Evaluation of the Comparability of Wantai Wan200+ Instrument with Routine Laboratory Assays for 21 Different Analytes
Abstract
:1. Introduction
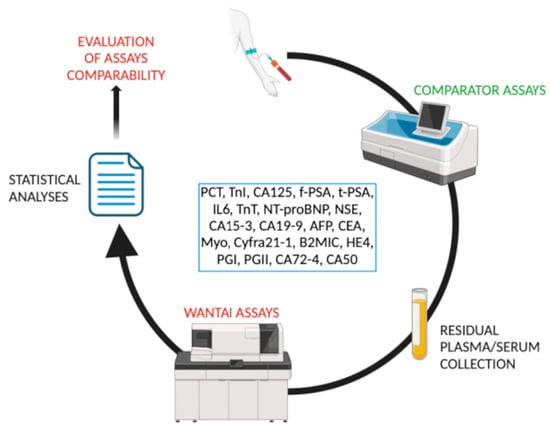
2. Materials and Methods
2.1. Sample Collection and Preparation
2.2. Sample analysis
- Plasma procalcitonin (PCT) (n = 300 samples), plasma Troponin I (TROPI) (n = 398 samples), serum CA 125 (n = 300 samples), serum-free PSA (f-PSA) (n = 300 samples) and serum total PSA (t-PSA) (n = 356 samples) samples were analyzed using a DXI 800 (Beckman Coulter, Brea, CA, USA);
- Serum IL-6 (n = 300 samples) samples were analyzed using a Snibe Diagnostic (Shenzen, China) Maglumi 4000 plus;
- Plasma troponin T (TROPT) (n = 317 samples), plasma NT-proBNP (n = 301 samples) and plasma Neuron-Specific Enolase (NSE) (n = 126 samples) samples were analyzed using a Roche (Basel, Switzerland) Cobas 8000 e801;
- Serum CA 15-3 (n = 300 samples), serum CA 19-9 (n = 302 samples), serum AFP (n = 305 samples) and serum CEA (n = 300 samples) samples were analyzed using a DiaSorin (Sallugia, Italy) Liaison XL.
- Plasma Myoglobin (n = 127 samples) samples were analyzed using a Beckman Coulter (Brea, CA, USA) DXI 800;
- Plasma Cyfra 21-1 (Cyfra) (n = 129 samples) samples were analyzed using a Roche (Basel, Switzerland) Cobas 8000 e801;
- Serum β-2 microglobulin (B2MIC) (n = 206 samples) samples were analyzed using a Binding Site (Birmingham, Great Britain), Optilite;
- Serum HE4 (n = 123 samples), serum PGI (n = 164 samples), serum PGII (n = 164 samples), serum CA 72-4 (n = 108 samples) and serum CA 50 (n = 120 samples) samples were analyzed using a Snibe Diagnostic (Shenzen, China) Maglumi 4000 plus.
- Freshly collected samples: plasma procalcitonin (PCT), plasma Troponin I (TROPI), serum CA 125, serum-free PSA (f-PSA), serum total PSA (t-PSA), serum IL-6, plasma troponin T (TROPT), plasma NT-proBNP, plasma Neuron-Specific Enolase (NSE), serum CA 15-3, serum CA 19-9, serum AFP and serum CEA samples;
- Frozen samples: plasma Myoglobin, plasma Cyfra 21-1 (Cyfra), serum β-2 microglobulin (B2MIC), serum HE4, serum PGI, serum PGII, serum CA 72-4 and serum CA 50 samples.
