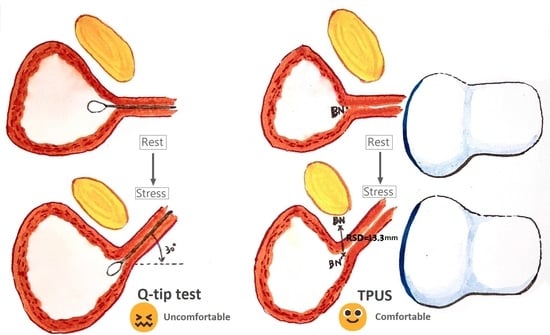
Relationship between Q-Tip Test and Urethral Hypermobility on Perineal Ultrasound
Abstract
:1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Haylen, B.T.; Maher, C.F.; Barber, M.D.; Camargo, S.; Dandolu, V.; Digesu, A.; Goldman, H.B.; Huser, M.; Milani, A.L.; Moran, P.A.; et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic organ prolapse (POP). Int. Urogynecology J. 2016, 27, 165–194. [Google Scholar] [CrossRef]
- Reynolds, W.S.; Dmochowski, R.R.; Penson, D.F. Epidemiology of stress urinary incontinence in women. Curr. Urol. Rep. 2011, 12, 370–376. [Google Scholar] [CrossRef]
- Zhang, R.Q.; Xia, M.C.; Cui, F.; Chen, J.W.; Bian, X.D.; Xie, H.J.; Shuang, W.B. Epidemiological survey of adult female stress urinary incontinence. BMC Women’s Health 2021, 21, 172. [Google Scholar] [CrossRef]
- Minassian, V.A.; Hagan, K.A.; Erekson, E.; Austin, A.M.; Carmichael, D.; Bynum, J.P.W.; Grodstein, F. The natural history of urinary incontinence subtypes in the Nurses’ Health Studies. Am. J. Obstet. Gynecol. 2020, 222, 163.E1–163.E8. [Google Scholar] [CrossRef]
- Nygaard, I.E.; Heit, M. Stress Urinary Incontinence. Obstet. Gynecol. 2004, 104, 607–620. [Google Scholar] [CrossRef]
- DeLancey, J.O. Structural support of the urethra as it relates to stress urinary incontinence: The hammock hypothesis. Am. J. Obstet. Gynecol. 1994, 170, 1713–1720. [Google Scholar] [CrossRef]
- Robinson, B.L.; Geller, E.J.; Parnell, B.A.; Crane, A.K.; Jannelli, M.L.; Wells, E.C.; Connolly, A.; Matthews, C.A. Diagnostic accuracy of visual urethral mobility exam versus Q-Tip test: A randomized crossover trial. Am. J. Obstet. Gynecol. 2012, 206, 528.E1–528.E6. [Google Scholar] [CrossRef]
- Bergman, A.; McCarthy, T.A.; Ballard, C.A.; Yanai, J. Role of the Q-tip test in evaluating stress urinary incontinence. J. Reprod. Med. 1987, 32, 273–275. [Google Scholar]
- Bump, R.C.; Mattiasson, A.; Bø, K.; Brubaker, L.P.; DeLancey, J.O.; Klarskov, P.; Shull, B.L.; Smith, A.R. The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am. J. Obstet. Gynecol. 1996, 175, 10–17. [Google Scholar] [CrossRef]
- Johnson, J.D.; Lamensdorf, H.; Hollander, I.N.; Thurman, A.E. Use of transvaginal endosonography in the evaluation of women with stress urinary incontinence. J. Urol. 1992, 147, 421–425. [Google Scholar] [CrossRef]
- Karram, M.M.; Bhatia, N.N. The Q-tip test: Standardization of the technique and its interpretation in women with urinary incontinence. Obstet. Gynecol. 1988, 71, 807–811. [Google Scholar]
- Walters, M.D.; Shields, L.E. The diagnostic value of history, physical examination, and the Q-tip cotton swab test in women with urinary incontinence. Am. J. Obstet. Gynecol. 1988, 159, 145–149. [Google Scholar] [CrossRef]
- Smith, P.P.; van Leijsen, S.A.; Heesakkers, J.P.; Abrams, P.; Smith, A.R. Can we, and do we need to, define bladder neck hypermobility and intrinsic sphincteric deficiency? ICI-RS 2011. Neurourol. Urodyn. 2012, 31, 309–312. [Google Scholar] [CrossRef]
