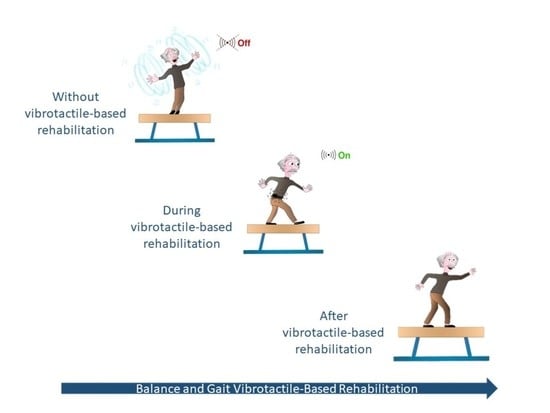
Vibrotactile-Based Rehabilitation on Balance and Gait in Patients with Neurological Diseases: A Systematic Review and Metanalysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Search Strategy and Eligibility Criteria
2.2. Study Selection and Data Collection Process
2.3. Measures and Synthesis of Results
3. Results
3.1. VF Effects on Pitch Sway Angular Velocity
3.2. VF Effects on Pitch Sway Angle
3.3. VF Effects on Roll Sway Angular Velocity
3.4. VF Effects on Roll Sway Angle
| Participants | Intervention | Outcome Measures | |
|---|---|---|---|
| Rossi, 2020 [32] | n = 27 (PD = 15; Healthy = 12) University laboratory Inclusion criteria: PD diagnosis Time since diagnosis onset (yr): 9.0 ± 4.9 Age (yr): PD (61 ± 7.3); Healthy (93.7 ± 13.6) | Participants were asked to walk in three different sensorial condition: - no-haptic suggestions mode: walked while no haptic suggestion was sent; - haptic-suggestions mode: as in the previously condition with the haptic stimuli switched on; - mixed mode: half walking path with stimuli and half without. Frequency: 1 time for 1 day | Step’s elevation and length; Velocity and inter-stride variance; FOG time. |
| Kodama, 2019 [34] | n = 9 (Stroke = 9) Hospital ward Inclusion criteria: Stroke: age 50–80 years, stroke > 6 months ago, completion of conventional therapy, stand up unsupported for 10 min, sense BF vibrations. Time since diagnosis onset (yr): 6.6 ± 3.6 Age (yr): 81.56 ± 44 | Two task-oriented balance training exercises: - standing on a rubber foam mat: participants stood barefoot on the mat with their eyes open and were instructed to use the BF information to stabilize their postural sway; -weight shifting to the paralyzed limb: participants were instructed to move their paralyzed lower limb forward and then put their weight on that limb. Frequency: 2 times a week for 2 weeks. | CoP A/P CoP M/L |
| Afzal, 2018 [50] | n = 10 (Stroke = 10) University hospital ward Inclusion criteria: subacute phase, able to walk 10m without assistance, Brunnstrom stage ≥ 3 Time since diagnosis onset (d): 62.5 ± 26.6 Age (yr): 57.7 ± 10.6 | Participants were asked to walk for 10 m in four different trial conditions: - Normal walk in a straight line without any assistance/cue. Subject maintains self-preferred walking speed an operator calculates the normal gait speed of the subject; - Walk with only tactile cue. Subject maintains self-preferred walking speed and operator calculates the gait speed; - Walk with only kinesthetic cue. Speed is set to normal gait speed + 0%, + 20% and + 40% in separate trials; - Walk with both tactile cue and kinesthetic cue. Speed is set to normal gait speed + 0% + 20% and + 40% in separate trials. Each trial condition was performed two times by the participants. | Gait speed (m/s) RMS of ML Tilt (degrees) Stance Symmetry Ratio - % muscle activity EMG |
| Fung, 2018 [45] | n = 10 (PD = 10) University laboratory Inclusion criteria: PD diagnosis, 2–4 H&Y, stand independently for 5 min, walk independently for 10 m. Time since diagnosis onset (yr): not declared Age (yr): PD (61 ± 7.3); Healthy (70.7 ± 7.89) | 24 trials of dynamic WSBE by using the SBS’s custom application that provided visual and auditory instructions pointing out the start and end of each trial. Frequency: 1 time for 1 day | LOS (A/P & M/L) XCOR (A/P & M/L) PE (A/P & M/L) PTA (A/P & M/L) |
| High, 2018 [44] | n = 10 (PD = 9, HO = 10, ORF = 9) University laboratory Inclusion criteria: PD participants: PD diagnosis, UPDRS motor score 25.22 ± 13.24); ORF participants: at least two falls in the last year (American and British Geriatric Society classification). Time since diagnosis onset (yr): not declared Age (yr): PD (69 ± 10.25), HO (76.4 ± 6.8), ORF (82 ± 9.72) | Stay still barefoot for 30s in each of the following conditions: (1) feet together, eyes open on firm surface (2) feet together, eyes closed on firm surface (3) feet together, eyes open on foam surface (4) feet together, eyes closed on foam surface (5) tandem stance with eyes open on firm surface Frequency: 2 consecutive trials for 1 day. | Path length Velocity Sway area Alpha M/L Alpha A/P |
