Copper Accumulation in the Lips of Brass Players: Case Report of a Rare Phenomenon
Abstract
:1. Introduction
2. Materials and Methods
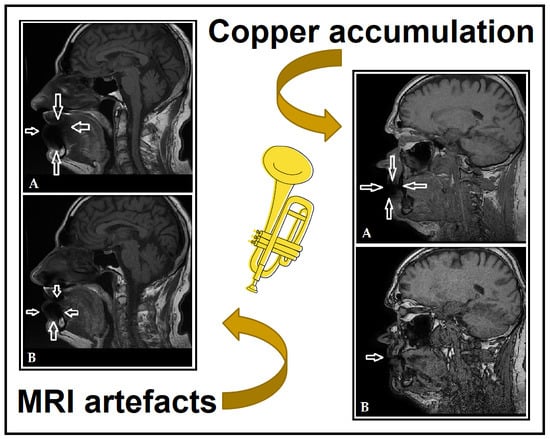
3. Results (Case Report)
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Rushton, L. The Global Burden of Occupational Disease. Curr. Environ. Health. Rep. 2017, 4, 340–348. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- WHO/ILO Joint Estimates of the Work-Related Burden of Disease and Injury, 2000–2016: Global Monitoring Report. Available online: https://www.who.int/publications/i/item/9789240034945 (accessed on 13 August 2022).
- Morell, S.; Kerr, C.; Driscoll, T.; Taylor, R.; Salkeld, G.; Corbett, S. Best estimate of the magnitude of mortality due to occupational exposure to hazardous substances. Occup. Environ. Med. 1998, 55, 634–641. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Takala, J.; Hamalainen, P.; Nenonen, N.; Takahashi, K.; Chimed-Ochir, O.; Rantanen, J. Comparative analysis of the burden of injury and illness at work in selected countries and regions. Cent. Eur. J. Occup. Environ. Med. 2017, 23, 6–31. [Google Scholar]
- Syurin, S.; Vinnikov, D. Occupational disease claims and non-occupational morbidity in a prospective cohort observation of nickel electrolysis workers. Sci. Rep. 2022, 12, e7092. [Google Scholar] [CrossRef]
- Shyagali, T.R.; Rai, N. Occupational dental health hazards: A review. Int. J. Contemp. Dent. Med. Rev. 2015, 2015, e140115. [Google Scholar]
- Petersen, P.E.; Henmar, P. Oral conditions among workers in the Danish granite industry. Scand. J. Work Environ. Health 1998, 14, 328–331. [Google Scholar] [CrossRef] [PubMed]
- Stobnicka, A.; Górny, R.L. Exposure to flour dust in the occupational environment. Int. J. Occup. Saf. Ergon. 2015, 21, 241–249. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, W.L.; Chen, Y.Y.; Wu, W.T.; Lai, C.H.; Sun, Y.S.; Wang, C.C. Examining relationship between occupational acid exposure and oral health in workplace. BMC Pub. Health 2020, 20, e1371. [Google Scholar] [CrossRef]
- Gupta, B.N. Occupational diseases of teeth. J. Soc. Occup. Med. 1990, 40, 149–152. [Google Scholar] [CrossRef] [PubMed]
- Gallagher, J.; Ashley, P.; Petrie, A.; Needleman, I. Oral health-related behaviours reported by elite and professional athletes. Brit. Dent. J. 2019, 227, 276–280. [Google Scholar] [CrossRef] [PubMed]
- Syed, M.; Chopra, R.; Sachdev, V. Allergic Reactions to Dental Materials-A Systematic Review. J. Clin. Diagn. Res. 2015, 9, ZE04–ZE09. [Google Scholar] [CrossRef]
- Lima, R.B.; Buarque, A. Oral health in the context of prevention of absenteeism and presenteeism in the workplace. Rev. Bras. Med. Trab. 2019, 17, 594–604. [Google Scholar] [CrossRef] [PubMed]
- Pilotto, L.M.; Celeste, R.K. The relationship between private health plans and use of medical and dental health services in the Brazilian health system. Ciência Saúde Coletiva 2019, 24, 2727–2736. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chong, J.; Lynden, M.; Harvey, D.; Peebles, M. Occupational Health Problems of Musicians. Can. Fam. Physician 1989, 35, 2341–2348. [Google Scholar] [PubMed]
- Yeo, D.K.L.; Pham, T.P.; Baker, J.; Porters, S.A.T. Specific orofacial problems experienced by musicians. Aust. Dent. J. 2002, 47, 2–11. [Google Scholar] [CrossRef] [PubMed]