- Yun, J.H.; Kim, J.H.; Park, S.; Lee, C. Changes in the Q-tip angle in relation to the patient position and bladder filling. BMC Urol. 2015, 15, 101. [Google Scholar] [CrossRef] [Green Version]
- Zyczynski, H.M.; Lloyd, L.K.; Kenton, K.; Menefee, S.; Boreham, M.; Stoddard, A.M. Correlation of Q-tip values and point Aa in stress-incontinent women. Obstet. Gynecol. 2007, 110, 39–43. [Google Scholar] [CrossRef]
- Mattison, M.E.; Simsiman, A.J.; Menefee, S.A. Can urethral mobility be assessed using the pelvic organ prolapse quantification system? An analysis of the correlation between point Aa and Q-tip angle in varying stages of prolapse. Urology 2006, 68, 1005–1008. [Google Scholar] [CrossRef]
- Dietz, H.P. Ultrasound imaging of the pelvic floor. Part I: Two-dimensional aspects. Ultrasound Obstet. Gynecol. Off. J. Int. Soc. Ultrasound Obstet. Gynecol. 2004, 23, 80–92. [Google Scholar] [CrossRef]
- Pregazzi, R.; Sartore, A.; Bortoli, P.; Grimaldi, E.; Troiano, L.; Guaschino, S. Perineal ultrasound evaluation of urethral angle and bladder neck mobility in women with stress urinary incontinence. BJOG Int. J. Obstet. Gynaecol. 2002, 109, 821–827. [Google Scholar] [CrossRef]
- Chen, G.D.; Su, T.H.; Lin, L.Y. Applicability of perineal sonography in anatomical evaluation of bladder neck in women with and without genuine stress incontinence. J. Clin. Ultrasound JCU 1997, 25, 189–194. [Google Scholar] [CrossRef]
- Long, C.-Y.; Hsu, S.-C.; Wu, T.-P.; Fu, J.-C.; Hsu, Y.-S.; Su, J.-H. Effect of laparoscopic hysterectomy on bladder neck and urinary symptoms. ANZJOG 2003, 43, 65–69. [Google Scholar] [CrossRef]
- Long, C.Y.; Hsu, S.C.; Chang, Y.; Chen, Y.C.; Su, J.H.; Tsai, E.M. The clinical and urodynamic effects of the tension free bladder neck sling procedure. Int. Urogynecology J. Pelvic Floor Dysfunct. 2004, 15, 344–349. [Google Scholar] [CrossRef]
- Long, C.Y.; Liu, C.M.; Wu, T.P.; Hsu, S.C.; Chang, Y.; Tsai, E.M. A randomized comparison of vesicourethral function after laparoscopic hysterectomy with and without vaginal cuff suspension. J. Minim. Invasive Gynecol. 2005, 12, 137–143. [Google Scholar] [CrossRef]
- Lin, K.L.; Juan, Y.S.; Lo, T.S.; Liu, C.M.; Tsai, E.M.; Long, C.Y. Three-dimensional ultrasonographic assessment of compression effect on urethra following tension-free vaginal tape and transobturator tape procedures. Ultrasound Obstet. Gynecol. Off. J. Int. Soc. Ultrasound Obstet. Gynecol. 2012, 39, 452–457. [Google Scholar] [CrossRef] [Green Version]
- Lin, K.-L.; Chou, S.-H.; Long, C.-Y. Effect of Er:YAG Laser for Women with Stress Urinary Incontinence. BioMed Res. Int. 2019, 2019, 7915813. [Google Scholar] [CrossRef] [Green Version]
- Lin, K.L.; Juan, Y.S.; Chou, S.H.; Long, C.Y. Ultrasonographic Assessment with Three-Dimensional Mode of the Urethral Compression Effect following Sling Surgery with and without Mesh Surgery. BioMed Res. Int. 2019, 2019, 8285351. [Google Scholar] [CrossRef] [Green Version]