| Lee, 2018 [46] | n = 18 (PD = 9, HO = 9) Undeclared setting Inclusion criteria: PD diagnosis, D3 < H&Y > 4 Time since diagnosis onset (yr): not declared Age (yr): PD (67.1 ± 6.5), HO (67.7 ± 6.9) | 12 familiarization trials to acclimate themselves to vibrotactile biofeedback; 5 min seated rest; 20 randomized trials of dynamic weight-shifting balance exercises as a function of the coding scheme and movement direction. Frequency: 1 time for 1 day | LOS (A/P & M/L) XCOR (A/P & M/L) PE (A/P & M/L) |
| Yasuda, 2018 [54] | n = 9 (Stroke = 9) Hospital ward Inclusion criteria: history of chronic stroke, age 50–80 years, stroke > 6 months ago, completion of conventional therapy, stand up unsupported for 10 min, sense BF vibrations. Time since diagnosis onset (mth): >6 Age (yr): 64.4 ± 9.2 | Two task-oriented balance training exercises were used: - standing on a rubber foam mat: participants stood barefoot on the mat with their eyes open and were instructed to use the BF information to stabilize their postural sway - weight shifting to the paralyzed limb: participants were instructed to move their paralyzed lower limb forward and then put their weight on that limb. Each training session comprised 10 repetitions of the balance task (1 min per repetition, 10 min total) with a short interval between repetitions. Frequency: 2 times a week for 2 weeks. | CoP pressure data Berg Balance Scale (BBS) Functional Reach Test (FRT) Timed-Up and Go Test (TUG) |
| Van Wegen, 2018 [43] | n = 15 (PD = 15) Home situation Inclusion criteria: PD diagnosis, 1–3 H&Y, score ≥ 2 on item 28 of UPDRS, correctable postural abnormality, sufficient cognitive function, absence of relevant comorbidities, stable medication regimen. Time since diagnosis onset (yr): 8.6 ± 4.8 Age (yr): PD (70.1 ± 8.7) | In the intervention period (week 2) the UpRight was active. Two trained assessors instructed the patients that they should consciously correct their posture in response to the sensory-feedback signal. Frequency: 2 weeks | Average trunk angle in the sagittal plane. Self-reported patient satisfaction to determine feasibility and user-friendliness of the UpRight. |
| Afzal, 2017 [51] | n = 6 (Stroke = 6) Undeclared setting Inclusion criteria: No limitations in joint range of motion and sensorial feedback abilities or other diagnosed neurologic or musculoskeletal disease Time since diagnosis onset (d): 69.7 ± 24.9 Age (yr): 55.0 ± 11.0 | Subjects walked 10 m distance two times in each trial. Kinesthetic stimuli were moved with the operator’s set velocity and provide a constant vibration on the skank during the swing phase. | RMS ML Stance ratio Muscle activity EMG |
| Yasuda, 2017 [55] | n = 17 (Stroke = 17) Rehabilitation center Inclusion criteria: stroke history, sufficient communication abilities, Brunsnstrom recovery Stage III, MMSE > 20, maintain balance in bipedal stance on a foam rubber mat for > 30 s, sense vibration of the BF. Time since diagnosis onset (d): 1144.94 ± 1451.63. Age (yr): 60.8 ± 17.3 | One familiarization session. The BF session comprised five repetitions of the balance task (15s each), with an interval of 1 min between each repetition. Frequency: 1 time for 1 day. | CoP spatial variability. Mean velocity of CoP displacement (mm/s) Mean CoP A/P and M/L distance. |
| Otis, 2016 [53] | n = 21 (12 PD, 9 Healthy) University laboratory Inclusion criteria: PD diagnosis, physically active, without musculoskeletal or other neurological disorders. Time since diagnosis onset: not declared Age (yr): PD (67.9 ± 10.0), Healthy (66.8 ± 8.0) | Firstly, the subject was asked to walk along a corridor by performing the TUG test without cueing. Secondly, participants performed two trials under vibratory stimulation condition at 10% above baseline cadence over each type of soil (concrete, parquet, broken stone, sand, carpet living room, and carpet foam) for a total of twenty-four trials for the two conditions. Frequency: 1 time for 1 day | TUG Risk of falling |
