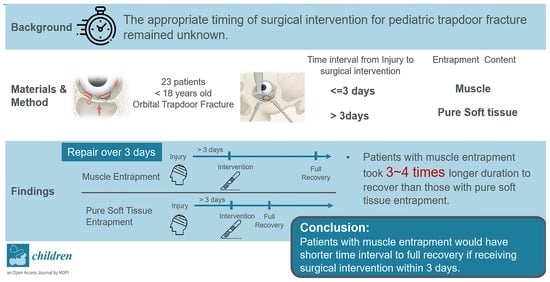
Outcome Analysis of Surgical Timing in Pediatric Orbital Trapdoor Fracture with Different Entrapment Contents: A Retrospective Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design and Participants
2.2. Procedures and Measures
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kim, J.; Lee, H.; Chi, M.; Park, M.; Lee, J.; Baek, S. Endoscope-Assisted Repair of Pediatric Trapdoor Fractures of the Orbital Floor: Characterization and Management. J. Craniofacial Surg. 2010, 21, 101–105. [Google Scholar] [CrossRef] [PubMed]
- Gerbino, G.; Roccia, F.; Bianchi, F.A.; Zavattero, E. Surgical Management of Orbital Trapdoor Fracture in a Pediatric Population. J. Oral Maxillofac. Surg. 2010, 68, 1310–1316. [Google Scholar] [CrossRef] [PubMed]
- Iliff, N.; Manson, P.N.; Katz, J.; Rever, L.; Yaremchuk, M. Mechanisms of Extraocular Muscle Injury in Orbital Fractures. Plast. Reconstr. Surg. 1999, 103, 787–799. [Google Scholar] [CrossRef] [PubMed]
- Smith, B.; Lisman, R.D.; Simonton, J.; della Rocca, R. Volkmann’s Contracture of the Extraocular Muscles Following Blowout Fracture. Plast. Reconstr. Surg. 1984, 74, 200–216. [Google Scholar] [CrossRef] [PubMed]
- Sugamata, A.; Yoshizawa, N.; Shimanaka, K. Timing of Operation for Blowout Fractures with Extraocular Muscle Entrapment. J. Plast. Surg. Hand Surg. 2013, 47, 454–457. [Google Scholar] [CrossRef] [PubMed]
- Grant, H.J., 3rd; Patrinely, J.R.; Weiss, A.H.; Kierney, P.C.; Gruss, J.S. Trapdoor Fracture of the Orbit in a Pediatric Population. Plast. Reconstr. Surg. 2002, 109, 482–489, discussion 90–95. [Google Scholar] [CrossRef] [PubMed]
- Neinstein, M.R.; Phillips, J.H.; Forrest, C.R. Pediatric Orbital Floor Trapdoor Fractures: Outcomes and Ct-Based Morphologic Assessment of the Inferior Rectus Muscle. J. Plast. Reconstr. Aesthet. Surg. 2012, 65, 869–874. [Google Scholar] [CrossRef] [PubMed]
- Yoon, C.K.; Seo, M.S.; Park, Y.G. Orbital Trapdoor Fracture in Children. J. Korean Med. Sci. 2003, 18, 881–885. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Su, Q.Y.; Shen, B.X.; Lin, M.; Fan, X. Delayed Surgical Treatment of Orbital Trapdoor Fracture in Paediatric Patients. Br. J. Ophthalmol. 2019, 103, 523–526. [Google Scholar] [CrossRef] [PubMed]
- Yang, W.J.; Woo, J.E.; An, H.J. Surgical Outcomes of Orbital Trapdoor Fracture in Children and Adolescents. J. Craniomaxillofac. Surg. 2015, 43, 444–447. [Google Scholar] [CrossRef] [PubMed]
- Criden, R.M.; Ellis, F.J. Linear Nondisplaced Orbital Fractures with Muscle Entrapment. J. Am. Assoc. Pediatr. Ophthalmol. Strabismus 2007, 11, 142–147. [Google Scholar] [CrossRef] [PubMed]
- Jordan, R.D.; Allen, L.H.; White, J.; Harvey, J.; Pashby, R.; Esmaeli, B. Intervention within Days for Some Orbital Floor Fractures: The White-Eyed Blowout. Ophthalmic Plast. Reconstr. Surg. 1998, 14, 379–390. [Google Scholar] [CrossRef] [PubMed]
- Alinasab, B.; Qureshi, A.R.; Stjärne, P. Prospective Study on Ocular Motility Limitation Due to Orbital Muscle Entrapment or Impingement Associated with Orbital Wall Fracture. Injury 2017, 48, 1408–1416. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Parbhu, C.K.; Galler, K.E.; Li, C.; Mawn, L.A. Underestimation of Soft Tissue Entrapment by Computed Tomography in Orbital Floor Fractures in the Pediatric Population. Ophthalmology 2008, 115, 1620–1625. [Google Scholar] [CrossRef] [PubMed]
