A Review of the Lidocaine in the Perioperative Period
Abstract
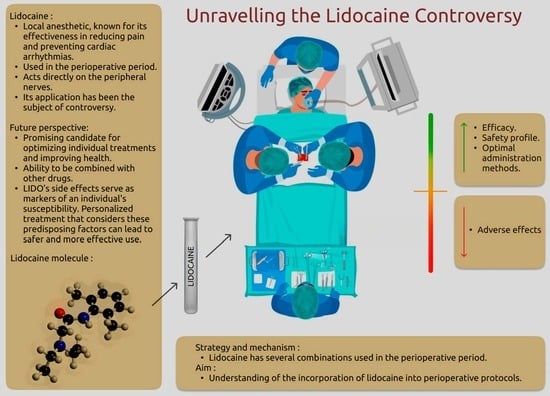
:1. Introduction
2. Initial Strategy
3. Pharmacology and Mechanism of Action
4. Adverse Effects
5. Combinations with LIDO
6. Interests with LIDO
7. Future of LIDO in Personalized Medicine
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Gordh, T.; Gordh, T.E.; Lindqvist, K.; Warner, D.S. LIDO: The origin of a modern local anesthetic. Anesthesiology 2010, 113, 1433–1437. [Google Scholar] [CrossRef] [PubMed]
- Beaussier, M.; Delbos, A.; Maurice-Szamburski, A.; Ecoffey, C.; Mercadal, L. Perioperative use of intravenous LIDO. Drugs 2018, 78, 1229–1246. [Google Scholar] [CrossRef] [PubMed]
- Voute, M.; Morel, V.; Pickering, G. Topical LIDO for chronic pain treatment. Drug Des. Dev. Ther. 2021, 15, 4091–4103. [Google Scholar] [CrossRef]
- Karnina, R.; Arif, S.K.; Hatta, M.; Bukhari, A. Molecular mechanisms of LIDO. Ann. Med. Surg. 2021, 69, 102733. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://pubchem.ncbi.nlm.nih.gov/compound/Lidocaine (accessed on 13 August 2023).
- Beecham, G.B.; Nessel, T.A.; Goyal, A. LIDO; StatPearls Publishing: St. Petersburg, FL, USA, 2022. [Google Scholar]
- Available online: https://www.uspharmacist.com/article/morphine-sulfate-swish-and-swallow-44276 (accessed on 15 August 2023).
- Wall, J.; Dhesi, J.; Snowden, C.; Swart, M. Perioperative medicine. Future Health J. 2022, 9, 138–143. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://www.longdom.org/scholarly/perioperative-care-journals-articles-ppts-list-1504.html (accessed on 25 October 2023).
- Doleman, B.; Leonardi-Bee, J.; Heinink, T.P.; Bhattacharjee, D.; Lund, J.N.; Williams, J.P. Pre-emptive and preventive opioids for postoperative pain in adults undergoing all types of surgery. Cochrane Libr. 2018, 2018, CD012624. [Google Scholar] [CrossRef] [PubMed]
- Torp, K.D.; Metheny, E.; Simon, L.V. LIDO Toxicity; StatPearls Publishing: St. Petersburg, FL, USA, 2022. [Google Scholar]
- Daraz, Y.M.; Abdelghffar, O.H. LIDO infusion: An antiarrhythmic with neurologic toxicities. Cureus 2022, 14, e23310. [Google Scholar]
- Zhang, T.; Leng, J.; Liu, Y. Deep learning for drug-drug interaction extraction from the literature: A review. Brief. Bioinform. 2020, 21, 1609–1627. [Google Scholar] [CrossRef]
- Roblek, T.; Vaupotic, T.; Mrhar, A.; Lainscak, M. Drug-drug interaction software in clinical practice: A systematic review. Eur. J. Clin. Pharmacol. 2015, 71, 131–142. [Google Scholar] [CrossRef]
- Chee, B.W.; Berlin, R.; Schatz, B. Predicting adverse drug events from personal health messages. In AMIA Annual Symposium Proceedings; American Medical Informatics Association: Washington, DC, USA, 2011; pp. 217–226. [Google Scholar]
- Aronson, J.K. Classifying drug interactions. Br. J. Clin. Pharmacol. 2004, 58, 343–344. [Google Scholar] [CrossRef]
- Chia, P.A.; Cannesson, M.; Bui, C.C.M. Opioid free anesthesia: Feasible? Curr. Opin. Anaesthesiol. 2020, 33, 512–517. [Google Scholar] [CrossRef] [PubMed]
- Electronic Medicines Compendium. Available online: https://www.medicines.org.uk/emc/product/290/pil#gref (accessed on 24 October 2023).