| van, der Logt 2016 [41] | n = 10 (MS = 10) Undeclared setting Inclusion criteria: MS diagnosis, able to walk without aids, without orthopedic problems or other diseases/disabilities than MS that could affect balance. Time since diagnosis onset: not declared Age (yr): 46.8 ± 7.7 | Assessment and training sequences consisting of stance and gait task while without shoes. Patients performed the assessment sequence three times and the training sequence of trial protocols once on the same day with sufficient breaks between sequences to avoid fatigue. Assessment sequence: 12 tasks, training sequence execute 3 consecutive times (7 tasks). Frequency: 1 time for 1 day | standing on one leg with eyes open standing on two legs with eyes closed standing on two legs with eyes open on foam standing on one leg with eyes open on foam standing on two legs eyes closed on foam tandem stance with eyes open and closed walking eight tandem steps with eyes open and closed - walk over a set of low (24 cm) barriers spaced one meter apart - walked eight meters with eyes open - three meters with eyes closed |
| Afzal, 2015 [52] | n = 9 (Stroke = 4, Healthy = 5) Undeclared setting Inclusion criteria: Stroke patients Time since diagnosis onset: undeclared Age (yr): (Stroke = 67.2 ± 5.5, Healthy = 26.2 ± 3.2) | The distance of the walking trial was 10 m for healthy and 6 m for stroke. The subject was asked to walk in three scenarios: normal walk, walk whit stance time matching constant vibration mode and with swing phase constant vibration mode. | Symmetry ratio M/L tilt-RMS M/L acceleration-RMS Right stance Left stance Gait speed |
| Lee, 2015 [47] | n = 20 (PD = 11, Healthy = 9) Clinical setting Inclusion criteria: PD diagnosis, 3–4 H&Y Time since diagnosis onset: not declared Age (yr): PD (70.0 ± 8.1); Healthy (67.8 ± 6.6) | All participants performed 12 familiarization trials (i.e., 3 modalities × 2 directions × 2 repetitions) to acclimate to the guidance modalities (visual, vibrotactile, and simultaneous visual and vibrotactile biofeedback) during dynamic weight-shifting balance exercises. After the completion of the familiarization trials, all participants were provided a 5 min seated rest. During the experimental session, all participants performed dynamic weight-shifting balance exercises as a function of the modality and direction with 5 repetitions for a total of 30 trials (i.e., 3 modalities × 2 directions × 5 repetitions). The order of trials was randomized for each participant. Frequency: 1 time for 1 day. | LOS (A/P & M/L) SOT score |
| Lee, 2013 [42] | n = 44 (Mild PD = 20, Advanced PD = 7; Healthy = 17) Undeclared setting Inclusion criteria: PD diagnosis, able to stand unaided, 1–3 H&Y Time since diagnosis onset: not declared Age (yr): Mild PD (67.5 ± 10.4);Advanced PD (68.6 ± 11.3);Healthy (67.5 ± 10.4) | Subjects stood on a motorized, computer-controlled platform that moved at a peak acceleration of 1.16 m/s2, a constant velocity of 0.48 m/s, and a peak deceleration of 0.58 m/s2. Thus, the stepping reaction is fairly automatic, although subjects were warned that stepping was the necessary reaction, and 3 practice trials in each direction were administered. Frequency: 1 time for 1 day | SRT step length step angular velocity number of steps total trunk displacement trunk displacement before taking the first protective step |
| Rossi-Izquierdo, 2013 [48] | n = 10 (PD = 10) Undeclared setting Inclusion criteria: 3–4 H&Y Time since diagnosis: not declared Age (yr): 67.0 (53–79 years) | A training session consisted of 5 repetitions of six selected training tasks as described above. The patient received a VF signal during training in those directions which showed a higher body sway than preset thresholds Frequency: 5 time/week for 2 weeks | Free-field body sway analysis (mobile posturography) SBDT or Gsbdt SOT DHI ABC number of falls in the least three months Comparison of the results of vibrotactile neurofeedback training with a CDP-training in PD patients |
| Nanhoe-Mahabier, 2012 [35] | n = 20 (PD = 20) Undeclared setting Inclusion criteria: PD diagnosis Time since diagnosis onset: not declared Age (yr): Feedback group (59.3±20.0); Control Group (58.6±2.5) | Real-time biofeedback during balance exercises. Frequency: 1 time for 1 day | Roll sway Pitc sway |
| Basta, 2011 [49] | n = 105 (Canal Paresis = 25), (Otolith disorder = 21), (Acustic Neuroma = 10), (Microvascualr syndrome = 12), (PD = 10), (Presbyvertigo = 13), (control group = 14) Undeclared setting Inclusion criteria: pathologic body sway at the SBDT or gSBDT tests. Time since diagnosis onset: not declared Age (yr): (Canal Paresis = 60.2 ± 13.6), (Otolith disorder = 54.6 ± 13.8), (Acustic Neuroma = 60.2 ± 10.1), (Microvascualr syndrome = 52.0 ± 10.8), PD (68.1 ± 9.1), Presbyvertigo (73.4 ± 6.0). | Vestibular rehabilitation exercise with Vertiguard training device. Frequency: 5 time/week for 2 weeks | SOT DHI VSS Pitch and Roll |
