Bioinformatic, Biochemical, and Immunological Mining of MHC Class I Restricted T Cell Epitopes for a Marburg Nucleoprotein Microparticle Vaccine
Abstract
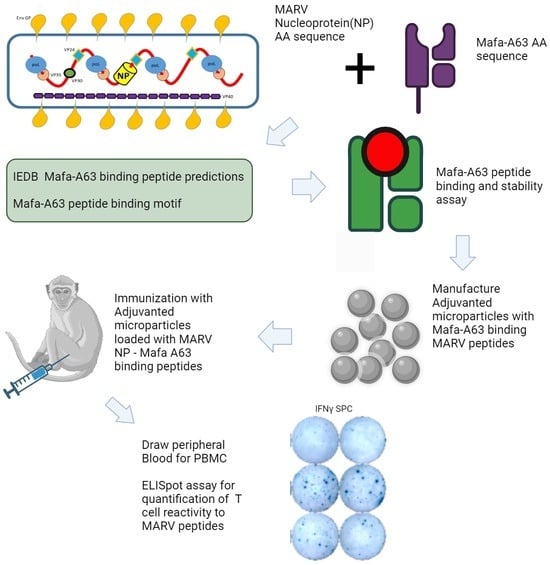
:1. Introduction
2. Materials and Methods
2.1. Immunoinformatics
2.1.1. Protein Sequence Variability/Shannon Entropy Scores
2.1.2. Antigenicity Predictions
2.1.3. In Silico MHC Class I Restricted T Cell Epitope Prediction
2.2. Biochemical Characterization of Peptide Binding to Mafa-A63 MHC Class I Molecules
2.2.1. Peptide Synthesis, MHC Class I Peptide Binding Affinity, and Stabilization Assays
2.2.2. Preparation of Adjuvanted MARV Microspheres for In Vivo Studies
2.3. In Vivo Experiments
2.3.1. Animal Care and Housing
2.3.2. MARV Microsphere Immunization
2.3.3. ELISpot Assays
3. Results and Discussion
3.1. Immunoinformatic Screening of Marburg Proteins: Shannon Sequence Variability and Antigenicity Predictions
3.2. Immunoinformatic Screening of Marburg Proteins: Prediction of Mafa–A063 T Cell Epitopes
3.3. MARV Peptide Binding to Mafa-A063 and HLA Class I Molecules
3.4. In Vivo Immunogenicity Testing of MARV Peptide-Containing Microspheres in Cynomolgus Macaques Carrying the Mafa–A1*063 MHC Class I Allele
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Number | Peptide Sequence | IEDB Focused on the Mafa-A63 Peptide Binding Motif | IEDB High Binding Score Rank without Motif | Mafa-A063 Positive or Negative Control Peptide |
|---|---|---|---|---|
| 1 | APFARVLNL | X | ||
| 2 | APHVRNKKV | X | ||
| 3 | APQEDTRAR | X | ||
| 4 | DPFALLNED | X | ||
| 5 | DPFGSIGDV | X | ||
| 6 | DPIQHPAVS | X | ||
| 7 | DPTPVEVTV | X | ||
| 8 | EPHYSPLIL | X | ||
| 9 | EPIRSPSSP | X | ||
| 10 | EPPRQSQDI | X | ||
| 11 | HPAVSSQDP | X | ||
| 12 | HPLVRTSKV | X | ||
| 13 | IPEPPRQSQ | X | ||
| 14 | IPNEPHYSP | X | ||
| 15 | IPSTTSREF | X | ||
| 16 | KPFLRYQEL | X | ||
| 17 | KPTAPHVRN | X | ||
| 18 | LPKLVVGDR | X | ||
| 19 | LPPPPLYAQ | X | ||
| 20 | LPPPVDSKI | X | ||
| 21 | LPPVQEDDE | X | ||
| 22 | NPPESLITA | X | ||
| 23 | NPVSAKELQ | X | ||
| 24 | PPESLITAL | X | ||
| 25 | PPLYAQEKR | X | ||
| 26 | PPPLYAQEK | X | ||
| 27 | PPPPLYAQE | X | ||
| 28 | PPPVDSKIE | X | ||
| 29 | PPRQSQDID | X | ||
| 30 | PPVDSKIEH | X | ||
| 31 | PPVQEDDES | X | ||
| 32 | QPGSDNEQG | X | ||
| 33 | RPINRPTAL | X | ||
| 34 | RPTALPPPV | X | ||
| 35 | SPDFTNYED | X | ||
| 36 | SPIAKYLRD | X | ||
| 37 | SPLILALKT | X | ||
| 38 | SPSAPQEDT | X | ||
| 39 | SPSSPSAPQ | X | ||
| 40 | TPVEVTVQA | X | ||
| 41 | WPDMSFDER | X | ||
| 42 | WPQRVVTKK | X | ||
| 43 | YPNDLLQTN | X | ||
| 44 | YPNHWLTTG | X | ||
| 45 | YPQLSAIAL | X | ||
| 46 | EVASFKQAL | X | ||
| 47 | GEYAPFARV | X | ||
| 48 | GLYPQLSAI | X | ||
| 49 | HYSPLILAL | X | ||
| 50 | KVKNEVASF | X | ||
| 51 | LEHGLYPQL | X | ||
| 52 | LIVKTVLEF | X | ||
| 53 | QLSAIALGV | X | ||
| 54 | TRFSGLLIV | X | ||
| 55 | TVLEFILQK | X | ||
| 56 | VGQTRFSGL | X | ||
| 57 | RPKQAWCWF | Control HIV ENV peptide with a motif | ||
| 59 | FLSFCSLFL | Negative Control-Low IEDB rank | ||
| 60 | LFLSFCSLF | Negative Control-Low IEDB rank | ||
| 61 | LYPQLSAIAL | Negative Control-Low IEDB rank | ||
| 62 | QTRFSGLLIV | Negative Control-Low IEDB rank | ||
| 63 | LSFCSLFLPK | Negative Control-Low IEDB rank Control | ||
| 64 | LLIVKTVL | Negative control reference: EBOV NP (8 mer) | ||
| 58 | RPKVPLRTM | Positive control reference SIV NEF [69] | ||
| 65 | GPRKPIKCW | Positive control reference–SIV GP [67] | ||
| 66 | HPAQTSQW | Positive control reference: SIV NEF [68] |
| Number | Peptide Sequence | IEDB-Predicted Binding Allele and Affinity (nM) | Measured Affinity as IC50 (nM) | IEDB-Predicted Binding Allele and Affinity (nM) | Measured Affinity as IC50 (nM) | IEDB-Predicted Binding Allele and Affinity (nM) | Measured Affinity as IC50 (nM) |
|---|---|---|---|---|---|---|---|
| 1 | APFARVLNL | HLA-B*07:02–32 | 0.21 | HLA-B*08:01–287 | 67 | ||
| 2 | HPLVRTSKV | HLA-B*07:02–87 | HLA-B*08:01–268 | ||||
| 3 | YPQLSAIAL | HLA-B*07:02–15 | 44 | HLA-B*08:01–481 | 17 | ||
| 4 | EVASFKQAL | HLA-A*26:01–574 | 86 | HLA-A*68:02 1 | 2.7 | HLA-B*07:02 | 250 |
| 5 | GEYAPFARV | HLA-B*40:01–145 | 107 | HLA-B*44:02 | 214 | ||
| 6 | GLYPQLSAI | HLA-A*02:01–18 | 5.9 | HLA-A*02:03 | 1.4 | HLA-A*02:06 | 6.9 |
| 7 | HYSPLILAL | HLA-A*24:02–190 | 64 | HLA-B*23:01 | 3.5 | ||
| 8 | KVKNEVASF | HLA-B*15:01–32 | 5.6 | HLA-A*32:01 | 2.9 | HLA-A*30:02 | 158 |
| 9 | LEHGLYPQL | HLA-B*40:01–23 | 14 | HLA-B*44:02 | 3.4 | ||
| 10 | LIVKTVLEF | HLA-B*15:01–26 | 0.80 | HLA-A*23:01 | 109 | ||
| 11 | QLSAIALGV | HLA-A*02:01–28 | 3.9 | HLA-A*02:03 HLA-A*02:06 | 4.4 12 | HLA-A*32:01 HLA-A*68:02 | 81 11 |
| 12 | TRFSGLLIV | HLA-B*27:05–116 | HLA-B*39:015–344 | ||||
| 13 | TVLEFILQK | HLA-A*03:01–64 | 19 | HLA-A*11:01 HLA-A*68:01 | 2.2 | HLA-A*30:01 | 365 |