- Becker, D.E.; Reed, K.L. Essentials of local anesthetic pharmacology. Anesth. Prog. 2006, 53, 98–109. [Google Scholar] [CrossRef] [PubMed]
- Becker, D.E.; Reed, K.L. Local anesthetics: Review of pharmacological considerations. Anesth. Prog. 2012, 59, 90–102. [Google Scholar] [CrossRef] [PubMed]
- Kumari, S.; Carmona, A.V.; Tiwari, A.K.; Trippier, P.C. Amide bond bioisosteres: Strategies, synthesis, and successes. J. Med. Chem. 2020, 63, 12290–12358. [Google Scholar] [CrossRef]
- Yang, X.; Wei, X.; Mu, Y.; Li, Q.; Liu, J. A review of the mechanism of the central analgesic effect of LIDO. Medicine 2020, 99, e19898. [Google Scholar] [CrossRef] [PubMed]
- Hermanns, H.; Hollmann, M.W.; Stevens, M.F.; Lirk, P.; Brandenburger, T.; Piegeler, T.; Werdehausen, R. Molecular mechanisms of action of systemic LIDO in acute and chronic pain: A narrative review. Br. J. Anaesth. 2019, 123, 335–349. [Google Scholar] [CrossRef]
- Bernatoniene, J.; Sciupokas, A.; Kopustinskiene, D.M.; Petrikonis, K. Novel drug targets and emerging pharmacotherapies in neuropathic pain. Pharmaceutics 2023, 15, 1799. [Google Scholar] [CrossRef]
- Chemistry 212 Laboratory Synthesis of LIDO. Available online: https://www.cerritos.edu/chemistry/chem_212/Documents/Lab/10_lidocaine.pdf (accessed on 15 August 2023).
- The 2-Step Synthesis of LIDO Review. Available online: https://people.chem.umass.edu/mcdaniel/CHEM-267/Experiments/Lidocaine.pdf (accessed on 15 August 2023).
- Narang, P.K.; Crouthamel, W.G.; Carliner, N.H.; Fisher, M.L. Lidocaine and its active metabolites. Clin. Pharmacol. Ther. 1978, 24, 654–662. [Google Scholar] [CrossRef]
- INDICE.eu—Toda a Saúde. Available online: https://www.indice.eu/pt/medicamentos/DCI/lidocaina/informacao-geral (accessed on 20 September 2023).
- Tua Saúde. Available online: https://www.tuasaude.com/cloridrato-de-lidocaina/ (accessed on 17 August 2023).
- Estratégia de Uso da Lidocaína nos Hospitais. Available online: https://www.bing.com/search?q=estrat%C3%A9gia+de+uso+da+lidoca%C3%ADna+nos+hospitais&toWww=1&redig=A09E9E33ACEB4354BF0D3DF00287397D (accessed on 20 September 2023).
- CardioPapers. Available online: https://cardiopapers.com.br/bulario-lidocaina/ (accessed on 22 August 2023).