| First Author, Year | Study Type | Selection | Treatment Protocol | Outocome(s) | Total |
|---|---|---|---|---|---|
| Rossi, 2020 [32] | Proof-of-concept | * | ** | *** | 6/7 |
| Kodama, 2020 [34] | Clinical Trial | * | ** | *** | 6/7 |
| Afzal, 2018 [50] | Clinical Trial | * | * | *** | 5/7 |
| Fung, 2018 [45] | Longitudinal Study | * | * | *** | 5/7 |
| High, 2018 [44] | Clinical Trial | * | * | *** | 5/7 |
| Lee, 2018 [46] | Clinical Trial | * | * | *** | 5/7 |
| Yasuda, 2018 [54] | Clinical Trial | * | ** | *** | 6/7 |
| Van Wegen, 2018 [43] | Multiple case control pre-post design | * | * | ** | 4/7 |
| Afzal, 2017 [51] | Clinical trial | * | ** | *** | 6/7 |
| Otis, 2016 [53] | Clinical trial | * | ** | *** | 6/7 |
| Afzal, 2015 [52] | Clinical trial | N.A. | * | *** | 4/7 |
| Lee, 2015 [47] | Clinical Trial | * | ** | *** | 6/7 |
| Lee, 2013 [42] | Clinical Trial | * | ** | ** | 5/7 |
| Rossi-Izquierdo, 2013 [48] | Clinical Trial | * | ** | *** | 6/7 |
| First Author, Year | Study Type | Random Allocation | Concealed Allocation | Baseline Comparability | Participant Blinding | Therapist Blinding | Assessor Blinding | Adequate Follow-up | Intention-to-Treat Analysis | Between-Group Comparison | Point Estimates and Variability | Total (0 to 10) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Yasuda, 2017 [55] | RCT | N | N | Y | N | N | N | Y | Y | Y | Y | 5/10 |
| van der logt 2016 [41] | RCT (crossover study) | N | Y | N | N | N | N | N | N | Y | Y | 4/10 |
| Nanhoe-Mahabier, 2012 [35] | RCT | Y | N | Y | Y | N | N | Y | Y | Y | Y | 7/10 |
| Basta, 2011 [49] | RCT | Y | N | Y | Y | Y | N | N | N | Y | Y | 6/10 |
4. Discussion
4.1. Strengths of the Systematic Review
4.2. Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
Appendix A.1. Search Strategy in MEDLINE (PubMed)
Appendix A.2. Search Strategy in PEDro
- balance AND vibrotactile
- balance AND haptic
References
- Bruijn, S.M.; van Dieën, J.H. Control of human gait stability through foot placement. J. R. Soc. Interface 2018, 15, 20170816. [Google Scholar] [CrossRef] [PubMed]
- Tramontano, M.; Morone, G.; Curcio, A.; Temperoni, G.; Medici, A.; Morelli, D.; Caltagirone, C.; Paolucci, S.; Iosa, M. Maintaining gait stability during dual walking task: Effects of age and neurological disorders. Eur. J. Phys. Rehabil. Med. 2017, 53, 7–13. [Google Scholar] [CrossRef] [PubMed]
- Tramontano, M.; Bonnì, S.; Martino Cinnera, A.; Marchetti, F.; Caltagirone, C.; Koch, G.; Peppe, A. Blindfolded Balance Training in Patients with Parkinson’s Disease: A Sensory-Motor Strategy to Improve the Gait. Parkinsons Dis. 2016, 2016, 7536862. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bonnì, S.; Ponzo, V.; Tramontano, M.; Martino Cinnera, A.; Caltagirone, C.; Koch, G.; Peppe, A. Neurophysiological and clinical effects of blindfolded balance training (BBT) in Parkinson’s disease patients: A preliminary study. Eur. J. Phys. Rehabil. Med. 2018, 55, 176–182. [Google Scholar] [CrossRef] [PubMed]
- Palakurthi, B.; Burugupally, S.P. Postural Instability in Parkinson’s Disease: A Review. Brain Sci. 2019, 9, 239. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tramontano, M.; Dell’Uomo, D.; Cinnera, A.M.; Luciani, C.; Di Lorenzo, C.; Marcotulli, M.; Vona, F.; Mercuro, A.; Abbruzzese, S. Visual-spatial training in patients with sub-acute stroke without neglect: A randomized. single-blind controlled trial. Funct. Neurol. 2019, 34, 7–13. [Google Scholar]
- Tramontano, M.; Martino Cinnera, A.; Manzari, L.; Tozzi, F.F.; Caltagirone, C.; Morone, G.; Pompa, A.; Grasso, M.G. Vestibular rehabilitation has positive effects on balance, fatigue and activities of daily living in highly disabled multiple people: A preliminary randomized controlled trial. Restor. Neurol. Neurosci. 2018, 36, 709–718. [Google Scholar] [CrossRef]
- Cattaneo, D.; Gervasoni, E.; Pupillo, E.; Bianchi, E.; Aprile, I.; Imbimbo, I.; Russo, R.; Cruciani, A.; Turolla, A.; Jonsdottir, J.; et al. Educational and Exercise Intervention to Prevent Falls and Improve Participation in Subjects With Neurological Conditions: The NEUROFALL Randomized Controlled Trial. Front. Neurol. 2019, 10, 865. [Google Scholar] [CrossRef] [Green Version]
