Incident Rheumatoid Arthritis Following Statin Use: From the View of a National Cohort Study in Korea
Abstract
:1. Introduction
2. Patients and Methods
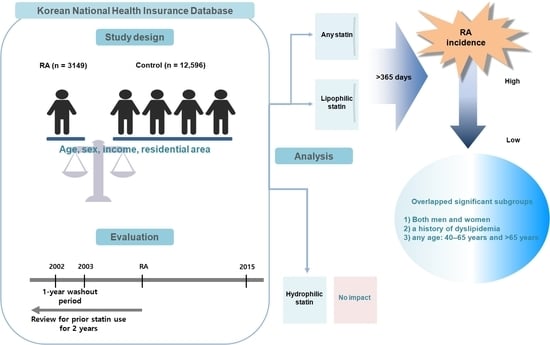
2.1. Study Design and Participants
2.2. Exposure (Statin)
2.3. Outcome (Rheumatoid Arthritis)
2.4. Covariates
2.5. Statistical Analyses
3. Results
3.1. Baseline Characteristics of the Study Participants
3.2. Odds Ratios of the Incidence of RA for the Duration of Use and Types of Statins
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lee, E.E.; Shin, A.; Lee, J.; Lee, J.H.; Ha, Y.J.; Lee, Y.J.; Lee, E.B.; Song, Y.W.; Kang, E.H. All-cause and cause-specific mortality of patients with rheumatoid arthritis in Korea: A nation-wide population-based study. Jt. Bone Spine 2021, 89, 105269. [Google Scholar] [CrossRef]
- Kim, H.; Sung, Y.-K. Epidemiology of Rheumatoid Arthritis in Korea. J. Rheum. Dis. 2021, 28, 60–67. [Google Scholar] [CrossRef]
- Hur, N.W.; Choi, C.B.; Uhm, W.S.; Bae, S.C. The prevalence and trend of arthritis in Korea: Results from Korea National Health and Nutrition Examination Surveys. J. Korean Rheum. Assoc. 2008, 10, 151–157. [Google Scholar] [CrossRef] [Green Version]
- Kato, E.; Sawada, T.; Tahara, K.; Hayashi, H.; Tago, M.; Mori, H.; Nishino, J.; Matsui, T.; Tohma, S. The age at onset of rheumatoid arthritis is increasing in Japan: A nationwide database study. Int. J. Rheum. Dis. 2017, 20, 839–845. [Google Scholar] [CrossRef] [PubMed]
- Cross, M.; Smith, E.; Hoy, D.; Carmona, L.; Wolfe, F.; Vos, T.; Williams, B.; Gabriel, S.; Lassere, M.; Johns, N.; et al. The global burden of rheumatoid arthritis: Estimates from the global burden of disease 2010 study. Ann. Rheum. Dis. 2014, 73, 1316–1322. [Google Scholar] [CrossRef] [PubMed]
- Safiri, S.; Kolahi, A.A.; Hoy, D.; Smith, E.; Bettampadi, D.; Mansournia, M.A.; Almasi-Hashiani, A.; Ashrafi-Asgarabad, A.; Moradi-Lakeh, M.; Qorbani, M.; et al. Global, regional and national burden of rheumatoid arthritis 1990-2017: A systematic analysis of the Global Burden of Disease study 2017. Ann. Rheum. Dis. 2019, 78, 1463–1471. [Google Scholar] [CrossRef]
- Choi, I.A.; Lee, J.S.; Song, Y.W.; Lee, E.Y. Mortality, disability, and healthcare expenditure of patients with seropositive rheumatoid arthritis in Korea: A nationwide population-based study. PLoS ONE 2019, 14, e0210471. [Google Scholar] [CrossRef]
- Zemedikun, D.T.; Gokhale, K.; Chandan, J.S.; Cooper, J.; Lord, J.M.; Filer, A.; Falahee, M.; Nirantharakumar, K.; Raza, K. Type 2 diabetes mellitus, glycaemic control, associated therapies and risk of rheumatoid arthritis: A retrospective cohort study. Rheumatology 2021, 60, 5567–5575. [Google Scholar] [CrossRef]
- Wells, I.; Zemedikun, D.T.; Simons, G.; Stack, R.J.; Mallen, C.D.; Raza, K.; Falahee, M. Predictors of interest in predictive testing for rheumatoid arthritis amongst first degree relatives of rheumatoid arthritis patients. Rheumatology 2021, keab890, online ahead of print. [Google Scholar] [CrossRef]