- Silva, G.H.; Combat, A.R.; Cesar, T.Z.; Cesar, T.Z. Lidocaine: Analysis of the intravenous use to mitigate the cardiovascular reflexes of laryngoscopy and tracheal intubation. RMMG 2015, 25, 17–20. [Google Scholar] [CrossRef]
- Scioli Montoto, S.; Ruiz, M.E. Intravenous Bolus and Infusion. The ADME Encyclopedia 2022; Springer International Publishing: New York, NY, USA, 2022; pp. 582–591. [Google Scholar]
- Dunn, L.K.; Durieux, M.E. Perioperative use of intravenous lidocaine. Anesthesiology 2017, 126, 729–737. [Google Scholar] [CrossRef]
- EH-Haj, B.M. Metabolic N-dealkylation and N-oxidation are elucidators of alkylamino moieties’ role in drugs acting at various receptors. Molecules 2021, 26, 1917. [Google Scholar] [CrossRef] [PubMed]
- Maloney, J.; Pew, S.; Wie, C.; Gupta, R.; Freeman, J.; Strand, N. Comprehensive review of topical analgesics for chronic pain. Curr. Pain Headache Rep. 2021, 25, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Anesthesia Key. Available online: https://aneskey.com/common-nerve-blocks/ (accessed on 29 August 2023).
- Reichel, C.; Skodra, T.; Nacke, A.; Spengler, U.; Sauerbruch, T. The lignocaine metabolite (MEGX) liver function test and P-450 induction in humans: MEGX test and P-450 induction. Br. J. Clin. Pharmacol. 1998, 46, 535–539. [Google Scholar] [CrossRef] [PubMed]
- Dickey, E.J.; McKenzie, H.C.; Brown, K.A.; de Solis, C.N. Serum concentrations of LIDO and its metabolites after prolonged infusion in healthy horses. Equine Vet. J. 2008, 40, 348–352. [Google Scholar] [CrossRef]
- Taylor, A.; McLeod, G. Basic pharmacology of local anesthetics. BJA Educ. 2020, 20, 34–41. [Google Scholar] [CrossRef]
- Jafri, M.S. Mechanisms of myofascial pain. Int. Sch. Res. Not. 2014, 2014, 1–16. [Google Scholar] [CrossRef]
- Louizos, C.; Yáñez, J.A.; Forrest, L.; Davies, N.M. Understanding the hysteresis loop conundrum in pharmacokinetic/pharmacodynamic relationships. J. Pharm. Pharm. Sci. Publ. Can. Soc. Pharm. Sci. Soc. Can. Sci. Pharm. 2014, 17, 34. [Google Scholar] [CrossRef]
- Tsuchiya, H. Local anesthetic failure associated with inflammation: Verification of the acidosis mechanism and the hypothetic participation of inflammatory peroxynitrite. J. Inflamm. Res. 2008, 1, 41. [Google Scholar] [CrossRef]
- Available online: https://www.drugs.com/pro/lidocaine-and-dextrose-intraspinal.html (accessed on 22 August 2023).
- Nelson, M.; Pal, N.; Tran, B. Perioperative LIDO infusions and pain measurements: Effect size matters. Anesth. Analg. 2023, 137, e24. [Google Scholar] [CrossRef]
- van Saet, A.; Tibboel, D. The influence of cardiopulmonary bypass on pediatric pharmacokinetics. Expert Opin. Drug Metab. Toxicol. 2023, 19, 333–344. [Google Scholar] [CrossRef]
- Imran, E.; Moeen, F.; Abbas, B.; Yaqoob, B.; Wajahat, M.; Khan, Q.; Khurshid, Z. Comparative analysis of different local anesthetic solutions available in market: An in vitro and clinical study. Eur. J. Dent. 2021, 15, 660–668. [Google Scholar] [CrossRef] [PubMed]
- Burm, A.G.L. Clinical pharmacokinetics of epidural and spinal anaesthesia. Clin. Pharmacokinet. 1989, 16, 283–311. [Google Scholar] [CrossRef] [PubMed]
- DailyMed. Available online: https://dailymed.nlm.nih.gov/dailymed/fda/fdaDrugXsl.cfm?setid=d1509740-f9f1-44e3-8fde-51d8683fcd87&type=display (accessed on 22 August 2023).