- Goto, Y.; Otaka, Y.; Suzuki, K.; Inoue, S.; Kondo, K.; Shimizu, E. Incidence and circumstances of falls among community-dwelling ambulatory stroke survivors: A prospective study. Geriatr. Gerontol. Int. 2019, 19, 240–244. [Google Scholar] [CrossRef]
- Silva-Batista, C.; Corcos, D.M.; Kanegusuku, H.; Piemonte, M.E.P.; Gobbi, L.T.B.; de Lima-Pardini, A.C.; de Mello, M.T.; Forjaz, C.L.M.; Ugrinowitsch, C. Balance and fear of falling in subjects with Parkinson’s disease is improved after exercises with motor complexity. Gait Posture 2018, 61, 90–97. [Google Scholar] [CrossRef] [Green Version]
- Rensink, M.; Schuurmans, M.; Lindeman, E.; Hafsteinsdóttir, T. Task-oriented training in rehabilitation after stroke: Systematic review. Adv. Nurs. 2009, 65, 737–754. [Google Scholar] [CrossRef] [PubMed]
- Obeso, J.A.; Rodríguez-Oroz, M.C.; Benitez-Temino, B.; Blesa, F.J.; Guridi, J.; Marin, C.; Rodriguez, M. Functional organization of the basal ganglia: Therapeutic implications for Parkinson’s disease. Mov. Disord. 2008, 23 (Suppl. 3), S548–S559. [Google Scholar] [CrossRef] [PubMed]
- Peppe, A.; Paravati, S.; Baldassarre, M.G.; Bakdounes, L.; Spolaor, F.; Guiotto, A.; Pavan, D.; Sawacha, Z.; Bottino, S.; Clerici, D.; et al. Proprioceptive Focal Stimulation (Equistasi®) May Improve the Quality of Gait in Middle-Moderate Parkinson’s Disease Patients. DoubleBlind, Double-Dummy, Randomized, Crossover, Italian Multicentric Study. Front. Neurol. 2019, 10, 998. [Google Scholar] [CrossRef] [PubMed]
- Tramontano, M.; Russo, V.; Spitoni, G.; Ciancarelli, I.; Paolucci, S.; Manzari, L.; Morone, G. The efficacy of vestibular rehabilitation in patients with neurological disorders: A systematic review. Arch. Phys. Med. Rehabil. 2020, in press. [Google Scholar] [CrossRef]
- Tramontano, M.; Bergamini, E.; Iosa, M.; Belluscio, V.; Vannozzi, G.; Morone, G. Vestibular rehabilitation training in patients with subacute stroke: A preliminary randomized controlled trial. NeuroRehabilitation 2018, 43, 247–254. [Google Scholar] [CrossRef]
- Tramontano, M.; Medici, A.; Iosa, M.; Chiariotti, A.; Fusillo, G.; Manzari, L.; Morelli, D. The effect of vestibular stimulation on motor functions of children with cerebral palsy. Mot. Control 2017, 21, 299–311. [Google Scholar] [CrossRef]
- Tramontano, M.; Grasso, M.G.; Soldi, S.; Casula, E.P.; Bonnì, S.; Mastrogiacomo, S.; D’Acunto, A.; Porrazzini, F.; Caltagirone, C.; Koch, G. Cerebellar Intermittent Theta-Burst Stimulation Combined with Vestibular Rehabilitation Improves Gait and Balance in Patients with Multiple Sclerosis: A Preliminary Double-Blind Randomized Controlled Trial. Cerebellum 2020, 19, 897–901. [Google Scholar] [CrossRef]
- Nam, S.M.; Kim, K.; Lee, D.Y. Effects of visual feedback balance training on the balance and ankle instability in adult men with functional ankle instability. J. Phys. Ther. Sci. 2018, 30, 113–115. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tramontano, M.; Morone, G.; Palomba, A.; De Angelis, S.; Mercuro, A.; Caltagirone, C.; Grasso, M.G. Effectiveness of a sensor-based technology in upper limb motor recovery in post-acute stroke neurorehabilitation: A randomized controlled trial. J. Biol. Regul. Homeost. Agents 2020, 34 (Suppl. 3), 165–174. [Google Scholar]
- Tramontano, M.; Morone, G.; De Angelis, S.; Casagrande Conti, L.; Galeoto, G.; Grasso, M.G. Sensor-based technology for upper limb rehabilitation in patients with multiple sclerosis: A randomized controlled trial. Restor. Neurol. Neurosci. 2020, 38, 333–341. [Google Scholar] [CrossRef]
- Kiper, P.; Baba, A.; Agostini, M.; Turolla, A. Proprioceptive Based Training for stroke recovery. Proposal of new treatment modality for rehabilitation of upper limb in neurological diseases. Arch. Physiother. 2015, 5, 6. [Google Scholar] [CrossRef]
- Abbruzzese, G.; Trompetto, C.; Mori, L.; Pelosin, E. Proprioceptive rehabilitation of upper limb dysfunction in movement disorders: A clinical perspective. Front. Hum. Neurosci. 2014, 8, 961. [Google Scholar] [CrossRef] [Green Version]