| 14 | VGQTRFSGL | HLA-B*08:01–442 | |||||
| 15 | FLSFCSLFL | HLA-A*02:01–4 | 1.8 | HLA-A*02:03 | 29 | HLA-A*02:06 | 121 |
| 16 | LFLSFCSLF | HLA-A*24:02–98 | 633 | HLA-A*23:01 | 33 | ||
| 17 | LYPQLSAIAL | HLA-A*24:02 −148 | 179 | HLA-B*07:02–120 | 134 | HLA-A*24:02 | 179 |
| 18 | QTRFSGLLIV | HLA-B*27:05–600 | 533 | HLA-A*30:01 | 421 | HLA-B*15:01 | 4682 |
| 19 | LSFCSLFLPK | HLA-A*03:01–38 | 4.3 | HLA-A*11:01 HLA-A*30:01 | 0.68 238 | HLA-A*31:01 HLA-A*68:01 | 686 1.0 |
| 20 | LLIVKTVL | HLA-B*08:01–179 | 6.1 |
| Peptides from Appendix A Table A2 Tested against the HLA Allele | Peptides Tested | # of. Binders |
|---|---|---|
| A*01:01 | 1 | 0 |
| A*02:01 | 5 | 3 |
| A*02:03 | 7 | 3 |
| A*02:06 | 9 | 3 |
| A*03:01 | 2 | 2 |
| A*11:01 | 2 | 2 |
| A*23:01 | 4 | 4 |
| A*24:02 | 3 | 2 |
| A*26:01 | 3 | 1 |
| A*30:01 | 4 | 3 |
| A*30:02 | 1 | 1 |
| A*31:01 | 2 | 0 |
| A*32:01 | 4 | 3 |
| A*33:01 | 3 | 0 |
| A*68:01 | 3 | 2 |
| A*68:02 | 5 | 2 |
| B*07:02 | 7 | 5 |
| B*08:01 | 7 | 4 |
| B*15:01 | 7 | 3 |
| B*27:05 | 2 | 1 |
| B*35:01 | 8 | 1 |
| B*39:01 | 0 | 0 |
| B*40:01 | 2 | 2 |
| B*44:02 | 2 | 2 |
| B*44:03 | 2 | 0 |
| B*51:01 | 5 | 0 |
| B*53:01 | 5 | 0 |
| B*57:01 | 1 | 0 |
| B*58:01 | 3 | 1 |
| Peptide Sequence | ID | DRB1_0104 1 | DRB1_0901 | DRB1_1602 | DRB5_0101 | ||||
|---|---|---|---|---|---|---|---|---|---|
| Core | nM | Core | nM | Core | nM | Core | nM | ||
| QYIKANSKFIGITEL | Tet 830–844 | YIKANSKFI | 27 | YIKANSKFI | 13 | YIKANSKFI | 13 | YIKANSKFI | 17 |
| VADSPLEASKRWAFRTGVPPKNVEYTE 2,3 | GP 59–85 | FRTGVPPKN | 122 | FRTGVPPKN LEASKRWAF | 85 | WAFRTGVPP | 165 | FRTGVPPKN | 46 |
| FISLILIQGIKTLPILEIASNNQPQN | GP 7–32 | IKTLPILEI | 19 | IKTLPILEI IQGIKTLPI | 62 | IKTLPILEI | 55 | IQGIKTLPI ILEIASNNQ | 117 |
| RVFTEGNIAAMIVNKTVHKMIFSRQ 4 | GP 158–182 | IAAMIVNKT | 69 | IAAMIVNKT | 286 | IAAMIVNKT | 223 | MIVNKTVHK | 114 |
| ID | Peptide Sequence | VaxiJen Score |
|---|---|---|
| SD9 | SPDFTNYED | 1.31 |
| IQ9 | IPEPPRQSQ | 0.156 |
| HP9 | HPAVSSQDP | 1.00 |
| LQ9 | LPPPPLYAQ | 0.872 |
| TA9 | TPVEVTVQA | 1.16 |
| PL9 | PPESLITAL | −0.094 |
| EI9 | EPPRQSQDI | 0.482 |
| LE9 | LPPVQEDDE | 0.669 |
| EP9 | EPIRSPSSP | −0.484 |
| YN9 | YPNDLLQTN | 0.212 |
| KF9 | KVKNEVASF | 0.610 |
| AL9 | APFARVLNL | 0.6130 |
| RV9 | RPTALPPPV | 0.9853 |
| HL9 | HYSPLILAL | 1.4600 |
| Advantages | Limitations |
|---|---|
| Cost-Effectiveness: Readily synthesized and peptides purified at low cost, making them economically viable. Deployable in areas where ring vaccination strategies might fail. Uses off-the-shelf reagents, simplifying the production process. | HLA Type Restriction: Class I MHC restriction limits the relevance of individual peptides to certain HLA types, reducing universality. |
| Stability: Stable at room temperature for more than six months, ensuring a longer shelf-life. Freedom from cold-chain logistic limitations. | Immune Response: T cell immune responses may be transient and/or of low magnitude, potentially impacting long-term efficacy. |
| Safety: Synthetic peptides have demonstrated safety in many human studies. The controlled-release adjuvanted microsphere–short peptide vaccine used in this study has demonstrated safety in rodent and NHP models. | Epitope Diversity: Peptide vaccine may have to include a large number of epitopes to confer disease protection across a wide range of patients. |
| Specificity and Targeted Delivery: Using defined epitopes avoids uncharacterized antigens that may cause non-therapeutic or autoimmune activity. Microsphere diameter is optimized to target APCs with phagocytic properties and avoids nonprofessional nonphagocytic APCs. | Induction of B cell antibody responses: Currently, there is limited information regarding Ebola or Marburg linear B cell epitopes [48] that might be included in the microspheres to induce an effective antibody response. At present, the microsphere platform is a “T cell vaccine” only. |
| Monitoring: Known MHC class I and class II epitope sequences enable direct monitoring of T cell responses, enhancing vaccine efficacy assessment. | Disease protection vs. Sterilizing immunity: T cell vaccines may not provide sterilizing immune protection, although they may prevent disease |
| Booster Vaccines: Feasibility of repeated booster vaccines to maintain or enhance immune responses No anti-vector immune response. | Inaccuracy of T cell epitope prediction methods: Bioinformatic T cell epitope prediction methods fall short of 100% accuracy in the absence of confirmational studies. |
| Protection: Peptide encapsulation in controlled release PLGA microspheres protects T cell epitopes from extracellular degradation. | |
| Adjuvant Efficacy: Microsphere-encapsulated synthetic adjuvants promote optimal co-stimulation molecule expression by targeted APCs. | |
