The Influence of Polishing and Artificial Aging on BioMed Amber® Resin’s Mechanical Properties
Abstract
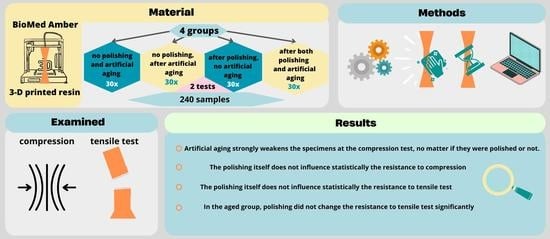
:1. Introduction
- 1.
- There was no influence of polishing on the properties of the examined resin;
- 2.
- There was no influence of artificial aging on the properties of the examined resin;
- 3.
- There was no influence when both polishing and artificial aging were applied on the properties of the examined resins;
- 4.
- No differences were observed between the polished and aged samples.
2. Materials and Methodology
2.1. Materials
2.2. Specimens’ Preparation and Artificial Aging
2.3. Compression Test
2.4. Tensile Test
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Dawood, A.; Marti, B.M.; Sauret-Jackson, V.; Darwood, A. 3D printing in dentistry. Br. Dent. J. 2016, 219, 521–529, Erratum in Br. Dent. J. 2016, 220, 86. [Google Scholar] [CrossRef] [PubMed]
- Tian, Y.; Chen, C.; Xu, X.; Wang, J.; Hou, X.; Li, K.; Lu, X.; Shi, H.; Lee, E.S.; Jiang, H.B. A Review of 3D Printing in Dentistry: Technologies, Affecting Factors, and Applications. Scanning 2021, 2021, 9950131. [Google Scholar] [CrossRef] [PubMed]
- Küffer, M.; Drescher, D.; Becker, K. Application of the Digital Workflow in Orofacial Orthopedics and Orthodontics: Printed Appliances with Skeletal Anchorage. Appl. Sci. 2022, 12, 3820. [Google Scholar] [CrossRef]
- Tack, P.; Victor, J.; Gemmel, P.; Annemans, L. 3D-printing techniques in a medical setting: A systematic literature review. Biomed. Eng. Online 2016, 15, 115. [Google Scholar] [CrossRef]
- Khorsandi, D.; Fahimipour, A.; Abasian, P.; Saber, S.S.; Seyedi, M.; Ghanavati, S.; Ahmad, A.; De Stephanis, A.A.; Taghavinezhaddilami, F.; Leonova, A.; et al. 3D and 4D printing in dentistry and maxillofacial surgery: Printing techniques, materials, and applications. Acta Biomater. 2021, 122, 26–49. [Google Scholar] [CrossRef]
- Paradowska-Stolarz, A.; Malysa, A.; Mikulewicz, M. Comparison of the Compression and Tensile Modulus of Two Chosen Resins Used in Dentistry for 3D Printing. Materials 2022, 15, 8956. [Google Scholar] [CrossRef]
- Paradowska-Stolarz, A.; Wezgowiec, J.; Mikulewicz, M. Comparison of Two Chosen 3D Printing Resins Designed for Orthodontic Use: An In Vitro Study. Materials 2023, 16, 2237. [Google Scholar] [CrossRef]
- Kul, E.; Abdulrahim, R.; Bayındır, F.; Matori, K.A.; Gül, P. Evaluation of the color stability of temporary materials produced with CAD/CAM. Dent. Med. Probl. 2021, 58, 187–191. [Google Scholar] [CrossRef]
- Grzebieluch, W.; Kowalewski, P.; Grygier, D.; Rutkowska-Gorczyca, M.; Kozakiewicz, M.; Jurczyszyn, K. Printable and Machinable Dental Restorative Composites for CAD/CAM Application-Comparison of Mechanical Properties, Fractographic, Texture and Fractal Dimension Analysis. Materials 2021, 14, 4919. [Google Scholar] [CrossRef]
- Hampe, R.; Theelke, B.; Lümkemann, N.; Stawarczyk, B. Impact of artificial aging by thermocycling on edge chipping resistance and Martens hardness of different dental CAD-CAM restorative materials. J. Prosthet. Dent. 2021, 125, 326–333. [Google Scholar] [CrossRef]
- Walczak, K.; Meißner, H.; Range, U.; Sakkas, A.; Boening, K.; Wieckiewicz, M.; Konstantinidis, I. Translucency of Zirconia Ceramics before and after Artificial Aging. J. Prosthodont. 2019, 28, e319–e324. [Google Scholar] [CrossRef] [PubMed]
- Ilie, N. Accelerated versus Slow In Vitro Aging Methods and Their Impact on Universal Chromatic, Urethane-Based Composites. Materials 2023, 16, 2143. [Google Scholar] [CrossRef] [PubMed]
- ISO 604:2002; Plastics-Determination of Compressive Properties. International Organization for Standardization: Geneva, Switzerland, 2002.
