Assessment of the Pharmacokinetics and Pharmacodynamics of Injectable Lidocaine and a Lidocaine-Impregnated Latex Band for Castration and Tail Docking in Lambs
Abstract
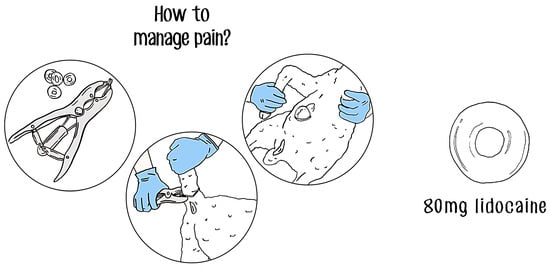
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. In Vitro Lidocaine Release from LLBs
2.2. Pharmacokinetics, Pharmacodynamics, and Effective Concentrations (EC50, EC95) of Injectable Lidocaine in Lamb Scrotal and Tail Tissue
2.3. In Vivo Delivery of Lidocaine from LLBs into Scrotal and Tail Tissues
2.4. Assessment of Tissue Lidocaine Concentrations
2.5. Assessment of Local Anesthesia in Control versus LLB-Banded Tails
2.6. Statistical Analysis
3. Results
3.1. In Vitro Lidocaine Release from LLBs
3.2. Determination of Pharmacokinetics, Pharmacodynamics, and Effective Concentrations of Injectable Lidocaine
3.3. In Vivo Delivery of Lidocaine from LLBs into Scrotal and Tail Tissues
3.4. Local Anesthesia in Control versus LLB-Banded Lambs
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- French, N.P.; Wall, R.; Morgan, K.L. Lamb tail docking: A controlled field study of the effects of tail amputation on health and productivity. Vet. Rec. 1994, 134, 463. [Google Scholar] [CrossRef] [PubMed]
- Archer, N. Differences in the acute pain responses of two breeds of lamb following castration and tail docking with the rubber ring method. Anim. Welf. 2004, 13, 135–141. [Google Scholar] [CrossRef]
- Baird, A.N.; Wolfe, D.F. Castration of normal male: Bulls, rams, and bucks. In Large Animal Urogenital Surgery; Williams & Wilkins: Baltimore, MD, USA, 1998; pp. 295–301. [Google Scholar]
- Gascoigne, E.; Mouland, C.; Lovatt, F. Considering the 3Rs for castration and tail docking in sheep. Practice 2021, 43, 152–162. [Google Scholar] [CrossRef]
- Meintjes, R.A. An overview of the physiology of pain for the veterinarian. Vet. J. 2012, 193, 344–348. [Google Scholar] [CrossRef] [PubMed]
- Mellor, D.J.; Stafford, K.J. Acute castration and/or tailing distress and it’s alleviation in lambs. N. Z. Vet. J. 2000, 48, 33–43. [Google Scholar] [CrossRef] [PubMed]
- Molony, V.; Kent, J.; Robertson, I. Behavioral responses of lambs of three ages in the first three hours after three methods of castration and tail docking. Res. Vet. Sci. 1993, 55, 236–245. [Google Scholar] [CrossRef] [PubMed]
- Kent, J.; Molony, V.; Graham, M. Comparison of methods for the reduction of acute pain produced by rubber ring castration or tail docking week-old lambs. Vet. J. 1998, 155, 39–51. [Google Scholar] [CrossRef]
- Thorton, P.D.; Waterman-Pearson, A.E. Quantification of the pain and distress responses to castration in young lambs. Res. Vet. Sci. 1999, 66, 107–118. [Google Scholar] [CrossRef]
- Kells, N.J.; Beausoleil, N.J.; Godfrey, A.J.R.; Littlewood, K.E.; Ward, R.N.; Johnson, C.B. Effect of analgesic strategies on pain behaviour associated with combined ring castration and hot iron tail docking in Merino lambs. Appl. Anim. Behav. Sci. 2019, 222, 104914. [Google Scholar] [CrossRef]
- Paull, D.R.; Small, A.H.; Lee, C.; Palladin, P.; Colditz, I.G. Evaluating a novel analgesic strategy for ring castration of ram lambs. Vet. Anaesth. Anal. 2012, 39, 539–549. [Google Scholar] [CrossRef]
- Small, A.H.; Belson, S.; Brewer, H.; Schmoelzl, S.M. Marking to weaning production aspects of lambs provided with NSAID analgesia compared with lambs receiving no analgesia at the time of elastrator ring marking. Aust. Vet. J. 2020, 99, 40–43. [Google Scholar] [CrossRef] [PubMed]
- Graham, M.J.; Kent, J.E.; Molony, V. Effects of four analgesic treatments on the behavioural and cortisol responses of 3-week-old lambs to tail docking. Vet. J. 1997, 153, 87–97. [Google Scholar] [CrossRef]
- Pollard, J.C.; Roos, V.; Littlejohn, R.P. Effects of an oral dose of acetyl salicylate at tail docking on the behaviour of lambs aged three to six weeks. Appl. Anim. Behav. Sci. 2001, 71, 29–42. [Google Scholar] [CrossRef] [PubMed]
- Cockram, M.S.; Menzies, P.; Barrett, D.; Hemsted, J. Code of Practice for the Care and Handling of Sheep: Review of Scientific Research on Priority Issues. 2012. Available online: https://www.nfacc.ca/resources/codes-of-practice/sheep/Sheep_SC_report_Oct_2012.pdf (accessed on 13 November 2023).
