An Open-Source Android Application to Measure Anterior–Posterior Knee Translation
Abstract
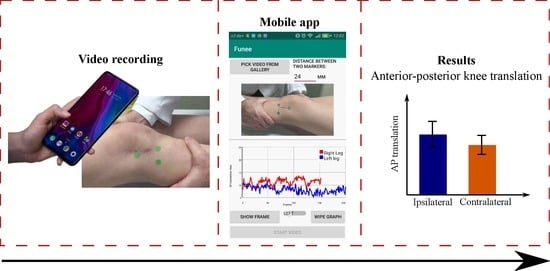
:Featured Application
Abstract
1. Introduction
2. Materials and Methods
2.1. Experimental Data
2.2. Image Processing
2.3. Calculation of the AP Translation
2.4. User Interface
2.5. Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Arastu, M.H.; Grange, S.; Twyman, R. Prevalence and consequences of delayed diagnosis of anterior cruciate ligament ruptures. Knee Surg. Sport. Traumatol. Arthrosc. 2015, 23, 1201–1205. [Google Scholar] [CrossRef] [PubMed]
- Gianotti, S.M.; Marshall, S.W.; Hume, P.A.; Bunt, L. Incidence of anterior cruciate ligament injury and other knee ligament injuries: A national population-based study. J. Sci. Med. Sport 2009, 12, 622–627. [Google Scholar] [CrossRef] [PubMed]
- Moses, B.; Orchard, J.; Orchard, J. Systematic review: Annual incidence of ACL injury and surgery in various populations. Res. Sport. Med. 2012, 20, 157–179. [Google Scholar] [CrossRef] [PubMed]
- Markolf, K.L.; Jackson, S.R.; McAllister, D.R. Relationship between the pivot shift and Lachman tests a cadaver study. J. Bone Jt. Surg. Ser. A 2010, 92, 2067–2075. [Google Scholar] [CrossRef] [PubMed]
- Kuroda, R.; Hoshino, Y.; Kubo, S.; Araki, D.; Oka, S.; Nagamune, K.; Kurosaka, M. Similarities and differences of diagnostic manual tests for anterior cruciate ligament insufficiency: A global survey and kinematics assessment. Am. J. Sports Med. 2012, 40, 91–99. [Google Scholar] [CrossRef]
- Berruto, M.; Uboldi, F.; Gala, L.; Marelli, B.; Albisetti, W. Is triaxial accelerometer reliable in the evaluation and grading of knee pivot-shift phenomenon? Knee Surg. Sport. Traumatol. Arthrosc. 2013, 21, 981–985. [Google Scholar] [CrossRef]
- Wiertsema, S.H.; van Hooff, H.J.A.; Migchelsen, L.A.A.; Steultjens, M.P.M. Reliability of the KT1000 arthrometer and the Lachman test in patients with an ACL rupture. Knee 2008, 15, 107–110. [Google Scholar] [CrossRef]
- Tashman, S.; Araki, D. Effects of ACL Reconstruction on In-Vivo, Dynamic Knee Function. Clin. Sport. Med. 2013, 32, 47–59. [Google Scholar] [CrossRef] [Green Version]
- Pulli, K.; Baksheev, A.; Kornyakov, K.; Eruhimov, V. Realtime computer vision with OpenCV. Queue 2012, 10, 1–17. [Google Scholar] [CrossRef]
- Hoshino, Y.; Araujo, P.; Irrgang, J.J.; Fu, F.H.; Musahl, V. An image analysis method to quantify the lateral pivot shift test. Knee Surg. Sport. Traumatol. Arthrosc. 2012, 20, 703–707. [Google Scholar] [CrossRef] [Green Version]
- Hoshino, Y.; Araujo, P.; Ahldén, M.; Samuelsson, K.; Muller, B.; Hofbauer, M.; Wolf, M.R.; Irrgang, J.J.; Fu, F.H.; Musahl, V. Quantitative evaluation of the pivot shift by image analysis using the iPad. Knee Surgery, Sport. Traumatol. Arthrosc. 2013, 21, 975–980. [Google Scholar] [CrossRef] [PubMed]
- van Duren, B.H.; Sugand, K.; Wescott, R.; Carrington, R.; Hart, A. Augmented reality fluoroscopy simulation of the guide-wire insertion in DHS surgery: A proof of concept study. Med. Eng. Phys. 2018, 55, 52–59. [Google Scholar] [CrossRef] [PubMed]
- Berber, T.; Alpkocak, A.; Balci, P.; Dicle, O. Breast mass contour segmentation algorithm in digital mammograms. Comput. Methods Programs Biomed. 2013, 110, 150–159. [Google Scholar] [CrossRef] [PubMed]
- Elloumi, Y.; Akil, M.; Kehtarnavaz, N. A mobile computer aided system for optic nerve head detection. Comput. Methods Programs Biomed. 2018, 162, 139–148. [Google Scholar] [CrossRef] [PubMed]
- Sedláček, M. Evaluation of RGB and HSV models in Human Faces Detection. In Proceedings of the Conference of Computer Systems and Image Processing, Budmerice, Slovak, 17 June 2004. [Google Scholar]
