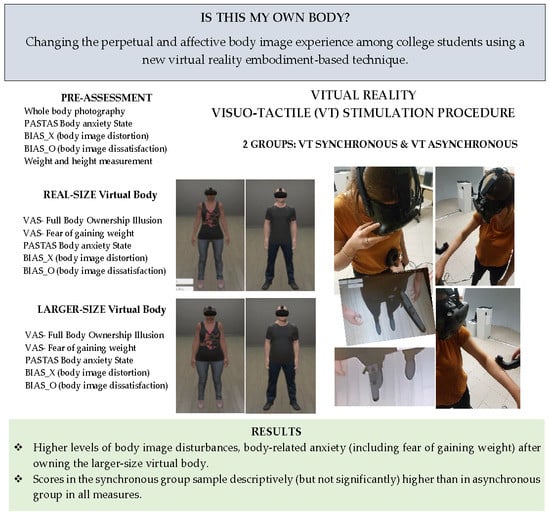
Is This My Own Body? Changing the Perceptual and Affective Body Image Experience among College Students Using a New Virtual Reality Embodiment-Based Technique
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Measures
2.2.1. Assessment of Body Image Disturbances and Body Anxiety
2.2.2. Assessment of the Full-Body Illusion (FBI)
2.3. Hardware and Software Features
2.4. Procedure
2.5. Statistical Analysis
3. Results
3.1. Descriptive Results
3.2. Statistical Analyses
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Cash, T.F. Cognitive-behavioural perspectives on body image. In Body Image: A Handbook of Theory, Research, and Clinical Practice; Cash, T.F., Pruzinsky, T., Eds.; Guilford Press: New York, NY, USA, 2002; pp. 38–46. [Google Scholar]
- Cash, T.F. Cognitive-Behavioral Perspectives on Body Image. In Body Image: A Handbook of Science, Practice, and Prevention; Cash, T.F., Smolak, L., Eds.; Guilford Press: New York, NY, USA, 2012; pp. 39–47. [Google Scholar]
- Gaudio, S.; Quattrocchi, C.C. Neural basis of a multidimensional model of body image distortion in anorexia nervosa. Neurosci. Biobehav. Rev. 2012, 36, 1839–1847. [Google Scholar] [CrossRef] [PubMed]
- Cash, T.F.; Deagle, E.A. The nature and extent of body-image disturbances in anorexia nervosa and bulimia nervosa: A meta-analysis. Int. J. Eat. Disord. 1997, 22, 107–126. [Google Scholar] [CrossRef]
- Hagman, J.; Gardner, R.M.; Brown, D.L.; Gralla, J.; Fier, J.M.; Frank, G.K.W. Body size overestimation and its association with body mass index, body dissatisfaction, and drive for thinness in anorexia nervosa. Eat. Weight Disord. 2015, 20, 449–455. [Google Scholar] [CrossRef] [PubMed]
- Ferrer-García, M.; Gutiérrez-Maldonado, J. The use of virtual reality in the study, assessment, and treatment of body image in eating disorders and nonclinical samples: A review of the literature. Body Image 2012, 9, 1–11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Legenbauer, T.; Thiemann, P.; Vocks, S. Body image disturbance in children and adolescents with eating disorders: Current evidence and future directions. Z. Kinder. Jugendpsychiatr. Psychother. 2014, 42, 51–59. [Google Scholar] [CrossRef] [PubMed]
- Espeset, E.M.S.; Gulliksen, K.S.; Nordbø, R.H.S.; Skårderud, F.; Holte, A. The link between negative emotions and eating disorder behaviour in patients with anorexia nervosa. Eur. Eat. Disord. Rev. 2012, 20, 451–460. [Google Scholar] [CrossRef]
- Maganto Mateo, C.; Cruz Saez, S. La insatisfacción corporal como variable explicativa de los trastornos alimenticios. Rev. Psicol. 2002, 10, 197–223. [Google Scholar]
- Bellisle, F.; Monneuse, M.O.; Steptoe, A.; Wardle, J. Weight concerns and eating patterns: A survey of university students in Europe. Int. J. Obes. Relat. Metab. Disord. 1995, 19, 723–730. [Google Scholar]
- Lameiras Fernández, M.; Calado Otero, M.; Rodríguez Castro, Y.; Fernández Prieto, M. Hábitos alimentarios e imagen corporal en estudiantes universitarios sin trastornos alimentarios. Rev. Int. Psicol. Clín. Salud 2003, 3, 23–33. [Google Scholar]
- Gardner, R.M.; Jappe, L.M.; Gardner, L. Development and validation of a new figural drawing scale for body-image assessment: The BIAS-BD. J. Clin. Psychol. 2009, 65, 113–122. [Google Scholar] [CrossRef]
- Gutiérrez-Maldonado, J.; Wiederhold, B.K.; Riva, G. Future Directions: How Virtual Reality Can Further Improve the Assessment and Treatment of Eating Disorders and Obesity. Cyberpsychol. Behav. Soc. Netw. 2016, 19, 148–153. [Google Scholar] [CrossRef] [PubMed]
