Mortality Risk Factors of Severely Injured Polytrauma Patients (Prehospital Mortality Prediction Score)
Abstract
:1. Introduction
2. Materials and Methods
3. Results
4. Discussion
4.1. Key Results
4.2. Limitations
4.3. Interpretation
4.4. Generalizability
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mohammad, A.; Branicki, F.; Abu-Zidan, F.M. Educational and clinical impact of Advanced Trauma Life Support (ATLS) courses: A systematic review. World J. Surg. 2014, 38, 322–329. [Google Scholar] [CrossRef] [PubMed]
- Saad, S. Venous glucose, serum lactate and base deficit as biochemical predictors of mortality in patients with polytrauma. Ulus. Travma Ve Acil Cerrahi Derg. 2016, 22, 29–33. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Qi, J.; Bao, L.; Yang, P.; Chen, D. Comparison of base excess, lactate and pH predicting 72-h mortality of multiple trauma. BMC Emerg. Med. 2021, 21, 80. [Google Scholar] [CrossRef]
- Heinonen, E.; Hardcastle, T.C.; Barle, H.; Muckart, D.J.J. Lactate clearance predicts outcome after major trauma. Afr. J. Emerg. Med. 2014, 4, 61–65. [Google Scholar] [CrossRef] [Green Version]
- Londoño, J.; Niño, C.; Díaz, J.; Morales, C.; Leon, J.; Bernal, E.; Vargas, C.; Mejía, L.; Hincapié, C.; Ascuntar, J.; et al. Association of Clinical Hypoperfusion Variables with Lactate Clearance and Hospital Mortality. Shock 2018, 50, 286–292. [Google Scholar] [CrossRef]
- Atik, B.; Kilinc, G.; Yarar, V. Predictive value of prognostic factors at multiple trauma patients in intensive care admission. Bratisl. Lek. Listy 2021, 122, 277–279. [Google Scholar] [CrossRef] [PubMed]
- Freitas, A.; Franzon, O. Lactate as Predictor of Mortality in Polytrauma. ABCD Arq. Bras. De Cir. Dig. 2015, 28, 163–166. [Google Scholar] [CrossRef] [Green Version]
- Emircan, S.; Ozgüç, H.; Akköse Aydın, S.; Ozdemir, F.; Köksal, O.; Bulut, M. Factors affecting mortality in patients with thorax trauma. Ulus. Travma Ve Acil Cerrahi Derg. 2011, 17, 329–333. [Google Scholar] [CrossRef]
- Rupprecht, H. The geriatric polytrauma: Risk profile and prognostic factors. Ulus. Travma Ve Acil Cerrahi Derg. 2016, 23, 156–162. [Google Scholar] [CrossRef]
- Da Costa, L.G.V.; Carmona, M.J.C.; Malbouisson, L.M.; Rizoli, S.; Rocha-Filho, J.A.; Cardoso, R.G.; Auler-Junior, J.O.C. Independent early predictors of mortality in polytrauma patients: A prospective, observational, longitudinal study. Clinics 2017, 72, 461–468. [Google Scholar] [CrossRef]
- Samuthtai, W.; Patumanond, J.; Samutrtai, P.; Charernboon, T.; Jearwattanakanok, K.; Khorana, J. Clinical Prediction Scoring Scheme for 24 h Mortality in Major Traumatic Adult Patients. Healthcare 2022, 10, 577. [Google Scholar] [CrossRef]