- Deane, K.D.; Demoruelle, M.K.; Kelmenson, L.B.; Kuhn, K.A.; Norris, J.M.; Holers, V.M. Genetic and environmental risk factors for rheumatoid arthritis. Best Pract. Res. Clin. Rheumatol. 2017, 31, 3–18. [Google Scholar] [CrossRef]
- Asoudeh, F.; Djafarian, K.; Akhalghi, M.; Mahmoudi, M.; Jamshidi, A.R.; Farhadi, E.; Esmaillzadeh, A. The effect of probiotic cheese consumption on inflammatory and anti-inflammatory markers, disease severity, and symptoms in patients with rheumatoid arthritis: Study protocol for a randomized, double-blind, placebo-controlled trial. Trials 2022, 23, 180. [Google Scholar] [CrossRef] [PubMed]
- Soulaidopoulos, S.; Nikiphorou, E.; Dimitroulas, T.; Kitas, G.D. The Role of Statins in Disease Modification and Cardiovascular Risk in Rheumatoid Arthritis. Front. Med. 2018, 5, 24. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Smeeth, L.; Douglas, I.; Hall, A.J.; Hubbard, R.; Evans, S. Effect of statins on a wide range of health outcomes: A cohort study validated by comparison with randomized trials. Br. J. Clin. Pharm. 2009, 67, 99–109. [Google Scholar] [CrossRef] [Green Version]
- Kwak, B.; Mulhaupt, F.; Myit, S.; Mach, F. Statins as a newly recognized type of immunomodulator. Nat. Med. 2000, 6, 1399–1402. [Google Scholar] [CrossRef] [PubMed]
- Noel, B. Lupus erythematosus and other autoimmune diseases related to statin therapy: A systematic review. J. Eur. Acad. Derm. Venereol. 2007, 21, 17–24. [Google Scholar] [CrossRef] [PubMed]
- Araki, Y.; Mimura, T. The Mechanisms Underlying Chronic Inflammation in Rheumatoid Arthritis from the Perspective of the Epigenetic Landscape. J. Immunol. Res. 2016, 2016, 6290682. [Google Scholar] [CrossRef] [Green Version]
- De Jong, H.J.I.; Cohen Tervaert, J.W.; Lalmohamed, A.; de Vries, F.; Vandebriel, R.J.; van Loveren, H.; Klungel, O.H.; van Staa, T.P. Pattern of risks of rheumatoid arthritis among patients using statins: A cohort study with the clinical practice research datalink. PLoS ONE 2018, 13, e0193297. [Google Scholar] [CrossRef] [Green Version]
- Jick, S.S.; Choi, H.; Li, L.; McInnes, I.B.; Sattar, N. Hyperlipidaemia, statin use and the risk of developing rheumatoid arthritis. Ann. Rheum. Dis. 2009, 68, 546–551. [Google Scholar] [CrossRef]
- De Jong, H.J.; Klungel, O.H.; van Dijk, L.; Vandebriel, R.J.; Leufkens, H.G.; van der Laan, J.W.; Cohen Tervaert, J.W.; van Loveren, H. Use of statins is associated with an increased risk of rheumatoid arthritis. Ann. Rheum. Dis. 2012, 71, 648–654. [Google Scholar] [CrossRef]
- Chodick, G.; Amital, H.; Shalem, Y.; Kokia, E.; Heymann, A.D.; Porath, A.; Shalev, V. Persistence with statins and onset of rheumatoid arthritis: A population-based cohort study. PLoS Med. 2010, 7, e1000336. [Google Scholar] [CrossRef] [Green Version]
- Peterson, M.N.; Dykhoff, H.J.; Crowson, C.S.; Davis, J.M., 3rd; Sangaralingham, L.R.; Myasoedova, E. Risk of rheumatoid arthritis diagnosis in statin users in a large nationwide US study. Arthritis Res. Ther. 2021, 23, 244. [Google Scholar] [CrossRef] [PubMed]
