Mechanisms Underlying Cytotoxicity Induced by Engineered Nanomaterials: A Review of In Vitro Studies
Abstract
:1. Introduction
2. In Vitro Toxicity Assessment
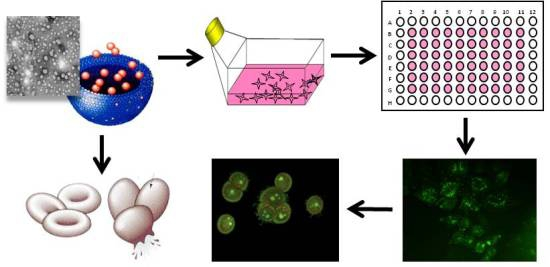
2.1. Cytotoxicity Activity
2.1.1. Cytotoxicity Assays
2.1.2. Three-Dimensional (3D) Cell Culture Systems

2.2. Alterations of Enzymatic Activity
2.3. Alterations on the Normal Cell Cycle
2.4. Induction of Apoptosis and Necrosis

2.5. Induction of Oxidative Stress

2.6. Induction of Injury in Specific Cell Organelles: Mitochondria and Lysosome
2.6.1. Mitochondrial Injury
2.6.2. Lysosomal Injury

2.7. Induction of DNA Damage and Genotoxicity

2.8. Inflammatory Responses
2.9. Interactions with Blood Components
3. Nanomaterials Characterization Needed for Reliable Nanotoxicological Assessment
4. Relationships between Cell Internalization of Nanomaterials and Their Toxicological Responses
5. Conclusions
Acknowledgments
Author contributions
Conflicts of Interest
References and Notes
- Hartung, T. Food and thought...on alternative methods for nanoparticle safety testing. ALTEX 2010, 27, 87–95. [Google Scholar]
- Horie, M.; Kato, H.; Fujita, K.; Endoh, S.; Iwahashi, H. In vitro evaluation of cellular response induced by manufactured nanoparticles. Chem. Res. Toxicol. 2012, 25, 605–619. [Google Scholar] [CrossRef]
- Paillard, A.; Hindré, F.; Vignes-Colombeix, C.; Benoit, J.-P.; Garcion, E. The importance of endo-lysosomal escape with lipid nanocapsules for drug subcellular bioavailability. Biomaterials 2010, 31, 7542–7554. [Google Scholar] [CrossRef]
- Singh, R.; Lillard, J.W., Jr. Nanoparticle-based target drug delivery. Exp. Mol. Pathol. 2009, 86, 215–223. [Google Scholar] [CrossRef]
- Sahoo, S.K.; Parveen, S.; Panda, J.J. The present and future of nanotechnology in human health care. Nanomedicine 2007, 3, 20–31. [Google Scholar] [CrossRef]
- Parveen, S.; Sahoo, S.K. Polymeric nanoparticles for cancer therapy. J. Drug Target. 2008, 16, 108–123. [Google Scholar] [CrossRef]
- Nogueira, D.R.; Tavano, L.; Mitjans, M.; Pérez, L.; Infante, M.R.; Vinardell, M.P. In vitro antitumor activity of methotrexate via pH-sensitive chitosan nanoparticles. Biomaterials 2013, 34, 2758–2772. [Google Scholar] [CrossRef]
- Robbens, J.; Vanparys, C.; Nobels, I.; Blust, R.; Hoecke, K.V.; Janssen, C.; Schamphelaere, K.D.; Roland, K.; Blanchard, G.; Silvestre, F.; et al. Eco-, geno-, and human toxicology of bio-active nanoparticles for biomedical applications. Toxicology 2010, 269, 170–181. [Google Scholar] [CrossRef]
- Donaldson, K.; Stone, V.; Tran, C.L.; Kreyling, W.; Borm, P.J.A. Nanotoxicology. Occup. Environ. Med. 2004, 61, 727–728. [Google Scholar] [CrossRef]
- Chen, C.; Li, Y.F.; Qu, Y.; Chai, Z.; Zhao, Y. Advanced nuclear analytical and related techniques for the growing challenges in nanotoxicology. Chem. Soc. Rev. 2013, 42, 8266–8303. [Google Scholar] [CrossRef]
- Oberdörster, G.; Stone, V.; Donaldson, K. Toxicology of nanoparticles: A historical perspective. Nanotoxicology 2007, 1, 1–25. [Google Scholar] [CrossRef]
- Borm, P.J.A.; Robbins, D.; Haubold, S.; Kuhlbusch, T.; Fissan, H.; Donaldson, K.; Schins, R.; Stone, V.; Kreyling, W.; Lademann, J.; et al. The potential risks of nanomaterials: A review carried out for ECETOC. Part. Fibre Toxicol. 2006, 3, 11. [Google Scholar] [CrossRef]
- Savolainen, K.; Alenius, H.; Norppa, H.; Pylkkänen, L.; Tuomi, T.; Kasper, G. Risk assessment of engineered nanomaterials and nanotechnologies—A review. Toxicology 2010, 269, 92–104. [Google Scholar] [CrossRef]
- Winkler, D.A.; Mombelli, E.; Pietroiusti, A.; Tran, L.; Worth, A.; Fadeel, B.; McCall, M.J. Applying quantitative structure-activity relationship approaches to nanotoxicology: Current status and future potential. Toxicology 2013, 313, 15–23. [Google Scholar] [CrossRef]
- Boverhof, D.R.; David, R.M. Nanomaterial characterization: Considerations and needs for hazard assessment and safety evaluation. Anal. Bioanal. Chem. 2010, 396, 953–961. [Google Scholar] [CrossRef]
- REACH (Registration, Evaluation, Authorisation and Restriction of Chemical substances), Regulation (EC) No 1907/2006 of the European Parliament and of the Council, of 18 December 2006.