- Sires, S.B.; Stanley, R.B., Jr.; Levine, L.M. Oculocardiac Reflex Caused by Orbital Floor Trapdoor Fracture: An Indication for Urgent Repair. Arch. Ophthalmol. 1998, 116, 955–956. [Google Scholar] [PubMed]
- Firriolo, M.J.; Ontiveros, N.C.; Pike, C.M.; Taghinia, A.H.; Rogers-Vizena, C.R.; Ganor, O.; Greene, A.K.; Meara, J.G.; Labow, B.I. Pediatric Orbital Floor Fractures: Clinical and Radiological Predictors of Tissue Entrapment and the Effect of Operative Timing on Ocular Outcomes. J. Craniofac. Surg. 2017, 28, 1966–1971. [Google Scholar] [CrossRef] [PubMed]
- Mehmood, N.; Hasan, A. Oculocardiac Reflex: An Underrecognized but Important Association with Orbital Trap Door Fractures. Pediatr. Emerg. Care 2021, 37, e1731–e1732. [Google Scholar] [CrossRef]
- Tarbet, C.; Siegal, N.; Tarbet, K. White-Eyed Blowout Fracture with Muscle Entrapment Misdiagnosed as Increased Intracranial Pressure: An Important Clinical Lesson. Am. J. Emerg. Med. 2021, 48, 375.e1–375.e3. [Google Scholar] [CrossRef] [PubMed]
| Score | Definition |
|---|---|
| 3 | No limitation in one direction of gaze |
| 2 | Active movement range > 50% of primary position to the edge of conjunctiva without full motion in one direction of gaze |
| 1 | Active movement range < 50% of primary position to the edge of conjunctiva without full motion in one direction of gaze |
| 0 | No movement in one direction of gaze |
| Patient Characteristics (n = 23) | Mean (SD) | |
|---|---|---|
| Age (Y) | 10.78 (±3.57) | |
| Gender (M:F) | 17:6 | |
| Side (Right: Left) | 15:11 | |
| Fracture Site (Orbital Floor: Medial Wall) | 20:3 | |
| Entrapment content (Muscle: Soft tissue) | 12:11 | |
| Injury Mechanism (n) | Fall: 7 | MVA: 3 |
| Assault: 6 | Sports: 2 | |
| Blunt trauma: 5 | ||
| Time Interval from Injury to Intervention (Days) | 12.95 (±16.84) | |
| Muscle: 6.03 (±8.79) | ||
| Soft Tissue: 20.50 (±19.99) | ||
| Pre-OP EOM movement Score | 0.90 (±1.07) | |
| Muscle: 0.25 (±0.60) | ||
| Soft Tissue: 1.59 (±1.04) | ||
| Post-OP EOM movement Score | 2.80 (±0.64) | |
| Improvement in EOM movement restriction | 1.9 (±1.1) | |
| Full Recovery Rate of EOM movement restriction | 87.0% (±33.68%) | |
| Pre-OP Diplopia (percentage) | 87.0% (±33.68%) | |
| Post-OP Diplopia (percentage) | 26.09% (±43.91%) | |
| Full Recovery Rate of Diplopia | 73.91% (±43.91%) | |
| Interval to full recovery of EOM movement restriction (Days) | 174.47 (±244.91) | |
| Interval to full recovery of Diplopia (Days) | 293.75 (±537.09) | |
| Time Interval (Days) | Pre-OP EOM Movement | Pre-OP Diplopia | Post-OP EOM Movement | EOM Movement Full Recovery Rate | Interval to Full EOM Movement Recovery | Persistent Diplopia | Interval to Diplopia Recovery |
|---|---|---|---|---|---|---|---|
| ≤3 Days (n = 7) | 0.21 ± 0.36 | 71.43 ± 45.18% | 2.86 ± 0.36 | 85.71 ± 34.99% | 84.07 ± 54.68 | 14.29% ± 34.99% | 91.06 ± 51.80 |
| >3 Days (n = 16) | 1.19 ± 1.18 | 93.75 ± 24.21% | 2.81 ± 0.73 | 87.50 ± 33.07% | 214.01 ± 291.70 | 31.25% ± 46.35% | 382.42 ± 643.04 |
| p-Value | p = 0.082 | p = 0.209 | p = 0.585 | p = 1.000 | p = 0.624 | p = 0.621 | p = 0.535 |
| Entrapment Content | Pre-OP EOM Movement | Pre-OP Diplopia | Post-OP EOM Movement | EOM Movement Full Recovery Rate | Interval to Full EOM Movement Recovery | Persistent Diplopia | Interval to Diplopia Recovery | |