- Sammy, I.; Lecky, F.; Sutton, A.; Leaviss, J.; O’Cathain, A. Factors affecting mortality in older trauma patients—A systematic review and meta-analysis. Injury 2016, 47, 1170–1183. [Google Scholar] [CrossRef]
- Baker, S.P.; O’Neill, B.; Haddon, W.; Long, W.B. The injury severity score: A method for describing patients with multiple injuries and evaluating emergency care. J. Trauma 1974, 14, 187–196. [Google Scholar] [CrossRef]
- Champion, H.R.; Sacco, W.J.; Carnazzo, A.J.; Copes, W.; Fouty, W.J. Trauma score. Crit. Care Med. 1981, 9, 672–676. [Google Scholar] [CrossRef]
- Boyd, C.R.; Tolson, M.A.; Copes, W.S. Evaluating trauma care: The TRISS method. Trauma Score and the Injury Severity Score. J. Trauma 1987, 27, 370–378. [Google Scholar] [CrossRef]
- Olsson, T.; Terent, A.; Lind, L. Rapid Emergency Medicine score: A new prognostic tool for in-hospital mortality in nonsurgical emergency department patients. J. Intern. Med. 2004, 255, 579–587. [Google Scholar] [CrossRef] [PubMed]
- Knaus, W.A.; Draper, E.A.; Wagner, D.P.; Zimmerman, J.E. APACHE II: A severity of disease classification system. Crit. Care Med. 1985, 13, 818–829. [Google Scholar] [CrossRef] [PubMed]
- Lefering, R.; Huber-Wagner, S.; Nienaber, U.; Maegele, M.; Bouillon, B. Update of the trauma risk adjustment model of the TraumaRegister DGU™: The Revised Injury Severity Classification, version II. Crit. Care 2014, 18, 476. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kunitake, R.C.; Kornblith, L.Z.; Cohen, M.J.; Callcut, R.A. Trauma Early Mortality Prediction Tool (TEMPT) for assessing 28-day mortality. Trauma Surg. Acute Care Open 2018, 3, e000131. [Google Scholar] [CrossRef]
- IBM. SPSS Statistics for Windows; IBM Corporation: Armonk, NY, USA, 2013; Available online: https://www.ibm.com/support/pages/spss-statistics-220-available-download (accessed on 5 May 2023).
- Dehli, T.; Monsen, S.A.; Fredriksen, K.; Bartnes, K. Evaluation of a trauma team activation protocol revision: A prospective cohort study. Scand. J. Trauma Resusc. Emerg. Med. 2016, 24, 105. [Google Scholar] [CrossRef] [Green Version]
- Bieler, D. Polytrauma/Schwerverletzten-Behandlung: S3-Leitlinie; der Deutschen Gesellschaft für Unfallchirurgie e.V.: Berlin, Germany, 2022. [Google Scholar]
- Cleophas, T.J.; Zwinderman, A.H. Multiplicity Analysis. In Understanding Clinical Data Analysis; Cleophas, T.J., Zwinderman, A.H., Eds.; Springer International Publishing: Cham, Switzerland, 2017; pp. 177–191. [Google Scholar]
- Li, G.; Taljaard, M.; van den Heuvel, E.R.; Levine, M.A.; Cook, D.J.; Wells, G.A.; Devereaux, P.J.; Thabane, L. An introduction to multiplicity issues in clinical trials: The what, why, when and how. Int. J. Epidemiol. 2017, 46, 746–755. [Google Scholar] [CrossRef] [Green Version]