- Clark, K.A.; White, R.H.; Silbergeld, E.K. Predictive models for nanotoxicology: Current challenges and future opportunities. Regulatory Toxicol. Pharmacol. 2011, 59, 361–363. [Google Scholar] [CrossRef]
- Ai, J.; Biazar, E.; Jafarpour, M.; Montazeri, M.; Majdi, A.; Aminifard, S.; Zafari, M.; Akbari, H.R.; Rad, H.G. Nanotoxicology and nanoparticle safety in biomedical designs. Int. J. Nanomed. 2011, 6, 1117–1127. [Google Scholar]
- Yang, H.; Liu, C.; Yang, D.; Zhang, H.; Xi, Z. Comparative study of cytotoxicity, oxidative stress and genotoxicity induced by four typical nanomaterials: The role of particle size, shape and composition. J. Appl. Toxicol. 2009, 29, 69–78. [Google Scholar] [CrossRef]
- Nogueira, D.R.; Morán, M.C.; Mitjans, M.; Pérez, L.; Ramos, D.; de Lapuente, J.; Vinardell, M.P. Lysine-based surfactants in nanovesicle formulations: The role of cationic charge position and hydrophobicity in in vitro cytotoxicity and intracellular delivery. Nanotoxicology 2014, 8, 404–421. [Google Scholar] [CrossRef]
- Hillegass, J.M.; Shukla, A.; Lathrop, S.A.; MacPherson, M.B.; Fukagawa, N.K.; Mossman, B.T. Assessing toxicity in cells in vitro. WIREs Nanomed. Nanotechnol. 2009, 2, 219–231. [Google Scholar]
- Jones, C.F.; Grainger, D.W. In vitro assessments of nanomaterial toxicity. Adv. Drug Deliv. Rev. 2009, 61, 438–456. [Google Scholar] [CrossRef]
- Oberdörster, G. Safety assessment for nanotechnology and nanomedicine: Concepts of nanotoxicology. J. Intern. Med. 2009, 267, 89–105. [Google Scholar] [CrossRef]
- Hartung, T. Food and thought...on cell culture. ALTEX 2007, 24, 143–147. [Google Scholar]
- Monteiro-Riviere, N.A.; Inman, A.O.; Zhang, L.W. Limitations and relative utility of screening assays to assess engineered nanoparticle toxicity in a human cell line. Toxicol. Appl. Pharmacol. 2009, 234, 222–235. [Google Scholar] [CrossRef]
- Monteiro-Riviere, N.A.; Oldenburg, S.J.; Inman, A.O. Interactions of aluminum nanoparticles with human epidermal keratinocytes. J. Appl. Toxicol. 2010, 30, 276–285. [Google Scholar] [CrossRef]
- Hartung, T.; Leist, M. Food and thought…on the evolution of toxicology and phasing out of animal testing. ALTEX 2008, 25, 91–96. [Google Scholar]
- Nyland, J.F.; Silbergeld, E.K. A nanobiological approach to nanotoxicology. Hum. Exp. Toxicol. 2009, 28, 393–400. [Google Scholar] [CrossRef]
- Oberdörster, G.; Maynard, A.; Donaldson, K.; Castranova, V.; Fitzpatrick, J.; Ausman, K.; Carter, J.; Karn, B.; Kreyling, W.; ILSI Research Foundation/Risk Science Institute Nanomaterial Toxicity Screening Working Group; et al. Principles for characterizing the potential human health effects from exposure to nanomaterials: Elements of a screening strategy. Part. Fibre Toxicol. 2005, 2, 8. [Google Scholar] [CrossRef]
- Guzelian, P.S.; Victoroff, M.S.; Halmes, C.; James, R.C. Clear path: Towards an evidence-based toxicology (EBT). Hum. Exp. Toxicol. 2009, 28, 71–79. [Google Scholar] [CrossRef]
- Nogueira, D.R.; Morán, M.C.; Mitjans, M.; Martínez, V.; Pérez, L.; Vinardell, M.P. New cationic nanovesicular systems containing lysine-based surfactants for topical administration: Toxicity assessment using representative skin cell lines. Eur. J. Pharm. Biopharm. 2013, 83, 33–43. [Google Scholar] [CrossRef]
- Ucciferri, N.; Collnot, E.-M.; Gaiser, B.; Tirella, A.; Stone, V.; Domenici, C.; Lehr, C.-M.; Ahluwalia, A. In vitro toxicological screening of nanoparticles on primary human endothelial cells and the role of flow in modulating cell respose. Nanotoxicology 2014, 8, 697–708. [Google Scholar] [CrossRef]
- Coulter, J.A.; Jain, S.; Butterworth, K.T.; Taggart, L.E.; Dickson, G.R.; McMahon, S.J.; Hyland, W.B.; Muir, M.F.; Trainor, C.; Hounsell, A.R.; et al. Cell type-dependent uptake, localization, and cytotoxicity of 1.9 nm gold nanoparticles. Int. J. Nanomed. 2012, 7, 2673–2685. [Google Scholar]
- Paul, A.; Das, S.; Das, J.; Samadder, A.; Khuda-Bukhsh, A.R. Cytotoxicity and apoptotic signalling cascade induced by chelidonine-loaded PLGA nanoparticles in HepG2 cells in vitro and bioavailability of nano-chelidonine in mice in vivo. Toxicol. Lett. 2013, 222, 10–22. [Google Scholar] [CrossRef]