- Bajwa, M.S.; Bashir, M.M.; Bajwa, M.H.; Iqbal, Z.; Salahuddin, M.A.; Hussain, A.; Shahzad, F. How long to wait after local infiltration anaesthesia: Systematic review. BJS Open. 2023, 7, zrad089. [Google Scholar] [CrossRef]
- Wang, J.; Ou, S.-W.; Wang, Y.-J. Distribution and function of voltage-gated sodium channels in the nervous system. Channels 2017, 11, 534–554. [Google Scholar] [CrossRef] [PubMed]
- Bennett, D.L.; Clark, A.J.; Huang, J.; Waxman, S.G.; Dib-Hajj, S.D. The role of voltage-gated sodium channels in pain signaling. Physiol. Rev. 2019, 99, 1079–1151. [Google Scholar] [CrossRef] [PubMed]
- Abram, S.E.; Yaksh, T.L. Systemic lidocaine blocks nerve injury-induced hyperalgesia and nociceptor-driven spinal sensitization in the rat. Anesthesiology 1994, 80, 383–391, discussion 25A. [Google Scholar] [CrossRef]
- Du, X.; Gamper, N. Potassium channels in peripheral pain pathways: Expression, function and therapeutic potential. Curr. Neuropharmacol. 2013, 11, 621–640. [Google Scholar] [CrossRef]
- Smith, P.A. K+ channels in primary afferents and their role in nerve injury-induced pain. Front. Cell Neurosci. 2020, 14, 566418. [Google Scholar] [CrossRef]
- Abele, K.; Yang, J. Regulation of voltage-gated calcium channels by proteolysis. Physiol. Sin. 2012, 64, 504–514. [Google Scholar]
- Bentham Science Publisher Bentham Science Publisher. Pharmacological inhibition of voltage-gated Ca2+ channels for chronic pain relief. Curr. Neuropharmacol. 2013, 11, 606–620. [Google Scholar] [CrossRef]
- Patapoutian, A.; Tate, S.; Woolf, C.J. Transient receptor potential channels: Targeting pain at the source. Nature Reviews. Drug Discov. 2009, 8, 55–68. [Google Scholar] [CrossRef]
- Mickle, A.D.; Shepherd, A.J.; Mohapatra, D.P. Sensory TRP Channels. Prog. Mol. Biol. Transl. Sci. 2015, 131, 73–118. [Google Scholar]
- Chang, X.; Wang, J.; Jiang, H.; Shi, L.; Xie, J. Hyperpolarization-activated cyclic nucleotide-gated channels: An emerging role in neurodegenerative diseases. Front. Mol. Neurosci. 2019, 12, 141. [Google Scholar] [CrossRef]
- Kweon, H.J.; Suh, B.C. Acid-sensing ion channels (ASICs): Therapeutic targets for neurological diseases and their regulation. BMB Rep. 2013, 46, 295–304. [Google Scholar] [CrossRef] [PubMed]
- Liapakis, G.; Cordomi, A.; Pardo, L. The G-protein coupled receptor family: Actors with many faces. Curr. Pharm. Des. 2012, 18, 175–185. [Google Scholar] [CrossRef] [PubMed]
- Unwin, N. Nicotinic acetylcholine receptor and the structural basis of neuromuscular transmission: Insights. Torpedopostsynaptic membranes. Q. Rev. Biophys. 2013, 46, 283–322. [Google Scholar] [CrossRef]
- Bardin, L. The complex role of serotonin and 5-HT receptors in chronic pain. Behav. Pharmacol. 2011, 22, 390–404. [Google Scholar] [CrossRef]
- Okura, D.; Horishita, T.; Ueno, S.; Yanagihara, N.; Sudo, Y.; Uezono, Y.; Minami, T.; Kawasaki, T.; Sata, T. Lidocaine preferentially inhibits the function of purinergic P2X7 receptors expressed in Xenopus oocytes. Anesth. Analg. 2015, 120, 597–605. [Google Scholar] [CrossRef]
- Kumar, H.; Kawai, T.; Akira, S. Toll-like receptors and innate immunity. Biochem. Biophys. Res. Commun. 2009, 388, 621–625. [Google Scholar] [CrossRef] [PubMed]
- Bista, Imlach. Pathological mechanisms and therapeutic targets for trigeminal neuropathic pain. Medicines 2019, 6, 91. [Google Scholar] [CrossRef]