- Dimmitt, S.; Stampfer, H.; Martin, J.H. When less is more—Efficacy with less toxicity at the ED50. Br. J. Clin. Pharmacol. 2017, 83, 1365–1368. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, T.; Popitz-Bergez, F.; Birknes, J.; Strichartz, G.R. The critical role of concentration for lidocaine block of peripheral nerve in vivo: Studies of function and drug uptake in the rate. J. Am. Soc. Anesthesiol. 2003, 99, 1189–1197. [Google Scholar] [CrossRef] [PubMed]
- Yartsev, A. Therapeutic Index, ED50, TD50, and LD50. Deranged Physiology, Pharmacodynamics. 2015. Available online: https://derangedphysiology.com/main/cicm-primary-exam/required-reading/pharmacodynamics/Chapter%20413/therapeutic-index-ed50-td50-and-ld50 (accessed on 26 October 2023).
- Yoshida, E.T.K.; Kawaai, H.; Yamazaki, S. Lidocaine Concentration in Oral Tissue by the Addition of Epinephrine. Anesth. Prog. 2016, 63, 17–24. [Google Scholar]
- Irwin, R.J.; Hautus, M.J.; Dawson, N.J.; Welch, D.; Bayly, M.F. Discriminability of electrocutaneous stimuli after topical anesthesia: Detection-theory measurement of sensitivity to painful stimuli. Percep. Psych. 1994, 55, 125–132. [Google Scholar] [CrossRef]
- Gordh, T.; Gordh, T.E.; Lindqvist, K. Lidocaine: The origin of a modern local anesthetic. J. Am. Soc. Anesthesiol. 2010, 113, 1433–1437. [Google Scholar] [CrossRef]
- Weinberg, L.; Peake, B.; Tan, C.; Nikfarjam, M. Pharmacokinetics and pharmacodynamics of lignocaine: A review. World J. Anesthesiol. 2015, 4, 17–29. [Google Scholar] [CrossRef]
- Yang, X.; Wei, X.; Mu, Y.; Li, Q.; Liu, J. A review of the mechanism of the central analgesic effect of lidocaine. Medicine 2020, 99, e19898. [Google Scholar] [CrossRef]
- Morishima, H.O.; Finster, M.; Pedersen, H.; Fukunaga, A.; Ronfeld, R.A.; Vassallo, H.G.; Covino, B.G. Pharmacokinetics of lidocaine in fetal and neonatal lambs and adult sheep. Anesthesiology 1979, 50, 431–436. [Google Scholar] [CrossRef] [PubMed]
- Bloedow, D.C.; Ralston, D.H.; Hargrove, J.C. Lidocaine pharmacokinetics in pregnant and nonpregnant sheep. J. Pharm. Sci. 1980, 69, 32–37. [Google Scholar] [CrossRef]
- Small, A.; Fisher, A.D.; Lee, C.; Colditz, I. Analgesia for sheep in commercial production: Where to next? Animals 2021, 11, 1127. [Google Scholar] [CrossRef] [PubMed]
- National Farm Animal Care Council. Code of Practice for the Care and Handling of Sheep. 2013. Available online: https://www.nfacc.ca/pdfs/codes/sheep_code_of_practice.pdf (accessed on 26 October 2023).