2.3. Wantai Wan200+ Analyses
2.4. Statistical Analyses
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Riben, M. Laboratory Automation and Middleware. Surg. Pathol. Clin. 2015, 8, 175–186. [Google Scholar] [CrossRef] [PubMed]
- Zaninotto, M.; Plebani, M. The “hospital central laboratory”: Automation, integration and clinical usefulness. Clin. Chem. Lab. Med. 2010, 48, 911–917. [Google Scholar] [CrossRef] [PubMed]
- Dolci, A.; Giavarina, D.; Pasqualetti, S.; Szőke, D.; Panteghini, M. Total laboratory automation: Do stat tests still matter? Clin. Biochem. 2017, 50, 605–611. [Google Scholar] [CrossRef] [PubMed]
- Plebani, M. Errors in laboratory medicine and patient safety: The road ahead. Clin. Chem. Lab. Med. 2007, 45, 700–707. [Google Scholar] [CrossRef] [PubMed]
- Lubin, I.M.; Astles, J.R.; Shahangian, S.; Madison, B.; Parry, R.; Schmidt, R.L.; Rubinstein, M.L. Bringing the clinical laboratory into the strategy to advance diagnostic excellence. Diagnosis 2021, 8, 281–294. [Google Scholar] [CrossRef] [PubMed]
- Lippi, G.; Da Rin, G. Advantages and limitations of total laboratory automation: A personal overview. Clin. Chem. Lab. Med. 2019, 57, 802–811. [Google Scholar] [CrossRef] [PubMed]
- Hawker, C.D. Nonanalytic Laboratory Automation: A Quarter Century of Progress. Clin. Chem. 2017, 63, 1074–1082. [Google Scholar] [CrossRef] [PubMed]
- Nam, Y.; Lee, J.H.; Kim, S.M.; Jun, S.H.; Song, S.H.; Lee, K.; Song, J. Periodic Comparability Verification and Within-Laboratory Harmonization of Clinical Chemistry Laboratory Results at a Large Healthcare Center With Multiple Instruments. Ann. Lab. Med. 2022, 42, 150–159. [Google Scholar] [CrossRef]
- Miller, W.G.; Myers, G.; Cobbaert, C.M.; Young, I.S.; Theodorsson, E.; Wielgosz, R.I.; Westwood, S.; Maniguet, S.; Gillery, P. Overcoming challenges regarding reference materials and regulations that influence global standardization of medical laboratory testing results. Clin. Chem. Lab. Med. 2022, 61, 48–54. [Google Scholar] [CrossRef]
- Panteghini, M.; Braga, F. Implementation of metrological traceability in laboratory medicine: Where we are and what is missing. Clin. Chem. Lab. Med. 2020, 58, 1200–1204. [Google Scholar] [CrossRef]
- Cava, F.; González, C.; Pascual, M.J.; Navajo, J.A.; González-Buitrago, J.M. Biological variation of interleukin 6 (IL-6) and soluble interleukin 2 receptor (sIL2R) in serum of healthy individuals. Cytokine 2000, 12, 1423–1425. [Google Scholar] [CrossRef] [PubMed]
- Carobene, A.; Guerra, E.; Locatelli, M.; Ceriotti, F.; Sandberg, S.; Fernandez-Calle, P.; Coşkun, A.; Aarsand, A.K.; European Federation of Clinical Chemistry and Laboratory Medicine Working Group on Biological Variation. Providing Correct Estimates of Biological Variation-Not an Easy Task. The Example of S100-β Protein and Neuron-Specific Enolase. Clin. Chem. 2018, 64, 1537–1539. [Google Scholar] [CrossRef]
- Ross, S.M.; Fraser, C.G. Biological variation of cardiac markers: Analytical and clinical considerations. Ann. Clin. Biochem. 1998, 35, 80–84. [Google Scholar] [CrossRef]