- Sambandam, B.; Palanisami, E.; Abbugounder, R.; Prakhya, B.; Thiyagarajan, D. Characterizations of coal fly ash nanoparticles and induced in vitro toxicity in cell lines. J. Nanopart. Res. 2014, 16. [Google Scholar] [CrossRef]
- L’Azou, B.; Passagne, I.; Mounicou, S.; Tréguer-Delapierre, M.; Puljalté, I.; Szpunar, J.; Lobinski, R.; Ohayon-Courtès, C. Comparative cytotoxicity of cadmium forms (CdCl2, CdO, CdS micro- and nanoparticles) in renal cells. Toxicol. Res. 2014, 3, 32–41. [Google Scholar] [CrossRef]
- Ghosh, M.; Chakraborty, A.; Mukherjee, A. Cytotoxic, genotoxic and the hemolytic effect of titanium dioxide (TiO2) nanoparticles on human erythrocyte and lymphocyte cells in vitro. J. Appl. Toxicol. 2013, 33, 1097–1110. [Google Scholar] [CrossRef]
- Liao, K.-H.; Lin, Y.-S.; Macosko, C.W.; Haynes, C.L. Cytotoxicity of graphene oxide and graphene in human erythrocytes and skin fibroblasts. ACS Appl. Mater. Interfaces 2011, 3, 2607–2615. [Google Scholar] [CrossRef]
- Berridge, M.V.; Herst, P.M.; Tan, A.S. Tetrazolium dyes as tools in cell biology: New insights into their cellular reduction. Biotechnol. Annu. Rev. 2005, 11, 127–152. [Google Scholar]
- Chueh, P.J.; Lianga, R.-Y.; Leea, Y.-H.; Zenga, Z.-M.; Chuanga, S.-M. Differential cytotoxic effects of gold nanoparticles in different mammalian cell lines. J. Hazard. Mat. 2014, 264, 303–312. [Google Scholar] [CrossRef]
- Xia, T.; Kovochich, M.; Liong, M.; Zink, J.I.; Nel, A.E. Cationic polystyrene nanosphere toxicity depends on cell-specific endocytic and mitochondrial injury pathways. ACS Nano 2008, 2, 85–96. [Google Scholar] [CrossRef]
- Ojer, P.; Neutsch, L.; Gabor, F.; Irache, J.M.; de Cerain, A.L. Cytotoxicity and cell interaction studies of bioadhesivepoly(anhydride) nanoparticles for oral antigen/drug delivery. J. Biomed. Nanotechnol. 2013, 9, 1891–1903. [Google Scholar] [CrossRef]
- Vetten, M.A.; Tlotleng, N.; Rascher, D.T.; Skepu, A.; Keter, F.K.; Boodhia, K.; Koekemoer, L.A.; Andraos, C.; Tshikhudo, R.; Gulumian, M. Label-free in vitro toxicity and uptake assessment of citrate stabilised gold nanoparticles in three cell lines. Part. Fibre Toxicol. 2013, 10, 50. [Google Scholar] [CrossRef]
- Ha, S.-W.; Sikorski, J.A.; Weitzmann, M.N.; Beck, G.R., Jr. Bio-active engineered 50 nm silica nanoparticles with bone anabolic activity: Therapeutic index, effective concentration, and cytotoxicity profile in vitro. Toxicol. In Vitro 2014, 28, 354–364. [Google Scholar] [CrossRef]
- Foldbjerg, R.; Wang, J.; Beer, C.; Thorsen, K.; Sutherland, D.S.; Autrup, H. Biological effects induced by BSA-stabilized silica nanoparticles in mammalian cell lines. Chem. Biol. Interac. 2013, 204, 28–38. [Google Scholar] [CrossRef]
- Sun, X.; Wang, Z.; Zhai, S.; Cheng, Y.; Liu, J.; Liu, B. In vitro cytotoxicity of silver nanoparticles in primary rat hepatic stellate cells. Mol. Med. Rep. 2013, 8, 1365–1372. [Google Scholar]
- Chuang, S.M.; Lee, Y.H.; Liang, R.Y.; Roam, G.D.; Zeng, Z.M.; Tu, H.F.; Wang, S.K.; Chueh, P.J. Extensive evaluations of the cytotoxic effects of gold nanoparticles. Biochim. Biophys. Acta 2013, 830, 4960–4973. [Google Scholar]
- Nymark, P.; Catalán, J.; Suhonen, S.; Jarventaus, H.; Birkedal, R.; Clausen, P.A.; Jensen, K.A.; Vippola, M.; Savolainen, K.; Norppa, H. Genotoxicity of polyvinylpyrrolidone-coated silver nanoparticles in BEAS 2B cells. Toxicology 2013, 313, 38–48. [Google Scholar] [CrossRef]
- Karlsson, H.L.; Cronholm, P.; Hedberg, Y.; Tornberg, M.; de Battice, L.; Svedhem, S.; Wallinder, I.O. Cell membrane damage and protein interaction induced by copper containing nanoparticles—Importance of the metal release process. Toxicology 2013, 313, 59–69. [Google Scholar] [CrossRef]
- Hwang, T.-L.; Sung, C.T.; Aljuffali, I.A.; Chang, Y.-T.; Fang, J.-Y. Cationic surfactants in the form of nanoparticles and micelles elicit different human neutrophil responses: A toxicological study. Colloids Surf. B Biointerfaces 2014, 114, 334–341. [Google Scholar] [CrossRef]