- Waydhas, C.; Bieler, D.; Hamsen, U.; Baacke, M.; Lefering, R. ISS alone, is not sufficient to correctly assign patients post hoc to trauma team requirement. Eur. J. Trauma Emerg. Surg. 2022, 48, 383–392. [Google Scholar] [CrossRef] [PubMed]
- Fitschen-Oestern, S.; Lippross, S.; Lefering, R.; Klüter, T.; Weuster, M.; Franke, G.M.; Kirsten, N.; Müller, M.; Schröder, O.; Seekamp, A.; et al. Does the time of the day affect multiple trauma care in hospitals? A retrospective analysis of data from the TraumaRegister DGU®. BMC Emerg. Med. 2021, 21, 134. [Google Scholar] [CrossRef]
- Fröhlich, M.; Caspers, M.; Lefering, R.; Driessen, A.; Bouillon, B.; Maegele, M.; Wafaisade, A.; The TraumaRegister DGU. Do elderly trauma patients receive the required treatment? Epidemiology and outcome of geriatric trauma patients treated at different levels of trauma care. Eur. J. Trauma Emerg. Surg. 2020, 46, 1463–1469. [Google Scholar] [CrossRef] [PubMed]
- Schieren, M.; Böhmer, A.B.; Lefering, R.; Paffrath, T.; Wappler, F.; Defosse, J. Impact of body mass index on outcomes after thoracic trauma—A matched-triplet analysis of the TraumaRegister DGU®. Injury 2019, 50, 96–100. [Google Scholar] [CrossRef] [PubMed]
- Höfer, C.; Lefering, R. Jahresbericht 2022—TraumaRegister DGU®: Für das Unfalljahr 2021; Klinikum Aschaffenburg-Alzenau gGmbH, Standort Aschaffenburg; TraumaRegister DGU®: Köln, Germany, 2022. [Google Scholar]







| Variable | Mean | Median | Maximum | Minimum | Valid n | Missing | Standard Deviation |
|---|---|---|---|---|---|---|---|
| age (years) | 56 | 60 | 95 | 0 | 167 | 0 | 21 |
| BMI (kg/m2) | 26.32 | 25.38 | 54.08 | 17.71 | 106 | 61 | 4.79 |
| height (cm) | 174 | 175 | 200 | 83 | 107 | 60 | 14 |
| weight (kg) | 80 | 80 | 160 | 12 | 109 | 58 | 20 |
| RR systolic (mmHG) | 136 | 136 | 230 | 30 | 160 | 7 | 32 |
| RR diastolic (mmHG) | 81 | 80 | 160 | 10 | 150 | 17 | 19 |
| temperature (°C) | 36.2 | 36.4 | 38.5 | 34 | 117 | 50 | 0.8 |
| breathing rate (1/min) | 17 | 17 | 34 | 3 | 149 | 18 | 5 |
| oxygen saturation (%) | 96.49 | 98 | 100 | 20 | 160 | 7 | 7.2 |
| heart rate (1/min) | 88 | 83 | 170 | 50 | 159 | 8 | 22 |
| GCS | 11 | 14 | 15 | 3 | 165 | 2 | 5 |
| NRS | 5 | 5 | 10 | 0 | 53 | 114 | 2 |
| pH | 7.31 | 7.33 | 7.52 | 6.8 | 148 | 19 | 0.119 |
| base excess | −2.14 | 0.7 | 8.2 | −27.8 | 133 | 34 | 6.04 |
| lactate (mmol/L) | 2.7 | 2 | 14.7 | 0.5 | 143 | 24 | 2.39 |
| CRP (mg/L) | 4.56 | 1.4 | 85.1 | 0.6 | 165 | 2 | 11.68 |
| troponin (pg/mL) | 30.96 | 8 | 565 | 0 | 144 | 23 | 83.15 |
| leukocytes (103/µL) | 11.68 | 10.57 | 41.16 | 3.27 | 166 | 1 | 5.82 |
| erythrocytes (106/µL) | 4.58 | 4.51 | 16 | 1.6 | 166 | 1 | 1.11 |
| hemoglobin (g/dL) | 14.61 | 14 | 134 | 1.4 | 166 | 1 | 9.92 |
| sodium (mmol/L) | 139.68 | 140 | 149 | 120 | 165 | 2 | 3.35 |
| potassium (mmol/L) | 4.02 | 4 | 5.7 | 3 | 161 | 6 | 0.56 |