- Tramontano, M.; Consorti, G.; Morone, G.; Lunghi, C. Vertigo and Balance Disorders—The Role of Osteopathic Manipulative Treatment: A Systematic Review. Schwindel und Gleichgewichtsstörungen—Rolle der osteopathischen Manipulationstherapie: Eine systematische Übersichtsarbeit. Complement. Med. Res. 2020, 1–10. [Google Scholar] [CrossRef]
- De Bartolo, D.; Spitoni, G.F.; Iosa, M.; Morone, G.; Ciancarelli, I.; Paolucci, S.; Antonucci, G. From movement to thought and back: A review on the role of cognitive factors influencing technological neurorehabilitation. Funct. Neurol. 2019, 34, 131–144. [Google Scholar]
- Morone, G.; Spitoni, G.F.; De Bartolo, D.; Ghanbari Ghooshchy, S.; Di Iulio, F.; Paolucci, S.; Zoccolotti, P.; Iosa, M. Rehabilitative devices for a top-down approach. Expert Rev. Med. Devices. 2019, 16, 187–195. [Google Scholar] [CrossRef] [PubMed]
- Kearney, E.; Shellikeri, S.; Martino, R.; Yunusova, Y. Augmented visual feedback-aided interventions for motor rehabilitation in Parkinson’s disease: A systematic review. Disabil. Rehabil. 2019, 41, 995–1011. [Google Scholar] [CrossRef] [PubMed]
- Verna, V.; De Bartolo, D.; Iosa, M.; Fadda, L.; Pinto, G.; Caltagirone, C.; De Angelis, S.; Tramontano, M. Te.M.P.O. an app for using temporal musical mismatch in post-stroke neurorehabilitation: A preliminary randomized controlled study. NeuroRehabilitation 2020, 47, 201–208. [Google Scholar] [CrossRef]
- van Breda, E.; Verwulgen, S.; Saeys, W.; Wuyts, K.; Peeters, T.; Truijen, S. Vibrotactile feedback as a tool to improve motor learning and sports performance: A systematic review. BMJ Open Sport Exerc. Med. 2017, 3, e000216. [Google Scholar] [CrossRef] [PubMed]
- Scotto di Luzio, F.; Lauretti, C.; Cordella, F.; Draicchio, F.; Zollo, L. Visual vs vibrotactile feedback for posture assessment during upper-limb robot-aided rehabilitation. Appl. Ergon. 2020, 82, 102950. [Google Scholar] [CrossRef]
- Bark, K.; Hyman, E.; Tan, F.; Cha, E.; Jax, S.A.; Buxbaum, L.J.; Kuchenbecker, K.J. Effects of vibrotactile feedback on human learning of arm motions. IEEE Trans. Neural Syst. Rehabil. Eng. 2015, 23, 51–63. [Google Scholar] [CrossRef] [Green Version]
- Choi, S.; Kuchenbecker, K.J. Vibrotactile Display: Perception, Technology, and Applications. Proc. IEEE 2013, 101, 2093–2104. [Google Scholar] [CrossRef]
- Rossi, S.; Lisini Baldi, T.; Aggravi, M.; Ulivelli, M.; Cioncoloni, D.; Niccolini, V.; Donati, L.; Prattichizzo, D. Wearable haptic anklets for gait and freezing improvement in Parkinson’s disease: A proof-of-concept study. Neurol. Sci. 2020, 41, 3643–3651. [Google Scholar] [CrossRef]
- Prewett, M.S.; Elliott, L.R.; Walvoord, A.G.; Coovert, M.D. A Meta-Analysis of Vibrotactile and Visual Information Displays for Improving Task Performance. IEEE Trans. Syst. Man Cybern. Part C (Appl. Rev.) 2012, 42, 123–132. [Google Scholar] [CrossRef]
- Kodama, K.; Yasuda, K.; Kuznetsov, N.A.; Hayashi, Y.; Iwata, H. Balance Training With a Vibrotactile Biofeedback System Affects the Dynamical Structure of the Center of Pressure Trajectories in Chronic Stroke Patients. Front. Hum. Neurosci. 2019, 13, 84. [Google Scholar] [CrossRef]
- Nanhoe-Mahabier, W.; Allum, J.H.; Pasman, E.P.; Overeem, S.; Bloem, B.R. The effects of vibrotactile biofeedback training on trunk sway in Parkinson’s disease patients. Parkinsonism Relat. Disord. 2012, 18, 1017–1021. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Held, J.P.; Klaassen, B.; van Beijnum, B.F.; Luft, A.R.; Veltink, P.H. Usability Evaluation of a VibroTactile Feedback System in Stroke Subjects. Front. Bioeng. Biotechnol. 2017, 4, 98. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ 2009, 339, b2535. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Higgins, J.P.T.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. Cochrane Handbook for Systematic Reviews of Interventions; Version 6.1; Cochrane: London, UK, 2020. [Google Scholar]
- de Morton, N.A. The PEDro scale is a valid measure of the methodological quality of clinical trials: A demographic study. Aust. J. Physiother. 2009, 55, 129–133. [Google Scholar] [CrossRef] [Green Version]
- Wells, G.; Shea, B.; O’Connell, D.; Peterson, J.; Welch, V.; Losos, M.; Tugwell, P. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analysis. Available online: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (accessed on 14 December 2020).