- Braga, F.; Ferraro, S.; Mozzi, R.; Panteghini, M. The importance of individual biology in the clinical use of serum biomarkers for ovarian cancer. Clin. Chem. Lab. Med. 2014, 52, 1625–1631. [Google Scholar] [CrossRef]
- Carobene, A.; Aarsand, A.K.; Guerra, E.; Bartlett, W.A.; Coşkun, A.; Díaz-Garzón, J.; Fernandez-Calle, P.; Jonker, N.; Locatelli, M.; Sandberg, S.; et al. European Biological Variation Study (EuBIVAS): Within- and Between-Subject Biological Variation Data for 15 Frequently Measured Proteins. Clin. Chem. 2019, 65, 1031–1041. [Google Scholar] [CrossRef] [PubMed]
- Qi, Z.; Zhang, L.; Chen, Y.; Ma, X.; Gao, X.; Du, J.; Zhang, F.; Cheng, X.; Cui, W. Biological variations of seven tumor markers. Clin. Chim. Acta 2015, 450, 233–236. [Google Scholar] [CrossRef]
- Carobene, A.; Guerra, E.; Locatelli, M.; Cucchiara, V.; Briganti, A.; Aarsand, A.K.; Coşkun, A.; Díaz-Garzón, J.; Fernandez-Calle, P.; Røraas, T.; et al. Biological variation estimates for prostate specific antigen from the European Biological Variation Study; consequences for diagnosis and monitoring of prostate cancer. Clin. Chim. Acta 2018, 486, 185–191. [Google Scholar] [CrossRef] [PubMed]
- Meijers, W.C.; van der Velde, A.R.; Muller Kobold, A.C.; Dijck-Brouwer, J.; Wu, A.H.; Jaffe, A.; de Boer, R.A. Variability of biomarkers in patients with chronic heart failure and healthy controls. Eur. J. Heart Fail. 2017, 19, 357–365. [Google Scholar] [CrossRef]
- Coşkun, A.; Aarsand, A.K.; Sandberg, S.; Guerra, E.; Locatelli, M.; Díaz-Garzón, J.; Fernandez-Calle, P.; Ceriotti, F.; Jonker, N.; Bartlett, W.A.; et al. Within- and between-subject biological variation data for tumor markers based on the European Biological Variation Study. Clin. Chem. Lab. Med. 2021, 60, 543–552. [Google Scholar] [CrossRef]
- Ceriotti, F.; Díaz-Garzón Marco, J.; Fernández-Calle, P.; Maregnani, A.; Aarsand, A.K.; Coskun, A.; Jonker, N.; Sandberg, S.; Carobene, A.; European Federation of Clinical Chemistry and Laboratory Medicine (EFLM) Working Group on Biological Variation. The European Biological Variation Study (EuBIVAS): Weekly biological variation of cardiac troponin I estimated by the use of two different high-sensitivity cardiac troponin I assays. Clin. Chem. Lab. Med. 2020, 58, 1741–1747. [Google Scholar] [CrossRef]
- Melzi d’Eril, G.; Tagnochetti, T.; Nauti, A.; Klersy, C.; Papalia, A.; Vadacca, G.; Moratti, R.; Merlini, G. Biological variation of N-terminal pro-brain natriuretic peptide in healthy individuals. Clin. Chem. 2003, 49, 1554–1555. [Google Scholar] [CrossRef] [PubMed]
- Bottani, M.; Aarsand, A.K.; Banfi, G.; Locatelli, M.; Coşkun, A.; Díaz-Garzón, J.; Fernandez-Calle, P.; Sandberg, S.; Ceriotti, F.; Carobene, A. European Biological Variation Study (EuBIVAS): Within- and between-subject biological variation estimates for serum thyroid biomarkers based on weekly samplings from 91 healthy participants. Clin. Chem. Lab. Med. 2021, 60, 523–532. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Zhao, M.; Mu, R.; Zhang, X.; Yun, K.; Shang, H. Biological variation of serum neuron-specific enolase and carbohydrate antigen 724 tumor markers. J. Clin. Lab. Anal. 2018, 32, e22327. [Google Scholar] [CrossRef] [PubMed]
