Sanitization of Early Life and Microbial Dysbiosis
Abstract
:1. Introduction
2. The Modern Hospital
3. Medicalization of Birth: Home to Hospital
4. Sanitization of Birth: Caesarean Delivery
5. Sanitization of Birth: Antibiotics during Vaginal Birth
6. Sanitization in the Home after Childbirth
7. Sanitization of Breastfeeding in Canada
8. The Clean Road Ahead?
Author Contributions
Acknowledgments
Conflicts of Interest
References
- Parry, D.C. “We wanted a birth experience, not a medical experience”: Exploring Canadian women’s use of midwifery. Health Care Women Int. 2008, 29, 784–806. [Google Scholar] [CrossRef] [PubMed]
- Lerner, H.; Berg, C. A Comparison of Three Holistic Approaches to Health: One Health, EcoHealth, and Planetary Health. Front. Vet. Sci. 2017, 4, 163. [Google Scholar] [CrossRef] [PubMed]
- Whitmee, S.; Haines, A.; Beyrer, C.; Boltz, F.; Capon, A.G.; de Souza Dias, B.F.; Ezeh, A.; Frumkin, H.; Gong, P.; Head, P.; et al. Safeguarding human health in the Anthropocene epoch: Report of the Rockefeller Foundation-Lancet Commission on planetary health. Lancet 2015, 386, 1973–2028. [Google Scholar] [CrossRef]
- Zafar, N.; Wallace, C.M.; Kieffer, P.; Schroeder, P.; Schootman, M.; Hamvas, A. Improving survival of vulnerable infants increases neonatal intensive care unit nosocomial infection rate. Arch. Pediatr. Adolesc. Med. 2001, 155, 1098–1104. [Google Scholar] [CrossRef] [PubMed]
- Sevelsted, A.; Stokholm, J.; Bonnelykke, K.; Bisgaard, H. Cesarean section and chronic immune disorders. Pediatrics 2015, 135, e92–e98. [Google Scholar] [CrossRef] [PubMed]
- Houghteling, P.D.; Walker, W.A. Why is initial bacterial colonization of the intestine important to infants’ and children’s health? J. Pediatr. Gastroenterol. Nutr. 2015, 60, 294–307. [Google Scholar] [CrossRef] [PubMed]
- Gomez Pineda, F.H. Incorporation of the health care system in the west. Colomb. Med. 2015, 46, 144–149. [Google Scholar] [PubMed]
- Leavitt, J.W. What do men have to do with it? Fathers and mid-twentieth-century childbirth. Bull. Hist. Med. 2003, 77, 235–262. [Google Scholar] [CrossRef] [PubMed]
- Carter, K.C. Ignaz Semmelweis, Carl Mayrhofer, and the rise of germ theory. Med. Hist. 1985, 29, 33–53. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Vries, R.; Lemmens, T. The social and cultural shaping of medical evidence: Case studies from pharmaceutical research and obstetric science. Soc. Sci. Med. 2006, 62, 2694–2706. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Townend, J.; Rowe, R.; Brocklehurst, P.; Knight, M.; Linsell, L.; Macfarlane, A.; McCourt, C.; Newburn, M.; Marlow, N.; et al. Perinatal and maternal outcomes in planned home and obstetric unit births in women at ‘higher risk’ of complications: Secondary analysis of the Birthplace national prospective cohort study. BJOG 2015, 122, 741–753. [Google Scholar] [CrossRef] [PubMed]