- Haniu, H.; Saito, N.; Matsuda, Y.; Kim, Y.A.; Park, K.C.; Tsukahara, T.; Usui, Y.; Aoki, K.; Shimizu, M.; Ogihara, N.; et al. Elucidation mechanism of different biological responses to multi-walled carbon nanotubes using four cell lines. Int. J. Nanomed. 2011, 6, 3487–3497. [Google Scholar]
- Darolles, C.; Sage, N.; Armengaud, J.; Malard, V. In vitro assessment of cobalt oxide particle toxicity: Identifying and circumventing interference. Toxicol. In Vitro 2013, 27, 1699–1710. [Google Scholar] [CrossRef]
- Sahu, S.C.; Zheng, J.; Graham, L.; Chen, L.; Ihried, J.; Yourick, J.J.; Sprando, R.L. Comparative cytotoxicity of nanosilver in human liver HepG2 and colon Caco2 cells in culture. J. Appl. Toxicol. 2014. [Google Scholar] [CrossRef]
- Everett, W.N.; Chernb, C.; Suna, D.; McMahonb, R.E.; Zhanga, X.; Chenc, W.-J.A.; Hahn, M.S.; Sue, H.-J. Phosphate-enhanced cytotoxicity of zinc oxide nanoparticles andagglomerates. Toxicol. Lett. 2014, 225, 177–184. [Google Scholar] [CrossRef]
- Demir, E.; Akça, H.; Kaya, B.; Burgucu, D.; Tokgün, O.; Turna, F.; Aksakal, S.; Vales, G.; Creus, A.; Marcos, R. Zinc oxide nanoparticles: Genotoxicity, interactions with UV-light and cell-transforming potential. J. Hazard Mater. 2014, 264, 420–429. [Google Scholar] [CrossRef]
- De Simone, U.; Manzo, L.; Profumo, A.; Coccini, T. In vitro toxicity evaluation of engineered cadmium-coated silica nanoparticles on human pulmonary cells. J. Toxicol. 2013, 2013. [Google Scholar] [CrossRef]
- Prodan, A.M.; Iconaru, S.L.; Ciobanu, C.S.; Chifiriuc, M.C.; Stoicea, M.; Predoi, D. Iron oxide magnetic nanoparticles: Characterization and toxicity evaluation by in vitro and in vivo assays. J. Nanomater. 2013, 2013, 587021:1–587021:10. [Google Scholar]
- Tran, T.B.; Nguyen, P.D.; Um, S.H.; Son, S.J.; Min, J. Real-time monitoring in vitro cellular cytotoxicity of silica nanotubes using electric cell-substrate impedance sensing (ECIS). J. Biomed. Nanotechnol. 2013, 9, 286–290. [Google Scholar] [CrossRef]
- Zimmer, C.C.; Liu, Y.X.; Morgan, J.T.; Yang, G.; Wang, K.H.; Kennedy, I.M.; Barakat, A.I.; Liu, G.Y. New approach to investigate the cytotoxicity of nanomaterials using single cell mechanics. J. Phys. Chem. B 2014, 118, 1246–1255. [Google Scholar] [CrossRef]
- Frohlich, E.; Meindl, C.; Roblegg, E.; Griesbacher, A.; Pieber, T.R. Cytotoxicity of nanoparticles is influenced by size, proliferation and embryogenic origin of the cells used for testing. Nanotoxicology 2012, 6, 424–439. [Google Scholar] [CrossRef]
- Nogueira, D.R.; Mitjans, M.; Infante, M.R.; Vinardell, M.P. Comparative sensitivity of tumor and non-tumor cell lines as a reliable approach for in vitro cytotoxicity screening of lysine-based surfactants with potential pharmaceutical applications. Int. J. Pharm. 2011, 420, 51–58. [Google Scholar] [CrossRef]
- Schroterová, L.; Králová, V.; Vorácová, A.; Hascová, P.; Rudorlf, E. Antiproliferative effects of selenium compounds in colon cancer cells: Comparison of different cytotoxicity assays. Toxicol. In Vitro 2009, 23, 1406–1411. [Google Scholar] [CrossRef]
- Guadagnini, R.; Halamoda Kenzaoui, B.; Cartwright, L.; Pojana, G.; Magdolenova, Z.; Bilanicova, D.; Saunders, M.; Juillerat, L.; Marcomini, A.; et al. Toxicity screenings of nanomaterials: Challenges due to interference with assay processes and components of classic in vitro tests. Nanotoxicology 2013. [Google Scholar] [CrossRef]
- Hashimoto, M.; Hirokazu, T.; Yonezawa, T.; Kawai, K.; Iijima, M.; Endo, K. Evaluation of Silver Nanoparticle toxicity to RAW264.7 cells in a three-dimensional cell culture. J. Biomater. Tissue Eng. 2014, 4, 51–58. [Google Scholar] [CrossRef]
- Sanchez, V.C.; Weston, P.; Yan, A.; Hurt, R.H.; Kane, A.B. A 3-dimensional in vitro model of epithelioidgranulomas induced by high aspect rationanomaterials. Part Fibre Toxicol. 2011, 8. [Google Scholar] [CrossRef]
- Gao, Y.; Li, M.; Chen, B.; Shen, Z.; Guo, P.; Wientjes, M.G.; Au, J.L. Predictive models of diffusive nanoparticle transport in 3-dimensional tumor cell spheroids. AAPS J. 2013, 15, 816–831. [Google Scholar] [CrossRef]