- Saville, J.W.; Ross, J.A.; Trefz, T.; Schatz, C.; Matheson-Bird, H.; Ralston, B.; Granot, O.; Schmid, K.; Terry, R.; Allan, N.D.; et al. Development and field validation of lidocaine-loaded castration bands for bovine pain mitigation. Animals 2020, 10, 2363. [Google Scholar] [CrossRef]
- Fierheller, E.E.; Caulkett, N.A.; Haley, D.B.; Florence, D.; Doepel, L. Onset, duration, and efficacy of four methods of local anesthesia. Vet. Anesth. Analg. 2012, 39, 431–435. [Google Scholar] [CrossRef] [PubMed]
- Small, A.; Fetiveau, M.; Smith, R.; Colditz, I. Three studies evaluating the potential for lidocaine, bupivacaine or procaine to reduce pain-related behaviours following ring castration and/or tail docking in lambs. Animals 2021, 11, 3583. [Google Scholar] [CrossRef] [PubMed]
- Mellema, S.C.; Doherr, M.G.; Wechsler, B.; Thueer, S.; Steiner, A. Influence of local anaesthesia on pain and distress induced by two bloodless castration methods in young lambs. Vet. J. 2006, 172, 274–283. [Google Scholar] [CrossRef]
- Stewart, M.; Beausoleil, N.J.; Johnson, C.B.; Webster, J.R.; Schütz, K.E.; Cox, N.; Stafford, K.J. Do rubber rings coated with lignocaine reduce the pain associated with ring castration of lambs? Appl. Anim. Behav. Sci. 2014, 160, 56–63. [Google Scholar] [CrossRef]
- Ghadirian, S.; Vesal, N.; Maghsoudi, B.; Akhlagh, S.H. Comparison of lidocaine, lidocaine-morphine, lidocaine-tramadol or bupivacaine for neural blockade of the brachial plexus in fat-tailed lambs. Vet. Anesth. Analg. 2016, 43, 109–116. [Google Scholar] [CrossRef]
- Lizarraga, I.; Janovyak, E.; Beths, T. Comparing lidocaine, bupivacaine and a lidocaine–bupivacaine mixture as a metacarpal block in sheep. Vet. J. 2013, 197, 515–518. [Google Scholar] [CrossRef]
- Rostami, M.; Vesal, N. The effects of adding epinephrine or xylazine to lidocaine solution for lumbosacral epidural analgesia in fat-tailed sheep. J. S. Afr. Vet. Assoc. 2012, 83, 7. [Google Scholar] [CrossRef] [PubMed]
- Stafford, K.J.; Mellor, D.J.; Todd, S.E.; Bruce, R.A.; Ward, R.N. Effects of local anaesthesia or local anaesthesia plus a non-steriodal anti-inflammatory drug on the acute cortisol response of calves to five different methods of castration. Res. Vet. Sci. 2002, 73, 61–70. [Google Scholar] [CrossRef] [PubMed]
- Melendez, D.M.; Marti, S.; Pajor, E.A.; Sidhu, P.K.; Gellatly, D.; Moya, D.; Janzen, E.D.; Coetzee, J.F.; Schwartzkopf-Genswein, K.S. Effect of meloxicam and lidocaine administered alone or in combination on indicators of pain and distress during and after knife castration in weaned beef calves. PLoS ONE 2018, 13, e020. [Google Scholar] [CrossRef] [PubMed]





| Graded Response | Description of Positive Avoidance Response |
|---|---|
| 0 | No reaction |
| 1 | Slight reaction: Moves side to side and tail flick |
| 2 | Moderate reaction: Moves side to side and tail flick, slight kick, or jump |
| 3 | Severe reaction: Moves side to side and tail flick, pronounced kick or jump, bawling, head shaking, or vocalization |
| Parameter | Details |
|---|---|
| HPLC | Agilent 1100 and 1200 Series |
| Column | ZORBAX Extend-C18; 4.6 × 150 mm; 3.5 µm |
| Mobile Phase | 40:60—Acetonitrile:PBS, pH 7.4 |
| Analysis Time | 15 min |
| Flow Rate | 1.0 mL/min |
| Injection Volume | 10 µL |
| Column Temperature | 28 °C |
| Detector | Agilent G1315B Diode Array Detector (DAD) |
| Wavelength | 210 nm |
| Bandwidth | 4 nm |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ross, J.A.; Roche, S.M.; Beaugrand, K.; Schatz, C.; Hammad, A.; Ralston, B.J.; Hanson, A.M.; Allan, N.; Olson, M. Assessment of the Pharmacokinetics and Pharmacodynamics of Injectable Lidocaine and a Lidocaine-Impregnated Latex Band for Castration and Tail Docking in Lambs. Animals 2024, 14, 255. https://doi.org/10.3390/ani14020255
Ross JA, Roche SM, Beaugrand K, Schatz C, Hammad A, Ralston BJ, Hanson AM, Allan N, Olson M. Assessment of the Pharmacokinetics and Pharmacodynamics of Injectable Lidocaine and a Lidocaine-Impregnated Latex Band for Castration and Tail Docking in Lambs. Animals. 2024; 14(2):255. https://doi.org/10.3390/ani14020255
Chicago/Turabian StyleRoss, Joseph A., Steven M. Roche, Kendall Beaugrand, Crystal Schatz, Ann Hammad, Brenda J. Ralston, Andrea M. Hanson, Nicholas Allan, and Merle Olson. 2024. "Assessment of the Pharmacokinetics and Pharmacodynamics of Injectable Lidocaine and a Lidocaine-Impregnated Latex Band for Castration and Tail Docking in Lambs" Animals 14, no. 2: 255. https://doi.org/10.3390/ani14020255
APA StyleRoss, J. A., Roche, S. M., Beaugrand, K., Schatz, C., Hammad, A., Ralston, B. J., Hanson, A. M., Allan, N., & Olson, M. (2024). Assessment of the Pharmacokinetics and Pharmacodynamics of Injectable Lidocaine and a Lidocaine-Impregnated Latex Band for Castration and Tail Docking in Lambs. Animals, 14(2), 255. https://doi.org/10.3390/ani14020255