- ISO 527-1:2019; Plastics—Determination of Tensile Properties—Part 1: General Principles. International Organization for Standardization: Geneva, Switzerland, 2019.
- Vasoglou, G.; Stefanidaki, I.; Apostolopoulos, K.; Fotakidou, E.; Vasoglou, M. Accuracy of Mini-Implant Placement Using a Computer-Aided Designed Surgical Guide, with Information of Intraoral Scan and the Use of a Cone-Beam CT. Dent. J. 2022, 10, 104. [Google Scholar] [CrossRef] [PubMed]
- Malysa, A.; Wezgowiec, J.; Grzebieluch, W.; Danel, D.P.; Wieckiewicz, M. Effect of Thermocycling on the Bond Strength of Self-Adhesive Resin Cements Used for Luting CAD/CAM Ceramics to Human Dentin. Int. J. Mol. Sci. 2022, 23, 745. [Google Scholar] [CrossRef]
- Miletic, V.; Trifković, B.; Stamenković, D.; Tango, R.N.; Paravina, R.D. Effects of staining and artificial aging on optical properties of gingiva-colored resin-based restorative materials. Clin. Oral Investig. 2022, 26, 6817–6827. [Google Scholar] [CrossRef]
- Valizadeh, S.; Asiaie, Z.; Kiomarsi, N.; Kharazifard, M.J. Color stability of self-adhering composite resins in different solutions. Dent. Med. Probl. 2020, 7, 31–38. [Google Scholar] [CrossRef]
- El-Rashidy, A.A.; Abdelraouf, R.M.; Habib, N.A. Effect of two artificial aging protocols on color and gloss of single-shade versus multi-shade resin composites. BMC Oral Health 2022, 22, 321. [Google Scholar] [CrossRef]
- Gómez-Polo, C.; Martín Casado, A.M.; Quispe, N.; Gallardo, E.R.; Montero, J. Colour Changes of Acetal Resins (CAD-CAM) In Vivo. Appl. Sci. 2023, 13, 181. [Google Scholar] [CrossRef]
- Mazzitelli, C.; Paolone, G.; Sabbagh, J.; Scotti, N.; Vichi, A. Color Stability of Resin Cements after Water Aging. Polymers 2023, 15, 655. [Google Scholar] [CrossRef]
- Warnecki, M.; Sarul, M.; Kozakiewicz, M.; Zięty, A.; Babiarczuk, B.; Kawala, B.; Jurczyszyn, K. Surface Evaluation of Aligners after Immersion in Coca-Cola and Orange Juice. Materials 2022, 15, 6341. [Google Scholar] [CrossRef]
- Karatas, O.; Gul, P.; Akgul, N.; Celik, N.; Gundogdu, M.; Duymus, Z.; Seven, N. Effect of staining and bleaching on the microhardness, surface roughness and color of different composite resins. Dent Med. Probl. 2021, 58, 369–376. [Google Scholar] [CrossRef] [PubMed]
- Paolone, G.; Mandurino, M.; De Palma, F.; Mazzitelli, C.; Scotti, N.; Breschi, L.; Gherlone, E.; Cantatore, G.; Vichi, A. Color Stability of Polymer-Based Composite CAD/CAM Blocks: A Systematic Review. Polymers 2023, 15, 464. [Google Scholar] [CrossRef] [PubMed]
- Ling, L.; Ma, Y.; Malyala, R. A novel CAD/CAM resin composite block with high mechanical properties. Dent Mater. 2021, 37, 1150–1155. [Google Scholar] [CrossRef] [PubMed]
- Wieckiewicz, M.; Boening, K.W.; Richter, G.; Wieckiewicz, W. Effect of thermocycling on the shear bond strength of different resins bonded to thermoplastic foil applied in occlusal splint therapy. J. Prosthodont. 2015, 24, 220–224. [Google Scholar] [CrossRef] [PubMed]
- Matzinger, M.; Hahnel, S.; Preis, V.; Rosentritt, M. Polishing effects and wear performance of chairside CAD/CAM materials. Clin. Oral Investig. 2019, 23, 725–737. [Google Scholar] [CrossRef] [PubMed]
- Rezaie, F.; Farshbaf, M.; Dahri, M.; Masjedi, M.; Maleki, R.; Amini, F.; Wirth, J.; Moharamzadeh, K.; Weber, F.E.; Tayebi, L. 3D Printing of Dental Prostheses: Current and Emerging Applications. J. Compos. Sci. 2023, 7, 80. [Google Scholar] [CrossRef]