- Gallagher, C.I.; Ha, D.A.; Harvey, R.J.; Vandenberg, R.J. Positive allosteric modulators of Glycine receptors and their potential use in pain therapies. Pharmacol. Rev. 2022, 74, 933–961. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.-H.; Tsai, P.-S.; Kai, Y.-F.; Yang, C.-H.; Huang, C.-J. Lidocaine inhibition of inducible nitric oxide synthase and cationic amino acid transporter-2 transcription in activated Murine macrophages may involve voltage-sensitive Na+ channels. Anesth. Analg. 2006, 102, 1739–1744. [Google Scholar] [CrossRef] [PubMed]
- El-Boghdadly, K.; Pawa, A.; Chin, K.J. Local anesthetic systemic toxicity: Current perspectives. Local Reg. Anesth. 2018, 11, 35–44. [Google Scholar] [CrossRef]
- Koo, C.H.; Shin, H.J.; Han, S.H.; Ryu, J.H. LIDO vs. Other local anesthetics in the development of transient neurologic symptoms (TNS) following spinal anesthesia: A meta-analysis of randomized controlled trials. J. Clin. Med. 2020, 9, 493. [Google Scholar] [CrossRef] [PubMed]
- Bahar, E.; Yoon, H. LIDO: A local anesthetic, its adverse effects and management. Medicine 2021, 57, 782. [Google Scholar]
- Lidocaine Hydrochloride and EPINEPHrine Injection USP. Available online: https://pdf.hres.ca/dpd_pm/00065511.PDF (accessed on 23 August 2023).
- Rademaker, A.W.; Kellen, J.; Tam, Y.K.; Wyse, D.G. Character of adverse effects of prophylactic LIDO in the coronary care unit. Clin. Pharmacol. Ther. 1986, 40, 71–80. [Google Scholar] [CrossRef]
- LIDO Side Effects. Available online: https://www.drugs.com/sfx/lidocaine-side-effects.html (accessed on 22 August 2023).
- Adamsen, S.; Vargo, J.J. Propofol and lidocaine for ERCP: Two is better than one? Gastrointest. Endosc. 2020, 92, 308–309. [Google Scholar] [CrossRef]
- Forster, C.; Vanhaudenhuyse, A.; Gast, P.; Louis, E.; Hick, G.; Brichant, J.F.; Joris, J. Intravenous infusion of lidocaine significantly reduces propofol dose for colonoscopy: A randomized placebo-controlled study. Br. J. Anaesth. 2018, 121, 1059–1064. [Google Scholar] [CrossRef]
- Cherobin, A.C.F.P.; Tavares, G.T. Safety of local anesthetics. An. Bras. Dermatol. 2020, 95, 82–90. [Google Scholar] [CrossRef]
- Knapp, A.B. The cimetidine-lidocaine interaction. Ann. Intern. Med. 1983, 98, 174. [Google Scholar] [CrossRef]
- Shibasaki, S.; Kawamata, Y.; Ueno, F.; Koyama, C.; Itho, H.; Nishigaki, R.; Umemura, K. Effects of cimetidine on lidocaine distribution in rats. J. Pharmacobio-Dyn. 1988, 11, 785–793. [Google Scholar] [CrossRef]
- Feely, J. Increased toxicity and reduced clearance of lidocaine by cimetidine. Ann. Intern. Med. 1982, 96, 592. [Google Scholar] [CrossRef]
- Bosco, F.A.P.; Braz, J.R.C. Beta-bloqueadores em anestesiologia: Aspectos farmacológicos e clínicos. Rev. Bras. De Anestesiol. 2001, 51, 431–447. [Google Scholar] [CrossRef]
- Lidocaine. Available online: https://go.drugbank.com/drugs/DB00281 (accessed on 13 September 2023).
- Kwon, S.; Sevick-Muraca, E.M. Effect of LIDO with and without epinephrine on lymphatic contractile activity in mice in vivo. J. Anesth. 2016, 30, 1091–1094. [Google Scholar] [CrossRef]
- dos Reis Júnior, A.; Quinto, D. Digital block with or without the addition of epinephrine in the anesthetic solution. Braz. J. Anesthesiol. 2016, 66, 63–71. [Google Scholar] [CrossRef] [PubMed]
- Scully, C. Perioperative care. In Scully’s Medical Problems in Dentistry; Elsevier: Amsterdam, The Netherlands, 2014; pp. 51–96. [Google Scholar]
- Eletronics Medicine Compendium. Available online: https://www.medicines.org.uk/emc/product/2397/smpc (accessed on 23 August 2023).