| creatinine (mg/dL) | 1.43 | 1,03 | 51 | 0.26 | 165 | 2 | 3.97 |
| creatine kinase (U/L) | 326.8 | 232 | 2807 | 62 | 159 | 8 | 355.81 |
| Patient Characteristic | Adjusted Count | Layer n% | |
|---|---|---|---|
| hypertension | no hypertension | 96 | 57.50% |
| hypertension | 71 | 42.50% | |
| diabetes | no diabetes | 144 | 86.20% |
| diabetes type II | 23 | 13.80% | |
| COPD | no COPD | 161 | 96.40% |
| COPD | 6 | 3.60% | |
| hyperlipidemia | no hyperlipidemia | 90 | 53.90% |
| hyperlipidemia | 77 | 46.10% | |
| CHD | no CHD | 141 | 84.40% |
| CHD | 26 | 15.60% | |
| renal insufficiency | no renal insufficiency | 153 | 91.60% |
| renal insufficiency | 14 | 8.40% | |
| anticoagulation | no anticoagulation | 129 | 77.20% |
| Enoxaparin sodium | 2 | 1.20% | |
| n.f.d. | 5 | 3.00% | |
| ASA | 17 | 10.20% | |
| Phenprocoumon | 6 | 3.60% | |
| Clopidogrel | 2 | 1.20% | |
| Apixaban | 3 | 1.80% | |
| Rivaroxaban | 2 | 1.20% | |
| Edoxaban | 1 | 0.60% | |
| Calculation Steps | Variables | Significance |
|---|---|---|
| Step 1 | Age | 0.073 |
| Sex | 0.19 | |
| pH | 0.5 | |
| Lactate | 0.925 | |
| Hemoglobin | 0.58 | |
| BE | 0.463 | |
| GFR | 0.879 | |
| Hypertension | 0.32 | |
| CHD | 0.129 | |
| COPD | 0.366 | |
| Diabetes | 0.842 | |
| Accident Mechanism | 0.414 | |
| Service Shift | 0.99 | |
| CPR | 0.021 | |
| GCS | 0.033 | |
| Step 11 | Age | 0.029 |
| Sex | 0.013 | |
| CHD | 0.015 | |
| CPR | 0 | |
| GCS | 0 |
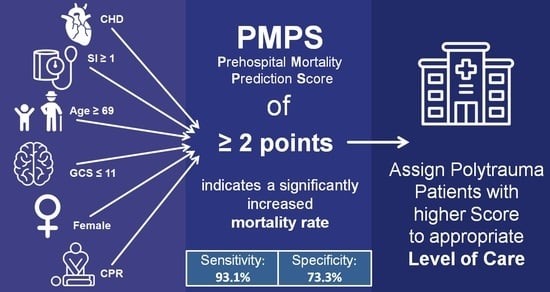
| Condition/Risk Factor | Points |
|---|---|
| Coronary Heart Disease | 1 |
| Cardiopulmonary Resuscitation | 1 |
| Age ≥ 69 years | 1 |
| Glascow Coma Scale ≤ 11 | 1 |
| Sex category (female) | 1 |
| Shock Index ≥ 1 | 1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vorbeck, J.; Bachmann, M.; Düsing, H.; Hartensuer, R. Mortality Risk Factors of Severely Injured Polytrauma Patients (Prehospital Mortality Prediction Score). J. Clin. Med. 2023, 12, 4724. https://doi.org/10.3390/jcm12144724
Vorbeck J, Bachmann M, Düsing H, Hartensuer R. Mortality Risk Factors of Severely Injured Polytrauma Patients (Prehospital Mortality Prediction Score). Journal of Clinical Medicine. 2023; 12(14):4724. https://doi.org/10.3390/jcm12144724
Chicago/Turabian StyleVorbeck, Jana, Manuel Bachmann, Helena Düsing, and René Hartensuer. 2023. "Mortality Risk Factors of Severely Injured Polytrauma Patients (Prehospital Mortality Prediction Score)" Journal of Clinical Medicine 12, no. 14: 4724. https://doi.org/10.3390/jcm12144724
APA StyleVorbeck, J., Bachmann, M., Düsing, H., & Hartensuer, R. (2023). Mortality Risk Factors of Severely Injured Polytrauma Patients (Prehospital Mortality Prediction Score). Journal of Clinical Medicine, 12(14), 4724. https://doi.org/10.3390/jcm12144724