- Tascilar, K.; Dell’Aniello, S.; Hudson, M.; Suissa, S. Statins and Risk of Rheumatoid Arthritis: A Nested Case-Control Study. Arthritis Rheumatol. 2016, 68, 2603–2611. [Google Scholar] [CrossRef] [PubMed]
- Myasoedova, E.; Karmacharya, P.; Duarte-Garcia, A.; Davis, J.M., 3rd; Murad, M.H.; Crowson, C.S. Effect of statin use on the risk of rheumatoid arthritis: A systematic review and meta-analysis. Semin. Arthritis Rheum. 2020, 50, 1348–1356. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.Y.; Min, C.; Oh, D.J.; Choi, H.G. Tobacco Smoking and Alcohol Consumption Are Related to Benign Parotid Tumor: A Nested Case-Control Study Using a National Health Screening Cohort. Clin. Exp. Otorhinolaryngol. 2019, 12, 412–419. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pratt, A.G.; Lendrem, D.; Hargreaves, B.; Aslam, O.; Galloway, J.B.; Isaacs, J.D. Components of treatment delay in rheumatoid arthritis differ according to autoantibody status: Validation of a single-centre observation using national audit data. Rheumatology 2016, 55, 1843–1848. [Google Scholar] [CrossRef] [Green Version]
- Orkaby, A.R.; Driver, J.A.; Ho, Y.L.; Lu, B.; Costa, L.; Honerlaw, J.; Galloway, A.; Vassy, J.L.; Forman, D.E.; Gaziano, J.M.; et al. Association of Statin Use With All-Cause and Cardiovascular Mortality in US Veterans 75 Years and Older. JAMA 2020, 324, 68–78. [Google Scholar] [CrossRef]
- Schmidt, T.; Battafarano, D.F.; Mortensen, E.M.; Frei, C.R.; Mansi, I. Frequency of development of connective tissue disease in statin-users versus nonusers. Am. J. Cardiol. 2013, 112, 883–888. [Google Scholar] [CrossRef] [Green Version]
- Cho, S.K.; Sung, Y.K.; Choi, C.B.; Kwon, J.M.; Lee, E.K.; Bae, S.C. Development of an algorithm for identifying rheumatoid arthritis in the Korean National Health Insurance claims database. Rheumatol. Int. 2013, 33, 2985–2992. [Google Scholar] [CrossRef]
- Kim, S.Y.; Min, C.; Oh, D.J.; Choi, H.G. Bidirectional Association Between GERD and Asthma: Two Longitudinal Follow-Up Studies Using a National Sample Cohort. J. Allergy Clin. Immunol. Pract. 2020, 8, 1005–1013.e9. [Google Scholar] [CrossRef]
- Austin, P.C. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat. Med. 2009, 28, 3083–3107. [Google Scholar] [CrossRef] [Green Version]
- Thomas, L.E.; Li, F.; Pencina, M.J. Overlap Weighting: A Propensity Score Method That Mimics Attributes of a Randomized Clinical Trial. JAMA 2020, 323, 2417–2418. [Google Scholar] [CrossRef] [PubMed]
- Furukawa, H.; Oka, S.; Shimada, K.; Hashimoto, A.; Tohma, S. Human leukocyte antigen polymorphisms and personalized medicine for rheumatoid arthritis. J. Hum. Genet. 2015, 60, 691–696. [Google Scholar] [CrossRef] [PubMed]
- Lubbers, J.; Vosslamber, S.; van de Stadt, L.A.; van Beers-Tas, M.; Wesseling, J.G.; von Blomberg, B.M.; Witte, B.I.; Bontkes, H.J.; van Schaardenburg, D.; Verweij, C.L. B cell signature contributes to the prediction of RA development in patients with arthralgia. Ann. Rheum. Dis. 2015, 74, 1786–1788. [Google Scholar] [CrossRef] [PubMed]