| Mucosal Delivery: Adjuvanted microspheres are suitable for mucosal surface delivery by inhalation, broadening the application scope. | |
| Compliance with Standards: The Microsphere vaccine platform is animal product-free and conforms to halal standards. |
References
- CDC Strategic Planning Workgroup. Biological and chemical terrorism: Strategic plan for preparedness and response. Recommendations of the CDC Strategic Planning Workgroup. MMWR Recomm. Rep. 2000, 49, 1–14. [Google Scholar]
- Salvaggio, M.R.; Baddley, J.W. Other viral bioweapons: Ebola and Marburg hemorrhagic fever. Dermatol. Clin. 2004, 22, 291–302. [Google Scholar] [CrossRef] [PubMed]
- Meadows, A.J.; Stephenson, N.; Madhav, N.K.; Oppenheim, B. Historical trends demonstrate a pattern of increasingly frequent and severe spillover events of high-consequence zoonotic viruses. BMJ Glob. Health 2023, 8, e012026. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Marburg Virus Disease—Equatorial Guinea. Available online: https://www.who.int/emergencies/disease-outbreak-news/item/2023-DON472 (accessed on 11 May 2023).
- Suschak, J.J.; Schmaljohn, C.S. Vaccines against Ebola virus and Marburg virus: Recent advances and promising candidates. Hum. Vaccines Immunother. 2019, 15, 2359–2377. [Google Scholar] [CrossRef] [PubMed]
- Davis, C.J. Nuclear blindness: An overview of the biological weapons programs of the former Soviet Union and Iraq. Emerg. Infect. Dis. 1999, 5, 509–512. [Google Scholar] [CrossRef] [PubMed]
- Miller, J.; Broad, W.J.; Engelberg, S. Germs: Biological Weapons and America’s Secret War; Miller, J., Engelberg, S., Broad, W., Eds.; Simon & Schuster: New York, NY, USA, 2001; Volume 323. [Google Scholar]
- Borio, L.; Inglesby, T.; Peters, C.J.; Schmaljohn, A.L.; Hughes, J.M.; Jahrling, P.B.; Ksiazek, T.; Johnson, K.M.; Meyerhoff, A.; O’Toole, T.; et al. Hemorrhagic fever viruses as biological weapons: Medical and public health management. JAMA 2002, 287, 2391–2405. [Google Scholar] [CrossRef] [PubMed]
- Bausch, D.G.; Ksiazek, T.G. Viral hemorrhagic fevers including hantavirus pulmonary syndrome in the Americas. Clin. Lab. Med. 2002, 22, 981–1020. [Google Scholar] [CrossRef]
- Srivastava, D.; Kutikuppala, L.V.S.; Shanker, P.; Sahoo, R.N.; Pattnaik, G.; Dash, R.; Kandi, V.; Ansari, A.; Mishra, S.; Desai, D.N.; et al. The neglected continuously emerging Marburg virus disease in Africa: A global public health threat. Health Sci. Rep. 2023, 6, e1661. [Google Scholar] [CrossRef]
- Abir, M.H.; Rahman, T.; Das, A.; Etu, S.N.; Nafiz, I.H.; Rakib, A.; Mitra, S.; Emran, T.B.; Dhama, K.; Islam, A.; et al. Pathogenicity and virulence of Marburg virus. Virulence 2022, 13, 609–633. [Google Scholar] [CrossRef]
- Klenk, H.D.; Slenczka, W. Marburg- and Ebolaviruses: A Look Back and Lessons for the Future. In Ebolaviruses: Methods and Protocols; Hoenen, T., Groseth, A., Eds.; Springer: New York, NY, USA, 2017; pp. 3–14. [Google Scholar] [CrossRef]
- Slenczka, W.G. The Marburg virus outbreak of 1967 and subsequent episodes. Curr. Top Microbiol. Immunol. 1999, 235, 49–75. [Google Scholar] [CrossRef]
- Hunter, N.; Rathish, B. Marburg Fever. In StatPearls; StatPearls: Treasure Island, FL, USA, 2023. [Google Scholar]
- Bosio, C.M.; Aman, M.J.; Grogan, C.; Hogan, R.; Ruthel, G.; Negley, D.; Mohamadzadeh, M.; Bavari, S.; Schmaljohn, A. Ebola and Marburg viruses replicate in monocyte-derived dendritic cells without inducing the production of cytokines and full maturation. J. Infect. Dis. 2003, 188, 1630–1638. [Google Scholar] [CrossRef] [PubMed]
- Fernando, L.; Qiu, X.; Melito, P.L.; Williams, K.J.; Feldmann, F.; Feldmann, H.; Jones, S.M.; Alimonti, J.B. Immune Response to Marburg Virus Angola Infection in Nonhuman Primates. J. Infect. Dis. 2015, 212 (Suppl. S2), S234–S241. [Google Scholar] [CrossRef] [PubMed]
- Prator, C.A.; Dorratt, B.M.; O’Donnell, K.L.; Lack, J.; Pinski, A.N.; Ricklefs, S.; Martens, C.A.; Messaoudi, I.; Marzi, A. Transcriptional profiling of immune responses in NHPs after low-dose, VSV-based vaccination against Marburg virus. Emerg. Microbes Infect. 2023, 12, 2252513. [Google Scholar] [CrossRef] [PubMed]
- Rubsamen, R.; Burkholz, S.; Massey, C.; Brasel, T.; Hodge, T.; Wang, L.; Herst, C.; Carback, R.; Harris, P. Anti-IL-6 Versus Anti-IL-6R Blocking Antibodies to Treat Acute Ebola Infection in BALB/c Mice: Potential Implications for Treating Cytokine Release Syndrome. Front. Pharmacol. 2020, 11, 574703. [Google Scholar] [CrossRef] [PubMed]
- Woolsey, C.; Geisbert, T.W. Current state of Ebola virus vaccines: A snapshot. PLoS Pathog. 2021, 17, e1010078. [Google Scholar] [CrossRef]
- Parish, L.A.; Stavale, E.J.; Houchens, C.R.; Wolfe, D.N. Developing Vaccines to Improve Preparedness for Filovirus Outbreaks: The Perspective of the USA Biomedical Advanced Research and Development Authority (BARDA). Vaccines 2023, 11, 1120. [Google Scholar] [CrossRef]
