Neuropsychiatric Aspects of Sotos Syndrome: Explorative Review Building Multidisciplinary Bridges in Clinical Practice
Abstract
:1. Introduction
2. Materials and Methods
3. Results
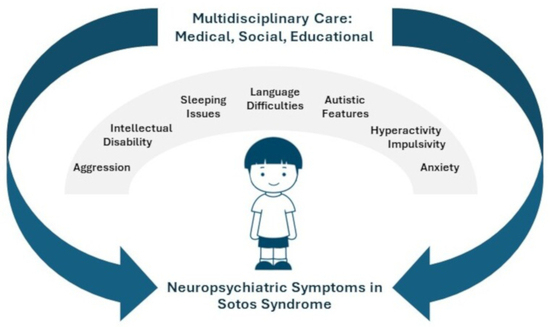
3.1. Neurobehavioral Phenotype in Sotos Syndrome
3.2. Intelligence Quotient (IQ)
3.3. Language
3.4. Aggression and Tantrums
3.5. Autistic Features
3.6. Attention Deficit Hyperactivity Disorder (ADHD)
3.7. Anxiety
3.8. Unusual Sleep Habits
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tatton-Brown, K.; Cole, T.R.P.; Rahman, N. Sotos Syndrome. In GeneReviews®; Adam, M.P., Feldman, J., Mirzaa, G.M., Pagon, R.A., Wallace, S.E., Bean, L.J.H., Gripp, K.W., Amemiya, A., Eds.; University of Washington, Seattle: Seattle, WA, USA, 1993. [Google Scholar]
- Cole, T.R.; Hughes, H.E. Sotos syndrome: A study of the diagnostic criteria and natural history. J. Med. Genet. 1994, 31, 20–32. [Google Scholar] [CrossRef]
- Tatton-Brown, K.; Rahman, N. Clinical features of NSD1-positive Sotos syndrome. Clin. Dysmorphol. 2004, 13, 199–204. [Google Scholar] [CrossRef] [PubMed]
- Kurotaki, N.; Imaizumi, K.; Harada, N.; Masuno, M.; Kondoh, T.; Nagai, T.; Ohashi, H.; Naritomi, K.; Tsukahara, M.; Makita, Y.; et al. Haploinsufficiency of NSD1 causes Sotos syndrome. Nat. Genet. 2002, 30, 365–366. [Google Scholar] [CrossRef]
- Tatton-Brown, K.; Douglas, J.; Coleman, K.; Baujat, G.; Chandler, K.; Clarke, A.; Collins, A.; Davies, S.; Faravelli, F.; Firth, H.; et al. Multiple mechanisms are implicated in the generation of 5q35 microdeletions in Sotos syndrome. J. Med. Genet. 2005, 42, 307–313. [Google Scholar] [CrossRef]
- Sotos, J.F. Sotos syndrome 1 and 2. Pediatr. Endocrinol. Rev. 2014, 12, 2–16. [Google Scholar]
- Testa, B.; Conteduca, G.; Grasso, M.; Cecconi, M.; Lantieri, F.; Baldo, C.; Arado, A.; Andraghetti, L.; Malacarne, M.; Milani, D.; et al. Molecular Analysis and Reclassification of NSD1 Gene Variants in a Cohort of Patients with Clinical Suspicion of Sotos Syndrome. Genes 2023, 14, 295. [Google Scholar] [CrossRef] [PubMed]
- Baujat, G.; Cormier-Daire, V. Sotos syndrome. Orphanet J. Rare Dis. 2007, 2, 36. [Google Scholar] [CrossRef] [PubMed]
- Foster, A.; Zachariou, A.; Loveday, C.; Ashraf, T.; Blair, E.; Clayton-Smith, J.; Dorkins, H.; Fryer, A.; Gener, B.; Goudie, D.; et al. The phenotype of Sotos syndrome in adulthood: A review of 44 individuals. Am. J. Med. Genet. C Semin. Med. Genet. 2019, 181, 502–508. [Google Scholar] [CrossRef] [PubMed]
- Muhsin, E.; Basak, G.; Banu, D.; Alper, G.; Mustafa, S. Neurodevelopment and Genetic Evaluation of Sotos Syndrome Cases with a Novel Mutation: A Single-Center Experience. J. Mol. Neurosci. 2022, 72, 149–157. [Google Scholar] [CrossRef]
- Mouridsen, S.E.; Hansen, M.B. Neuropsychiatric aspects of Sotos syndrome. A review and two case illustrations. Eur. Child. Adolesc. Psychiatry 2002, 11, 43–48. [Google Scholar] [CrossRef] [PubMed]
- Harris, J.R.; Fahrner, J.A. Disrupted epigenetics in the Sotos syndrome neurobehavioral phenotype. Curr. Opin. Psychiatry 2019, 32, 55–59. [Google Scholar] [CrossRef] [PubMed]
- Lane, C.; Milne, E.; Freeth, M. Cognition and Behaviour in Sotos Syndrome: A Systematic Review. PLoS ONE 2016, 11, e0149189. [Google Scholar] [CrossRef] [PubMed]
- Lane, C.; Milne, E.; Freeth, M. The cognitive profile of Sotos syndrome. J. Neuropsychol. 2019, 13, 240–252. [Google Scholar] [CrossRef] [PubMed]
