Immunogenicity and Protective Efficacy of a Non-Living Anthrax Vaccine versus a Live Spore Vaccine with Simultaneous Penicillin-G Treatment in Cattle
Abstract
:1. Introduction
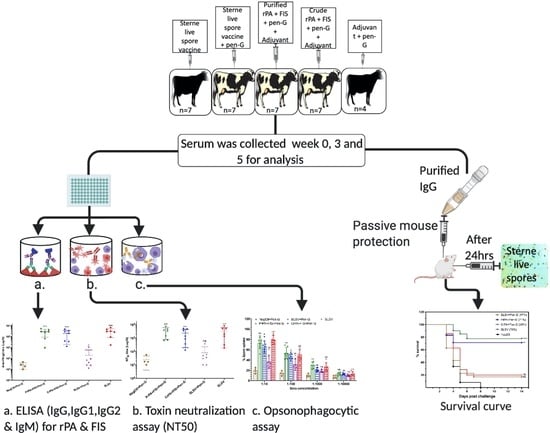
2. Materials and Methods
2.1. Recombinant Protein Expression and Purification
2.2. Formalin-Inactivated Spores (FIS) Preparation
2.3. Non-Living Anthrax Vaccines
2.4. Animals and Approvals
2.5. Enzyme-linked Immunosorbent Assay (ELISA) for Serum Immunoglobulins Titre
2.6. Toxin Neutralisation Titre (TNA) for Neutralising Antibodies Titre
2.7. Opsonophagocytic Assay
2.8. Statistical Analysis
3. Results
3.1. Humoral IgG Titre
3.2. Humoral IgM and IgG Isotypes Titre
3.3. Toxin Neutralisation Antibodies Titre (NT50)
3.4. Macrophages Spore Uptake Induced by Opsonising Antibodies
3.5. Protection Conferred on A/J Mice by Antibodies from Cattle Immune Sera
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Hambleton, P.; Carman, J.; Melling, J. Anthrax: The disease in relation to vaccines. Vaccine 1984, 2, 125–132. [Google Scholar] [CrossRef]
- Cote, C.K.; Kaatz, L.; Reinhardt, J.; Bozue, J.A.; Tobery, S.A.; Bassett, A.D.; Sanz, P.; Darnell, S.C.; Alem, F.; O’Brien, A.D.; et al. Characterization of a multi-component anthrax vaccine designed to target the initial stages of infection as well as toxaemia. J. Med. Microbiol. 2012, 61, 1380–1392. [Google Scholar] [CrossRef] [PubMed]
- Leppla, S. Anthrax Toxins. In Bacterial Toxins and Virulence Factors in Disease. Handbook of Natural Toxins; Moss, J., Iglewski, B., Vaughan, M., Tu, A.T., Eds.; Marcel Dekker: New York, NY, USA, 1995; Volume 8. [Google Scholar]
- Guidi-Rontani, C.; Weber-Levy, M.; Labruyère, E.; Mock, M. Germination of Bacillus anthracis spores within alveolar macrophages. Mol. Microbiol. 1999, 31, 9–17. [Google Scholar] [CrossRef] [PubMed]
- Turnbull, P.C.B. Anthrax in Humans and Animals, 4th ed.; World Health Organization: Geneva, Swtzerland, 2008. [Google Scholar]
- Welkos, S.; Friedländer, A.; Weeks, S.; Little, S.; Mendelson, I. In-vitro characterisation of the phagocytosis and fate of anthrax spores in macrophages and the effects of anti-PA antibody. J. Med. Microbiol. 2002, 51, 821–831. [Google Scholar] [CrossRef] [Green Version]
- Molin, F.D.; Fasanella, A.; Simonato, M.; Garofolo, G.; Montecucco, C.; Tonello, F. Ratio of lethal and edema factors in rabbit systemic anthrax. Toxicon 2008, 52, 824–828. [Google Scholar] [CrossRef]
- Leppla, S.H. Anthrax toxin edema factor: A bacterial adenylate cyclase that increases cyclic AMP concentrations of eukaryotic cells. Proc. Natl. Acad. Sci. USA 1982, 79, 3162–3166. [Google Scholar] [CrossRef] [Green Version]
- Mikesell, P.; Ivins, B.E.; Ristroph, J.D.; Dreier, T.M. Evidence for plasmid-mediated toxin production in Bacillus anthracis. Infect. Immun. 1983, 39, 371–376. [Google Scholar] [CrossRef] [Green Version]
- Sterne, M. The use of anthrax vaccines prepared from avirulent (uncapsulated) variants of Bacillus anthracis. Onderstepoort J. Vet. 1939, 13, 307–312. [Google Scholar]
- Sterne, M. The action of saponin and other excipients on the virulence and the immunizing of anthrax strains. J. S. Afr. Vet. Assoc. 1945, 16, 53–58. [Google Scholar]
- Nicol, J.; Sterne, M.L.M. The effect of large scale active immunization against anthrax. J. S. Afr. Vet. Assoc. 1942, 13, 53–63. [Google Scholar]
- Cartwright, M.E.; McChesney, A.E.; Jones, R.L. Vaccination-related anthrax in three llamas. J. Am. Veter. Med. Assoc. 1987, 191, 715–716. [Google Scholar]