- El-Dakdouki, M.H.; Puré, E.; Huang, X. Development of drug loaded nanoparticles for tumor targeting. Part 2: Enhancement of tumor penetration through receptor mediated transcytosis in 3D tumor models. Nanoscale 2013, 5, 3904–3911. [Google Scholar] [CrossRef]
- Shi, W.-B.; Le, V.-M.; Gu, C.-H.; Zheng, Y.-H.; Lang, M.-D.; Lu, Y.-H.; Liu, J.-W. Overcoming multidrug resistance in 2D and 3D culture models by controlled drug chitosan-graft poly(caprolactone)-based nanoparticles. J. Pharm. Sci. 2014, 103, 1064–1074. [Google Scholar] [CrossRef]
- Xu, X.; Sabanayagam, C.R.; Harrington, D.A.; Farach-Carson, M.C.; Jia, X. A hydrogel-based tumor model for the evaluation of nanoparticle-based cancer therapeutics. Biomaterials 2014, 35, 3319–3330. [Google Scholar] [CrossRef]
- Rocha, E.L.; Porto, L.M.; Rambo, C.R. Nanotechnology meets 3D in vitro models: Tissue engineered tumors and cancer therapies. Mater. Sci. Eng. C 2014, 34, 270–279. [Google Scholar] [CrossRef]
- Šinko, G.; Vrček, I.V.; Goessler, W.; Leitinger, G.; Dijanošić, A.; Miljanić, S. Alteration of cholinesterase activity as possible mechanism of silver nanoparticle toxicity. Environ. Sci. Pollut. Res. 2014, 21, 1391–1400. [Google Scholar] [CrossRef]
- Wang, Z.; Zhao, J.; Li, F.; Gao, D.; Xing, B. Adsorption and inhibition of acetylcholinesterase by different nanoparticles. Chemosphere 2009, 77, 67–73. [Google Scholar] [CrossRef]
- Wang, Z.; Zhang, K.; Zhao, J.; Liu, X.; Xing, B. Adsorption and inhibition of butyrylcholinesterase by different engineered nanoparticles. Chemosphere 2010, 79, 86–92. [Google Scholar] [CrossRef]
- Ellman, G.L.; Courtney, K.D.; Andres, V.; Feather-stone, R.M. A new rapid colorimetric determination of acetylcholinesterase activity. Biochem. Pharmacol. 1961, 7, 88–95. [Google Scholar] [CrossRef]
- Deng, Z.J.; Butcher, N.J.; Mortimer, G.M.; Jia, Z.; Monteiro, M.J.; Martin, D.J.; Minchin, R.F. Interaction of human arylamine N-acetyltransferase 1 with different nanomaterials. Drug Metab. Dispos. 2014, 42, 377–383. [Google Scholar] [CrossRef]
- Käkinen, A.; Ding, F.; Chen, P.; Mortimer, M.; Kahru, A.; Ke, P.C. Interaction of firefly luciferase and silver nanoparticles and its impact on enzyme activity. Nanotechnology 2013, 24, 345101:1–345101:9. [Google Scholar]
- Ciolkowski, M.; Rozanek, M.; Bryszewska, M.; Klajnert, B. The influence of PAMAM dendrimers surface groups on their interaction with porcine pepsin. Biochim. Biophys. Acta 2013, 1834, 1982–1987. [Google Scholar] [CrossRef]
- Wang, Y.; Zhang, X.; Cheng, C.; Li, C. Mucoadhesive and enzymatic inhibitory nanoparticles for transnasal insulin delivery. Nanomedicine 2014, 9, 541–464. [Google Scholar]
- Chairuangkitti, P.; Lawanprasert, S.; Roytrakul, S.; Aueviriyavit, S.; Phummiratch, D.; Kulthong, K.; Chanvorachote, P.; Maniratanachote, R. Silver nanoparticles induce toxicity in A549 cells via ROS-dependent and ROS-independent pathways. Toxicol. In Vitro 2013, 27, 330–338. [Google Scholar] [CrossRef]
- Khatri, M.; Bello, D.; Pal, A.K.; Cohen, J.M.; Woskie, S.; Gassert, T.; Lan, J.; Gu, A.Z.; Demokritou, P.; Gaines, P. Evaluation of cytotoxic, genotoxic and inflammatory responses of nanoparticles from photocopiers in three human cell lines. Part. Fibre Toxicol. 2013, 10, 42. [Google Scholar] [CrossRef]
- McCracken, C.; Zane, A.; Knight, D.A.; Dutta, P.K.; Waldman, W.J. Minimal intestinal epithelial cell toxicity in response to short- and long-term food-relevant inorganic nanoparticle exposure. Chem. Res. Toxicol. 2013, 26, 1514–1525. [Google Scholar]
- Valodkar, M.; Jadeja, R.N.; Thounaojam, M.C.; Devkar, R.V.; Thakore, S. In vitro toxicity study of plant latex capped silver nanoparticles in human lung carcinoma cells. Mater. Sci. Eng. C 2011, 31, 1723–1728. [Google Scholar] [CrossRef]
- VanOs, R.; Lildhar, L.L.; Lehoux, E.A.; Beaulé, P.E.; Catelas, I. In vitro macrophage response to nanometer-size chromium oxide particles. J. Biomed. Mater. Res. B Appl. Biomater. 2014, 102, 149–159. [Google Scholar] [CrossRef]