- Alper, T.; Cetinkaya, M.; Okutgen, S.; Kökçü, A.; Malatyalioğlu, E. Evaluation of urethrovesical angle by ultrasound in women with and without urinary stress incontinence. Int. Urogynecology J. Pelvic Floor Dysfunct. 2001, 12, 308–311. [Google Scholar] [CrossRef]
- Dietz, H.P.; Clarke, B.; Herbison, P. Bladder neck mobility and urethral closure pressure as predictors of genuine stress incontinence. Int. Urogynecology J. Pelvic Floor Dysfunct. 2002, 13, 289–293. [Google Scholar] [CrossRef]
- Dietz, H.P.; Wilson, P.D. The influence of bladder volume on the position and mobility of the urethrovesical junction. Int. Urogynecology J. Pelvic Floor Dysfunct. 1999, 10, 3–6. [Google Scholar] [CrossRef]
- Robledo, D.; Zuluaga, L.; Bravo-Balado, A.; Domínguez, C.; Trujillo, C.G.; Caicedo, J.I.; Rondón, M.; Azuero, J.; Plata, M. Present value of the Urethral mobility test as a tool to assess Stress urinary incontinence due to Intrinsic sphincteric deficiency. Sci. Rep. 2020, 10, 20993. [Google Scholar] [CrossRef]
- Turkoglu, A.; Coskun, A.D.E.; Arinkan, S.A.; Vural, F. The role of transperineal ultrasound in the evaluation of stress urinary incontinence cases. Int. Braz J Urol Off. J. Braz. Soc. Urol. 2022, 48, 70–77. [Google Scholar] [CrossRef]


| Parameters | Mean ± SD n (%) |
|---|---|
| Age (years) | 54.5 ± 11.3 |
| Parity | 2.5 ± 1.1 |
| BMI (kg/m2) | 25.5 ± 4.6 |
| Menopause | 93 (70.5) |
| History of hysterectomy | 19 (14.4) |
| Diabetes mellitus | 8 (6.1) |
| Hypertension | 24 (18.2) |
| Current smoker | 2 (1.5) |
| Bladder-Neck Mobility > 13.3 mm | |
|---|---|
| Sensitivity | 76.5% |
| Specificity | 93.3% |
| Positive predictive value | 95.1% |
| Negative predictive value | 52.0% |
| Positive likelihood ratio | 11.5 |
| Negative likelihood ratio | 0.25 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Long, C.-Y.; Loo, Z.-X.; Wu, C.-H.; Lin, K.-L.; Yeh, C.-L.; Feng, C.-W.; Wu, P.-C. Relationship between Q-Tip Test and Urethral Hypermobility on Perineal Ultrasound. J. Clin. Med. 2023, 12, 4863. https://doi.org/10.3390/jcm12144863
Long C-Y, Loo Z-X, Wu C-H, Lin K-L, Yeh C-L, Feng C-W, Wu P-C. Relationship between Q-Tip Test and Urethral Hypermobility on Perineal Ultrasound. Journal of Clinical Medicine. 2023; 12(14):4863. https://doi.org/10.3390/jcm12144863
Chicago/Turabian StyleLong, Cheng-Yu, Zi-Xi Loo, Ching-Hu Wu, Kun-Ling Lin, Chang-Lin Yeh, Chien-Wei Feng, and Pei-Chi Wu. 2023. "Relationship between Q-Tip Test and Urethral Hypermobility on Perineal Ultrasound" Journal of Clinical Medicine 12, no. 14: 4863. https://doi.org/10.3390/jcm12144863
APA StyleLong, C. -Y., Loo, Z. -X., Wu, C. -H., Lin, K. -L., Yeh, C. -L., Feng, C. -W., & Wu, P. -C. (2023). Relationship between Q-Tip Test and Urethral Hypermobility on Perineal Ultrasound. Journal of Clinical Medicine, 12(14), 4863. https://doi.org/10.3390/jcm12144863