- Geisbert, T.W.; Geisbert, J.B.; Leung, A.; Daddario-DiCaprio, K.M.; Hensley, L.E.; Grolla, A.; Feldmann, H. Single-injection vaccine protects nonhuman primates against infection with marburg virus and three species of ebola virus. J. Virol. 2009, 83, 7296–7304. [Google Scholar] [CrossRef]
- Reiter, D. $35.7 Million Awarded for Marburg Virus Vaccine Development. Available online: https://www.precisionvaccinations.com/iavi-rvsv%CE%B4g-marv-gp-marburg-virus-vaccine-candidate (accessed on 15 November 2023).
- Hamer, M.J.; Houser, K.V.; Hofstetter, A.R.; Ortega-Villa, A.M.; Lee, C.; Preston, A.; Augustine, B.; Andrews, C.; Yamshchikov, G.V.; Hickman, S.; et al. Safety, tolerability, and immunogenicity of the chimpanzee adenovirus type 3-vectored Marburg virus (cAd3-Marburg) vaccine in healthy adults in the USA: A first-in-human, phase 1, open-label, dose-escalation trial. Lancet 2023, 401, 294–302. [Google Scholar] [CrossRef]
- Hunegnaw, R.; Honko, A.N.; Wang, L.; Carr, D.; Murray, T.; Shi, W.; Nguyen, L.; Storm, N.; Dulan, C.N.M.; Foulds, K.E.; et al. A single-shot ChAd3-MARV vaccine confers rapid and durable protection against Marburg virus in nonhuman primates. Sci. Transl. Med. 2022, 14, eabq6364. [Google Scholar] [CrossRef]
- McCann, N.; O’Connor, D.; Lambe, T.; Pollard, A.J. Viral vector vaccines. Curr. Opin. Immunol. 2022, 77, 102210. [Google Scholar] [CrossRef]
- Berg, A.; Wright, D.; Dulal, P.; Stedman, A.; Fedosyuk, S.; Francis, M.J.; Charleston, B.; Warimwe, G.M.; Douglas, A.D. Stability of Chimpanzee Adenovirus Vectored Vaccines (ChAdOx1 and ChAdOx2) in Liquid and Lyophilised Formulations. Vaccines 2021, 9, 1249. [Google Scholar] [CrossRef] [PubMed]
- Toniolo, S.P.; Afkhami, S.; D’Agostino, M.R.; Lichty, B.D.; Cranston, E.D.; Xing, Z.; Thompson, M.R. Spray dried VSV-vectored vaccine is thermally stable and immunologically active in vivo. Sci. Rep. 2020, 10, 13349. [Google Scholar] [CrossRef]
- Afley, P.; Dohre, S.K.; Prasad, G.B.; Kumar, S. Prediction of T cell epitopes of Brucella abortus and evaluation of their protective role in mice. Appl. Microbiol. Biotechnol. 2015, 99, 7625–7637. [Google Scholar] [CrossRef]
- Cunha-Neto, E.; Rosa, D.S.; Harris, P.E.; Olson, T.; Morrow, A.; Ciotlos, S.; Herst, C.V.; Rubsamen, R.M. An Approach for a Synthetic CTL Vaccine Design against Zika Flavivirus Using Class I and Class II Epitopes Identified by Computer Modeling. Front. Immunol. 2017, 8, 640. [Google Scholar] [CrossRef]
- Harris, P.E.; Brasel, T.; Massey, C.; Herst, C.V.; Burkholz, S.; Lloyd, P.; Blankenberg, T.; Bey, T.M.; Carback, R.; Hodge, T.; et al. A Synthetic Peptide CTL Vaccine Targeting Nucleocapsid Confers Protection from SARS-CoV-2 Challenge in Rhesus Macaques. Vaccines 2021, 9, 520. [Google Scholar] [CrossRef] [PubMed]
- Heng, W.T.; Lim, H.X.; Tan, K.O.; Poh, C.L. Validation of Multi-epitope Peptides Encapsulated in PLGA Nanoparticles Against Influenza A Virus. Pharm. Res. 2023, 40, 1999–2025. [Google Scholar] [CrossRef] [PubMed]
- Herst, C.V.; Burkholz, S.; Sidney, J.; Sette, A.; Harris, P.E.; Massey, S.; Brasel, T.; Cunha-Neto, E.; Rosa, D.S.; Chao, W.C.H.; et al. An effective CTL peptide vaccine for Ebola Zaire Based on Survivors’ CD8+ targeting of a particular nucleocapsid protein epitope with potential implications for COVID-19 vaccine design. Vaccine 2020, 38, 4464–4475. [Google Scholar] [CrossRef]
- Hiremath, J.; Kang, K.I.; Xia, M.; Elaish, M.; Binjawadagi, B.; Ouyang, K.; Dhakal, S.; Arcos, J.; Torrelles, J.B.; Jiang, X.; et al. Entrapment of H1N1 Influenza Virus Derived Conserved Peptides in PLGA Nanoparticles Enhances T Cell Response and Vaccine Efficacy in Pigs. PLoS ONE 2016, 11, e0151922. [Google Scholar] [CrossRef]
- Nixon, D.F.; Hioe, C.; Chen, P.D.; Bian, Z.; Kuebler, P.; Li, M.L.; Qiu, H.; Li, X.M.; Singh, M.; Richardson, J.; et al. Synthetic peptides entrapped in microparticles can elicit cytotoxic T cell activity. Vaccine 1996, 14, 1523–1530. [Google Scholar] [CrossRef]
- Roozbehani, M.; Falak, R.; Mohammadi, M.; Hemphill, A.; Razmjou, E.; Meamar, A.R.; Masoori, L.; Khoshmirsafa, M.; Moradi, M.; Gharavi, M.J. Characterization of a multi-epitope peptide with selective MHC-binding capabilities encapsulated in PLGA nanoparticles as a novel vaccine candidate against Toxoplasma gondii infection. Vaccine 2018, 36, 6124–6132. [Google Scholar] [CrossRef]
- Rubsamen, R.M.; Herst, C.V.; Lloyd, P.M.; Heckerman, D.E. Eliciting cytotoxic T-lymphocyte responses from synthetic vectors containing one or two epitopes in a C57BL/6 mouse model using peptide-containing biodegradable microspheres and adjuvants. Vaccine 2014, 32, 4111–4116. [Google Scholar] [CrossRef]