- Yan, L.; Gu, Z.; Zhao, Y. Chemical mechanisms of the toxicological properties of nanomaterials: Generation of intracellular reactive oxygen species. Chem. Asian J. 2013, 8, 2342–2353. [Google Scholar] [CrossRef]
- Passagne, I.; Morille, M.; Rousset, M.; Pujalté, I.; L’azou, B. Implication of oxidative stress in size-dependent toxicity of silica nanoparticles in kidney cells. Toxicology 2012, 299, 112–124. [Google Scholar] [CrossRef]
- LeBlanc, A.J.; Moseley, A.M.; Chen, B.T.; Frazer, D.; Castranova, V.; Nurkiewicz, T.R. Nanoparticle inhalation impairs coronary microvascular reactivity via a local reactive oxygen species-dependent mechanism. Cardiovasc. Toxicol. 2010, 10, 27–36. [Google Scholar] [CrossRef]
- Shen, C.; James, S.A.; de Jonge, M.D.; Turney, T.W.; Wright, P.F.A.; Feltis, B.N. Relating cytotoxicity, zinc ions, and reactive oxygen in ZnO nanoparticle–exposed human immune cells. Toxicol. Sci. 2013, 136, 120–130. [Google Scholar] [CrossRef]
- Prasad, R.Y.; McGee, J.K.; Killius, M.G.; Suarez, D.A.; Blackman, C.F.; DeMarini, D.M.; Simmons, S.O. Investigating oxidative stress and inflammatory responses elicited by silver nanoparticles using high-throughput reporter genes in HepG2 cells: Effect of size, surface coating, and intracellular uptake. Toxicol. In Vitro 2013, 27, 2013–2021. [Google Scholar] [CrossRef]
- Akhtar, M.J.; Ahamed, M.; Kumar, S.; Siddiqui, H.; Patil, G.; Ashquin, M.; Ahmad, I. Nanotoxicity of pure silica mediated through oxidant generation rather than glutathione depletion in human lung epithelial cells. Toxicology 2010, 276, 95–102. [Google Scholar] [CrossRef]
- Roy, R.; Parashar, V.; Chauhan, L.K.; Shanker, R.; Das, M.; Tripathi, A.; Dwivedi, P.D. Mechanism of uptake of ZnO nanoparticles and inflammatory responses in macrophages require PI3K mediated MAPKs signaling. Toxicol. In Vitro 2014, 28, 457–467. [Google Scholar] [CrossRef]
- Choi, A.O.; Cho, S.J.; Desbarats, J.; Lovric, J.; Maysinger, D. Quantum dot-induced cell death involves Fas upregulation and lipid peroxidation in human neuroblastoma cells. J. Nanobiotechnol. 2007, 5, 1. [Google Scholar] [CrossRef]
- Tang, Y.; Wang, F.; Jin, C.; Liang, H.; Zhong, X.; Yang, Y. Mitochondrial injury induced by nanosized titanium dioxide in A549 cells and rats. Environ. Toxicol. Pharmacol. 2013, 36, 66–72. [Google Scholar] [CrossRef]
- Baracca, A.; Sgarbi, G.; Solaini, G.; Lenaz, G. Rhodamine 123 as a probe of mitochondrial membrane potential: Evaluation of proton flux through F(0) during ATP synthesis. Biochim. Biophys. Acta 2003, 1606, 137–146. [Google Scholar] [CrossRef]
- Kang, S.J.; Lee, Y.J.; Kim, B.M.; Choi, Y.J.; Chung, H.W. Cytotoxicity and genotoxicity of titanium dioxide nanoparticles in UVA-irradiated normal peripheral blood lymphocytes. Drug Chem. Toxicol. 2011, 34, 277–284. [Google Scholar] [CrossRef]
- Sohaebuddin, S.; Thevenot, P.T.; Baker, D.; Eaton, J.W.; Tang, L. Nanomaterial cytotoxicity is composition, size, and cell type dependent. Part. Fibre Toxicol. 2010, 7, 22. [Google Scholar] [CrossRef]
- Fröhlich, E.; Meindl, C.; Roblegg, E.; Ebner, B.; Absenger, M.; Pieber, T.R. Action of polystyrene nanoparticles of different sizes on lysosomal function and integrity. Part. Fibre Toxicol. 2012, 9, 26. [Google Scholar] [CrossRef]
- Lindberg, H.K.; Falck, G.C.; Singh, R.; Suhonen, S.; Järventaus, H.; Vanhala, E.; Catalán, J.; Farmer, P.B.; Savolainen, K.M.; Norppa, H. Genotoxicity of short single-wall and multi-wall carbon nanotubes in human bronchial epithelial and mesothelial cells in vitro. Toxicology 2013, 313, 24–37. [Google Scholar] [CrossRef]
- Shahbazi, M.A.; Hamidi, M.; Mäkilä, E.M.; Zhang, H.; Almeida, P.V.; Kaasalainen, M.; Salonen, J.J.; Hirvonen, J.T.; Santos, H.A. The mechanisms of surface chemistry effects of mesoporous silicon nanoparticles on immunotoxicity and biocompatibility. Biomaterials 2013, 34, 7776–7789. [Google Scholar] [CrossRef]
- Hsiao, I.-L.; Huang, Y.-J. Effects of serum on cytotoxicity of nano- and micro-sized ZnO particles. J. Nanopart. Res. 2013, 15, 1829. [Google Scholar] [CrossRef]