- Van Boheemen, L.; Turk, S.; Beers-Tas, M.V.; Bos, W.; Marsman, D.; Griep, E.N.; Starmans-Kool, M.; Popa, C.D.; van Sijl, A.; Boers, M.; et al. Atorvastatin is unlikely to prevent rheumatoid arthritis in high risk individuals: Results from the prematurely stopped STAtins to Prevent Rheumatoid Arthritis (STAPRA) trial. RMD Open 2021, 7, e001591. [Google Scholar] [CrossRef] [PubMed]
- Hippisley-Cox, J.; Coupland, C. Unintended effects of statins in men and women in England and Wales: Population based cohort study using the QResearch database. BMJ 2010, 340, c2197. [Google Scholar] [CrossRef] [Green Version]
- Spah, F. Inflammation in atherosclerosis and psoriasis: Common pathogenic mechanisms and the potential for an integrated treatment approach. Br. J. Derm. 2008, 159 (Suppl. 2), 10–17. [Google Scholar] [CrossRef]
- McInnes, I.B.; McCarey, D.W.; Sattar, N. Do statins offer therapeutic potential in inflammatory arthritis? Ann. Rheum. Dis. 2004, 63, 1535–1537. [Google Scholar] [CrossRef]
- Chen, W.; Wang, Q.; Zhou, B.; Zhang, L.; Zhu, H. Lipid Metabolism Profiles in Rheumatic Diseases. Front. Pharm. 2021, 12, 643520. [Google Scholar] [CrossRef]
- McCarey, D.W.; McInnes, I.B.; Madhok, R.; Hampson, R.; Scherbakov, O.; Ford, I.; Capell, H.A.; Sattar, N. Trial of Atorvastatin in Rheumatoid Arthritis (TARA): Double-blind, randomised placebo-controlled trial. Lancet 2004, 363, 2015–2021. [Google Scholar] [CrossRef]
- Leung, B.P.; Sattar, N.; Crilly, A.; Prach, M.; McCarey, D.W.; Payne, H.; Madhok, R.; Campbell, C.; Gracie, J.A.; Liew, F.Y.; et al. A novel anti-inflammatory role for simvastatin in inflammatory arthritis. J. Immunol. 2003, 170, 1524–1530. [Google Scholar] [CrossRef] [Green Version]
- Kaestner, R.; Darden, M.; Lakdawalla, D. Are investments in disease prevention complements? The case of statins and health behaviors. J. Health Econ. 2014, 36, 151–163. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Baganha, F.; de Jong, R.C.M.; Peters, E.A.; Voorham, W.; Jukema, J.W.; Delibegovic, M.; de Vries, M.R.; Quax, P.H.A. Atorvastatin pleiotropically decreases intraplaque angiogenesis and intraplaque haemorrhage by inhibiting ANGPT2 release and VE-Cadherin internalization. Angiogenesis 2021, 24, 567–581. [Google Scholar] [CrossRef] [PubMed]
- Barahona-Correa, J.E.; Florez-Suarez, J.; Coral-Alvarado, P.; Mendez-Patarroyo, P.; Quintana-Lopez, G. Does healthcare regime affiliation influence the clinical outcomes of patients with rheumatoid arthritis? Clin. Rheumatol. 2021, 40, 877–886. [Google Scholar] [CrossRef] [PubMed]



| Characteristics | before Overlap Weighting Adjustment | after Overlap Weighting Adjustment | ||||
|---|---|---|---|---|---|---|
| RA (n = 3149) | Control (n = 12,596) | SMD | RA (n = 2499) | Control (n = 2499) | SMD | |
| Age (%) | 0.00 | 0.00 | ||||
| 40–44 | 109 (3.46%) | 436 (3.46%) | 86 (3.44%) | 86 (3.44%) | ||
| 45–49 | 365 (11.59%) | 1460 (11.59%) | 289 (11.58%) | 289 (11.58%) | ||
