. [Google Scholar] [CrossRef]
- Pompili, M.; Murri, M.B.; Patti, S.; Innamorati, M.; Lester, D.; Girardi, P.; Amore, M. The communication of suicidal intentions: A meta-analysis. Psychol. Med. 2016, 46, 2239–2253. [Google Scholar] [CrossRef] [PubMed]
- Fazel, S.; O’Reilly, L. Machine Learning for Suicide Research—Can It Improve Risk Factor Identification? JAMA Psychiatry 2020, 77, 13–14. [Google Scholar] [CrossRef]
- Menton, W.H. Generalizability of statistical prediction from psychological assessment data: An investigation with the MMPI-2-RF. Psychol. Assess. 2020, 32, 473–492. [Google Scholar] [CrossRef] [Green Version]
- Efron, B.; Hastie, T. Computer Age Statistical Inference, Student Edition: Algorithms, Evidence, and Data Science; Cambridge University Press: Cambridge, UK, 2021; Volume 6. [Google Scholar]
- Hastie, T.; Tibshirani, R.; Friedman, J.H.; Friedman, J.H. The Elements of Statistical Learning: Data Mining, Inference, and Prediction; Springer: Berlin/Heidelberg, Germany, 2009; Volume 2. [Google Scholar]
- Yarkoni, T.; Westfall, J. Choosing prediction over explanation in psychology: Lessons from machine learning. Perspect. Psychol. Sci. 2017, 12, 1100–1122. [Google Scholar] [CrossRef] [PubMed]
- Linthicum, K.P.; Schafer, K.M.; Ribeiro, J.D. Machine learning in suicide science: Applications and ethics. Behav. Sci. Law 2019, 37, 214–222. [Google Scholar] [CrossRef] [PubMed]
- Lim, J.T.; Park, J.-H.; Lee, J.-S.; Oh, J.; Kim, Y. The Relationship Between the Social Network of Community-living Elders and Their Health-related Quality of Life in Korean Province. J. Prev. Med. Public Health 2013, 46, 28–38. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Farberow, N.L.; Heilig, S.; Litman, R.E. Evaluation and management of suicidal persons. In The Psychology of Suicide; Shneidman, E.S., Farberow, N.L., Litman, R.E., Eds.; New York Science House: New York, NY, USA, 1970; pp. 273–291. [Google Scholar]
- Jacobs, J. Adolescent Suicide; American Psychological Association: Washington, DC, USA, 1971. [Google Scholar]
- Cheng, A.T.; Chen, T.H.; Chen, C.-C.; Jenkins, R. Psychosocial and psychiatric risk factors for suicide: Case-control psychological autopsy study. Br. J. Psychiatry 2000, 177, 360–365. [Google Scholar] [CrossRef] [Green Version]
- Denney, J.T. Family and Household Formations and Suicide in the United States. J. Marriage Fam. 2010, 72, 202–213. [Google Scholar] [CrossRef]
- Denney, J.T.; Rogers, R.G.; Krueger, P.M.; Wadsworth, T. Adult Suicide Mortality in the United States: Marital Status, Family Size, Socioeconomic Status, and Differences by Sex. Soc. Sci. Q. 2009, 90, 1167–1185. [Google Scholar] [CrossRef] [Green Version]
- Duberstein, P.; Conwell, Y.; Conner, K.R.; Eberly, S.; Caine, E.D. Suicide at 50 years of age and older: Perceived physical illness, family discord and financial strain. Psychol. Med. 2004, 34, 137–146. [Google Scholar] [CrossRef]
- Kposowa, A.J. Marital status and suicide in the National Longitudinal Mortality Study. J. Epidemiol. Community Health 2000, 54, 254–261. [Google Scholar] [CrossRef] [Green Version]
- Qin, P.; Mortensen, P.B. The Impact of Parental Status on the Risk of Completed Suicide. Arch. Gen. Psychiatry 2003, 60, 797–802. [Google Scholar] [CrossRef]