- Sarimski, K. Behavioural and emotional characteristics in children with Sotos syndrome and learning disabilities. Dev. Med. Child. Neurol. 2003, 45, 172–178. [Google Scholar] [CrossRef]
- Sheth, K.; Moss, J.; Hyland, S.; Stinton, C.; Cole, T.; Oliver, C. The behavioral characteristics of Sotos syndrome. Am. J. Med. Genet. A 2015, 167A, 2945–2956. [Google Scholar] [CrossRef]
- Lane, C.; Van Herwegen, J.; Freeth, M. Parent-Reported Communication Abilities of Children with Sotos Syndrome: Evidence from the Children’s Communication Checklist-2. J. Autism Dev. Disord. 2019, 49, 1475–1483. [Google Scholar] [CrossRef] [PubMed]
- Lane, C.; Milne, E.; Freeth, M. Characteristics of Autism Spectrum Disorder in Sotos Syndrome. J. Autism Dev. Disord. 2017, 47, 135–143. [Google Scholar] [CrossRef]
- Siracusano, M.; Riccioni, A.; Fagiolo, I.; Segatori, E.; Gialloreti, L.E.; Galasso, C.; Curatolo, P.; Mazzone, L. COVID-19 and social responsiveness: A comparison between children with Sotos syndrome and autism. Psychiatry Res. 2021, 299, 113851. [Google Scholar] [CrossRef] [PubMed]
- Goulding-Talbot, J. An Exploration of the Psychological and Behavioural Profile of Specific Genetic Syndromes, Including Malan Syndrome and Sotos Syndrome. Ph.D. Thesis, University of Leicester, Leicester, UK, 2022. [Google Scholar]
- Stafford, C.F.; Ward, C.; Ward, S.L.D.; Sanchez-Lara, P.A. Characterization of sleep habits of children with Sotos syndrome. Am. J. Med. Genet. A 2021, 185, 2815–2820. [Google Scholar] [CrossRef]
- Khan, I.; Leventhal, B.L. Developmental Delay. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2024. [Google Scholar]
- McLaughlin, M.R. Speech and language delay in children. Am. Fam. Physician 2011, 83, 1183–1188. [Google Scholar]
- Hyman, S.L.; Levy, S.E.; Myers, S.M.; Council on Children with Disabilities, Section on Developmental and Behavioral Pediatrics; Kuo, D.Z.; Apkon, S.; Davidson, L.F.; Ellerbeck, K.A.; Foster, J.E.A.; Noritz, G.H.; et al. Identification, Evaluation, and Management of Children with Autism Spectrum Disorder. Pediatrics 2020, 145, e20193447. [Google Scholar] [CrossRef] [PubMed]
- Felt, B.T.; Biermann, B.; Christner, J.G.; Kochhar, P.; Harrison, R.V. Diagnosis and management of ADHD in children. Am. Fam. Physician 2014, 90, 456–464. [Google Scholar] [PubMed]
- Solomon, B.D.; Muenke, M. When to suspect a genetic syndrome. Am. Fam. Physician 2012, 86, 826–833. [Google Scholar] [PubMed]
- Gomes-Silva, J.M.; Ruviere, D.B.; Segatto, R.A.; de Queiroz, A.M.; de Freitas, A.C. Sotos syndrome: A case report. Spec. Care Dent. 2006, 26, 257–262. [Google Scholar] [CrossRef] [PubMed]
- Kamal, N.M.; Althobiti, J.M.; Alsaedi, A.; Bakkar, A.; Alkaabi, T. Sotos syndrome: A case report of 1st genetically proven case from Saudi Arabia with a novel mutation in NSD1 gene. Medicine 2018, 97, e12867. [Google Scholar] [CrossRef]
- Liu, X.; Chen, C.; Wan, L.; Zhu, G.; Zhao, Y.; Hu, L.; Liang, Y.; Gao, J.; Wang, J.; Yang, G. A novel nonsense variant in NSD1 gene in a female child with Sotos syndrome: A case report and literature review. Brain Behav. 2023, 13, e3290. [Google Scholar] [CrossRef]
- Favi Bocca, L.; Pereira Rodrigues, T.; Bortholin, T.; Targas Yacubian, E.M.; Carrete Junior, H.; Guaranha, M.; Silva Centeno, R. Case report: Successful anterior temporal lobectomy in drug-resistant temporal lobe epilepsy associated with Sotos syndrome. Front. Neurol. 2023, 14, 1126327. [Google Scholar] [CrossRef]