- Burkholz, S.R.; Herst, C.V.; Carback, R.T.; Harris, P.E.; Rubsamen, R.M. Survivin (BIRC5) Peptide Vaccine in the 4T1 Murine Mammary Tumor Model: A Potential Neoadjuvant T Cell Immunotherapy for Triple Negative Breast Cancer: A Preliminary Study. Vaccines 2023, 11, 644. [Google Scholar] [CrossRef]
- Chen, Q.; Bao, Y.; Burner, D.; Kaushal, S.; Zhang, Y.; Mendoza, T.; Bouvet, M.; Ozkan, C.; Minev, B.; Ma, W. Tumor growth inhibition by mSTEAP peptide nanovaccine inducing augmented CD8(+) T cell immune responses. Drug Deliv. Transl. Res. 2019, 9, 1095–1105. [Google Scholar] [CrossRef]
- Herrmann, V.L.; Wieland, D.E.; Legler, D.F.; Wittmann, V.; Groettrup, M. The STEAP1(262-270) peptide encapsulated into PLGA microspheres elicits strong cytotoxic T cell immunity in HLA-A*0201 transgenic mice—A new approach to immunotherapy against prostate carcinoma. Prostate 2016, 76, 456–468. [Google Scholar] [CrossRef] [PubMed]
- Ma, W.; Smith, T.; Bogin, V.; Zhang, Y.; Ozkan, C.; Ozkan, M.; Hayden, M.; Schroter, S.; Carrier, E.; Messmer, D.; et al. Enhanced presentation of MHC class Ia, Ib and class II-restricted peptides encapsulated in biodegradable nanoparticles: A promising strategy for tumor immunotherapy. J. Transl. Med. 2011, 9, 34. [Google Scholar] [CrossRef] [PubMed]
- Horvath, D.; Basler, M. PLGA Particles in Immunotherapy. Pharmaceutics 2023, 15, 615. [Google Scholar] [CrossRef]
- McHugh, K.J.; Nguyen, T.D.; Linehan, A.R.; Yang, D.; Behrens, A.M.; Rose, S.; Tochka, Z.L.; Tzeng, S.Y.; Norman, J.J.; Anselmo, A.C.; et al. Fabrication of fillable microparticles and other complex 3D microstructures. Science 2017, 357, 1138–1142. [Google Scholar] [CrossRef] [PubMed]
- Furuyama, W.; Shifflett, K.; Pinski, A.N.; Griffin, A.J.; Feldmann, F.; Okumura, A.; Gourdine, T.; Jankeel, A.; Lovaglio, J.; Hanley, P.W.; et al. Rapid Protection from COVID-19 in Nonhuman Primates Vaccinated Intramuscularly but Not Intranasally with a Single Dose of a Vesicular Stomatitis Virus-Based Vaccine. mBio 2022, 13, e0337921. [Google Scholar] [CrossRef]
- Tioni, M.F.; Jordan, R.; Pena, A.S.; Garg, A.; Wu, D.; Phan, S.I.; Weiss, C.M.; Cheng, X.; Greenhouse, J.; Orekov, T.; et al. Mucosal administration of a live attenuated recombinant COVID-19 vaccine protects nonhuman primates from SARS-CoV-2. NPJ Vaccines 2022, 7, 85. [Google Scholar] [CrossRef]
- Woolsey, C.; Cross, R.W.; Agans, K.N.; Borisevich, V.; Deer, D.J.; Geisbert, J.B.; Gerardi, C.; Latham, T.E.; Fenton, K.A.; Egan, M.A.; et al. A highly attenuated Vesiculovax vaccine rapidly protects nonhuman primates against lethal Marburg virus challenge. PLoS Neglected Trop. Dis. 2022, 16, e0010433. [Google Scholar] [CrossRef]
- Albaqami, F.F.; Altharawi, A.; Althurwi, H.N.; Alharthy, K.M.; Qasim, M.; Muhseen, Z.T.; Tahir Ul Qamar, M. Computational Modeling and Evaluation of Potential mRNA and Peptide-Based Vaccine against Marburg Virus (MARV) to Provide Immune Protection against Hemorrhagic Fever. Biomed. Res. Int. 2023, 2023, 5560605. [Google Scholar] [CrossRef]
- Dhasmana, A.; Dhasmana, S.; Alsulimani, A.; Kotnala, S.; Kashyap, V.K.; Haque, S.; Jaggi, M.; Yallapu, M.M.; Chauhan, S.C. In silico CD4 + T-cell multiepitope prediction and HLA distribution analysis for Marburg Virus—A strategy for vaccine designing. J. King Saud Univ. Sci. 2022, 34, 101751. [Google Scholar] [CrossRef]
- Babirye, P.; Musubika, C.; Kirimunda, S.; Downing, R.; Lutwama, J.J.; Mbidde, E.K.; Weyer, J.; Paweska, J.T.; Joloba, M.L.; Wayengera, M. Identity and validity of conserved B cell epitopes of filovirus glycoprotein: Towards rapid diagnostic testing for Ebola and possibly Marburg virus disease. BMC Infect. Dis. 2018, 18, 498. [Google Scholar] [CrossRef]
- Baral, P.; Pavadai, E.; Zhou, Z.; Xu, Y.; Tison, C.K.; Pokhrel, R.; Gerstman, B.S.; Chapagain, P.P. Immunoinformatic screening of Marburgvirus epitopes and computational investigations of epitope-allele complexes. Int. Immunopharmacol. 2022, 111, 109109. [Google Scholar] [CrossRef] [PubMed]
- Debroy, B.; Chowdhury, S.; Pal, K. Designing a novel and combinatorial multi-antigenic epitope-based vaccine “MarVax” against Marburg virus-a reverse vaccinology and immunoinformatics approach. J. Genet. Eng. Biotechnol. 2023, 21, 143. [Google Scholar] [CrossRef]
- Hasan, M.; Azim, K.F.; Begum, A.; Khan, N.A.; Shammi, T.S.; Imran, A.S.; Chowdhury, I.M.; Urme, S.R.A. Vaccinomics strategy for developing a unique multi-epitope monovalent vaccine against Marburg marburgvirus. Infect. Genet. Evol. 2019, 70, 140–157. [Google Scholar] [CrossRef]
- Mujahed, I.; Mustafa, S.W.S. Next generation multi epitope based peptide vaccine against Marburg Virus disease combined with molecular docking studies. Inform. Med. Unlocked 2022, 33, 101087. [Google Scholar] [CrossRef]