- Carr, A.; Ferguson, M. What is the evidence to support clonidine as an adjuvant analgesic? Pract. Pain. Manag. 2019, 19, 1. [Google Scholar]
- Pöpping, D.M.; Elia, N.; Marret, E.; Wenk, M.; Tramèr, M.R.; Warner, D.S.; Warner, M.A. Clonidine as an adjuvant to local anesthetics for peripheral nerve and plexus blocks. Anesthesiology 2009, 111, 406–415. [Google Scholar] [CrossRef] [PubMed]
- DrugBank. Available online: https://go.drugbank.com/drugs/DB01232 (accessed on 13 September 2023).
- National HIV Curriculum. Available online: https://www.hiv.uw.edu/page/treatment/drugs/saquinavir (accessed on 13 September 2023).
- Available online: https://www.drugs.com/interactions-check.php?drug_list=434-0,1464-0 (accessed on 13 September 2023).
- Berksun, H.; Akpek, E.A.; Arslan, G. Methemoglobin levels during epidural anesthesia for renal transplantation--comparison of prilocaine with bupivacaine. Middle East J. Anesthesiol. 2008, 19, 997–1011. [Google Scholar] [PubMed]
- Available online: https://www.drugs.com/interactions-check.php?drug_list=786-0,1464-0 (accessed on 14 September 2023).
- Dekkers, B.G.J.; Bierman, W.F.W.; Touw, D.J.; Alffenaar, J.-W.C. Relevance of the drug–drug interactions between lidocaine and the pharmacokinetic enhancers ritonavir and cobicistat. AIDS 2019, 33, 1100–1102. [Google Scholar] [CrossRef]
- Available online: https://www.drugs.com/interactions-check.php?drug_list=272-0,1464-0 (accessed on 14 September 2023).
- Croom, K.F.; Dhillon, S.; Keam, S.J. Atazanavir: A review of its use in the management of HIV-1 infection. Drugs 2009, 69, 1107–1140. [Google Scholar] [CrossRef]
- Chow, M.S.; Lebsack, C.; Hilleman, D. Propafenone: A new antiarrhythmic agent. Clin. Pharm. 1988, 7, 869–877. [Google Scholar] [PubMed]
- Severinghaus, J.W. Intrathecally, Caine may dis-Able. Reflections on lidocaine for spinal anesthesia. Acta Anaesthesiol. Scand. 1998, 113, 3–7. [Google Scholar] [CrossRef] [PubMed]
- Gaiser, R.R. Should intrathecal lidocaine be used in the 21st century? J. Clin. Anesth. 2000, 12, 476–481. [Google Scholar] [CrossRef] [PubMed]
- McCleane, G. Intravenous lidocaine: An outdated or underutilized treatment for pain? J. Palliat. Med. 2007, 10, 798–805. [Google Scholar] [CrossRef]
- Estebe, J.P. Intravenous lidocaine. Best Practice & Research. Clin. Anaesthesiol. 2017, 31, 513–521. [Google Scholar]
- Lee, I.W.S.; Schraag, S. The use of intravenous lidocaine in perioperative medicine: Anaesthetic, analgesic and immune-modulatory aspects. J. Clin. Med. 2022, 11, 3543. [Google Scholar] [CrossRef]
- Kim, J.H.; Kang, D.W.; Choi, G.W.; Lee, S.B.; Lee, S.; Cho, H.Y. Evaluation of lidocaine and metabolite pharmacokinetics in hyaluronic acid injection. Pharmaceutics 2021, 13, 203. [Google Scholar] [CrossRef]


| Drug Name | Drugs in Its Composition | Application Method | Concentration (%) |
|---|---|---|---|
| Lidocaine | Lidocaine | Topical | 5 |
| Lidocaine and Prilocaine | Lidocaine; Prilocaine | Topical | 2.5; 2.5 |
| Lidoderm | Lidocaine | Topical | 5 |
| Oraqix | Lidocaine; Prilocaine | Periodontal | 2.5; 2.5 |
| Pliaglis | Lidocaine; Tetracaine | Topical | 7; 7 |
| Versatis | Lidocaine | Topical | 700 mg |
| Xylocaine | Lidocaine | Topical | 5 |
| Xylocaine | Lidocaine hydrochloride | Injectable | 0.5 to 2 |