- Battig, L.; Rosch, R.; Steindl, K.; Burki, S.E.; Ramantani, G. Sotos syndrome: A pitfall in the presurgical workup of temporal lobe epilepsy. Epileptic Disord. 2021, 23, 506–510. [Google Scholar] [CrossRef] [PubMed]
| Study | Author, Year | Section in Which the Article is Included | Type of the Study | Number of Patients with Sotos Syndrome Included |
|---|---|---|---|---|
| Disrupted epigenetics in the Sotos syndrome neurobehavioral phenotype | Harris, J.R. et al., 2019 [12] | Neurobehavioral phenotype | Literature review | - |
| Cognition and Behaviour in Sotos Syndrome: A Systematic Review | Lane, C. et al., 2016 [13] | Intelligence quotient, language, aggression and tantrums, autistic features, attention deficit hyperactivity disorder, anxiety | Systematic review | 247 |
| The cognitive profile of Sotos syndrome | Lane, C. et al., 2019 [14] | Intelligence quotient | Cross-sectional | 52 |
| Behavioural and emotional characteristics in children with Sotos syndrome and learning disabilities | Sarimski, K., 2003 [15] | Language, anxiety | Cross-sectional | 27 |
| The behavioral characteristics of Sotos syndrome | Sheth K. et al., 2015 [16] | Language, aggression and tantrums, autistic features | Cross-sectional | 38 |
| Parent-Reported Communication Abilities of Children with Sotos Syndrome: Evidence from the Children’s Communication Checklist-2 | Lane, C. et al., 2019 [17] | Autistic features | Cross-sectional | 31 |
| Characteristics of Autism Spectrum Disorder in Sotos Syndrome | Lane, C. et al., 2017 [18] | Autistic features | Cross-sectional | 78 |
| COVID-19 and social responsiveness: A comparison between children with Sotos syndrome and autism | Siracusano, M. et al., 2021 [19] | Autistic features | Cross-sectional | 12 |
| An exploration of the psychological and behavioural profile of specific genetic syndromes, including Malan Syndrome and Sotos Syndrome | Goulding-Talbot, J. 2022 [20] | Anxiety | Cross-sectional | 9 |
| Characterization of sleep habits of children with Sotos syndrome | Stafford, C.F., et al., 2021 [21] | Unusual sleep habits | Cross-sectional | 49 |
| Neuropsychiatric aspects of Sotos syndrome. A review and two case illustration | Mouridsen, S.E. et al., 2002 [11] | Unusual sleep habits | Literature review and case reports | - |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lesinskiene, S.; Montvilaite, R.; Pociute, K.; Matuleviciene, A.; Utkus, A. Neuropsychiatric Aspects of Sotos Syndrome: Explorative Review Building Multidisciplinary Bridges in Clinical Practice. J. Clin. Med. 2024, 13, 2204. https://doi.org/10.3390/jcm13082204
Lesinskiene S, Montvilaite R, Pociute K, Matuleviciene A, Utkus A. Neuropsychiatric Aspects of Sotos Syndrome: Explorative Review Building Multidisciplinary Bridges in Clinical Practice. Journal of Clinical Medicine. 2024; 13(8):2204. https://doi.org/10.3390/jcm13082204
Chicago/Turabian StyleLesinskiene, Sigita, Reda Montvilaite, Kamile Pociute, Ausra Matuleviciene, and Algirdas Utkus. 2024. "Neuropsychiatric Aspects of Sotos Syndrome: Explorative Review Building Multidisciplinary Bridges in Clinical Practice" Journal of Clinical Medicine 13, no. 8: 2204. https://doi.org/10.3390/jcm13082204
APA StyleLesinskiene, S., Montvilaite, R., Pociute, K., Matuleviciene, A., & Utkus, A. (2024). Neuropsychiatric Aspects of Sotos Syndrome: Explorative Review Building Multidisciplinary Bridges in Clinical Practice. Journal of Clinical Medicine, 13(8), 2204. https://doi.org/10.3390/jcm13082204