- Newnham, E.C.; McKellar, L.V.; Pincombe, J.I. Paradox of the institution: Findings from a hospital labour ward ethnography. BMC Pregnancy Childbirth 2017, 17, 2. [Google Scholar] [CrossRef] [PubMed]
- Drife, J. The start of life: A history of obstetrics. Postgrad. Med. J. 2002, 78, 311–315. [Google Scholar] [CrossRef] [PubMed]
- Van Schalkwyk, J.; Van Eyk, N.; Infectious Diseases Committee. Antibiotic prophylaxis in obstetric procedures. J. Obstet. Gynaecol. Can. 2010, 32, 878–884. [Google Scholar] [CrossRef]
- Betran, A.P.; Temmerman, M.; Kingdon, C.; Mohiddin, A.; Opiyo, N.; Torloni, M.R.; Zhang, J.; Musana, O.; Wanyonyi, S.Z.; Gulmezoglu, A.M.; et al. Interventions to reduce unnecessary caesarean sections in healthy women and babies. Lancet 2018, 392, 1358–1368. [Google Scholar] [CrossRef]
- Boerma, T.; Ronsmans, C.; Melesse, D.Y.; Barros, A.J.D.; Barros, F.C.; Juan, L.; Moller, A.B.; Say, L.; Hosseinpoor, A.R.; Yi, M.; et al. Global epidemiology of use of and disparities in caesarean sections. Lancet 2018, 392, 1341–1348. [Google Scholar] [CrossRef]
- Betrán, A.P.; Ye, J.; Moller, A.B.; Zhang, J.; Gülmezoglu, A.M.; Torloni, M.R. The increasing trend in caesarean section rates: Global, regional and national estimates: 1990–2014. PLoS ONE 2016. [Google Scholar] [CrossRef] [PubMed]
- Betran, A.P.; Torloni, M.R.; Zhang, J.; Ye, J.; Mikolajczyk, R.; Deneux-Tharaux, C.; Oladapo, O.T.; Souza, J.P.; Tunçalp, O.Z.; Vogel, J.P.; et al. What is the optimal rate of caesarean section at population level? A systematic review of ecologic studies. Reprod. Health 2015, 12, 57. [Google Scholar] [CrossRef] [PubMed]
- Kelly, S.; Sprague, A.; Fell, D.B.; Murphy, P.; Aelicks, N.; Guo, Y.; Fahey, J.; Lauzon, L.; Scott, H.; Lee, L.; et al. Examining caesarean section rates in Canada using the Robson classification system. J. Obstet. Gynaecol. Can. 2013, 35, 206–214. [Google Scholar] [CrossRef]
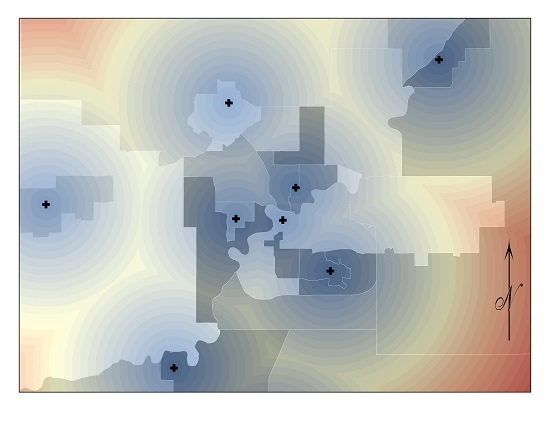
- Alberta Health. Hospital Delivery Method Age-Standardized Percent—by Geography, 1997–2014 [Digital Data]. Available online: http://www.ahw.gov.ab.ca/IHDA_Retrieval/redirectToURL.do?cat=4&subCat=767 (accessed on 12 December 2018).