| 50–54 | 682 (21.66%) | 2728 (21.66%) | 541 (21.67%) | 541 (21.67%) | ||
| 55–59 | 591 (18.77%) | 2364 (18.77%) | 470 (18.79%) | 470 (18.79%) | ||
| 60–64 | 552 (17.53%) | 2208 (17.53%) | 439 (17.56%) | 439 (17.56%) | ||
| 65–69 | 428 (13.59%) | 1712 (13.59%) | 340 (13.60%) | 340 (13.60%) | ||
| 70–74 | 248 (7.88%) | 992 (7.88%) | 196 (7.86%) | 196 (7.86%) | ||
| 75–79 | 134 (4.26%) | 536 (4.26%) | 106 (4.24%) | 106 (4.24%) | ||
| 80–84 | 35 (1.11%) | 140 (1.11%) | 28 (1.1%) | 28 (1.1%) | ||
| 85+ | 5 (0.16%) | 20 (0.16%) | 4 (0.16%) | 4 (0.16%) | ||
| Sex (%) | 0.00 | 0.00 | ||||
| Male | 845 (26.83%) | 3380 (26.83%) | 668 (26.72%) | 668 (26.72%) | ||
| Female | 2304 (73.17%) | 9216 (73.17%) | 1831 (73.28%) | 1831 (73.28%) | ||
| Income (%) | 0.00 | 0.00 | ||||
| 1 (lowest) | 529 (16.8%) | 2116 (16.8%) | 419 (16.76%) | 419 (16.76%) | ||
| 2 | 476 (15.12%) | 1904 (15.12%) | 379 (15.15%) | 379 (15.15%) | ||
| 3 | 541 (17.18%) | 2164 (17.18%) | 430 (17.2%) | 430 (17.2%) | ||
| 4 | 669 (21.24%) | 2676 (21.24%) | 531 (21.23%) | 531 (21.23%) | ||
| 5 (highest) | 934 (29.66%) | 3736 (29.66%) | 741 (29.66%) | 741 (29.66%) | ||
| Region of residence (%) | 0.00 | 0.00 | ||||
| Urban | 1360 (43.19%) | 5440 (43.19%) | 1080 (43.21%) | 1080 (43.21%) | ||
| Rural | 1789 (56.81%) | 7156 (56.81%) | 1419 (56.79%) | 1419 (56.79%) | ||
| Obesity † (%) | 0.05 | 0.00 | ||||
| Underweight | 61 (1.94%) | 283 (2.25%) | 50 (1.98%) | 50 (1.98%) | ||
| Normal | 1201 (38.14%) | 4567 (36.26%) | 943 (37.75%) | 943 (37.75%) | ||
| Overweight | 826 (26.23%) | 3360 (26.68%) | 658 (26.31%) | 658 (26.31%) | ||
| Obese I | 970 (30.8%) | 3974 (31.55%) | 775 (31.01%) | 775 (31.01%) | ||
| Obese II | 91 (2.89%) | 412 (3.27%) | 74 (2.95%) | 74 (2.95%) | ||
| Smoking status (%) | 0.04 | 0.00 | ||||
| Nonsmoker | 2585 (82.09%) | 10,494 (83.31%) | 2061 (82.46%) | 2061 (82.46%) | ||
| Past smoker | 217 (6.89%) | 770 (6.11%) | 167 (6.67%) | 167 (6.67%) | ||
| Current smoker | 347 (11.02%) | 1332 (10.57%) | 272 (10.87%) | 272 (10.87%) | ||
| Alcohol consumption (%) | 0.05 | 0.00 | ||||
| <1 time a week | 2537 (80.57%) | 9883 (78.46%) | 2004 (80.21%) | 2004 (80.21%) | ||
| ≥1 time a week | 612 (19.43%) | 2713 (21.54%) | 495 (19.79%) | 495 (19.79%) | ||
| SBP (Mean, SD) | 125.13 (16·37) | 126.10 (17.48) | 0.06 | 125.30 (14.60) | 125.30 (7.67) | 0.00 |
| DBP (Mean, SD) | 77.52 (10.79) | 78.08 (11.05) | 0.05 | 77.62 (9.61) | 77.62 (4.87) | 0.00 |
| FBG (Mean, SD) | 96.85 (27.20) | 99.37 (29.65) | 0.03 | 97.30 (25.12) | 97.30 (11.03) | 0.00 |
| Total cholesterol (Mean, SD) | 200.62 (38.09) | 201.91 (38.70) | 0.09 | 200.87 (33.93) | 200.87 (17.12) | 0.00 |
| Hemoglobin (Mean, SD) | 13.22 (1.42) | 13.37 (1.41) | 0.11 | 13.25 (1.26) | 13.25 (0.64) | 0.00 |
| CCI score (Mean, SD) | 0.92 (1.52) | 0·66 (1.40) | 0.04 | 0.71 (1.33) | 0.71 (0.65) | 0.00 |
| Dyslipidemia history (%) | 1553 (49.32%) | 5598 (44.44%) | 0.1 | 1207 (48.32%) | 1207 (48.32%) | 0.00 |
| Any statin (%) | 0.04 | 0.03 | ||||
| <90 days | 2818 (88.49%) | 11,247 (89.29%) | 2239 (89.59%) | 2217 (88.71%) | ||