- Fasanella, A.; Tonello, F.; Garofolo, G.; Muraro, L.; Carattoli, A.; Adone, R.; Montecucco, C. Protective activity and immunogenicity of two recombinant anthrax vaccines for veterinary use. Vaccine 2008, 26, 5684–5688. [Google Scholar] [CrossRef] [PubMed]
- Stepanov, A.; Marinin, L.; Pomerantsev, A.; Staritsin, N. Development of novel vaccines against anthrax in man. J. Biotechnol. 1996, 44, 155–160. [Google Scholar] [CrossRef]
- Webster, A. Inhibiting effect of antibiotics on anthrax vaccination. Aust. Veter. J. 1973, 49, 545. [Google Scholar] [CrossRef]
- Welkos, S.; Little, S.; Friedlander, A.; Fritz, D.; Fellows, P. The role of antibodies to Bacillus anthracis and anthrax toxin components in inhibiting the early stages of infection by anthrax spores. Microbiol. 2001, 147, 1677–1685. [Google Scholar] [CrossRef] [Green Version]
- Bellanti, J.A.; Lin, F.Y.C.; Chu, C.; Shiloach, J.; Leppla, S.H.; Benavides, G.A.; Karpas, A.; Moayeri, M.; Guo, C.; Robbins, J.B.; et al. Phase 1 study of a recombinant mutant protective antigen of bacillus anthracis. Clin. Vaccine Immunol. 2011, 19, 140–145. [Google Scholar] [CrossRef] [Green Version]
- Brown, B.K.; Cox, J.; Gillis, A.; VanCott, T.C.; Marovich, M.; Milazzo, M.; Antonille, T.S.; Wieczorek, L.; McKee, K.T.; Metcalfe, K.; et al. Phase I study of safety and immunogenicity of an Escherichia coli-derived recombinant protective antigen (rPA) vaccine to prevent anthrax in adults. PLoS ONE 2010, 5, e13849. [Google Scholar] [CrossRef]
- Campbell, J.D.; Clement, K.H.; Wasserman, S.S.; Donegan, S.; Chrisley, L.; Kotloff, K.L. Safety, reactogenicity, and immunogenicity of a recombinant protective antigen anthrax vaccine given to healthy adults. Hum. Vaccines 2007, 3, 205–211. [Google Scholar] [CrossRef]
- Mukarati, N.L.; Ndumnego, O.C.; Ochai, S.O.; Jauro, S.; Loveridge, A.; Van Heerden, H.; Matope, G.; Caron, A.; Hanyire, T.G.; De Garine-Wichatitsky, M.; et al. A serological survey of Bacillus anthracis reveals widespread exposure to the pathogen in free-range and captive lions in Zimbabwe. Transbound. Emerg. Dis. 2020, 30, 490–502. [Google Scholar] [CrossRef]
- Fellows, P.F.; Linscott, M.; Ivins, B.; Pitt, M.; Rossi, C.; Gibbs, P.; Friedlander, A.M. Efficacy of a human anthrax vaccine in guinea pigs, rabbits, and rhesus macaques against challenge by Bacillus anthracis isolates of diverse geographical origin. Vaccine 2001, 19, 3241–3247. [Google Scholar] [CrossRef]
- Ivins, B. Experimental anthrax vaccines: Efficacy of adjuvants combined with protective antigen against an aerosol Bacillus anthracis spore challenge in guinea pigs. Vaccine 1995, 13, 1779–1784. [Google Scholar] [CrossRef]
- Ivins, B.; Pitt, M.; Fellows, P.F.; Farchaus, J.W.; Benner, G.; Waag, D.; Little, S.; Anderson, G.W.; Gibbs, P.; Friedlander, A.M. Comparative efficacy of experimental anthrax vaccine candidates against inhalation anthrax in rhesus macaques. Vaccine 1998, 16, 1141–1148. [Google Scholar] [CrossRef]
- Ivins, B.E.; Welkos, S.L.; Little, S.F.; Crumrine, M.H.; Nelson, G.O. Immunization against anthrax with Bacillus anthracis protective antigen combined with adjuvants. Infect. Immun. 1992, 60, 662–668. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Welkos, S.; Friedlander, A.M. Comparative safety and efficacy against Bacillus anthracis of protective antigen and live vaccines in mice. Microb. Pathog. 1988, 5, 127–139. [Google Scholar] [CrossRef] [Green Version]
- Uchida, M.; Harada, T.; Enkhtuya, J.; Kusumoto, A.; Kobayashi, Y.; Chiba, S.; Shyaka, A.; Kawamoto, K. Protective effect of Bacillus anthracis surface protein EA1 against anthrax in mice. Biochem. Biophys. Res. Commun. 2012, 421, 323–328. [Google Scholar] [CrossRef]