- Kocaagaoglu, H.; Aslan, T.; Gürbulak, A.; Albayrak, H.; Taşdemir, Z.; Gumus, H. Efficacy of polishing kits on the surface roughness and color stability of different composite resins. Niger J. Clin. Pract. 2017, 20, 557–565. [Google Scholar] [CrossRef]
- Jaramillo-Cartagena, R.; López-Galeano, E.J.; Latorre-Correa, F.; Agudelo-Suárez, A.A. Effect of Polishing Systems on the Surface Roughness of Nano-Hybrid and Nano-Filling Composite Resins: A Systematic Review. Dent. J. 2021, 9, 95. [Google Scholar] [CrossRef]
- Shimizu, Y.; Tada, K.; Seki, H.; Kakuta, K.; Miyagawa, Y.; Shen, J.F.; Morozumi, Y.; Kamoi, H.; Sato, S. Effects of air polishing on the resin composite-dentin interface. Odontology 2014, 102, 279–283. [Google Scholar] [CrossRef]
- Paradowska-Stolarz, A.; Wieckiewicz, M.; Kozakiewicz, M.; Jurczyszyn, K. Mechanical Properties, Fractal Dimension, and Texture Analysis of Selected 3D-Printed Resins Used in Dentistry That Underwent the Compression Test. Polymers 2023, 15, 1772. [Google Scholar] [CrossRef]





| Resin | Application |
|---|---|
| BioMed Amber Resin | Biocompatible applications requiring short-term skin or mucosal membrane contact suitable for:
|
| E (GPa) | Polishing | Aging | N | M ± SD | Me [Q1–Q3] | Min–Max |
|---|---|---|---|---|---|---|
| Compression Ec | No | No | 30 | 0.88 ± 0.03 | 0.88 [0.85–0.90] | 0.83–0.92 |
| No | Yes | 30 | 0.70 ± 0.02 | 0.70 [0.68–0.71] | 0.66–0.74 | |
| Yes | No | 31 | 0.84 ± 0.04 | 0.85 [0.81–0.87] | 0.73–0.89 | |
| Yes | Yes | 30 | 0.72 ± 0.03 | 0.71 [0.70–0.74] | 0.66–0.78 | |
| Tensile Et | No | No | 30 | 2.88 ± 0.26 | 2.83 [2.74–3.11] | 2.30–3.33 |
| No | Yes | 30 | 2.07 ± 0.30 | 2.07 [0.88–2.45] | 2.30–3.33 | |
| Yes | No | 28 | 2.67 ± 0.36 | 2.72 [2.39–2.98] | 1.78–3.17 | |
| Yes | Yes | 30 | 2.05 ± 0.28 | 2.11 [2.01–2.19] | 0.74–2.30 |
| Effect | SS | df | MS | F | p |
|---|---|---|---|---|---|
| Constant | 73.26 | 1 | 73.26 | 71835 | <0.000 |
| Artificial aging | 0.674 | 1 | 0.674 | 660.6 | <0.000 |
| Polishing | 0.002 | 1 | 0.002 | 2.28 | 0.134 |
| Artificial aging × polishing | 0.026 | 1 | 0.026 | 25.3 | <0.000 |
| Error | 0.118 | 116 |
| Effect | SS | df | MS | F | p |
|---|---|---|---|---|---|
| Constant | 702.2 | 1 | 702.2 | 7870 | <0.000 |
| Artificial aging | 15.46 | 1 | 15.46 | 173.3 | <0.000 |
| Polishing | 0.420 | 1 | 0.420 | 4.711 | <0.032 |
| Artificial aging × polishing | 0.237 | 1 | 0.237 | 2.656 | 0.106 |
| Error | 10.35 | 116 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Paradowska-Stolarz, A.; Mikulewicz, M.; Wieckiewicz, M.; Wezgowiec, J. The Influence of Polishing and Artificial Aging on BioMed Amber® Resin’s Mechanical Properties. J. Funct. Biomater. 2023, 14, 254. https://doi.org/10.3390/jfb14050254
Paradowska-Stolarz A, Mikulewicz M, Wieckiewicz M, Wezgowiec J. The Influence of Polishing and Artificial Aging on BioMed Amber® Resin’s Mechanical Properties. Journal of Functional Biomaterials. 2023; 14(5):254. https://doi.org/10.3390/jfb14050254
Chicago/Turabian StyleParadowska-Stolarz, Anna, Marcin Mikulewicz, Mieszko Wieckiewicz, and Joanna Wezgowiec. 2023. "The Influence of Polishing and Artificial Aging on BioMed Amber® Resin’s Mechanical Properties" Journal of Functional Biomaterials 14, no. 5: 254. https://doi.org/10.3390/jfb14050254
APA StyleParadowska-Stolarz, A., Mikulewicz, M., Wieckiewicz, M., & Wezgowiec, J. (2023). The Influence of Polishing and Artificial Aging on BioMed Amber® Resin’s Mechanical Properties. Journal of Functional Biomaterials, 14(5), 254. https://doi.org/10.3390/jfb14050254