- Keag, O.E.; Norman, J.E.; Stock, S.J. Long-term risks and benefits associated with cesarean delivery for mother, baby, and subsequent pregnancies: Systematic review and meta-analysis. PLoS Med. 2018, 15, e1002494. [Google Scholar] [CrossRef] [PubMed]
- Forbes, J.D.; Azad, M.B.; Vehling, L.; Tun, H.M.; Konya, T.B.; Guttman, D.S.; Field, C.J.; Lefebvre, D.; Sears, M.R.; Becker, A.B.; et al. Association of Exposure to Formula in the Hospital and Subsequent Infant Feeding Practices with Gut Microbiota and Risk of Overweight in the First Year of Life. JAMA Pediatr. 2018, 172, e181161. [Google Scholar] [CrossRef] [PubMed]
- Carter, F.A.; Frampton, C.M.; Mulder, R.T. Cesarean section and postpartum depression: A review of the evidence examining the link. Psychosom. Med. 2006, 68, 321–330. [Google Scholar] [CrossRef] [PubMed]
- Blaser, M.J.; Dominguez-Bello, M.G. The Human Microbiome before Birth. Cell Host Microbe 2016, 20, 558–560. [Google Scholar] [CrossRef] [PubMed]
- Koren, O.; Goodrich, J.K.; Cullender, T.C.; Spor, A.; Laitinen, K.; Backhed, H.K.; Gonzalez, A.; Werner, J.J.; Angenent, L.T.; Knight, R.; et al. Host remodeling of the gut microbiome and metabolic changes during pregnancy. Cell 2012, 150, 470–480. [Google Scholar] [CrossRef] [PubMed]
- Koleva, P.T.; Kim, J.S.; Scott, J.A.; Kozyrskyj, A.L. Microbial programming of health and disease starts during fetal life. Birth Defects Res C Embryo Today 2015, 105, 265–277. [Google Scholar] [CrossRef] [PubMed]
- Ho, N.T.; Li, F.; Lee-Sarwar, K.A.; Tun, H.M.; Brown, B.P.; Pannaraj, P.S.; Bender, J.M.; Azad, M.B.; Thompson, A.L.; Weiss, S.T.; et al. Meta-analysis of effects of exclusive breastfeeding on infant gut microbiota across populations. Nat. Commun. 2018, 9, 4169. [Google Scholar] [CrossRef] [PubMed]
- Tun, H.M.; Bridgman, S.L.; Chari, R.; Field, C.J.; Guttman, D.S.; Becker, A.B.; Mandhane, P.J.; Turvey, S.E.; Subbarao, P.; Sears, M.R.; et al. Roles of Birth Mode and Infant Gut Microbiota in Intergenerational Transmission of Overweight and Obesity from Mother to Offspring. JAMA Pediatr. 2018, 172, 368–377. [Google Scholar] [CrossRef] [PubMed]
- Homer, C.S.; Scarf, V.; Catling, C.; Davis, D. Culture-based versus risk-based screening for the prevention of group B streptococcal disease in newborns: A review of national guidelines. Women Birth 2014, 27, 46–51. [Google Scholar] [CrossRef] [PubMed]
- Tumbaga, P.F.; Philip, A.G.S. Perinatal Group B Streptococcal Infections: Past, Present, and Future. NeoReviews 2003, 4, e65–e72. [Google Scholar] [CrossRef]
- Le Doare, K.; O’Driscoll, M.; Turner, K.; Seedat, F.; Russell, N.J.; Seale, A.C.; Heath, P.T.; Lawn, J.E.; Baker, C.J.; Bartlett, L.; et al. Intrapartum Antibiotic Chemoprophylaxis Policies for the Prevention of Group B Streptococcal Disease Worldwide: Systematic Review. Clin. Infect. Dis. 2017, 65, S143–S151. [Google Scholar] [CrossRef] [PubMed]
- Jefferies, A.L. Management of term infants at increased risk for early-onset bacterial sepsis. Paediatr. Child Health 2017, 22, 223–228. [Google Scholar] [CrossRef] [PubMed]
- Azad, M.B.; Konya, T.; Persaud, R.R.; Guttman, D.S.; Chari, R.S.; Field, C.J.; Sears, M.R.; Mandhane, P.J.; Turvey, S.E.; Subbarao, P.; et al. Impact of maternal intrapartum antibiotics, method of birth and breastfeeding on gut microbiota during the first year of life: A prospective cohort study. BJOG 2016, 123, 983–993. [Google Scholar] [CrossRef] [PubMed]