|---|---|---|---|---|---|---|---|---|
| ≤3 Day (n = 7) | Muscle (n = 6): | 0.17 ± 0.37 | 83.33 ± 37.27% | 2.83 ± 0.37 | 83.33 ± 37.27% | 96.46 ± 49.13 | 83.33 ± 37.27% | 104.62 ± 42.94 |
| Soft Tissue (n = 1): | 0.50 | 100.00% | 3.00 | 100.00% | 9.72 | 0.00% | 9.72 | |
| p-Value | p = 0.334 | p = 0.286 | p = 0.683 | p = 1.000 | p = 0.699 | p = 1.000 | p = 0.699 | |
| >3 Day (n = 16) | Muscle (n = 6): | 0.33 ± 0.75 | 83.33 ± 37.27% | 2.50 ± 1.12 | 66.67 ± 47.14% | 399.51 ± 358.18 | 50.00 ± 50.00% | 751.26 ± 832.75 |
| Soft Tissue (n = 10): | 1.70 ± 1.03 | 90.91 ± 0.29% | 3.00 | 100.00% | 102.72 ± 132.78 | 20.00 ± 40.00% | 161.11 ± 271.22 | |
| p-Value | p = 0.026 | p = 0.375 | p = 0.197 | p = 0. 125 | p = 0.030 | p = 0.299 | p = 0.030 | |
| Entrapment Content | Pre-OP EOM Movement | Pre-OP Diplopia | Post-OP EOM Movement | EOM Movement Full Recovery Rate | Interval to Full EOM Movement Recovery | Persistent Diplopia | Interval to Diplopia Recovery |
|---|---|---|---|---|---|---|---|
| Muscle (n = 12) | 0.25 ± 0.60 | 83.33 ± 37.27% | 2.67 ± 0.85 | 75.00 ± 43.30% | 247.99 ± 297.17 | 66.67 ± 47.14% | 541.78 ± 742.00 |
| Soft Tissue (n = 11) | 1.59 ± 1.04 | 90.91 ± 28.75% | 3.0 | 100.00% | 94.26 ± 129.39 | 81.82 ± 38.57% | 147.35 ± 262.23 |
| p-Value | p = 0.002 | p = 1.000 | p = 0.166 | p = 0.217 | p = 0.036 | p = 0.640 | p = 0.042 |
| Time Interval (Days) | Pre-OP EOM Movement | Pre-OP Diplopia | Post-OP EOM Movement | EOM Movement Full Recovery Rate | Interval to Full EOM Movement Recovery | Persistent Diplopia | Interval to Diplopia Recovery | |
|---|---|---|---|---|---|---|---|---|
| Muscle (n = 12) | ≤3 Days (n = 6): | 0.17 ± 0.37 | 83.33 ± 37.27% | 2.83 ± 0.37 | 83.33 ± 37.27% | 96.46 ± 49.13 | 83.33 ± 37.27% | 104.62 ± 42.94 |
| >3 Days (n = 6): | 0.33 ± 0.75 | 83.33 ± 37.27% | 2.50 ± 1.12 | 66.67 ± 47.14% | 399.51 ± 358.18 | 50.00 ± 50.00% | 751.26 ± 832.75 | |
| p-Value | p = 0.902 | p = 1.000 | p = 0.902 | p = 1.000 | p = 0.078 | p = 0.545 | p = 0.078 | |
| Soft Tissue (n = 11) | ≤3 Days (n = 1): | 0.50 | 100.00% | 3.00 | 100.00% | 9.72 | 0.00% | 9.72 |
| >3 Days (n = 10): | 1.70 ± 1.03 | 90.91 ± 0.29% | 3.00 | 100.00% | 102.72 ± 132.78 | 20.00 ± 40.00% | 161.11 ± 271.22 | |
| p-Value | p = 0.336 | p = 0.091 | - | - | p = 0.527 | p = 1.000 | p = 0.343 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hsieh, P.-J.; Liao, H.-T. Outcome Analysis of Surgical Timing in Pediatric Orbital Trapdoor Fracture with Different Entrapment Contents: A Retrospective Study. Children 2022, 9, 398. https://doi.org/10.3390/children9030398
Hsieh P-J, Liao H-T. Outcome Analysis of Surgical Timing in Pediatric Orbital Trapdoor Fracture with Different Entrapment Contents: A Retrospective Study. Children. 2022; 9(3):398. https://doi.org/10.3390/children9030398
Chicago/Turabian StyleHsieh, Pei-Ju, and Han-Tsung Liao. 2022. "Outcome Analysis of Surgical Timing in Pediatric Orbital Trapdoor Fracture with Different Entrapment Contents: A Retrospective Study" Children 9, no. 3: 398. https://doi.org/10.3390/children9030398
APA StyleHsieh, P. -J., & Liao, H. -T. (2022). Outcome Analysis of Surgical Timing in Pediatric Orbital Trapdoor Fracture with Different Entrapment Contents: A Retrospective Study. Children, 9(3), 398. https://doi.org/10.3390/children9030398