- Gutiérrez-Maldonado, J.; Ferrer-García, M.; Dakanalis, A.; Riva, G. Virtual Reality: Applications to Eating Disorders. In The Oxford Handbook of Eating Disorders, 2nd ed.; Agras, W.S., Robinson, A.H., Eds.; Oxford University Press: Oxford, UK, 2018; Volume 19, pp. 148–153. [Google Scholar]
- Preston, C.; Ehrsson, H.H. Illusory changes in body size modulate body satisfaction in a way that is related to non-clinical eating disorder psychopathology. PLoS ONE 2014, 9, e85773. [Google Scholar] [CrossRef] [PubMed]
- Preston, C.; Kuper-Smith, B.J.; Henrik Ehrsson, H. Owning the body in the mirror: The effect of visual perspective and mirror view on the full-body illusion. Sci. Rep. 2015, 5, 18345. [Google Scholar] [CrossRef]
- Piryankova, I.V.; Wong, H.Y.; Linkenauger, S.A.; Stinson, C.; Longo, M.R.; Bülthoff, H.H.; Mohler, B.J. Owning an overweight or underweight body: Distinguishing the physical, experienced and virtual body. PLoS ONE 2014, 9, e103428. [Google Scholar] [CrossRef] [PubMed]
- Serino, S.; Pedroli, E.; Keizer, A.; Triberti, S.; Dakanalis, A.; Pallavicini, F.; Chirico, A.; Riva, G. Virtual Reality Body Swapping: A Tool for Modifying the Allocentric Memory of the Body. Cyberpsychol. Behav. Soc. Netw. 2016, 19, 127–133. [Google Scholar] [CrossRef] [PubMed]
- Botvinick, M.; Cohen, J. Rubber hands “feel” touch that eyes see. Nature 1998, 301, 756. [Google Scholar] [CrossRef] [PubMed]
- Kokkinara, E.; Slater, M. Measuring the effects through time of the influence of visuomotor and visuotactile synchronous stimulation on a virtual body ownership illusion. Perception 2014, 43, 43–58. [Google Scholar] [CrossRef]
- Petkova, V.I.; Ehrsson, H.H. If I were you: Perceptual illusion of body swapping. PLoS ONE 2008, 3, e3832. [Google Scholar] [CrossRef]
- Normand, J.M.; Giannopoulos, E.; Spanlang, B.; Slater, M. Multisensory stimulation can induce an illusion of larger belly size in immersive virtual reality. PLoS ONE 2011, 6, e16128. [Google Scholar] [CrossRef]
- Keizer, A.; van Elburg, A.; Helms, R.; Dijkerman, H.C. A virtual reality full body illusion improves body image disturbance in anorexia nervosa. PLoS ONE 2016, 11, e0163921. [Google Scholar] [CrossRef]
- Gonzalez-Franco, M.; Perez-Marcos, D.; Spanlang, B.; Slater, M. The contribution of real-time mirror reflections of motor actions on virtual body ownership in an immersive virtual environment. In Proceedings of the IEEE Virtual Reality Conference (VR), Waltham, MA, USA, 20–24 March 2010. [Google Scholar] [CrossRef]
- Slater, M.; Spanlang, B.; Sanchez-Vives, M.V.; Blanke, O. First person experience of body transfer in virtual reality. PLoS ONE 2010, 5, e10564. [Google Scholar] [CrossRef] [PubMed]
- Ehrsson, H.H. The Concept of Body Ownership and Its Relation to Multisensory Integration. In The New Handbook of Multisensory Processes; Stein, B.E., Ed.; MIT Press: Cambridge, MA, USA, 2012; pp. 775–792. [Google Scholar]
- Petkova, V.I.; Khoshnevis, M.; Ehrsson, H.H. The perspective matters! Multisensory integration in ego-centric reference frames determines full-body ownership. Front. Psychol. 2011, 2, 35. [Google Scholar] [CrossRef] [PubMed]
- Preston, C.; Newport, R. How long is your arm? Using multisensory illusions to modify body image from the third person perspective. Perception 2012, 41, 247–249. [Google Scholar] [CrossRef] [PubMed]
