A Study on the Sense of Parental Competence, Health Locus of Control and Levels of Anxiety, Depression and Somatization in Parents of Children with Type 1 Diabetes: Evidence on a Possible Relationship
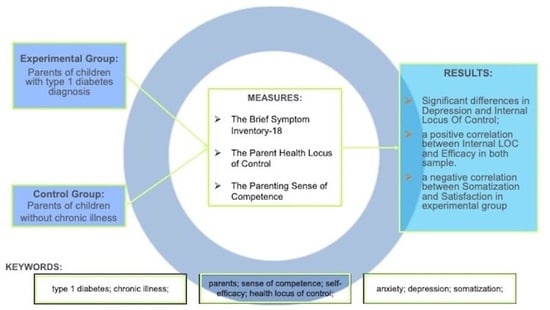
Abstract
:1. Introduction
2. Materials and Methods
2.1. Sample
2.2. Measures
3. Results
3.1. Psychological Distress
3.2. Parental Health Locus of Control
3.3. Parenting Sense of Competence
- -
- Experimental group.
3.4. Association between BSI-18 and PSOC (Experimental Group)
3.5. Association between PHLOC and PSOC (Experimental Group)
3.6. Association between BSI-18 and PHLOC (Experimental Group)
- -
- Control group.
3.7. Association between BSI-18 and PSOC (Control Group)
3.8. Association between PHLOC and PSOC (Control Group)
3.9. Association between BSI-18 and PHLOC (Control Group)
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Stein, R.E.K.; Silver, E.J. Operationalizing a conceptually based noncategorial definition. Arch. Pediatr. Adolesc. Med. 1999, 153, 68–74. [Google Scholar] [CrossRef] [PubMed]
- Lawrence, J.M.; Divers, J.; Isom, S.; Saydah, S.; Imperatore, G.; Pihoker, C.; Marcovina, S.M.; Mayer-Davis, E.J.; Hamman, R.F.; Dolan, L.; et al. Trends in Prevalence of Type 1 and Type 2 Diabetes in Children and Adolescents in the US, 2001–2017. JAMA 2021, 326, 717–727. [Google Scholar] [CrossRef] [PubMed]
- Institute for Health Metrics and Evaluation. Global Burden of Disease Study 2019 (GBD 2019) Input Sources Tool. Available online: https://vizhub.healthdata.org/gbd-results (accessed on 9 September 2023).
- Vanderniet, J.A.; Jenkins, A.J.; Donaghue, K.C. Epidemiology of Type 1 Diabetes. Curr. Cardiol. Rep. 2022, 24, 1455–1465. [Google Scholar] [CrossRef] [PubMed]
- Kazak, A.E. The social context of coping with childhood illness: Family systems and social support. In Stress and Coping in Child Health; La Greca, A.M., Siegel, L.J., Wallander, J.L., Walker, C.E., Eds.; The Guilford Press: New York, NY, USA, 1992; pp. 262–278. [Google Scholar]
- Streisand, R.; Monaghan, M. Young children with type 1 diabetes: Challenges, research, and future directions. Curr. Diabetes Rep. 2014, 14, 520. [Google Scholar] [CrossRef] [PubMed]
- Iversen, A.S.; Graue, M.; Haugstvedt, A.; Råheim, M. Being mothers and fathers of a child with type 1 diabetes aged 1 to 7 years: A phenomenological study of parents’ experiences. Int. J. Qual. Stud. Health Well-Being 2018, 13, 1487758. [Google Scholar] [CrossRef] [PubMed]
- Whittemore, R.; Jaser, S.; Chao, A.; Jang, M.; Grey, M. Psychological experience of parents of children with type 1 diabetes: A systematic mixed-studies review. Diabetes Educ. 2012, 38, 562–579. [Google Scholar] [CrossRef] [PubMed]
- Hansen, J.A.; Weissbrod, C.; Schwartz, D.D.; Taylor, W.P. Paternal involvement in pediatric Type 1 diabetes: Fathers’ and mothers’ psychological functioning and disease management. Fam. Syst. Health 2012, 30, 47–59. [Google Scholar] [CrossRef]
- Streisand, R.; Mackey, E.R.; Elliot, B.M.; Mednick, L.; Slaughter, I.M.; Turek, J.; Austin, A. Parental anxiety and depression associated with caring for a child newly diagnosed with type 1 diabetes: Opportunities for education and counseling. Patient Educ. Couns. 2008, 73, 333–338. [Google Scholar] [CrossRef] [PubMed]
- Streisand, R.; Swift, E.; Wickmark, T.; Chen, R.; Holmes, C.S. Pediatric parenting stress among parents of children with type 1 diabetes: The role of self-efficacy, responsibility, and fear. J. Pediatr. Psychol. 2005, 30, 513–521. [Google Scholar] [CrossRef]
- Bandura, A. Self-efficacy: Toward a unifying theory of behavioral change. Psychol. Rev. 1977, 84, 191–215. [Google Scholar] [CrossRef]