- Zaninotto, M.; Graziani, M.S.; Plebani, M. The harmonization issue in laboratory medicine: The commitment of CCLM. Clin. Chem. Lab. Med. 2022, 61, 721–731. [Google Scholar] [CrossRef] [PubMed]
- Fraser, C.G.; Petersen, P.H. Analytical performance characteristics should be judged against objective quality specifications. Clin. Chem. 1999, 45, 321–323. [Google Scholar] [CrossRef] [PubMed]
- Carobene, A.; Marino, I.; Coşkun, A.; Serteser, M.; Unsal, I.; Guerra, E.; Bartlett, W.A.; Sandberg, S.; Aarsand, A.K.; Sylte, M.S.; et al. The EuBIVAS Project: Within- and Between-Subject Biological Variation Data for Serum Creatinine Using Enzymatic and Alkaline Picrate Methods and Implications for Monitoring. Clin. Chem. 2017, 63, 1527–1536. [Google Scholar] [CrossRef]
- White, G.H. Metrological traceability in clinical biochemistry. Ann. Clin. Biochem. 2011, 48, 393–409. [Google Scholar] [CrossRef] [PubMed]
- Nasrollahzadeh, D.; Aghcheli, K.; Sotoudeh, M.; Shakeri, R.; Persson, E.C.; Islami, F.; Kamangar, F.; Abnet, C.C.; Boffetta, P.; Engstrand, L.; et al. Accuracy and cut-off values of pepsinogens I, II and gastrin 17 for diagnosis of gastric fundic atrophy: Influence of gastritis. PLoS ONE 2011, 6, e26957. [Google Scholar] [CrossRef]
- Tong, Y.; Wang, H.; Zhao, Y.; He, X.; Xu, H.; Li, H.; Shuai, P.; Gong, L.; Wu, H.; Xu, H.; et al. Serum pepsinogen levels in different regions of China and its influencing factors: A multicenter cross-sectional study. BMC Gastroenterol. 2021, 21, 264. [Google Scholar] [CrossRef]
- Fu, W.; Yue, Y.; Song, Y.; Zhang, S.; Shi, J.; Zhao, R.; Wang, Q.; Zhang, R. Comparable analysis of six immunoassays for carcinoembryonic antigen detection. Heliyon 2024, 10, e25158. [Google Scholar] [CrossRef]
- Walker, C.; Shuster, A.; Weber, C.; Gebhardt, K.; Scheidegger, M.; Swartzwelder, J.; Williams, J.; Li, J. Comparison of the Siemens Atellica BRAHMS and the Abbott Architect BRAHMS Procalcitonin Assays. Ann. Clin. Lab. Sci. 2021, 51, 241–244. [Google Scholar] [PubMed]
- Dipalo, M.; Guido, L.; Micca, G.; Pittalis, S.; Locatelli, M.; Motta, A.; Bianchi, V.; Callegari, T.; Aloe, R.; Da Rin, G.; et al. Multicenter comparison of automated procalcitonin immunoassays. Pract. Lab. Med. 2015, 2, 22–28. [Google Scholar] [CrossRef] [PubMed]
- Barr, C.E.; Funston, G.; Mounce, L.T.A.; Pemberton, P.W.; Howe, J.D.; Crosbie, E.J. Comparison of two immunoassays for the measurement of serum HE4 for ovarian cancer. Pract. Lab. Med. 2021, 26, e00235. [Google Scholar] [CrossRef] [PubMed]
- Genzen, J.R.; Burnham, C.D.; Felder, R.A.; Hawker, C.D.; Lippi, G.; Peck Palmer, O.M. Challenges and Opportunities in Implementing Total Laboratory Automation. Clin. Chem. 2018, 64, 259–264. [Google Scholar] [CrossRef]
- Thomson, R.B., Jr.; McElvania, E. Total Laboratory Automation: What Is Gained, What Is Lost, and Who Can Afford It? Clin. Lab. Med. 2019, 39, 371–389. [Google Scholar] [CrossRef]



| Analyte | Cohen’s Kappa (95% CI) | Slope (95% CI) | Intercept (95% CI) | Bias (%) (95% CI) | Desirable Bias (%) Estimated by BV * |
|---|---|---|---|---|---|