- Rubenowitz, E.; Waern, M.; Wilhelmson, K.; Allebeck, P. Life events and psychosocial factors in elderly suicides–A case—control study. Psychol. Med. 2001, 31, 1193–1202. [Google Scholar] [CrossRef] [PubMed]

| Variables | Items | No Suicidal Ideation (n = 7214) | With Suicidal Ideation (n = 780) | t or x2 | p |
|---|---|---|---|---|---|
| sex (male) | 2820 (39.1%) | 260 (33.3%) | 9.854 | 0.002 | |
| age | 56.08 ± 16.43 | 59.42 ± 17.55 | 5.071 | <0.001 | |
| PHQ-9 total | 1.86 ± 2.84 | 9.03 ± 6.59 | 30.082 | <0.001 | |
| LSNS | 30.26 ± 7.77 | 25.73 ± 8.29 | 14.573 | <0.001 | |
| family networks | 8.91 ± 3.11 | 7.45 ± 3.26 | 11.949 | <0.001 | |
| friend networks | 7.35 ± 3.45 | 5.62 ± 3.64 | 12.657 | <0.001 | |
| confidant relationships | 5.37 ± 2.66 | 4.66 ± 2.86 | 6.655 | <0.001 | |
| living arrangements | 2.13 ± 1.96 | 1.31 ± 1.75 | 4.764 | <0.001 | |
| ML Methods | Model | Validation Accuracy | Test Accuracy | Precision | Recall | F1 Score |
|---|---|---|---|---|---|---|
| KNN | model 1 1 | 0.920 | 0.916 | 0.901 | 0.916 | 0.903 |
| model 2 2 | 0.923 | 0.913 | 0.898 | 0.913 | 0.902 | |
| RF | model 1 | 0.905 | 0.907 | 0.896 | 0.907 | 0.900 |
| model 2 | 0.912 | 0.921 | 0.906 | 0.921 | 0.905 | |
| NN | model 1 | 0.909 | 0.921 | 0.912 | 0.921 | 0.911 |
| model 2 | 0.923 | 0.912 | 0.897 | 0.912 | 0.899 |
| ML Methods | Model | AUC | Sensitivity (%) | Specificity (%) | PPV (%) | NPV (%) |
|---|---|---|---|---|---|---|
| KNN | model 1 | 0.778 | 0.297 (22.504–37.787) | 0.959 (94.812–96.892) | 0.423 (34.061–51.006) | 0.932 (92.475–93.816) |
| model 2 | 0.830 | 0.325 (25.065–40.540) | 0.974 (96.493–98.193) | 0.570 (47.211–66.229) | 0.933 (92.522–93.919) | |
| RF | model 1 | 0.645 | 0.380 (30.382–46.027) | 0.965 (95.448–97.412) | 0.545 (46.129–62.710) | 0.934 (92.620–94.128) |
| model 2 | 0.836 | 0.252 (18.297–33.110) | 0.987 (97.968–99.212) | 0.655 (52.760–76.272) | 0.931 (92.425–93.656) | |
| NN | model 1 | 0.702 | 0.406 (33.136–48.375) | 0.982 (97.426–98.864) | 0.734 (64.250–80.911) | 0.933 (92.462–94.023) |
| model 2 | 0.643 | 0.313 (24.165–39.045) | 0.979 (97.035–98.588) | 0.625 (52.216–71.768) | 0.928 (92.017–93.427) |
| Variables | Mean Decrease in Accuracy | Total Increase in Node Purity |
|---|---|---|
| PHQ-9 total | 0.0230 | 0.2360 |
| LSNS total | −0.0005 | 0.0280 |
| Age | 0.0009 | −0.0009 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, S.; Lee, K. The Effectiveness of Predicting Suicidal Ideation through Depressive Symptoms and Social Isolation Using Machine Learning Techniques. J. Pers. Med. 2022, 12, 516. https://doi.org/10.3390/jpm12040516
Kim S, Lee K. The Effectiveness of Predicting Suicidal Ideation through Depressive Symptoms and Social Isolation Using Machine Learning Techniques. Journal of Personalized Medicine. 2022; 12(4):516. https://doi.org/10.3390/jpm12040516
Chicago/Turabian StyleKim, Sunhae, and Kounseok Lee. 2022. "The Effectiveness of Predicting Suicidal Ideation through Depressive Symptoms and Social Isolation Using Machine Learning Techniques" Journal of Personalized Medicine 12, no. 4: 516. https://doi.org/10.3390/jpm12040516
APA StyleKim, S., & Lee, K. (2022). The Effectiveness of Predicting Suicidal Ideation through Depressive Symptoms and Social Isolation Using Machine Learning Techniques. Journal of Personalized Medicine, 12(4), 516. https://doi.org/10.3390/jpm12040516