- Bandura, A. Health promotion by social cognitive means. Health Educ. Behav. 2004, 31, 143–164. [Google Scholar] [CrossRef]
- Girelli, L.; Cavicchiolo, E.; Alivernini, F.; Manganelli, S.; Chirico, A.; Galli, F.; Cozzolino, M.; Lucidi, F. Doping Use in High-School Students: Measuring Attitudes, Self-Efficacy, and Moral Disengagement across Genders and Countries. Front. Psychol. 2020, 11, 663. [Google Scholar] [CrossRef]
- Merkel, R.M.; Wright, T. Parental self-efficacy and online support among parents of children diagnosed with type 1 diabetes mellitus. Pediatr. Nurs. 2012, 38, 303–308. [Google Scholar]
- Leonard, B.J.; Skay, C.L.; Rheinberger, M.M. Self-management development in children and adolescents with diabetes: The role of maternal self-efficacy and conflict. J. Pediatr. Nurs. 1998, 13, 224–233. [Google Scholar] [CrossRef]
- Bassi, G.; Mancinelli, E.; Di Riso, D.; Salcuni, S. Parental Stress, Anxiety and Depression Symptoms Associated with Self-Efficacy in Paediatric Type 1 Diabetes: A Literature Review. Int. J. Environ. Res. Public Health 2020, 18, 152. [Google Scholar] [CrossRef] [PubMed]
- Peacock-Chambers, E.; Martin, J.T.; Necastro, K.A.; Cabral, H.J.; Bair-Merritt, M. The influence of parental self-efficacy and perceived control on the home learning environment of young children. Acad. Pediatr. 2017, 17, 176–183. [Google Scholar] [CrossRef]
- Rogers, H.; Matthews, J. The Parenting Sense of Competence Scale: Investigation of the factor structure, reliability, and validity for an Australian sample. Aust. Psychol. 2004, 39, 88–96. [Google Scholar] [CrossRef]
- Salari, R.; Wells, M.B.; Sarkadi, A. Child behaviour problems, parenting behaviours and parental adjustment in mothers and fathers in Sweden. Scand. J. Public Health 2014, 42, 547–553. [Google Scholar] [CrossRef] [PubMed]
- Wallston, K.A. The importance of placing measures of health locus of control beliefs in theoretical context. Health Educ. Res. 1991, 2, 251–252. [Google Scholar] [CrossRef]
- De Vellis, R.F.; De Vellis, B.M.; Blanchard, L.W.; Klotz, M.L.; Luchtok, K.; Voyce, C. Development and validation of the Parent Health Locus of Control Scales. Health Educ. Q. 1993, 20, 211–225. [Google Scholar] [CrossRef]
- Bornstein, M.H.; Cote, L.R. Mothers’ parenting cognitions in cultures of origin, acculturating cultures, and cultures of destination. Child Dev. 2004, 75, 221–235. [Google Scholar] [CrossRef] [PubMed]
- Bonichini, S.; Axia, G.; Bornstein, M.H. Validation of the Parent Health Locus of Control Scales in an Italian sample. Ital. J. Pediatr. 2009, 19, 13. [Google Scholar] [CrossRef] [PubMed]
- Cronbach, L.J. Coefficient alpha and internal structure of tests. Psychometrika 1951, 16, 297–334. [Google Scholar] [CrossRef]
- Derogatis, L.R. BSI-18: Administration, Scoring and Procedures Manual; National Computer Systems: Minneapolis, MN, USA, 2000. [Google Scholar]
- Derogatis, L.R. SCL-90-R: Symptom Checklist-90-R: Administration, Scoring and Procedures Manual; NCS Pearson Inc.: Bloomington, MN, USA, 1994. [Google Scholar]
- Derogatis, L.R. BSI, Brief Symptom Inventory: Administration, Scoring and Procedures Manual; NCS Pearson Inc.: Bloomington, MN, USA, 1993. [Google Scholar]
- Tremolada, M.; Taverna, L.; Bonichini, S.; Putti, M.C.; Pillon, M.; Biffi, A. Health locus of control in parents of children with leukemia and associations with their life perceptions and de-pression symptomatology. Children 2020, 7, 40. [Google Scholar] [CrossRef] [PubMed]