| IL6 [11] | 0.846 (95%CI: 0.78 to 0.91) | 0.91 (95%CI:0.85 to 0.95) | 0.4 (95%CI: 0.15 to 0.55) | −7.01 (95%CI: −14.95 to 0.93) p = 0.083 | 15.61 |
| NSE [12] | 0.76 (95%CI: 0.64 to 0.88) | 0.91 (95%CI: 0.84 to 0.96) | 0.54 (95%CI: −0.46 to 1.97) | −3.01 (95%CI: −5.21 to −0.82) p = 0.007 | 5.76 |
| MYO [13] | 0.79 (95%CI: 0.69 to 0.89) | 1.02 (95%CI: 0.99 to 1.05) | 3.82 (95%CI: 2.02 to 5.19) | 7.94 (95%CI: 5.65 to 10.23) p < 0.001 | 12.45 |
| HE4 [14] | 0.71 (95%CI: 0.54 to 0.88) | 1.00 (95%CI: 0.93 to 1.08) | 1.48 (95%CI: −2.90 to 5.28) | 3.08 (95%CI: −2.00 to 8.16) p = 0.233 | 4.76 |
| B2MIC [15] | 0.63 (95%CI: 0.52 to 0.74) | 1.05 (95%CI: 0.93 to 1.18) | −0.19 (95%CI: −0.53 to 0.05) | −0.32 (95%CI: −0.54 to 0.10) p = 0.005 | 2.97 |
| PGII [16] | 0.75 (95%CI: 0.57 to 0.93) | 1.07 (95%CI: 1.02 to 1.11) | −0.49 (95%CI: −0.98 to 0.004) | 0.31 (95%CI: 0.02 to 0.60) p = 0.034 | 9.82 |
| t-PSA [17] | 0.94 (95%CI: 0.90 to 0.98) | 1.02 (95%CI: 0.998 to 1.03) | 0.02 (95%CI: 0.01 to 0.03) | 2.25 (95%CI: −0.43 to 4.93) p = 0.099 | 10.64 |
| CA 50 | 0.66 (95%CI: 0.04 to 1.00) | 0.89 (95%CI: 0.85 to 0.93) | 0.28 (95%CI: 0.07 to 0.41) | −0.26 (95%CI: −0.58 to 0.07) p = 0.12 | - |
| TROPT [18] | 0.80 (95%CI: 0.66 to 0.93) | 0.98 (95%CI: 0.97 to 1.01) | 0.95 (95%CI: 0.93 to 0.97) | −2.43 (95%CI: −3.25 to −1.71) p = 0.146 | 13.41 |
| CA 15-3 [19] | 0.90 (95%CI: 0.85 to 0.96) | 1.00 (95%CI: 0.97 to 1.02) | −0.63 (95%CI: −1.11 to −0.21) | 0.13 (95%CI: −1.96 to 2.22) p = 0.902 | 9.27 |
| TROPI [20] | 0.77 (95%CI: 0.71 to 0.83) | 1.03 (95%CI: 0.99 to 1.06) | 1.06 (95%CI: 1.02 to 1.10) | 4.20 (95%CI: 3.01 to 4.24) p = 0.087 | 9.72 |
| Analyte | Cohen’s Kappa (95% CI) | Slope (95% CI) | Intercept (95% CI) | Bias (%) (95% CI) | Desirable/Minimum Bias (%) Estimated by BV * |
|---|---|---|---|---|---|
| NT-proBNP [21] | 0.93 (95%CI: 0.89 to 0.97) | 1.21 (95%CI: 1.20 to 1.22) | −8.18 (95%CI: −9.56 to −7.04) | 8.45 (95%CI: 6.74 to 10.16) p < 0.0001 | 4.17/6.26 |
| Cyfra 21-1 [19] | 0.79 (95%CI: 0.67 to 0.89) | 0.85 (95%CI: 0.82 to 0.89) | 0.17 (95%CI: 0.09 to 0.24) | −9.4 (95%CI: −14.6 to −4.21) p = 0.001 | 8.87/13.30 |
| PGI [16] | 0.15 (95%CI: −0.002 to 0.31) | 0.83 (95%CI: 0.78 to 0.87) | 0.37 (95%CI: −0.87 to 3.13) | −17.72 (95%CI: −20.77 to −14.68) p < 0.001 | 6.11/9.16 |
| PCT [22] | 0.93 (95%CI: 0.88 to 0.96) | 0.76 (95%CI: 0.74 to 0.77) | 0.02 (95%CI: 0.02 to 0.03) | −2.17 (95%CI: −3.35 to −0.998) p = 0.0003 | 16.77/25.15 |
| CA 125 [19] | 0.67 (95%CI: 0.58 to 0.76) | 0.67 (95%CI: 0.65 to 0.69) | 3.38 (95%CI: 3.02 to 3.78) | −10.43 (95%CI: −13.62 to −7.23) p < 0.001 | 10.45/15.67 |
| CA 19-9 [19] | 0.67 (95%CI: 0.59 to 0.75) | 0.77 (95%CI: 0.72 to 0.84) | 1.97 (95%CI: 1.52 to 2.60) | −9.97 (95%CI: −15.57 to −4.38) p < 0.001 | 14.04/21.05 |
| AFP [19] | 0.89 (95%CI: 0.82 to 0.96) | 1.20 (95%CI: 1.18 to 1.23) | −0.56 (95%CI: −0.64 to −0.49) | 1.14 (95%CI: 0.63 to 1.66) p < 0.001 | 17.70/26.54 |
| CEA [19] | 0.98 (95%CI: 0.96 to 1.00) | 1.32 (95%CI: 1.28 to 1.36) | 0.26 (95%CI: 0.17 to 0.36) | 4.51 (95%CI: −0.05 to 9.07) p = 0.053 | 15.04/22.55 |
| f-PSA [17] | 0.12 (95%CI: 0.01 to 0.23) | 0.69 (95%CI: 0.98 to 0.70) | 0.002 (95%CI: −0.002 to 0.008) | −0.26 (95%CI: −0.30 to −0.23) p < 0.0001 | 11.69/17.53 |