| 90–365 days | 182 (5.78%) | 612 (4.86%) | 143 (5.73%) | 127 (5.09%) | ||
| >365 days | 149 (4.73%) | 737 (5.85%) | 117 (4.67%) | 155 (6.20%) | ||
| Lipophilic statin (%) | 0.02 | 0.01 | ||||
| <90 days | 2864 (90.95%) | 11,391 (90.43%) | 2278 (91.03%) | 2247 (89.92%) | ||
| 90–365 days | 162 (5.14%) | 586 (4.65%) | 128 (5.11%) | 122 (4.87%) | ||
| >365 days | 123 (3.91%) | 619 (4·91%) | 96 (3.86%) | 130 (5.21%) | ||
| Hydrophilic statin (%) | 0.00 | 0.01 | ||||
| <90 days | 3092 (98.19%) | 12,379 (98.28%) | 2455 (98.23%) | 2454 (98.20%) | ||
| 90–365 days | 33 (1.05%) | 133 (1.06%) | 26 (1.02%) | 27 (1.09%) | ||
| >365 days | 24 (10.76%) | 84 (0.67%) | 19 (0.75%) | 18 (0.71%) | ||
| Characteristics | No. of RA | No. of Control | OR for RA (95% CI) | |||
|---|---|---|---|---|---|---|
| Exposure/Total (%) | Exposure/Total (%) | Crude | p Value | Overlap Weighted Model † | p Value | |
| Any statin | ||||||
| <90 days | 2818/3149 (89.5%) | 11,247/12,596 (89.3%) | 1 | 1 | ||
| 90–365 days | 182/3149 (5.8%) | 612/12,596 (4.9%) | 1.19 (1.00–1.41) | 0.049 * | 1.11 (0.96–1.28) | 0.173 |
| >365 days | 149/3149 (4.7%) | 737/12,596 (5.9%) | 0.81 (0.67–0.97) | 0.020 * | 0.73 (0.63–0.85) | <0.001 * |
| Lipophilic statin | ||||||
| <90 days | 2864/3149 (90.9%) | 11,391/12,596 (90.4%) | 1 | 1 | ||
| 90–365 days | 162/3149 (5.1%) | 586/12,596 (4.7%) | 1.10 (0.92–1.31) | 0.298 | 1.02 (0.88–1.19) | 0.774 |
| >365 days | 123/3149 (3.9%) | 619/12,596 (4.9%) | 0.79 (0.65–0.96) | 0.020 * | 0.71 (0.61–0.84) | <0.001 * |
| Hydrophilic statin | ||||||
| <90 days | 3092/3149 (98.2%) | 12,379/12,596 (98.3%) | 1 | 1 | ||
| 90–365 days | 33/3149 (1.0%) | 133/12,596 (1.1%) | 0.99 (0.68–1.46) | 0.973 | 0.94 (0.69–1.28) | 0.695 |
| >365 days | 24/3149 (0.8%) | 84/12,596 (0.7%) | 1.14 (0.73–1.80) | 0.563 | 1.05 (0.73–1.52) | 0.788 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kwon, M.J.; Kim, J.-H.; Kim, J.H.; Park, H.-R.; Kim, N.Y.; Hong, S.; Choi, H.G. Incident Rheumatoid Arthritis Following Statin Use: From the View of a National Cohort Study in Korea. J. Pers. Med. 2022, 12, 559. https://doi.org/10.3390/jpm12040559
Kwon MJ, Kim J-H, Kim JH, Park H-R, Kim NY, Hong S, Choi HG. Incident Rheumatoid Arthritis Following Statin Use: From the View of a National Cohort Study in Korea. Journal of Personalized Medicine. 2022; 12(4):559. https://doi.org/10.3390/jpm12040559
Chicago/Turabian StyleKwon, Mi Jung, Joo-Hee Kim, Ji Hee Kim, Hye-Rim Park, Nan Young Kim, Sangkyoon Hong, and Hyo Geun Choi. 2022. "Incident Rheumatoid Arthritis Following Statin Use: From the View of a National Cohort Study in Korea" Journal of Personalized Medicine 12, no. 4: 559. https://doi.org/10.3390/jpm12040559
APA StyleKwon, M. J., Kim, J. -H., Kim, J. H., Park, H. -R., Kim, N. Y., Hong, S., & Choi, H. G. (2022). Incident Rheumatoid Arthritis Following Statin Use: From the View of a National Cohort Study in Korea. Journal of Personalized Medicine, 12(4), 559. https://doi.org/10.3390/jpm12040559