- Gibaud-Wallston, J.; Wandersman, L.P. Development and Utility of the Parenting Sense of Competence Scale. In Proceedings of the 86th Annual Convention of the American Psychological Association, Toronto, ON, Canada, 28 August–1 September 1978. [Google Scholar]
- Johnston, C.; Mash, E.J. A measures of parenting satisfaction and efficacy. J. Clin. Child Psychol. 1989, 18, 167–175. [Google Scholar] [CrossRef]
- Brislin, R. The wording and translation of research instruments. In Field Methods in Cross-Cultural Research; Lonner, W.J., Berry, J.W., Eds.; Sage: Newbury Park, CA, USA, 1989; pp. 137–164. [Google Scholar]
- Chen, Z.; Wang, J.; Carru, C.; Coradduzza, D.; Li, Z. The prevalence of depression among parents of children/adolescents with type 1 diabetes: A systematic review and meta-analysis. Front. Endocrinol. 2023, 14, 1095729. [Google Scholar] [CrossRef] [PubMed]
- Franceschi, R.; Canale, M.; Piras, E.M.; Galvagni, L.; Vivori, C.; Cauvin, V.; Soffiati, M.; Maines, E. Influence of Parental Health Locus of Control on Behavior, Self-Management and Metabolic Control, in Pediatric Patients with Type 1 Diabetes. J. Pers. Med. 2022, 12, 1590. [Google Scholar] [CrossRef]
- Gilmore, L.; Cuskelly, M. The Parenting Sense of Competence scale: Updating a classic. Child Care Health Dev. 2023, 50, e13173. [Google Scholar] [CrossRef]
| Variable | Experimental Group (n = 31) | Control Group (n = 71) |
|---|---|---|
| Female | 22 | 64 |
| Male Age, y, mean (SD) | 9 46.33 (6.22) | 7 41.18 (6.76) |
| Experimental Group | Control Group | |||||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | F-Value | p-Value | |
| BSI_Depression | 5.09 | 4.30 | 3.42 | 2.63 | 5.81 | 0.018 |
| Experimental Group | Control Group | |||||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | F-Value | p-Value | |
| PHLOC_Child | 4.38 | 0.87 | 3.27 | 0.99 | 28.82 | 0.000 |
| PHLOC_Media | 3 | 1.33 | 3.61 | 1.32 | 4.61 | 0.034 |
| PHLOC_Professional | 4.34 | 0.78 | 3.49 | 0.93 | 19.65 | 0.000 |
| Experimental Group | Control Group | |||||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | F-Value | p-Value | |
| Internal LOC | 4.19 | 0.64 | 3.82 | 0.69 | 6.42 | 0.013 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Carosi Arcangeli, I.; Celia, G.; Girelli, L.; Fioretti, C.; Cozzolino, M. A Study on the Sense of Parental Competence, Health Locus of Control and Levels of Anxiety, Depression and Somatization in Parents of Children with Type 1 Diabetes: Evidence on a Possible Relationship. J. Clin. Med. 2024, 13, 2259. https://doi.org/10.3390/jcm13082259
Carosi Arcangeli I, Celia G, Girelli L, Fioretti C, Cozzolino M. A Study on the Sense of Parental Competence, Health Locus of Control and Levels of Anxiety, Depression and Somatization in Parents of Children with Type 1 Diabetes: Evidence on a Possible Relationship. Journal of Clinical Medicine. 2024; 13(8):2259. https://doi.org/10.3390/jcm13082259
Chicago/Turabian StyleCarosi Arcangeli, Ivonne, Giovanna Celia, Laura Girelli, Chiara Fioretti, and Mauro Cozzolino. 2024. "A Study on the Sense of Parental Competence, Health Locus of Control and Levels of Anxiety, Depression and Somatization in Parents of Children with Type 1 Diabetes: Evidence on a Possible Relationship" Journal of Clinical Medicine 13, no. 8: 2259. https://doi.org/10.3390/jcm13082259
APA StyleCarosi Arcangeli, I., Celia, G., Girelli, L., Fioretti, C., & Cozzolino, M. (2024). A Study on the Sense of Parental Competence, Health Locus of Control and Levels of Anxiety, Depression and Somatization in Parents of Children with Type 1 Diabetes: Evidence on a Possible Relationship. Journal of Clinical Medicine, 13(8), 2259. https://doi.org/10.3390/jcm13082259