- Nogacka, A.; Salazar, N.; Suarez, M.; Milani, C.; Arboleya, S.; Solis, G.; Fernandez, N.; Alaez, L.; Hernandez-Barranco, A.M.; de Los Reyes-Gavilan, C.G.; et al. Impact of intrapartum antimicrobial prophylaxis upon the intestinal microbiota and the prevalence of antibiotic resistance genes in vaginally delivered full-term neonates. Microbiome 2017, 5, 93. [Google Scholar] [CrossRef] [PubMed]
- Stearns, J.C.; Simioni, J.; Gunn, E.; McDonald, H.; Holloway, A.C.; Thabane, L.; Mousseau, A.; Schertzer, J.D.; Ratcliffe, E.M.; Rossi, L.; et al. Intrapartum antibiotics for GBS prophylaxis alter colonization patterns in the early infant gut microbiome of low risk infants. Sci. Rep. 2017, 7, 16527. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kurz, E.; Davis, D. Routine culture-based screening versus risk-based management for the prevention of early-onset group B streptococcus disease in the neonate: A systematic review. JBI Database Syst. Rev. Implement. Rep. 2015, 13, 206–246. [Google Scholar] [CrossRef] [PubMed]
- Lynch, K.D. Advertising Motherhood: Image, Ideology, and Consumption. Berkeley J. Sociol. 2005, 49, 32–57. [Google Scholar]
- Huffman, W. Household Production and the Demand for Food and Other Inputs: US Evidence. J. Agric. Resour. Econ. 2011, 36, 465–487. [Google Scholar]
- Curtis, V.; Biran, A.; Deverell, K.; Hughes, C.; Bellamy, K.; Drasar, B. Hygiene in the home: Relating bugs and behaviour. Soc. Sci. Med. 2003, 57, 657–672. [Google Scholar] [CrossRef]
- Kanki, B.; Curtis, V.; Mertens, T.; Cousens, S.; Traoré, E. Measuring Hygiene Behaviours: Experiences of a Comprehensive approach in Burkina Faso. In Studying Hygiene Behaviour: Issues and Experiences; Cairnross, S., Kochar, V., Eds.; Sage Publications: London, UK, 1994. [Google Scholar]
- Broege, N.; Owens, A.; Graesch, A.P.; Arnold, J.E.; Schneider, B. Calibrating measures of family activities between large- and small-scale data sets. Sociol. Methodol. 2007, 37, 119–149. [Google Scholar] [CrossRef]
- Hobbs, J.E.; Tschudy, M.; Hussey-Gardner, B.; Jennings, J.; Boss, R.D. “I Don’t Know What I Was Expecting”: Home Visit. By Neonatol. Fellows Infants Discharged NICU. Birth 2017, 44. [Google Scholar] [CrossRef] [PubMed]
- Tun, M.H.; Tun, H.M.; Mahoney, J.J.; Konya, T.B.; Guttman, D.S.; Becker, A.B.; Mandhane, P.J.; Turvey, S.E.; Subbarao, P.; Sears, M.R.; et al. Postnatal exposure to household disinfectants, infant gut microbiota and subsequent risk of overweight in children. CMAJ 2018, 190, E1097–E1107. [Google Scholar] [CrossRef] [PubMed]
- Vermeil, T.; Peters, A.; Kilpatrick, C.; Pires, D.; Allegranzi, B.; Pittet, D. Hand hygiene in hospitals: Anatomy of a revolution. J. Hosp. Infect. 2018. [Google Scholar] [CrossRef] [PubMed]
- Stevens, E.E.; Patrick, T.E.; Pickler, R. A history of infant feeding. J. Périnat. Educ. 2009, 18, 32–39. [Google Scholar] [CrossRef] [PubMed]
- Newhook, J.T.; Ludlow, V.; Newhook, L.A.; Bonia, K.; Goodridge, J.M.; Twells, L. Infant-feeding among low-income women: The social context that shapes their perspectives and experiences. Can. J. Nurs. Res. 2013, 45, 28–49. [Google Scholar] [CrossRef] [PubMed]