- Elsabahy, M.; Li, A.; Zhang, F.; Sultan, D.; Liu, Y.; Wooley, K.L. Differential immunotoxicities of poly(ethylene glycol)- vs. poly(carboxybetaine)-coated nanoparticles. J. Control. Release 2013, 172, 641–652. [Google Scholar] [CrossRef]
- Ricklin, D.; Hajishengallis, G.; Yang, K.; Lambris, J.D. Complement: A key system for immune surveillance and homeostasis. Nat. Immunol. 2010, 11, 785. [Google Scholar] [CrossRef]
- Pham, C.T.N.; Thomas, D.G.; Beiser, J.; Mitchell, L.M.; Huang, J.L.; Senpan, A.; Hu, G.; Gordon, M.; Baker, N.A.; Pan, D.; et al. Application of a hemolysis assay for analysis of complement activation by perfluorocarbon nanoparticles. Nanomed. Nanotechnol. Biol. Med. 2013. [Google Scholar] [CrossRef]
- Zarrabi, A.; Shokrgozar, M.A.; Vossoughi, M.; Farokhi, M. In vitro biocompatibility evaluations of hyperbranched polyglycerol hybrid nanostructure as a candidate for nanomedicine applications. J. Mater. Sci. Mater. Med. 2014, 25, 499–506. [Google Scholar] [CrossRef]
- Holl, M.M.B. Nanotoxicology: A personal perspective. Wiley Interdiscip. Rev. Nanomed. Nanobiotechnol. 2009, 1, 353–359. [Google Scholar] [CrossRef]
- Gaumet, M.; Vargas, A.; Gurny, R.; Delie, F. Nanoparticles for drug delivery: The need for precision in reporting particlesize parameters. Eur. J. Pharm. Biopharm. 2008, 69, 1–9. [Google Scholar] [CrossRef]
- Izak-Nau, E.; Voetz, M.; Eiden, S.; Duschl, A.; Puntes, V.F. Altered characteristics of silica nanoparticles in bovine and human serum: The importance of nanomaterial characterization prior to its toxicological evaluation. Part. Fibre Toxicol. 2013, 10, 56. [Google Scholar] [CrossRef]
- Kroll, A.; Pillukat, M.H.; Hahn, D.; Schnekenburger, J. Current in vitro methods in nanoparticle risk assessment: Limitations and challenges. Eur. J. Pharm. Biopharm. 2009, 72, 370–377. [Google Scholar] [CrossRef]
- Kang, Y.; Wu, J.; Yin, G.; Huang, Z.; Yao, Y.; Liao, X.; Chen, A.; Pu, X.; Liao, L. Preparation, characterization and in vitro cytotoxicity of indomethacin-loaded PLLA/PLGA microparticles using supercritical CO2 technique. Eur. J. Pharm. Biopharm. 2008, 70, 85–97. [Google Scholar] [CrossRef]
- Yu, L.; Cai, D.; Wang, H.; Titirici, M.-M. Synthesis of microspherical LiFePO4-carbon composites for lithium-ion batteries. Nanomaterials 2013, 3, 443–452. [Google Scholar] [CrossRef]
- How, C.W.; Rasedee, A.; Manickam, S.; Rosli, R. Tamoxifen-loaded nanostructured lipid carrier as a drug delivery system: Characterization, stability assessment and cytotoxicity. Colloids Surf. B Biointerfaces 2013, 112, 393–399. [Google Scholar] [CrossRef]
- Abdel-Mohsen, A.M.; Abdel-Rahman, R.M.; Fouda, M.M.G.; Vojtova, L.; Uhrova, L.; Hassan, A.F.; Al-Deyab, S.S.; El-Shamy, I.E.; Jancar, J. Preparation, characterization and cytotoxicity of schizophyllan/silver nanoparticle composite. Carbohydr. Polym. 2014, 102, 238–245. [Google Scholar] [CrossRef]
- Helfrich, A.; Bruchert, W.; Bettmer, J. Size characterization of Au nanoparticles by ICP-MS coupling techniques. J. Anal. At. Spectrom. 2006, 21, 431–434. [Google Scholar] [CrossRef]
- Yu, X.; Fan, H.; Liu, Y.; Shi, Z.; Jin, Z. Characterization of carbonized polydopamine nanoparticles suggests ordered supramolecular structure of polydopamine. Langmuir 2014, 30, 5497–5505. [Google Scholar] [CrossRef]
- Anuratha, M.; Jawahar, A.; Umadevi, M.; Sathe, V.G.; Vanelle, P.; Terme, T.; Meenakumari, V.; Benial, A.M.F. Orientation of N-(1-(2-chlorophenyl)-2-(2-nitrophenyl)ethyl)-4-methylbenzenesulfonamide on silver nanoparticles: SERS studies. Spectrochim. Acta A Mol. Biomol. Spectrosc. 2014, 131C, 261–267. [Google Scholar]
- Shi, J.; Hedberg, Y.; Lundin, M.; Wallinder, I.O.; Karlsson, H.L.; Möller, L. Hemolytic properties of synthetic nano- and porous silica particles: The effect of surface properties and the protection by the plasma corona. Acta Biomater. 2012, 8, 3478–3490. [Google Scholar]