- Raymond, D.M.; Romeo, J.H.; Kumke, K.V. A pilot study of occupational injury and illness experienced by classical musicians. Workplace Health Saf. 2012, 60, 19–24. [Google Scholar] [CrossRef]
- Cavalcanti, A.L.; Souto, J.M.V.; Brand, L.M.T.; Fernandes, L.H.F.; de Alencar, C.R.B.; Cavalcanti, A.F.C. Is playing string or wind musical instruments a risk factor for temporomandibular dysfunction? A Systematic Review. J. Oral Res. 2017, 6, 299–306. [Google Scholar] [CrossRef] [Green Version]
- Eisen, D.; Zee, R.Y.L.; Farmelant, J.; Eisen, S.E. Contaminated Musical Wind Instruments as a Vector for Disease Transmission. Adv. Dent. Oral Health 2022, 15, 555912. [Google Scholar]
- Lund, A.E. Used musical instruments may pose oral health risk. J. Am. Dent. Assoc. 2011, 142, 490–491. [Google Scholar] [CrossRef]
- Barbieri, C.B.; Diomede, A.; Domingues, N.R.A.P.; Pasquinelli, F.; Pimentel, A.C.; Roman-Torres, C.V.G. Musicians of wind instruments and oral condition. J. Dent. Oral Care Med. 2020, 6, 1–4. [Google Scholar]
- Tischenko, K.I.; Beloglazkina, E.K.; Mazhuga, A.G.; Zyk, N.V. Copper-containing enzymes: Site types and low-molecular-weight model compounds. Rev. J. Chem. 2016, 6, 49–82. [Google Scholar] [CrossRef]
- Taylor, A.A.; Tsuji, J.S.; Garry, M.R.; McArdle, M.E.; Goodfellow, W.L., Jr.; Adams, W.J.; Menzie, C.A. Critical Review of Exposure and Effects: Implications for Setting Regulatory Health Criteria for Ingested Copper. Environ. Manag. 2020, 65, 131–159. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Haase, L.M.; Birk, T.; Bachand, A.; Mundt, K. A Health Surveillance Study of Workers Employed at a Copper Smelter—Effects of Long-Term Exposure to Copper on Lung Function Using Spirometric Data. J. Occup. Environ. Med. 2021, 63, e480–e489. [Google Scholar] [CrossRef]
- Ozturk, M.; Karacelebi, E.; Gungor, K.; Coskun, S.; Boysan, E. Evaluation of oxidative events and copper accumulatıon in oral tissues of patients wıth Wilson’s disease: Three case report. Int. J. Clin. Exp. Pathol. 2015, 8, 3943–3945. [Google Scholar]
- Donoghue, A.M.; Ferguson, M.M. Superficial copper staining of the teeth in a brass foundry worker. Occup. Med. 1996, 46, 233–234. [Google Scholar] [CrossRef] [PubMed]
- Herrström, P.; Högstedt, B. Clinical study of oral galvanism: No evidence of toxic mercury exposure but anxiety disorder an important background factor. Scand. J. Dent. Res. 1993, 101, 232–237. [Google Scholar] [CrossRef] [PubMed]
- Quezada-Castillo, E.; Aguilar-Castro, W.; Quezada-Alván, B. Corrosion of galvanic pairs of dental alloys copper base with silver amalgams in artificial saliva. Matéria 2019, 24, e12299. [Google Scholar] [CrossRef]
- Sutow, E.J.; Maillet, W.A.; Taylor, J.C.; Hall, G.C. In vivo galvanic currents of intermittently contacting dental amalgam and other metallic restorations. Dent. Mater. 2004, 20, 823–831. [Google Scholar] [CrossRef] [PubMed]
- Nagao, T.; Warnakulasuriya, S.; Hasegawa, S.; Sakuma, H.; Miyabe, S.; Komaki, K.; Ishii, K.; Machida, J.; Kimura, H.; Kuroyanagi, N.; et al. Elucidating risk factors for oral leukoplakia affecting gingivae in Japanese subjects. Transl. Res. Oral Oncol. 2016, 1, 1–11. [Google Scholar] [CrossRef] [Green Version]