- Pervin, T.; Oany, A.R. Vaccinomics approach for scheming potential epitope-based peptide vaccine by targeting l-protein of Marburg virus. In Silico Pharmacol. 2021, 9, 21. [Google Scholar] [CrossRef] [PubMed]
- Mahmud, S.M.N.; Rahman, M.; Kar, A.; Jahan, N.; Khan, A. Designing of an Epitope-Based Universal Peptide Vaccine against Highly Conserved Regions in RNA Dependent RNA Polymerase Protein of Human Marburg Virus: A Computational Assay. Anti Infect Agents 2020, 18, 294–305. [Google Scholar] [CrossRef]
- Sami, S.A.; Marma, K.K.S.; Mahmud, S.; Khan, M.A.N.; Albogami, S.; El-Shehawi, A.M.; Rakib, A.; Chakraborty, A.; Mohiuddin, M.; Dhama, K.; et al. Designing of a Multi-epitope Vaccine against the Structural Proteins of Marburg Virus Exploiting the Immunoinformatics Approach. ACS Omega 2021, 6, 32043–32071. [Google Scholar] [CrossRef]
- Soltan, M.A.; Abdulsahib, W.K.; Amer, M.; Refaat, A.M.; Bagalagel, A.A.; Diri, R.M.; Albogami, S.; Fayad, E.; Eid, R.A.; Sharaf, S.M.A.; et al. Mining of Marburg Virus Proteome for Designing an Epitope-Based Vaccine. Front. Immunol. 2022, 13, 907481. [Google Scholar] [CrossRef]
- Yousaf, H.; Naz, A.; Zaman, N.; Hassan, M.; Obaid, A.; Awan, F.M.; Azam, S.S. Immunoinformatic and reverse vaccinology-based designing of potent multi-epitope vaccine against Marburgvirus targeting the glycoprotein. Heliyon 2023, 9, e18059. [Google Scholar] [CrossRef]
- Supply of Monkeys for Research Is at a Crisis Point, U.S. Government Report Concludes. Available online: https://www.science.org/content/article/supply-monkeys-research-crisis-point-u-s-government-report-concludes (accessed on 11 May 2023).
- Garcia-Boronat, M.; Diez-Rivero, C.M.; Reinherz, E.L.; Reche, P.A. PVS: A web server for protein sequence variability analysis tuned to facilitate conserved epitope discovery. Nucleic Acids Res. 2008, 36, W35–W41. [Google Scholar] [CrossRef]
- Mullick, B.; Magar, R.; Jhunjhunwala, A.; Barati Farimani, A. Understanding mutation hotspots for the SARS-CoV-2 spike protein using Shannon Entropy and K-means clustering. Comput. Biol. Med. 2021, 138, 104915. [Google Scholar] [CrossRef] [PubMed]
- Zaharieva, N.; Dimitrov, I.; Flower, D.; Doytchinova, I. Immunogenicity prediction by VaxiJen: A ten year overview. J. Proteom. Bioinform. 2017, 10, 298–310. [Google Scholar]
- Lin, K.L.; Twenhafel, N.A.; Connor, J.H.; Cashman, K.A.; Shamblin, J.D.; Donnelly, G.C.; Esham, H.L.; Wlazlowski, C.B.; Johnson, J.C.; Honko, A.N.; et al. Temporal Characterization of Marburg Virus Angola Infection following Aerosol Challenge in Rhesus Macaques. J. Virol. 2015, 89, 9875–9885. [Google Scholar] [CrossRef] [PubMed]
- Callaway, E. Labs rush to study coronavirus in transgenic animals—Some are in short supply. Nature 2020, 579, 183–184. [Google Scholar] [CrossRef] [PubMed]
- Neergaard, L. Research Monkey Shortage Undermines US Readiness, Panel Says; Associated Press: New York, NY, USA, 2023. [Google Scholar]
- Reynisson, B.; Alvarez, B.; Paul, S.; Peters, B.; Nielsen, M. NetMHCpan-4.1 and NetMHCIIpan-4.0: Improved predictions of MHC antigen presentation by concurrent motif deconvolution and integration of MS MHC eluted ligand data. Nucleic Acids Res. 2020, 48, W449–W454. [Google Scholar] [CrossRef] [PubMed]
- Lan Zhang, G.; Budde, M.L.; Lhost, J.J.; O’Connor, D.H.; Hildebrand, W.H.; Brusic, V. PREDmafa: A system for prediction of peptide binding to several MHC class I molecules in cynomolgus macaques. In Proceedings of the 2nd ACM Conference on Bioinformatics, Computational Biology and Biomedicine, New York, NY, USA, 1–3 August 2011; pp. 602–606. [Google Scholar]
- Budde, M.L.; Greene, J.M.; Chin, E.N.; Ericsen, A.J.; Scarlotta, M.; Cain, B.T.; Pham, N.H.; Becker, E.A.; Harris, M.; Weinfurter, J.T.; et al. Specific CD8+ T cell responses correlate with control of simian immunodeficiency virus replication in Mauritian cynomolgus macaques. J. Virol. 2012, 86, 7596–7604. [Google Scholar] [CrossRef] [PubMed]
- Mohns, M.S.; Greene, J.M.; Cain, B.T.; Pham, N.H.; Gostick, E.; Price, D.A.; O’Connor, D.H. Expansion of Simian Immunodeficiency Virus (SIV)-Specific CD8 T Cell Lines from SIV-Naive Mauritian Cynomolgus Macaques for Adoptive Transfer. J. Virol. 2015, 89, 9748–9757. [Google Scholar] [CrossRef] [PubMed]
- Passaes, C.; Millet, A.; Madelain, V.; Monceaux, V.; David, A.; Versmisse, P.; Sylla, N.; Gostick, E.; Llewellyn-Lacey, S.; Price, D.A.; et al. Optimal Maturation of the SIV-Specific CD8(+) T Cell Response after Primary Infection Is Associated with Natural Control of SIV: ANRS SIC Study. Cell Rep. 2020, 32, 108174. [Google Scholar] [CrossRef]
- Sylvester-Hvid, C.; Kristensen, N.; Blicher, T.; Ferre, H.; Lauemoller, S.L.; Wolf, X.A.; Lamberth, K.; Nissen, M.H.; Pedersen, L.O.; Buus, S. Establishment of a quantitative ELISA capable of determining peptide—MHC class I interaction. Tissue Antigens 2002, 59, 251–258. [Google Scholar] [CrossRef] [PubMed]