- Majumder, S.; Das, S.; Somani, V.K.; Makam, S.S.; Kingston, J.J.; Bhatnagar, R. A bivalent protein r-PAbxpB comprising PA domain IV and exosporium protein BxpB confers protection against B. anthracis spores and toxin. Front. Immunol. 2019, 10, 498. [Google Scholar] [CrossRef]
- Hahn, U.K.; Boehm, R.; Beyer, W. DNA vaccination against anthrax in mice—Combination of anti-spore and anti-toxin components. Vaccine 2006, 24, 4569–4571. [Google Scholar] [CrossRef]
- Köhler, S.M.; Baillie, L.W.; Beyer, W. BclA and toxin antigens augment each other to protect NMRI mice from lethal Bacillus anthracis challenge. Vaccine 2015, 33, 2771–2777. [Google Scholar] [CrossRef] [Green Version]
- Majumder, S.; Das, S.; Somani, V.; Makam, S.S.; Kingston, J.J.; Bhatnagar, R. A bivalent protein r-PB, comprising PA and BclA immunodominant regions for comprehensive protection against Bacillus anthracis. Sci. Rep. 2018, 8, 7242. [Google Scholar] [CrossRef] [Green Version]
- Steichen, C.; Chen, P.; Kearney, J.F.; Turnbough, J.C.L. Identification of the immunodominant protein and other proteins of the Bacillus anthracis exosporium. J. Bacteriol. 2003, 185, 1903–1910. [Google Scholar] [CrossRef] [Green Version]
- Brossier, F.; Levy, M.; Mock, M. Anthrax spores make an essential contribution to vaccine efficacy. Infect. Immun. 2002, 70, 661–664. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cybulski, R.J.; Sanz, P.; McDaniel, D.; Darnell, S.; Bull, R.L.; O’Brien, A.D. Recombinant Bacillus anthracis spore proteins enhance protection of mice primed with suboptimal amounts of protective antigen. Vaccine 2008, 26, 4927–4939. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gauthier, Y.P.; Tournier, J.-N.; Paucod, J.C.; Corre, J.P.; Mock, M.; Goossens, P.L.; Vidal, D.R. Efficacy of a vaccine based on protective antigen and killed spores against experimental inhalational anthrax. Infect. Immun. 2008, 77, 1197–1207. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Koehler, S.M.; Büyük, F.; Celebi, O.; Demiraslan, H.; Doganay, M.; Sahin, M.; Moehring, J.; Ndumnego, O.C.; Otlu, S.; Van Heerden, H.; et al. Protection of farm goats by combinations of recombinant peptides and formalin inactivated spores from a lethal Bacillus anthracis challenge under field conditions. BMC Veter. Res. 2017, 13, 220. [Google Scholar] [CrossRef]
- Ndumnego, O.C. Comparative Studies on the Immunogenicity of the Live Spore Anthrax Vaccine Versus Non-living Vaccine Candidates in Goats and Protective Capacity of Immune Sera in Mice. Ph.D. Thesis, University of Pretoria, Pretoria, South Africa, 2016. [Google Scholar]
- Ndumnego, O.C.; Koehler, S.M.; Crafford, J.E.; Beyer, W.; Van Heerden, H. Immunogenicity of anthrax recombinant peptides and killed spores in goats and protective efficacy of immune sera in A/J mouse model. Sci. Rep. 2018, 8, 16937. [Google Scholar] [CrossRef] [Green Version]
- Vergis, J.M.; Cote, C.K.; Bozue, J.A.; Alem, F.; Ventura, C.L.; Welkos, S.; O’Brien, A.D. Immunization of mice with formalin-inactivated spores from avirulent Bacillus cereus strains provides significant protection from challenge with Bacillus anthracis Ames. Clin. Vaccine Immunol. 2012, 20, 56–65. [Google Scholar] [CrossRef] [Green Version]
- Ndumnego, O.C.; Köhler, S.M.; Crafford, J.; Van Heerden, H.; Beyer, W. Comparative analysis of the immunologic response induced by the Sterne 34F2 live spore Bacillus anthracis vaccine in a ruminant model. Veter. Immunol. Immunopathol. 2016, 178, 14–21. [Google Scholar] [CrossRef] [Green Version]