| CA 72-4 [23] | 0.79 (95%CI: 0.55 to 1.00) | 2.32 (95%CI: 1.70 to 7.17) | −0.63 (95%CI: −2.96 to −0.33) | 0.57 (95%CI: 0.29 to 0.85) p < 0.0001 | 28.75/43.12 |
| Analyte | Metrological Traceability of Comparator Assays | Metrological Traceability of Wantai |
|---|---|---|
| IL6 | NIBSC 89/548 | NIBSC 89/548 |
| NSE * | Enzymun Test NSE | Inhouse reference material |
| MYO * | Access internal reference material | No high-order traceability |
| HE4 * | SNIBE internal reference material | Inhouse reference material |
| B2MIC | 1st International Standard NIBSC β2M | First International Standard for Beta2 Microglobulin NIBSC code: B2M |
| PGII * | SNIBE internal reference material | No high-order traceability |
| t-PSA | WHO 96/670 | WHO 96/670 |
| CA 50 * | SNIBE internal reference material | Inhouse reference material |
| TROPT * | Enzymun Test Troponin T (cardiac) | Inhouse reference material |
| CA 15-3 * | IRMA CA15-3 (Fujirebio) | Inhouse reference material |
| TROPI * | Access internal reference material | No high-order traceability |
| NT-proBNP * | NT-proBNP (1-76) | No high-order traceability |
| Cyfra 21-1 * | Enzymun Test Cyfra21-1 | Inhouse reference material |
| PGI * | SNIBE internal reference material | No high-order traceability |
| PCT * | Access internal reference material | No high-order traceability |
| CA 125 * | Access internal reference material | Inhouse reference material |
| CA 19-9 * | IRMA CA19-9 (Fujirebio) | Inhouse reference material |
| AFP | MRC 72/225 | First IRP WHO Reference Standard 72/225 |
| CEA | MRC 73/601 | First IRP WHO Reference Standard 73/601 |
| f-PSA | WHO 96/668 | WHO 96/668 |
| CA 72-4 * | SNIBE internal reference material | Inhouse reference material |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Talli, I.; Padoan, A.; Cosma, C.; Furlan, G.; Zaninotto, M.; Marchioro, L.; Galozzi, P.; Basso, D.; Plebani, M. Evaluation of the Comparability of Wantai Wan200+ Instrument with Routine Laboratory Assays for 21 Different Analytes. J. Clin. Med. 2024, 13, 2246. https://doi.org/10.3390/jcm13082246
Talli I, Padoan A, Cosma C, Furlan G, Zaninotto M, Marchioro L, Galozzi P, Basso D, Plebani M. Evaluation of the Comparability of Wantai Wan200+ Instrument with Routine Laboratory Assays for 21 Different Analytes. Journal of Clinical Medicine. 2024; 13(8):2246. https://doi.org/10.3390/jcm13082246
Chicago/Turabian StyleTalli, Ilaria, Andrea Padoan, Chiara Cosma, Giulia Furlan, Martina Zaninotto, Lucio Marchioro, Paola Galozzi, Daniela Basso, and Mario Plebani. 2024. "Evaluation of the Comparability of Wantai Wan200+ Instrument with Routine Laboratory Assays for 21 Different Analytes" Journal of Clinical Medicine 13, no. 8: 2246. https://doi.org/10.3390/jcm13082246
APA StyleTalli, I., Padoan, A., Cosma, C., Furlan, G., Zaninotto, M., Marchioro, L., Galozzi, P., Basso, D., & Plebani, M. (2024). Evaluation of the Comparability of Wantai Wan200+ Instrument with Routine Laboratory Assays for 21 Different Analytes. Journal of Clinical Medicine, 13(8), 2246. https://doi.org/10.3390/jcm13082246