- Kilteni, K.; Normand, J.M.; Sanchez-Vives, M.V.; Slater, M. Extending body space in immersive virtual reality: A very long arm illusion. PLoS ONE 2012, 7, e40867. [Google Scholar] [CrossRef]
- Serino, S.; Polli, N.; Riva, G. From avatars to body swapping: The use of virtual reality for assessing and treating body-size distortion in individuals with anorexia. J. Clin. Psychol. 2018, 75, 313–322. [Google Scholar] [CrossRef]
- Ferrer-Garcia, M.; Porras-Garcia, B.; Gonzalez-Ibanez, C.; Gracia-Blanes, M.; Vilalta-Abella, F.; Pla-Sanjuanelo, J.; Gutierrez-Maldonado, J.; Achotegui-Loizate, J.; Riva, G.; Dakanalis, K.; et al. Does owning a “fatter” virtual body increase body anxiety in college students? Annu. Rev. Cyber Ther. Telemed. 2017, 15, 147–153. [Google Scholar]
- World Health Organization. ICD-10 International Statistical Classification of Diseases and Related Health Problems: Tenth Revision, 2nd ed.; World Health Organization: Geneva, Switzerland, 2004; Volume 3, ISBN 9241546492. [Google Scholar]
- Reed, D.L.; Thompson, J.K.; Brannick, M.T.; Sacco, W.P. Development and validation of the physical appearance state and trait anxiety scale (PASTAS). J. Anxiety Disord. 1991, 5, 323–332. [Google Scholar] [CrossRef]
- Garner, D. Eating Disorder Inventory-3: Professional Manual; Psychological Assessment Resources: Lutz, FL, USA, 2004. [Google Scholar]
- Schmider, E.; Ziegler, M.; Danay, E.; Beyer, L.; Bühner, M. Is it really robust? Reinvestigating the robustness of ANOVA against violations of the normal distribution assumption. Methodol. Eur. J. Res. Methods Behav. Soc. Sci. 2010, 6, 147–151. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Lawrence Erlbaum Associates: Hillsdale, NJ, USA, 1988. [Google Scholar]
- Jakatdar, T.; Cash, T.; Engle, E. Body-image thought processes: The development and initial validation of the Assessment of Body-Image Cognitive Distortions. Body Image 2006, 3, 325–333. [Google Scholar] [CrossRef]
- Maselli, A.; Slater, M. The building blocks of the full body ownership illusion. Front. Hum. Neurosci. 2013, 7, 83. [Google Scholar] [CrossRef] [Green Version]
- Tsakiris, M.; Carpenter, L.; James, D.; Fotopoulou, A. Hands only illusion: Multisensory integration elicits sense of ownership for body parts but not for non-corporeal objects. Exp. Brain Res. 2010, 204, 343–352. [Google Scholar] [CrossRef] [PubMed]
- Jansen, A.; Nederkoorn, C.; Mulkens, S. Selective visual attention for ugly and beautiful body parts in eating disorders. Behav. Res. Ther. 2005, 43, 183–196. [Google Scholar] [CrossRef]
- Tuschen-Caffier, B.; Bender, C.; Caffier, D.; Klenner, K.; Braks, K.; Svaldi, J. Selective visual attention during mirror exposure in anorexia and bulimia nervosa. PLoS ONE 2015, 10, e0145886. [Google Scholar] [CrossRef] [PubMed]
- Weinberger, N.A.; Kersting, A.; Riedel-Heller, S.G.; Luck-Sikorski, C. Body Dissatisfaction in Individuals with Obesity Compared to Normal-Weight Individuals: A Systematic Review and Meta-Analysis. Obes. Facts 2017, 9, 424–441. [Google Scholar] [CrossRef] [PubMed]
- Cornelissen, K.; Bester, A.; Cairns, P.; Tovée, M.; Cornelissen, P. The influence of personal BMI on body size estimations and sensitivity to body size change in anorexia spectrum disorders. Body Image 2015, 13, 75–85. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cornelissen, K.; McCarty, K.; Cornelissen, P.; Tovée, M. Body size estimation in women with anorexia nervosa and healthy controls using 3D avatars. Sci. Rep. 2017, 7, 15773. [Google Scholar] [CrossRef] [PubMed]