- van der Logt, R.P.; Findling, O.; Rust, H.; Yaldizli, O.; Allum, J.H. The effect of vibrotactile biofeedback of trunk sway on balance control in multiple sclerosis. Mult. Scler. Relat. Disord. 2016, 8, 58–63. [Google Scholar] [CrossRef]
- Lee, P.Y.; Gadareh, K.; Naushahi, M.J.; Gresty, M.; Bronstein, A.M. Protective stepping response in Parkinsonian patients and the effect of vibrotactile feedback. Mov. Disord. 2013, 28, 482–489. [Google Scholar] [CrossRef]
- van Wegen, E.E.H.; de Goede, C.J.T.; Kwakkel, G.; van Kordelaar, J. Sensor assisted self-management in Parkinson’s disease: A feasibility study of ambulatory posture detection and feedback to treat stooped posture. Parkinsonism Relat. Disord. 2018, 46 (Suppl. 1), S57–S61. [Google Scholar] [CrossRef]
- High, C.M.; McHugh, H.F.; Mills, S.C.; Amano, S.; Freund, J.E.; Vallabhajosula, S. Vibrotactile Feedback Alters Dynamics Of Static Postural Control In Persons With Parkinson’s Disease But Not Older Adults At High Fall Risk. Gait Posture 2018, 63, 202–207. [Google Scholar] [CrossRef]
- Fung, A.; Lai, E.C.; Lee, B.C. Usability and Validation of the Smarter Balance System: An Unsupervised Dynamic Balance Exercises System for Individuals With Parkinson’s Disease. IEEE Trans. Neural Syst. Rehabil. Eng. 2018, 26, 798–806. [Google Scholar] [CrossRef]
- Lee, B.C.; Fung, A.; Thrasher, T.A. The Effects of Coding Schemes on Vibrotactile Biofeedback for Dynamic Balance Training in Parkinson’s Disease and Healthy Elderly Individuals. IEEE Trans. Neural Syst. Rehabil. Eng. 2018, 26, 153–160. [Google Scholar] [CrossRef] [PubMed]
- Lee, B.C.; Thrasher, T.A.; Fisher, S.P.; Layne, C.S. The effects of different sensory augmentation on weight-shifting balance exercises in Parkinson’s disease and healthy elderly people: A proof-of-concept study. J. Neuroeng. Rehabil. 2015, 12, 75. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rossi-Izquierdo, M.; Ernst, A.; Soto-Varela, A.; Santos-Pérez, S.; Faraldo-García, A.; Sesar-Ignacio, Á.; Basta, D. Vibrotactile neurofeedback balance training in patients with Parkinson’s disease: Reducing the number of falls. Gait Posture 2013, 37, 195–200. [Google Scholar] [CrossRef] [PubMed]
- Basta, D.; Rossi-Izquierdo, M.; Soto-Varela, A.; Greters, M.E.; Bittar, R.S.; Steinhagen-Thiessen, E.; Eckardt, R.; Harada, T.; Goto, F.; Ogawa, K.; et al. Efficacy of a Vibrotactile Neurofeedback Training in Stance and Gait Conditions for the Treatment of Balance Deficits. Otol. Neurotol. 2011, 32, 1492–1499. [Google Scholar] [CrossRef] [Green Version]
- Afzal, M.R.; Pyo, S.; Oh, M.K.; Park, Y.S.; Yoon, J. Evaluating the effects of delivering integrated kinesthetic and tactile cues to individuals with unilateral hemiparetic stroke during overground walking. J. Neuroeng. Rehabil. 2018, 15, 33. [Google Scholar] [CrossRef]
- Afzal, M.R.; Pyo, S.; Oh, M.K.; Park, Y.S.; Yoon, J. Identifying the effects of using integrated haptic feedback for gait rehabilitation of stroke patients. IEEE Int. Conf. Rehabil. Robot. 2017, 2017, 1055–1060. [Google Scholar] [CrossRef]
- Afzal, M.R.; Oh, M.K.; Lee, C.H.; Park, Y.S.; Yoon, J. A Portable Gait Asymmetry Rehabilitation System for Individuals with Stroke Using a Vibrotactile Feedback. Biomed. Res. Int. 2015, 2015, 375638. [Google Scholar] [CrossRef]
- Otis, M.J.; Ayena, J.C.; Tremblay, L.E.; Fortin, P.E.; Ménélas, B.A. Use of an Enactive Insole for Reducing the Risk of Falling on Different Types of Soil Using Vibrotactile Cueing for the Elderly. PLoS ONE 2016, 11, e0162107. [Google Scholar] [CrossRef]