- Jauro, S.; Ndumnego, O.C.; Ellis, C.; Buys, A.; Beyer, W.; Van Heerden, H. Immunogenicity of non-living anthrax vaccine candidates in cattle and protective efficacy of immune sera in A/J mouse model compared to the sterne live spore vaccine. Pathogens 2020, 9, 557. [Google Scholar] [CrossRef]
- Coffman, R.L.; Sher, A.; Seder, R.A. Vaccine adjuvants: Putting innate immunity to work. Immunity 2010, 33, 492–503. [Google Scholar] [CrossRef] [Green Version]
- Gupta, R. Aluminum compounds as vaccine adjuvants. Adv. Drug Deliv. Rev. 1998, 32, 155–172. [Google Scholar] [CrossRef]
- Kaur, M.; Saxena, A.; Rai, A.; Bhatnagar, R. Rabies DNA vaccine encoding lysosome-targeted glycoprotein supplemented with Emulsigen-D confers complete protection in preexposure and postexposure studies in BALB/c mice. FASEB J. 2009, 24, 173–183. [Google Scholar] [CrossRef] [PubMed]
- Marrack, P.; McKee, A.S.; Munks, M.W. Towards an understanding of the adjuvant action of aluminium. Nat. Rev. Immunol. 2009, 9, 287–293. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shabana, W.; Ismail, H.M.; Mossad, W. Using Emulsigen-D as recent adjuvant in trivalent foot and mouth disease vaccine. Glob. J. Med. Res. 2018, 17, 1–9. [Google Scholar]
- Williamson, E.D.; Hodgson, I.; Walker, N.J.; Topping, A.W.; Duchars, M.G.; Mott, J.M.; Estep, J.; LeButt, C.; Flick-Smith, H.C.; Jones, H.E.; et al. Immunogenicity of recombinant protective antigen and efficacy against aerosol challenge with anthrax. Infect. Immun. 2005, 73, 5978–5987. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Holman, D.B.; Yang, W.; Alexander, T.W. Antibiotic treatment in feedlot cattle: A longitudinal study of the effect of oxytetracycline and tulathromycin on the fecal and nasopharyngeal microbiota. Microbiome 2019, 7, 86. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Casadevall, A. Antibody-based defense strategies against biological weapons. ASM News 2005, 71, 28–33. [Google Scholar]
- Kang, T.J.; Fenton, M.J.; Weiner, M.A.; Hibbs, S.; Basu, S.; Baillie, L.W.; Cross, A.S. Murine macrophages kill the vegetative form of Bacillus anthracis. Infect. Immun. 2005, 73, 7495–7501. [Google Scholar] [CrossRef] [Green Version]
- U.S. & Drugs Administration. FDA Approves New Treatment for Inhalation Anthrax; FDA: Silver Spring, MD, USA, 2016. Available online: https://www.fda.gov/news-events/press-announcements/fda-approves-new-treatment-inhalation-anthrax (accessed on 23 February 2020).









Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jauro, S.; Ndumnego, O.C.; Ellis, C.; Buys, A.; Beyer, W.; van Heerden, H. Immunogenicity and Protective Efficacy of a Non-Living Anthrax Vaccine versus a Live Spore Vaccine with Simultaneous Penicillin-G Treatment in Cattle. Vaccines 2020, 8, 595. https://doi.org/10.3390/vaccines8040595
Jauro S, Ndumnego OC, Ellis C, Buys A, Beyer W, van Heerden H. Immunogenicity and Protective Efficacy of a Non-Living Anthrax Vaccine versus a Live Spore Vaccine with Simultaneous Penicillin-G Treatment in Cattle. Vaccines. 2020; 8(4):595. https://doi.org/10.3390/vaccines8040595
Chicago/Turabian StyleJauro, Solomon, Okechukwu C. Ndumnego, Charlotte Ellis, Angela Buys, Wolfgang Beyer, and Henriette van Heerden. 2020. "Immunogenicity and Protective Efficacy of a Non-Living Anthrax Vaccine versus a Live Spore Vaccine with Simultaneous Penicillin-G Treatment in Cattle" Vaccines 8, no. 4: 595. https://doi.org/10.3390/vaccines8040595
APA StyleJauro, S., Ndumnego, O. C., Ellis, C., Buys, A., Beyer, W., & van Heerden, H. (2020). Immunogenicity and Protective Efficacy of a Non-Living Anthrax Vaccine versus a Live Spore Vaccine with Simultaneous Penicillin-G Treatment in Cattle. Vaccines, 8(4), 595. https://doi.org/10.3390/vaccines8040595