- Liu, Y.; Zhang, J.; Tian, J. An image localization system based on gradient Hough transform. In Proceedings of the MIPPR 2015: Remote Sensing Image Processing, Geographic Information Systems, and Other Applications; SPIE Press: Bellingham, DC, USA, 2015; Volume 9815, p. 98151F. [Google Scholar] [CrossRef]
- Della Croce, U.; Cappozzo, A.; Kerrigan, D.C. Pelvis and lower limb anatomical landmark calibration precision and its propagation to bone geometry and joint angles. Med. Biol. Eng. Comput. 1999, 37, 155–161. [Google Scholar] [CrossRef] [PubMed]
- Matsushita, T.; Oka, S.; Nagamune, K.; Matsumoto, T.; Nishizawa, Y.; Hoshino, Y.; Kubo, S.; Kurosaka, M.; Kuroda, R. Differences in knee kinematics between awake and anesthetized patients during the Lachman and pivot-shift Tests for anterior cruciate ligament deficiency. Orthop. J. Sport. Med. 2013, 1, 1–6. [Google Scholar] [CrossRef] [Green Version]
- Sundemo, D.; Alentorn-geli, E.; Hoshino, Y.; Musahl, V.; Karlsson, J.; Samuelsson, K. Objective measures on knee instability: Dynamic tests: A review of devices for assessment of dynamic knee laxity through utilization of the pivot shift test. Curr. Rev. Musculoskelet. Med. 2016, 9, 148–159. [Google Scholar] [CrossRef] [Green Version]
- Kopf, S.; Kauert, R.; Halfpaap, J.; Jung, T.; Becker, R. A new quantitative method for pivot shift grading. Knee Surg. Sport. Traumatol. Arthrosc. 2012, 20, 718–723. [Google Scholar] [CrossRef]
- Lopomo, N.; Signorelli, C.; Bonanzinga, T.; Muccioli, G.M.M.; Visani, A.; Zaffagnini, S. Quantitative assessment of pivot-shift using inertial sensors. Knee Surg. Sport. Traumatol. Arthrosc. 2012, 20, 713–717. [Google Scholar] [CrossRef]
- Freedman, V.A.; Spillman, B.C. Validation of a Method for Combining Biplanar Radiography and Magnetic Resonance Imaging to Estimate Knee Cartilage Contact. Med. Eng. Phys. 2015, 37, 937–947. [Google Scholar] [CrossRef]
- Moewis, P.; Boeth, H.; Heller, M.O.; Yntema, C.; Jung, T.; Doyscher, R.; Ehrig, R.M.; Zhong, Y.; Taylor, W.R. Towards understanding knee joint laxity: Errors in non-invasive assessment of joint rotation can be corrected. Med. Eng. Phys. 2014, 36, 889–895. [Google Scholar] [CrossRef] [PubMed]
- Fitriyah, H.; Wihandika, R.C. An Analysis of RGB, Hue and Grayscale under Various Illuminations. In Proceedings of the 2018 International Conference on Sustainable Information Engineering and Technology (SIET), Malang, Indonesia, 10–12 November 2018; pp. 38–41. [Google Scholar] [CrossRef]
- Yilmaz, A.; Javed, O.; Shah, M. Object tracking: A survey. ACM Comput. Surv. 2006, 38. [Google Scholar] [CrossRef]






© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Serrancolí, G.; Bogatikov, P.; Tanyà Palacios, G.; Torner, J.; Monllau, J.C.; Perelli, S. An Open-Source Android Application to Measure Anterior–Posterior Knee Translation. Appl. Sci. 2020, 10, 5896. https://doi.org/10.3390/app10175896
Serrancolí G, Bogatikov P, Tanyà Palacios G, Torner J, Monllau JC, Perelli S. An Open-Source Android Application to Measure Anterior–Posterior Knee Translation. Applied Sciences. 2020; 10(17):5896. https://doi.org/10.3390/app10175896
Chicago/Turabian StyleSerrancolí, Gil, Peter Bogatikov, Guillem Tanyà Palacios, Jordi Torner, Joan Carles Monllau, and Simone Perelli. 2020. "An Open-Source Android Application to Measure Anterior–Posterior Knee Translation" Applied Sciences 10, no. 17: 5896. https://doi.org/10.3390/app10175896
APA StyleSerrancolí, G., Bogatikov, P., Tanyà Palacios, G., Torner, J., Monllau, J. C., & Perelli, S. (2020). An Open-Source Android Application to Measure Anterior–Posterior Knee Translation. Applied Sciences, 10(17), 5896. https://doi.org/10.3390/app10175896