- Kuehl, C.; El-Gendy, N.; Berkland, C. NanoClusters surface area allows nanoparticle dissolution with microparticle properties. J. Pharm. Sci. 2014, 103, 1787–1798. [Google Scholar] [CrossRef]
- Nagaraja, A.T.; Pradhan, S.; McShane, M.J. Poly (vinylsulfonic acid) assisted synthesis of aqueous solution stable vaterite calcium carbonate nanoparticles. J. Colloid Interface Sci. 2014, 418, 366–372. [Google Scholar] [CrossRef]
- Rejman, J.; Oberle, V.; Zuhorn, I.S.; Hoekstra, D. Size-dependent internalization of particles via the pathways of chathrin- and caveolae-mediated endocytosis. Biochem. J. 2004, 377, 159–169. [Google Scholar] [CrossRef]
- Tavano, L.; Muzzalupo, R.; Mauro, L.; Pellegrino, M.; Andò, S.; Picci, N. Transferrin-conjugated pluronic niosomes as a new drug delivery system for anticancer therapy. Langmuir 2013, 29, 12638–12646. [Google Scholar] [CrossRef]
- Liu, D.; Chen, Y.; Feng, X.; Deng, M.; Xie, G.; Wang, J.; Zhang, L.; Liu, Q.; Yuan, P. Micellar nanoparticles loaded with gemcitabine and doxorubicin showed synergistic effect. Colloids Surf. B Biointerfaces 2014, 113, 158–168. [Google Scholar] [CrossRef]
- Al Faraj, A.; Shaik, A.S.; Afzal, S.; Al Sayed, B.; Halwani, R. MR imaging and targeting of a specific alveolar macrophage subpopulation in LPS-induced COPD animal model using antibody-conjugated magnetic nanoparticles. Int. J. Nanomedicine 2014, 9, 1491–1503. [Google Scholar]
- Min, Y.; Li, J.; Liu, F.; Padmanabhan, P.; Yeow, E.K.L.; Xing, B. Recent advance of biological molecular imaging based on lanthanide-doped upconversion-luminescent nanomaterials. Nanomaterials 2014, 4, 129–154. [Google Scholar] [CrossRef]
- Tavano, L.; Vivacqua, M.; Carito, V.; Muzzalupo, R.; Caroleo, M.C.; Nicoletta, F. Doxorubicin loaded magneto-niosomes for targeted drug delivery. Colloids Surf. B Biointerfaces 2013, 102, 803–807. [Google Scholar] [CrossRef]
- Morán, M.C.; Nogueira, D.R.; Vinardell, M.P.; Miguel, M.G.; Lindman, B. Mixed protein-DNA gel particles for DNA delivery: Role of protein composition and preparation method on biocompatibility. Int. J. Pharm. 2013, 454, 192–203. [Google Scholar] [CrossRef]
- Wang, X.; Zhen, X.; Wang, J.; Zhang, J.; Wu, W.; Jiang, X. Doxorubicin delivery to 3D multicellular spheroids and tumors based on boronic acid-rich chitosan nanoparticles. Biomaterials 2013, 34, 4667–4679. [Google Scholar] [CrossRef]
- Lv, S.; Li, M.; Tang, Z.; Song, W.; Sun, H.; Liu, H.; Chen, X. Doxorubicin-loaded amphiphilic polypeptide-based nanoparticles as an efficient drug delivery system for cancer therapy. Acta Biomater. 2013, 9, 9330–9342. [Google Scholar] [CrossRef]
- Pollock, S.; Antrobus, R.; Newton, L.; Kampa, B.; Rossa, J.; Latham, S.; Nichita, N.B.; Dwek, R.A.; Zitzmann, N. Uptake and trafficking of liposomes to the endoplasmic reticulum. FASEB J. 2010, 24, 1866–1878. [Google Scholar] [CrossRef]
- Ng, C.-T.; Li, J.J.; Gurung, R.L.; Hande, M.P.; Ong, C.-N.; Bay, B.-H.; Yung, L.-Y.L. Toxicological profile of small airway epithelial cells exposed to gold nanoparticles. Exp. Biol. Med. 2013, 238, 1355–1361. [Google Scholar]
© 2014 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Nogueira, D.R.; Mitjans, M.; Rolim, C.M.B.; Vinardell, M.P. Mechanisms Underlying Cytotoxicity Induced by Engineered Nanomaterials: A Review of In Vitro Studies. Nanomaterials 2014, 4, 454-484. https://doi.org/10.3390/nano4020454
Nogueira DR, Mitjans M, Rolim CMB, Vinardell MP. Mechanisms Underlying Cytotoxicity Induced by Engineered Nanomaterials: A Review of In Vitro Studies. Nanomaterials. 2014; 4(2):454-484. https://doi.org/10.3390/nano4020454
Chicago/Turabian StyleNogueira, Daniele R., Montserrat Mitjans, Clarice M.B. Rolim, and M. Pilar Vinardell. 2014. "Mechanisms Underlying Cytotoxicity Induced by Engineered Nanomaterials: A Review of In Vitro Studies" Nanomaterials 4, no. 2: 454-484. https://doi.org/10.3390/nano4020454
APA StyleNogueira, D. R., Mitjans, M., Rolim, C. M. B., & Vinardell, M. P. (2014). Mechanisms Underlying Cytotoxicity Induced by Engineered Nanomaterials: A Review of In Vitro Studies. Nanomaterials, 4(2), 454-484. https://doi.org/10.3390/nano4020454