| Xylocaine | Lidocaine hydrochloride | Topical | 2 |
| Zingo | Lidocaine; Hydrochloride | Intradermal | 0.5 mg |
| ZTLIDO | Lidocaine | Topical | 1.8 |
| Type of Surgery | Bolus (mg/kg) | Infusion (mg kg−1 h−1) |
|---|---|---|
| Open abdominal | 1.5–2 | 1.5–5 |
| Laparoscopic abdominal | 1.5 | 1–2 |
| Prostate | 1.5 | 1.5–2 |
| Breast | 1.5 | 1.5–2 |
| Ambulatory | 1.5 | 2 |
| Multilevel spine | No bolus | 2 |
| Cardiac | 1–1.5 | 0.033 |
| Laparoscopic renal | 1.5 | 2 then 1.3 PO |
| Abdominal hysterectomy | 1.5 | 2–3 |
| Hip arthroplasty | 1.5 | 1.5 |
| Thoracic | No bolus | 0.033 |
| Drugs Combination with LIDO | Effect | Administration |
|---|---|---|
| Propofol | The combination resulted in a 50% reduction in propofol dose. Fatigue and pain felt after the surgery. | IV injection |
| Epinephrine | Increases the duration of action of lidocaine, prolonging its effect. | Injection |
| Antiarrhythmic (ex: Amiodarone) | The risk or severity of generalized seizure and bradycardia can be increased when amiodarone is combined with lidocaine. | IV, Oral |
| Cimetidine | Cimetidine reduces the systemic clearance of lidocaine. The absorption of lidocaine by erythrocytes is decreased by cimetidine. There is an interaction between lidocaine and cimetidine in terms of increasing lidocaine serum levels, as this may be mediated by cimetidine’s inhibition of the H2 receptor. | IV, Oral |
| Anti-hypertensive (e.g.: Beta-blockers) | This can result in bradycardia (slow heart rate) and hypotension (low blood pressure). Beta-blockers can potentiate the effects of lidocaine, increasing the duration of its action. | IV, Oral |
| Anticoagulants (e.g.: Warfarin) | The metabolism of warfarin can be decreased when combined with lidocaine. | Oral |
| Drugs Combination with LIDO | Effect |
|---|---|
| Propafenone | The serum concentration of lidocaine can be increased when it is combined with propafenone. |
| Saquinavir | The metabolism of lidocaine can be decreased when combined with saquinavir, also saquinavir can increase the blood levels of lidocaine to dangerous levels and cause an irregular heart rhythm. |
| Darunavir/Cobicistat | The metabolism of lidocaine can be decreased when these two drugs are used together. Also, these drugs can affect the rhythm of your heart and cause cardiovascular problems. |
| Atazanavir | Using these drugs can increase the effects of lidocaine and affect the rhythm of the heart. Irregular heartbeat, chest tightness, blurred vision, or nausea can be adverse effects. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Silva, A.; Mourão, J.; Vale, N. A Review of the Lidocaine in the Perioperative Period. J. Pers. Med. 2023, 13, 1699. https://doi.org/10.3390/jpm13121699
Silva A, Mourão J, Vale N. A Review of the Lidocaine in the Perioperative Period. Journal of Personalized Medicine. 2023; 13(12):1699. https://doi.org/10.3390/jpm13121699
Chicago/Turabian StyleSilva, Abigail, Joana Mourão, and Nuno Vale. 2023. "A Review of the Lidocaine in the Perioperative Period" Journal of Personalized Medicine 13, no. 12: 1699. https://doi.org/10.3390/jpm13121699
APA StyleSilva, A., Mourão, J., & Vale, N. (2023). A Review of the Lidocaine in the Perioperative Period. Journal of Personalized Medicine, 13(12), 1699. https://doi.org/10.3390/jpm13121699