- Azad, M.B.; Konya, T.; Maughan, H.; Guttman, D.S.; Field, C.J.; Chari, R.S.; Sears, M.R.; Becker, A.B.; Scott, J.A.; Kozyrskyj, A.L.; et al. Gut microbiota of healthy Canadian infants: Profiles by mode of delivery and infant diet at 4 months. Can. Med. Assoc. J. 2013, 185, 385–394. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, S.; Friedberg, I.; Ivanov, I.V.; Davidson, L.A.; Goldsby, J.S.; Dahl, D.B.; Herman, D.; Wang, M.; Donovan, S.M.; Chapkin, R.S. A metagenomic study of diet-dependent interaction between gut microbiota and host in infants reveals differences in immune response. Genome Biol. 2012, 13, r32. [Google Scholar] [CrossRef] [PubMed]
- Pannaraj, P.S.; Li, F.; Cerini, C.; Bender, J.M.; Yang, S.; Rollie, A.; Adisetiyo, H.; Zabih, S.; Lincez, P.J.; Bittinger, K.; et al. Association Between Breast Milk Bacterial Communities and Establishment and Development of the Infant Gut Microbiome. JAMA Pediatr. 2017, 171, 647–654. [Google Scholar] [CrossRef] [PubMed]
- Eidelman, A.I.; Schanler, R.J.; Johnston, M.; Landers, S.; Noble, L.; Szucs, K.; Viehmann, L.; Feldman-Winter, L.; Lawrence, R.; Kim, S.; et al. Breastfeeding and the use of human milk. Pediatrics 2012, 129, e827–e841. [Google Scholar] [CrossRef]
- Spagnuolo, M.I.; Chiatto, F.; Buccigrossi, V.; Morlando, A.; Mambretti, D.; Aceto, B.; Laudiero, F.; Giordano, F.; Guarino, A. P154 Analysis of the pediatric home enteral nutrition in Campania region: Implementation rates and observed trends during the past 10 years. Dig. Liver Dis. 2018, 50, e412. [Google Scholar] [CrossRef]
- Christiaens, W.; Bracke, P. Place of birth and satisfaction with childbirth in Belgium and The Netherlands. Midwifery 2009, 25, e11–e19. [Google Scholar] [CrossRef] [PubMed]
- Ohlsson, A.; Shah, V.S. Intrapartum antibiotics for known maternal Group B streptococcal colonization. Cochrane Database Syst. Rev. 2014. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wu, P.; Feldman, A.S.; Rosas-Salazar, C.; James, K.; Escobar, G.; Gebretsadik, T.; Li, S.X.; Carroll, K.N.; Walsh, E.; Mitchel, E.; et al. Relative importance and additive effects of maternal and infant risk factors on childhood asthma. PLoS ONE 2016, 11, e0151705. [Google Scholar] [CrossRef] [PubMed]
- Wohl, D.L.; Curry, W.J.; Mauger, D.; Miller, J.; Tyrie, K. Intrapartum Antibiotics and Childhood Atopic Dermatitis. J. Am. Board Fam. Med. 2015, 28, 82–89. [Google Scholar] [CrossRef] [PubMed] [Green Version]

© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jun, S.; Drall, K.; Matenchuk, B.; McLean, C.; Nielsen, C.; Obiakor, C.V.; Van der Leek, A.; Kozyrskyj, A. Sanitization of Early Life and Microbial Dysbiosis. Challenges 2018, 9, 43. https://doi.org/10.3390/challe9020043
Jun S, Drall K, Matenchuk B, McLean C, Nielsen C, Obiakor CV, Van der Leek A, Kozyrskyj A. Sanitization of Early Life and Microbial Dysbiosis. Challenges. 2018; 9(2):43. https://doi.org/10.3390/challe9020043
Chicago/Turabian StyleJun, Shelly, Kelsea Drall, Brittany Matenchuk, Cara McLean, Charlene Nielsen, Chinwe V. Obiakor, Aaron Van der Leek, and Anita Kozyrskyj. 2018. "Sanitization of Early Life and Microbial Dysbiosis" Challenges 9, no. 2: 43. https://doi.org/10.3390/challe9020043
APA StyleJun, S., Drall, K., Matenchuk, B., McLean, C., Nielsen, C., Obiakor, C. V., Van der Leek, A., & Kozyrskyj, A. (2018). Sanitization of Early Life and Microbial Dysbiosis. Challenges, 9(2), 43. https://doi.org/10.3390/challe9020043