| Pre-Assessment | Real-Size VB | Larger-Size VB | ||||
|---|---|---|---|---|---|---|
| Asyn-Group n = 24 M (SD) | Syn-Group n = 26 M (SD) | Asyn-Group n = 24 M (SD) | Syn-Group n = 26 M (SD) | Asyn- Group n = 24 M (SD) | Syn-Group n = 26 M (SD) | |
| PASTAS | 5.00 (5.87) | 5.92 (5.31) | 4.96 (5.46) | 6.23 (5.77) | 5.71 (6.07) | 9.15 (6.89) |
| BIAS_X | 9.58 (16,68) | 13.65 (16.40) | 9.17 (12.22) | 12.50 (15.25) | 18.54 (18.56) | 19.62 (18.92) |
| BIAS_O | 8.75 (18.72) | 14.40 (21.81) | 7.29 (14.06) | 10.60 (19.22) | 16.67 (18.57) | 18.40 (22.39) |
| VAS-FBI | - | 48.33 (20.44) | 65.46 (19.15) | 42.71 (28.97) | 55.58 (23.07) | |
| VAS-FGW | - | 23.33 (26.77) | 33.00 (29.34) | 29.79 (29.39) | 48.77 (29.48) | |
| Time x Group | Time of Assessment | |||||
|---|---|---|---|---|---|---|
| F | p | η2 | F | p | η2 | |
| PASTAS | 3.297 | 0.041 * | 0.064 | 8.554 | 0.001 * | 0.151 |
| BIAS_X | 0.347 | 0.707 | 0.007 | 11.798 | 0.001 * | 0.197 |
| BIAS_O | 0.410 | 0.665 | 0.009 | 8.177 | 0.001 * | 0.148 |
| VAS-FBI | 0.312 | 0.579 | 0.006 | 4.130 | 0.048 * | 0.079 |
| VAS-FGW | 3.855 | 0.055 | 0.074 | 21.968 | 0.001 * | 0.314 |
| Assessment Time Conditions | ||||||
|---|---|---|---|---|---|---|
| Pre-Assessment versus Real-Size VB | Larger-Size VB versus Real-Size VB | Larger-Size VB versus Pre-Assessment | ||||
| MD | SE | MD | SE | MD | SE | |
| PASTAS | 0.133 | 0.491 | 1.837 * | 0.517 | 1.970 * | 0.584 |
| BIAS_X | 0.785 | 1.717 | 8.245 * | 1.957 | 7.460 * | 1.938 |
| BIAS_O | 2.629 | 1.915 | 8.588 * | 2.133 | 5.958 | 2.448 |
| VAS-FBI | −7.755 * | 3.816 | ||||
| VAS-FGW | 11.114 * | 2.371 | ||||
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Porras Garcia, B.; Ferrer Garcia, M.; Olszewska, A.; Yilmaz, L.; González Ibañez, C.; Gracia Blanes, M.; Gültekin, G.; Serrano Troncoso, E.; Gutiérrez Maldonado, J. Is This My Own Body? Changing the Perceptual and Affective Body Image Experience among College Students Using a New Virtual Reality Embodiment-Based Technique. J. Clin. Med. 2019, 8, 925. https://doi.org/10.3390/jcm8070925
Porras Garcia B, Ferrer Garcia M, Olszewska A, Yilmaz L, González Ibañez C, Gracia Blanes M, Gültekin G, Serrano Troncoso E, Gutiérrez Maldonado J. Is This My Own Body? Changing the Perceptual and Affective Body Image Experience among College Students Using a New Virtual Reality Embodiment-Based Technique. Journal of Clinical Medicine. 2019; 8(7):925. https://doi.org/10.3390/jcm8070925
Chicago/Turabian StylePorras Garcia, Bruno, Marta Ferrer Garcia, Agata Olszewska, Lena Yilmaz, Cristina González Ibañez, Mireia Gracia Blanes, Gamze Gültekin, Eduardo Serrano Troncoso, and José Gutiérrez Maldonado. 2019. "Is This My Own Body? Changing the Perceptual and Affective Body Image Experience among College Students Using a New Virtual Reality Embodiment-Based Technique" Journal of Clinical Medicine 8, no. 7: 925. https://doi.org/10.3390/jcm8070925
APA StylePorras Garcia, B., Ferrer Garcia, M., Olszewska, A., Yilmaz, L., González Ibañez, C., Gracia Blanes, M., Gültekin, G., Serrano Troncoso, E., & Gutiérrez Maldonado, J. (2019). Is This My Own Body? Changing the Perceptual and Affective Body Image Experience among College Students Using a New Virtual Reality Embodiment-Based Technique. Journal of Clinical Medicine, 8(7), 925. https://doi.org/10.3390/jcm8070925