- Ostergaard Pedersen, L.; Nissen, M.H.; Hansen, N.J.; Nielsen, L.L.; Lauenmoller, S.L.; Blicher, T.; Nansen, A.; Sylvester-Hvid, C.; Thromsen, A.R.; Buus, S. Efficient assembly of recombinant major histocompatibility complex class I molecules with preformed disulfide bonds. Eur. J. Immunol. 2001, 31, 2986–2996. [Google Scholar] [CrossRef]
- Sarkar, R.; Sharma, Y.; Jain, A.; Tehseen, A.; Singh, S.; Sehrawat, S. A Combinatorial in-silico, in-vitro and in-vivo Approach to Quantitatively Study Peptide Induced MHC Stability. Bio. Protoc. 2021, 11, e4255. [Google Scholar] [CrossRef] [PubMed]
- Justesen, S.; Harndahl, M.; Lamberth, K.; Nielsen, L.L.; Buus, S. Functional recombinant MHC class II molecules and high-throughput peptide-binding assays. Immunome. Res. 2009, 5, 2. [Google Scholar] [CrossRef] [PubMed]
- Harndahl, M.; Rasmussen, M.; Roder, G.; Dalgaard Pedersen, I.; Sorensen, M.; Nielsen, M.; Buus, S. Peptide-MHC class I stability is a better predictor than peptide affinity of CTL immunogenicity. Eur. J. Immunol. 2012, 42, 1405–1416. [Google Scholar] [CrossRef]
- Sidney, J.; Southwood, S.; Moore, C.; Oseroff, C.; Pinilla, C.; Grey, H.M.; Sette, A. Measurement of MHC/peptide interactions by gel filtration or monoclonal antibody capture. Curr. Protoc. Immunol. 2013, 100, 18.3.1–18.3.36. [Google Scholar] [CrossRef]
- Fraser, C.C.; Altreuter, D.H.; Ilyinskii, P.; Pittet, L.; LaMothe, R.A.; Keegan, M.; Johnston, L.; Kishimoto, T.K. Generation of a universal CD4 memory T cell recall peptide effective in humans, mice and non-human primates. Vaccine 2014, 32, 2896–2903. [Google Scholar] [CrossRef]
- Laubreton, D.; Bay, S.; Sedlik, C.; Artaud, C.; Ganneau, C.; Deriaud, E.; Viel, S.; Puaux, A.L.; Amigorena, S.; Gerard, C.; et al. The fully synthetic MAG-Tn3 therapeutic vaccine containing the tetanus toxoid-derived TT830-844 universal epitope provides anti-tumor immunity. Cancer Immunol. Immunother. 2016, 65, 315–325. [Google Scholar] [CrossRef]
- Berry, N.; Mee, E.T.; Almond, N.; Rose, N.J. The Impact and Effects of Host Immunogenetics on Infectious Disease Studies Using Non-Human Primates in Biomedical Research. Microorganisms 2024, 12, 155. [Google Scholar] [CrossRef]
- Agarwal, D.; Liu, C.; Bhoj, V.; Kearns, J.; Bharani, T.; Choe, I.; Vivek, K.; O’Connor, D.H.; Wiseman, R.W.; Duquesnoy, R.J.; et al. Adaptation of HLA testing to characterize the cynomolgus macaque MHC polymorphisms and alloantibody signatures. HLA 2023, 103, e15239. [Google Scholar] [CrossRef] [PubMed]
- Koehl, P.; Levitt, M. Sequence variations within protein families are linearly related to structural variations. J. Mol. Biol. 2002, 323, 551–562. [Google Scholar] [CrossRef]
- Liao, H.; Yeh, W.; Chiang, D.; Jernigan, R.L.; Lustig, B. Protein sequence entropy is closely related to packing density and hydrophobicity. Protein. Eng. Des. Sel. 2005, 18, 59–64. [Google Scholar] [CrossRef]
- Gaschen, B.; Taylor, J.; Yusim, K.; Foley, B.; Gao, F.; Lang, D.; Novitsky, V.; Haynes, B.; Hahn, B.H.; Bhattacharya, T.; et al. Diversity considerations in HIV-1 vaccine selection. Science 2002, 296, 2354–2360. [Google Scholar] [CrossRef] [PubMed]
- Kunwar, P.; Hawkins, N.; Dinges, W.L.; Liu, Y.; Gabriel, E.E.; Swan, D.A.; Stevens, C.E.; Maenza, J.; Collier, A.C.; Mullins, J.I.; et al. Superior control of HIV-1 replication by CD8+ T cells targeting conserved epitopes: Implications for HIV vaccine design. PLoS ONE 2013, 8, e64405. [Google Scholar] [CrossRef] [PubMed]
- Kumar, A.; Weiss, W.; Tine, J.A.; Hoffman, S.L.; Rogers, W.O. ELISPOT assay for detection of peptide specific interferon-gamma secreting cells in rhesus macaques. J. Immunol. Methods 2001, 247, 49–60. [Google Scholar] [CrossRef]
- Arrode-Bruses, G.; Moussa, M.; Baccard-Longere, M.; Villinger, F.; Chebloune, Y. Long-term central and effector SHIV-specific memory T cell responses elicited after a single immunization with a novel lentivector DNA vaccine. PLoS ONE 2014, 9, e110883. [Google Scholar] [CrossRef] [PubMed]
- Kamperschroer, C.; O’Donnell, L.M.; Schneider, P.A.; Li, D.; Roy, M.; Coskran, T.M.; Kawabata, T.T. Measuring T-cell responses against LCV and CMV in cynomolgus macaques using ELISPOT: Potential application to non-clinical testing of immunomodulatory therapeutics. J. Immunotoxicol. 2014, 11, 35–43. [Google Scholar] [CrossRef]
- Quinn, K.M.; Da Costa, A.; Yamamoto, A.; Berry, D.; Lindsay, R.W.; Darrah, P.A.; Wang, L.; Cheng, C.; Kong, W.P.; Gall, J.G.; et al. Comparative analysis of the magnitude, quality, phenotype, and protective capacity of simian immunodeficiency virus gag-specific CD8+ T cells following human-, simian-, and chimpanzee-derived recombinant adenoviral vector immunization. J. Immunol. 2013, 190, 2720–2735. [Google Scholar] [CrossRef]
