Management of Scar Contractures of the Hand—Our Therapeutic Strategy and Challenges
Abstract
:1. Background
2. Assessment of Scar Contractures
3. Surgical Indication and Timing
4. Treatment Strategy for Scar Contractures of the Hand
4.1. Small-Size Defect
4.2. Medium-Size Defect
4.3. Large-Size Defect
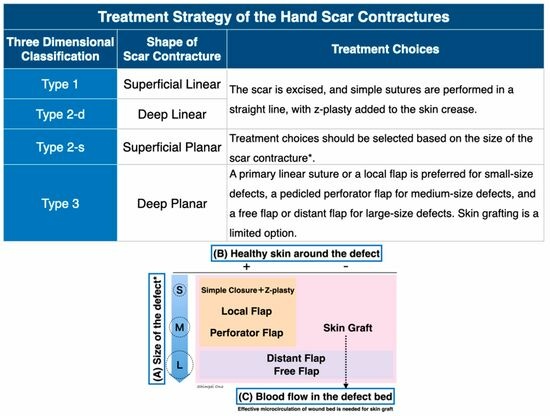
5. Treatment Choices Based on Dimensional Classification of Scar Contractures
5.1. Dimensional Classification of Scar Contractures
5.2. Scar Contracture Releasing
5.3. Treatment Policy for Each Type of Scar Contracture
5.4. Postoperative Management
6. Conclusions
Funding
Conflicts of Interest
References
- Chung, K.C.; Kotsis, S.V.; Kim, H.M.; Burke, F.D.; Wilgis, E.F. Reasons why rheumatoid arthritis patients seek surgical treatment for hand deformities. J. Hand Surg. Am. 2006, 31, 289–294. [Google Scholar] [CrossRef] [PubMed]
- Bogoch, E.R.; Escott, B.G.; Ronald, K. Hand appearance as a patient motivation for surgery and a determinant of satisfaction with metacarpophalangeal joint arthroplasty for rheumatoid arthritis. J. Hand Surg. Am. 2011, 36, 1007–1014.e4. [Google Scholar] [CrossRef] [PubMed]
- Bogoch, E.R.; Judd, M.G. The hand: A second face? J. Rheumatol. 2002, 29, 2477–2483. [Google Scholar] [PubMed]
- Ogawa, R. Keloid and Hypertrophic Scars Are the Result of Chronic Inflammation in the Reticular Dermis. Int. J. Mol. Sci. 2017, 18, 606. [Google Scholar] [CrossRef] [PubMed]
- Brown, M.; Chung, K.C. Postburn Contractures of the Hand. Hand Clin. 2017, 33, 317–331. [Google Scholar] [CrossRef] [PubMed]
- Fufa, D.T.; Chuang, S.S.; Yang, J.Y. Postburn contractures of the hand. J. Hand Surg. Am. 2014, 39, 1869–1876. [Google Scholar] [CrossRef] [PubMed]
- Sorkin, M.; Cholok, D.; Levi, B. Scar Management of the Burned Hand. Hand Clin. 2017, 33, 305–315. [Google Scholar] [CrossRef] [PubMed]
- Harrison, C.A.; MacNeil, S. The mechanism of skin graft contraction: An update on current research and potential future therapies. Burns 2008, 34, 153–163. [Google Scholar] [CrossRef] [PubMed]
- Hallock, G.G.; Morris, S.F. Skin grafts and local flaps. Plast. Reconstr. Surg. 2011, 127, 5e–22e. [Google Scholar] [CrossRef] [PubMed]
- Yoshino, Y.; Kubomura, K.; Ueda, H.; Tsuge, T.; Ogawa, R. Extension of flaps associated with burn scar reconstruction: A key difference between island and skin-pedicled flaps. Burns 2018, 44, 683–691. [Google Scholar] [CrossRef] [PubMed]
- Ono, S.; Sebastin, S.J.; Yazaki, N.; Hyakusoku, H.; Chung, K.C. Clinical applications of perforator-based propeller flaps in upper limb soft tissue reconstruction. J. Hand Surg. Am. 2011, 36, 853–863. [Google Scholar] [CrossRef] [PubMed]
- Hove, C.R.; Williams, E.F., 3rd; Rodgers, B.J. Z-plasty: A concise review. Facial Plast. Surg. 2001, 17, 289–294. [Google Scholar] [CrossRef] [PubMed]
- Robotti, E.B.; Edstrom, L.E. Split-thickness plantar skin grafts for coverage in the hand and digits. J. Hand Surg. Am. 1991, 16, 143–146. [Google Scholar] [CrossRef] [PubMed]
- Hashem, A.M. Full-thickness grafting from the ulnar border of the palm: Outcome and donor-site morbidity. Ann. Plast. Surg. 2011, 67, 123–128. [Google Scholar] [CrossRef] [PubMed]
- Corps, B.V. The effect of graft thickness, donor site and graft bed on graft shrinkage in the hooded rat. Br. J. Plast. 1969, 22, 125–133. [Google Scholar] [CrossRef] [PubMed]
- Askari, M.; Cohen, M.J.; Grossman, P.H.; Kulber, D.A. The use of acellular dermal matrix in release of burn contracture scars in the hand. Plast. Reconstr. Surg. 2011, 127, 1593–1599. [Google Scholar] [CrossRef] [PubMed]
- Frame, J.D.; Still, J.; Lakhel-LeCoadou, A.; Carstens, M.H.; Lorenz, C.; Orlet, H.; Spence, R.; Berger, A.C.; Dantzer, E.; Burd, A. Use of dermal regeneration template in contracture release procedures: A multicenter evaluation. Plast. Reconstr. Surg. 2004, 113, 1330–1338. [Google Scholar] [CrossRef] [PubMed]
- Figus, A.; Leon-Villapalos, J.; Philp, B.; Dziewulski, P. Severe multiple extensive postburn contractures: A simultaneous approach with total scar tissue excision and resurfacing with dermal regeneration template. J. Burn. Care Res. 2007, 28, 913–917. [Google Scholar] [CrossRef] [PubMed]












Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cho, H.; Ono, S.; Chung, K.C. Management of Scar Contractures of the Hand—Our Therapeutic Strategy and Challenges. J. Clin. Med. 2024, 13, 1516. https://doi.org/10.3390/jcm13051516
Cho H, Ono S, Chung KC. Management of Scar Contractures of the Hand—Our Therapeutic Strategy and Challenges. Journal of Clinical Medicine. 2024; 13(5):1516. https://doi.org/10.3390/jcm13051516
Chicago/Turabian StyleCho, Hoyu, Shimpei Ono, and Kevin C. Chung. 2024. "Management of Scar Contractures of the Hand—Our Therapeutic Strategy and Challenges" Journal of Clinical Medicine 13, no. 5: 1516. https://doi.org/10.3390/jcm13051516
APA StyleCho, H., Ono, S., & Chung, K. C. (2024). Management of Scar Contractures of the Hand—Our Therapeutic Strategy and Challenges. Journal of Clinical Medicine, 13(5), 1516. https://doi.org/10.3390/jcm13051516