- Sachdev, P.K.; Freeland-Graves, J.; Beretvas, N.S.; Sanjeevi, N. Zinc, Copper, and Iron in Oral Submucous Fibrosis: A Meta-Analysis. Int. J. Dent. 2018, 2018, e3472087. [Google Scholar] [CrossRef] [Green Version]
- Grover, N.; Sharma, J.; Sengupta, S.; Singh, S.; Singh, N.; Kaur, H. Long-term effect of tobacco on unstimulated salivary pH. J. Oral Maxilofac. Pathol. 2016, 20, 16–19. [Google Scholar] [CrossRef] [Green Version]
- Kanwar, A.; Sah, K.; Grover, N.; Chandra, S.; Singh, R.R. Long-term effect of tobacco on resting whole mouth salivary flow rate and pH: An institutional based comparative study. Exp. J. Gen. Dent. 2013, 2, 296–300. [Google Scholar] [CrossRef]
- Flügge, T.; Ludwig, U.; Amrein, P.; Kernen, F.; Vach, K.; Maier, J.; Nelson, K. MRI for the display of autologous onlay bone grafts during early healing—An experimental study. Dentomax. Radiol. 2020, 50, e2020068. [Google Scholar] [CrossRef]
- Wanner, L.; Ludwig, U.; Hövener, J.B.; Nelson, K.; Flügge, T. Magnetic resonance imaging—A diagnostic tool for postoperative evaluation of dental implants: A case report. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2018, 125, e103–e107. [Google Scholar] [CrossRef] [PubMed]
- Nagy, Á.L.; Tóth, Z.; Tarjányi, T.; Práger, N.T.; Baráth, Z.L. Biomechanical properties of the bone during implant placement. BMC Oral Health 2021, 21, e86. [Google Scholar] [CrossRef]
- Mohr, I.; Weiss, K.H. Current anti-copper therapies in management of Wilson disease. Ann. Transl. Med. 2019, 7, S69. [Google Scholar] [CrossRef] [PubMed]


| Patient 1 | Patient 2 | |
|---|---|---|
| Sex | male | male |
| Age | 63 years | 61 years |
| Underlying conditions | none | glaucoma |
| Medication use | none | latanoprost |
| Known allergies | none | none |
| Tobacco and alcohol consumption | alcohol: very rarely tobacco: between 5–10 cigarettes/day | alcohol: very rarely tobacco: >25 cigarettes/day |
| Oral health status | fixed implants, metal-ceramic crowns | composite and amalgam fillings, metal-fused porcelain bridge in the upper right quadrant, chronic periodontitis, partially missing teeth |
| Type of mouthpiece | Stowasser | Schlagmüller U3 |
| Instrument cleaning practices | infrequently, using Sidol | none reported |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Baráth, Z.; Heltai, N.; Kereszty, É.; Kiss, I.; Gajdács, M.; Práger, N.T.; Kárpáti, K.; Matusovits, D. Copper Accumulation in the Lips of Brass Players: Case Report of a Rare Phenomenon. Dent. J. 2022, 10, 203. https://doi.org/10.3390/dj10110203
Baráth Z, Heltai N, Kereszty É, Kiss I, Gajdács M, Práger NT, Kárpáti K, Matusovits D. Copper Accumulation in the Lips of Brass Players: Case Report of a Rare Phenomenon. Dentistry Journal. 2022; 10(11):203. https://doi.org/10.3390/dj10110203
Chicago/Turabian StyleBaráth, Zoltán, Nóra Heltai, Éva Kereszty, Ildikó Kiss, Márió Gajdács, Nándor Tamás Práger, Krisztina Kárpáti, and Danica Matusovits. 2022. "Copper Accumulation in the Lips of Brass Players: Case Report of a Rare Phenomenon" Dentistry Journal 10, no. 11: 203. https://doi.org/10.3390/dj10110203
APA StyleBaráth, Z., Heltai, N., Kereszty, É., Kiss, I., Gajdács, M., Práger, N. T., Kárpáti, K., & Matusovits, D. (2022). Copper Accumulation in the Lips of Brass Players: Case Report of a Rare Phenomenon. Dentistry Journal, 10(11), 203. https://doi.org/10.3390/dj10110203