- Nolz, J.C. Molecular mechanisms of CD8(+) T cell trafficking and localization. Cell Mol. Life Sci. 2015, 72, 2461–2473. [Google Scholar] [CrossRef]
- Hevey, M.; Negley, D.; Pushko, P.; Smith, J.; Schmaljohn, A. Marburg virus vaccines based upon alphavirus replicons protect guinea pigs and nonhuman primates. Virology 1998, 251, 28–37. [Google Scholar] [CrossRef]
- Feltkamp, M.C.; Vierboom, M.P.; Kast, W.M.; Melief, C.J. Efficient MHC class I-peptide binding is required but does not ensure MHC class I-restricted immunogenicity. Mol. Immunol. 1994, 31, 1391–1401. [Google Scholar] [CrossRef]
- Croft, N.P.; Smith, S.A.; Pickering, J.; Sidney, J.; Peters, B.; Faridi, P.; Witney, M.J.; Sebastian, P.; Flesch, I.E.A.; Heading, S.L.; et al. Most viral peptides displayed by class I MHC on infected cells are immunogenic. Proc. Natl. Acad. Sci. USA 2019, 116, 3112–3117. [Google Scholar] [CrossRef] [PubMed]
- Dulin, N.; Spanier, A.; Merino, K.; Hutter, J.N.; Waterman, P.E.; Lee, C.; Hamer, M.J. Systematic review of Marburg virus vaccine nonhuman primate studies and human clinical trials. Vaccine 2021, 39, 202–208. [Google Scholar] [CrossRef] [PubMed]
- Sharma, G.; Sharma, A.R.; Kim, J.-C. Recent Advancements in the Therapeutic Development for Marburg Virus: Updates on Clinical Trials. In Current Infectious Disease Reports; Springer: Berlin/Heidelberg, Germany, 2024; pp. 1–11. [Google Scholar]
- Feizollah, A.; Anuar, N.B.; Mehdi, R.; Firdaus, A.; Sulaiman, A. Understanding COVID-19 Halal Vaccination Discourse on Facebook and Twitter Using Aspect-Based Sentiment Analysis and Text Emotion Analysis. Int. J. Environ. Res. Public Health 2022, 19, 6269. [Google Scholar] [CrossRef] [PubMed]
- Meyer, M.; Garron, T.; Lubaki, N.M.; Mire, C.E.; Fenton, K.A.; Klages, C.; Olinger, G.G.; Geisbert, T.W.; Collins, P.L.; Bukreyev, A. Aerosolized Ebola vaccine protects primates and elicits lung-resident T cell responses. J. Clin. Investig. 2015, 125, 3241–3255. [Google Scholar] [CrossRef] [PubMed]
- Su, Y.; Zhang, B.; Sun, R.; Liu, W.; Zhu, Q.; Zhang, X.; Wang, R.; Chen, C. PLGA-based biodegradable microspheres in drug delivery: Recent advances in research and application. Drug Deliv. 2021, 28, 1397–1418. [Google Scholar] [CrossRef]
- Tadros, D.M.; Eggenschwiler, S.; Racle, J.; Gfeller, D. The MHC Motif Atlas: A database of MHC binding specificities and ligands. Nucleic Acids Res. 2023, 51, D428–D437. [Google Scholar] [CrossRef]
- O’Connor, S.L.; Blasky, A.J.; Pendley, C.J.; Becker, E.A.; Wiseman, R.W.; Karl, J.A.; Hughes, A.L.; O’Connor, D.H. Comprehensive characterization of MHC class II haplotypes in Mauritian cynomolgus macaques. Immunogenetics 2007, 59, 449–462. [Google Scholar] [CrossRef]



| Experiment Day | Blood Draw and ELISpot | MARV Microsphere Vaccination | TDaP Vaccination | MARV Microsphere with TpD and TT830–844 Vaccination |
|---|---|---|---|---|
| Day 0 (Baseline) | X | X | ||
| Day 6 | X | X | ||
| Day 13 | X | X | ||
| Day 21 | X | X | ||
| Day 28 | X | |||
| Day 63 | X | X | ||
| Day 81 | No ELISpot | X | ||
| Day 84 | X | X | ||
| Day 110 | X | X | X | |
| Day 150 | No ELISpot | X | X | |
| Day 164 | X |
| MARV Protein Name | Accession Number | VaxiJen Overall Protective Antigen Prediction Score |
|---|---|---|
| VP30 | ABA87128.1 | 0.5636 |
| glycoprotein GP | CAA78117.1 | 0.5481 |
| VP24 | ABA87129.1 | 0.5423 |
| Nucleoprotein (NP) | ABE27012.1 | 0.4784 |
| Polymerase (L) | ABA87130.1 | 0.4428 |
| VP35 | ABA87125.1 | 0.4316 |
| matrix protein VP40 | ABA87126.1 | 0.4107 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Harris, P.E.; Burkholz, S.; Herst, C.V.; Rubsamen, R.M. Bioinformatic, Biochemical, and Immunological Mining of MHC Class I Restricted T Cell Epitopes for a Marburg Nucleoprotein Microparticle Vaccine. Vaccines 2024, 12, 322. https://doi.org/10.3390/vaccines12030322
Harris PE, Burkholz S, Herst CV, Rubsamen RM. Bioinformatic, Biochemical, and Immunological Mining of MHC Class I Restricted T Cell Epitopes for a Marburg Nucleoprotein Microparticle Vaccine. Vaccines. 2024; 12(3):322. https://doi.org/10.3390/vaccines12030322
Chicago/Turabian StyleHarris, Paul E., Scott Burkholz, Charles V. Herst, and Reid M. Rubsamen. 2024. "Bioinformatic, Biochemical, and Immunological Mining of MHC Class I Restricted T Cell Epitopes for a Marburg Nucleoprotein Microparticle Vaccine" Vaccines 12, no. 3: 322. https://doi.org/10.3390/vaccines12030322
APA StyleHarris, P. E., Burkholz, S., Herst, C. V., & Rubsamen, R. M. (2024). Bioinformatic, Biochemical, and Immunological Mining of MHC Class I Restricted T Cell Epitopes for a Marburg Nucleoprotein Microparticle Vaccine. Vaccines, 12(3), 322. https://doi.org/10.3390/vaccines12030322