- Yasuda, K.; Saichi, K.; Kaibuki, N.; Harashima, H.; Iwata, H. Haptic-based perception-empathy biofeedback system for balance rehabilitation in patients with chronic stroke: Concepts and initial feasibility study. Gait Posture 2018, 62, 484–489. [Google Scholar] [CrossRef] [PubMed]
- Yasuda, K.; Kaibuki, N.; Harashima, H.; Iwata, H. The effect of a haptic biofeedback system on postural control in patients with stroke: An experimental pilot study. Somatosens. Mot. Res. 2017, 34, 65–71. [Google Scholar] [CrossRef] [PubMed]
- Ballardini, G.; Florio, V.; Canessa, A.; Carlini, G.; Morasso, P.; Casadio, M. Vibrotactile Feedback for Improving Standing Balance. Front. Bioeng. Biotechnol. 2020, 8, 94. [Google Scholar] [CrossRef] [PubMed]
- Stronks, H.C.; Walker, J.; Parker, D.J.; Barnes, N. Training Improves Vibrotactile Spatial Acuity and Intensity Discrimination on the Lower Back Using Coin Motors. Artif. Organs 2017, 41, 1059–1070. [Google Scholar] [CrossRef] [PubMed]
- Kuo, A.D. The relative roles of feedforward and feedback in the control of rhythmic movements. Mot. Control 2002, 6, 129–145. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dimitrijevic, M.R.; Gerasimenko, Y.; Pinter, M.M. Evidence for a spinal central pattern generator in humans. Ann. N. Y. Acad. Sci. 1998, 860, 360–376. [Google Scholar] [CrossRef]
- Verhoeff, L.L.; Horlings, C.G.; Janssen, L.J.; Bridenbaugh, S.A.; Allum, J.H. Effects of biofeedback on trunk sway during dual tasking in the healthy young and elderly. Gait Posture 2009, 30, 76–81. [Google Scholar] [CrossRef]
- Belluscio, V.; Bergamini, E.; Tramontano, M.; Formisano, R.; Buzzi, M.G.; Vannozzi, G. Does Curved Walking Sharpen the Assessment of Gait Disorders? An Instrumented Approach Based on Wearable Inertial Sensors. Sensors 2020, 20, 5244. [Google Scholar] [CrossRef]
- Belluscio, V.; Bergamini, E.; Tramontano, M.; Orejel Bustos, A.; Allevi, G.; Formisano, R.; Vannozzi, G.; Buzzi, M.G. Gait Quality Assessment in Survivors from Severe Traumatic Brain Injury: An Instrumented Approach Based on Inertial Sensors. Sensors 2019, 19, 5315. [Google Scholar] [CrossRef] [Green Version]
- Belluscio, V.; Bergamini, E.; Iosa, M.; Tramontano, M.; Morone, G.; Vannozzi, G. The iFST: An instrumented version of the Fukuda Stepping Test for balance assessment. Gait Posture 2018, 60, 203–208. [Google Scholar] [CrossRef] [PubMed]




Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
De Angelis, S.; Princi, A.A.; Dal Farra, F.; Morone, G.; Caltagirone, C.; Tramontano, M. Vibrotactile-Based Rehabilitation on Balance and Gait in Patients with Neurological Diseases: A Systematic Review and Metanalysis. Brain Sci. 2021, 11, 518. https://doi.org/10.3390/brainsci11040518
De Angelis S, Princi AA, Dal Farra F, Morone G, Caltagirone C, Tramontano M. Vibrotactile-Based Rehabilitation on Balance and Gait in Patients with Neurological Diseases: A Systematic Review and Metanalysis. Brain Sciences. 2021; 11(4):518. https://doi.org/10.3390/brainsci11040518
Chicago/Turabian StyleDe Angelis, Sara, Alessandro Antonio Princi, Fulvio Dal Farra, Giovanni Morone, Carlo Caltagirone, and Marco Tramontano. 2021. "Vibrotactile-Based Rehabilitation on Balance and Gait in Patients with Neurological Diseases: A Systematic Review and Metanalysis" Brain Sciences 11, no. 4: 518. https://doi.org/10.3390/brainsci11040518
APA StyleDe Angelis, S., Princi, A. A., Dal Farra, F., Morone, G., Caltagirone, C., & Tramontano, M. (2021). Vibrotactile-Based Rehabilitation on Balance and Gait in Patients with Neurological Diseases: A Systematic Review and Metanalysis. Brain Sciences, 11(4), 518. https://doi.org/10.3390/brainsci11040518